Evaluation of Long-Term Outcomes of Congenital Diaphragmatic Hernia
A special issue of Children (ISSN 2227-9067).
Deadline for manuscript submissions: closed (25 September 2022) | Viewed by 7704
Special Issue Editors
Interests: congenital diaphragmatic hernia; congenital anatomical malformations; outcome studies; neurodevelopmental outcomes; standardized assessment instruments; quality of life; risk stratification
Interests: myelomeningocele; pulmonary hypertension; pulmonary hypoplasia; perioperative care of the surgical neonate; ECMO; neonatal resuscitation
Special Issue Information
Dear Colleagues,
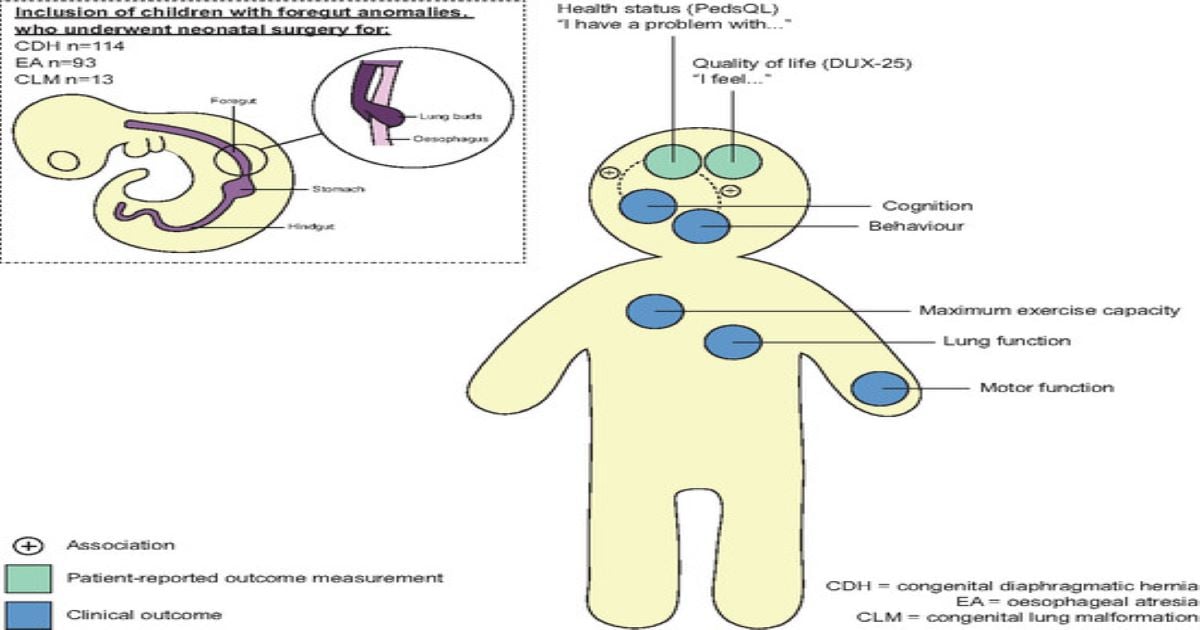
As a result of improved prenatal diagnosis, protocolized perinatal care, and implementation of new treatment modalities, more neonates born with Congenital Diaphragmatic Hernia (CDH) now survive. During the past decades, interest has shifted from survival to long-term outcomes. We have learned that, apart from having disease-specific morbidities, children with CDH are at risk for neurodevelopmental problems and failure of educational attainments which may affect their participation in society. International collaboration to develop long-term multidisciplinary follow-up programs for these children is important not only to improve their outcome at an individual level, but also to define universal outcome sets for future intervention trials.
This Special Edition will explore standardized outcomes in children and adolescents with CDH and the availability and validity of multidisciplinary assessment instruments that have been used in this population.
The goal is to provide an update of research in the field of long-term outcomes in CDH and to encourage clinicians to use standardized assessments for follow-up and intervention studies.
Dr. Hanneke IJsselstijn
Dr. Natalie E. Rintoul
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Children is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2400 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- congenital diaphragmatic hernia
- pulmonary imaging
- neuro-imaging
- outcome studies
- neurodevelopmental outcomes
- standardized assessment instruments
- proxy-reports
- self-reports
- quality of life
- risk stratification






