The Pain at Work Toolkit for Employees with Chronic or Persistent Pain: A Collaborative-Participatory Study
Abstract
:1. Introduction
2. Methods
2.1. Step 1: Stakeholder Consultation Event
2.2. Step 2: Employee Survey
2.3. Step 3: Employer Survey
2.4. Step 4: Toolkit Development and Expert Peer Review
3. Results
3.1. Step 1: Stakeholder Consultation Event
3.2. Step 2: Employee Survey
3.2.1. Employee Characteristics
3.2.2. Employee Concerns and Challenges
“Inability to have flexible working to help me manage my health and still do my role, not everyone needs to be in the office every day”.
“I share a workspace, so the fact that I have to adjust the chair, computer etc every shift, rather than having a permanent set up, can be difficult”.
“Going to meetings when I can’t have the right support. I need back support and a footrest then I’m fine, but meeting rooms usually have awful chairs-no back support and impossible to reach the floor. I also couldn’t hot desk as I need too many personal accessories, like a back rest, special mouse and keyboard, footrest”.
“I got pain and swelling in my wrists which can make typing and scrolling on computers difficult. I often have to stop writing which delays my work”.
“Continuing to meet my daily obligations, no matter how much pain I am in that day or that week. Hard sometimes to keep up a cheery exterior”.
“Not having a work life balance-putting too much energy into work and not leaving energy for fun or anything else…trying not to show how hard I work to prove I can still do it”.
“The sporadic nature of living with a long-term health condition… I can have periods of months with few problems and then a flare up which requires hospital treatment”.
“Some days can be much worse in terms of pain and the impact is greater”.
“Each day is changeable. I might be having a good day and able to meet some of the more physical elements of my role one day, then the next be struggling even with less active tasks”.
“Others not understanding that because you don’t ‘look in pain’ you must be a whinger or making it up. Fear if you admit how much pain you are in, they will fire you or retire you or you won’t get promotions”.
“Having a suitable ergonomic desk and chair has made a massive difference, but it has been challenging when colleagues have not appreciated how necessary or important these items are to me”.
“I work in large open plan office and if you ask for adjustments the other people in the office will complain and senior management will blame me for it”.
“I feel I have to apologise for being in pain. My job does not get adapted and I feel that if I make too much of an issue I will lose my employment, especially in these times”.
“[there is a] lack of clarity around how pain related sick leave would be managed in line with current HR policy”.
“Sickness absence policy isn’t set up for people with chronic or persistent pain”.
3.2.3. Impacts of a Global Pandemic on Work and Pain
“At work I have access to a standing desk and ergonomic chair. Since the pandemic hit, I’m working from home all the time, but I have no access to those”.
“Currently, I am on slightly reduced hours as I don’t have all my reasonable adjustments at home, but I am still completing the same work as I would in full-time hours”.
“Recent changes for COVID-19 mean I am now full time from home and coping extremely well”.
“My health has improved massively since lock down as I can start later and work later on days when pain and stiffness are too hard in the morning”.
“I work from home and do not work set hours, which means I can work around my pain, even working from bed when necessary”.
3.2.4. Employee Solutions
“The only thing which would make a work situation better is for there to be better understanding and training that chronic or persistent pain conditions are invisible and fluctuating. That would avoid some difficult conversations”.
“Educate people that not all disabilities are visible and that many of us live with conditions which are life limiting. It’s not our choice”.
“I have been provided with adapted workspace but was reminded of this repeatedly at staff meetings that it had eaten into budget”.
“Emotional support, reasonable adjustments, open environment to talk about it without me feeling embarrassed intimidated or uncomfortable or that I’m not pulling my weight or that I can’t do my job”.
3.3. Step 3: Employer Survey
3.3.1. Employer Characteristics
3.3.2. Employer Concerns and Challenges
“I am a medical doctor…before I had chronic or persistent pain it never occurred to me that there is so much ignorance and prejudice about chronic or persistent pain”.
“…Line managers ignoring the recommendations from the occupational health team…Delays in the approval and delivery of disability equipment”.
“‘anecdotal comments-Does she need a chair when a cushion will do?’ or ‘If she can’t drive long distances what’s wrong with stopping to stretch her legs?’”
“In a small company, the hardest thing is cover if someone is absent from work. People don’t tend to take sick days as they don’t want to let people down”.
3.3.3. Employer Solutions
“I thought we didn’t have anyone with chronic or persistent pain, but this did make me think about types of pain that are less visible, and as a leader it’s about being sensitive to that and knowing that people might be struggling but might not disclose it, in case they let you down. So, the biggest challenge is probably feeling safe to disclose health issues”.
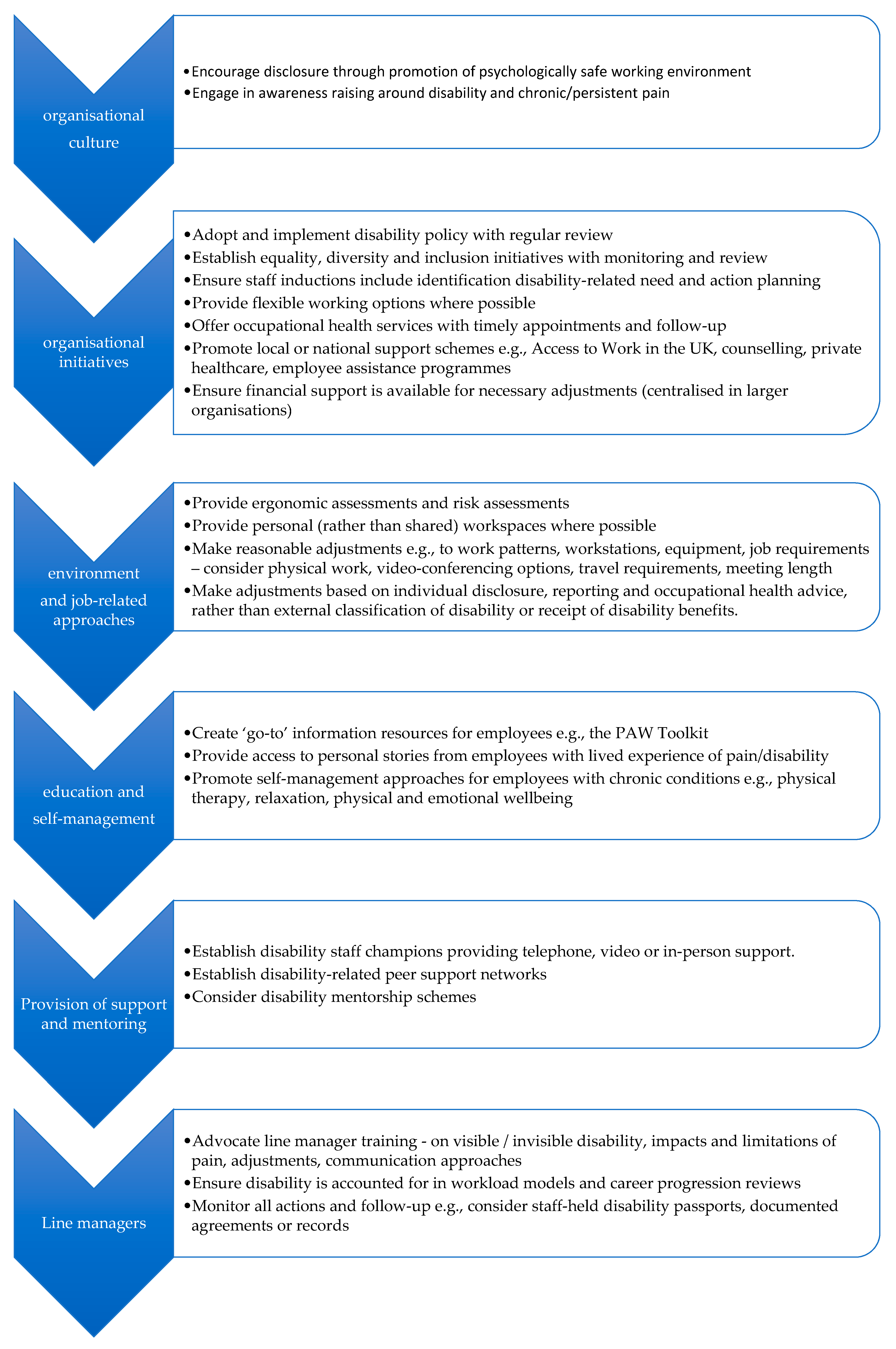
3.4. Step 4 Part 1: Virtual Peer Review Panel
3.5. Step 4 Part 2: The PAW Toolkit
4. Discussion
Study Limitations and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fayaz, A.; Croft, P.; Langford, R.M.; Donaldson, L.J.; Jones, G.T. Prevalence of chronic pain in the UK: A systematic review and meta-analysis of population studies. BMJ Open 2016, 6, e010364. [Google Scholar] [CrossRef]
- Swedish Council on Health Technology Assessment. Methods of Treating Chronic Pain: A Systematic Review; Swedish Council on Health Technology Assessment (SBU): Stockholm, Sweden, 2006. [Google Scholar]
- Iglesias-López, E.; García-Isidoro, S.; Castellanos-Sánchez, V.O. COVID-19 pandemic: Pain, quality of life and impact on public health in the confinement in Spain. Ann. Palliat. Med. 2021, 10, 4338–4353. [Google Scholar] [CrossRef]
- Shanthanna, H.; Strand, N.H.; Provenzano, D.A.; Lobo, C.A.; Eldabe, S.; Bhatia, A.; Wegener, J.; Curtis, K.; Cohen, S.P.; Narouze, S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia 2020, 75, 935–944. [Google Scholar] [CrossRef] [Green Version]
- Mun, C.J.; Campbell, C.M.; McGill, L.S.; Aaron, R.V. The Early Impact of COVID-19 on Chronic Pain: A Cross-Sectional Investigation of a Large Online Sample of Individuals with Chronic Pain in the United States, April to May, 2020. Pain Med. 2021, 22, 470–480. [Google Scholar] [CrossRef]
- Toye, F.; Seers, K.; Allcock, N.; Briggs, M.; Carr, E.; Barker, K. A synthesis of qualitative research exploring the barriers to staying in work with chronic musculoskeletal pain. Disabil. Rehabil. 2016, 38, 566–572. [Google Scholar] [CrossRef] [Green Version]
- Johannes, C.B.; Le, T.K.; Zhou, X.; Johnston, J.A.; Dworkin, R.H. The Prevalence of Chronic Pain in United States Adults: Results of an Internet-Based Survey. J. Pain 2010, 11, 1230–1239. [Google Scholar] [CrossRef]
- Breivik, H.; Collett, B.; Ventafridda, V.; Cohen, R.; Gallacher, D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 2006, 10, 287. [Google Scholar] [CrossRef]
- Karoly, P.; Ruehlman, L.S.; Okun, M.A. Psychosocial and demographic correlates of employment vs disability status in a national community sample of adults with chronic pain: Toward a psychology of pain presenteeism. Pain Med. 2013, 14, 1698–1707. [Google Scholar] [CrossRef] [Green Version]
- Jansson, C.; Mittendorfer-Rutz, E.; Alexanderson, K. Sickness absence because of musculoskeletal diagnoses and risk of all-cause and cause-specific mortality: A nationwide Swedish cohort study. Pain 2012, 153, 998–1005. [Google Scholar] [CrossRef]
- Pizzi, L.T.; Carter, C.T.; Howell, J.B.; Vallow, S.M.; Crawford, A.G.; Frank, E.D. Work Loss, Healthcare Utilization, and Costs among US Employees with Chronic Pain. Dis. Manag. Health Outcomes 2005, 13, 201–208. [Google Scholar] [CrossRef]
- Paul, K.; Moser, K. Unemployment impairs mental health: Meta-analyses. J. Vocat. Behav. 2009, 74, 264–282. [Google Scholar] [CrossRef]
- Wegrzynek, P.; Wainwright, E.; Ravalier, J. Return to work interventions for chronic pain: A systematic review. Occup. Med. 2020, 70, 268–277. [Google Scholar] [CrossRef]
- Grant, M.; O-Beirne-Elliman, J.; Froud, R.; Underwood, M.; Seers, K. The work of return to work. Challenges of returning to work when you have chronic pain: A meta-ethnography. BMJ Open 2019, 9, e025743. [Google Scholar] [CrossRef]
- Fragoso, Z.L.; McGonagle, A.K. Chronic pain in the workplace: A diary study of pain interference at work and worker strain. Stress Health 2018, 34, 416–424. [Google Scholar] [CrossRef]
- Agaliotis, M.; Mackey, M.G.; Jan, S.; Fransen, M. Perceptions of working with chronic knee pain: A qualitative study. Work 2018, 61, 379–390. [Google Scholar] [CrossRef]
- Oakman, J.; Kinsman, N.; Briggs, A.M. Working with Persistent Pain: An Exploration of Strategies Utilised to Stay Productive at Work. J. Occup. Rehabil. 2017, 27, 4–14. [Google Scholar] [CrossRef] [Green Version]
- Buruck, G.; Tomaschek, A.; Wendsche, J.; Ochsmann, E.; Dörfel, D. Psychosocial areas of worklife and chronic low back pain: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 480. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.T.; Smedley, J. Work relatedness of chronic neck pain with physical findings—A systematic review. Scand. J. Work. Environ. Health 2007, 33, 165–191. [Google Scholar] [CrossRef]
- Agaliotis, M.; Mackey, M.G.; Jan, S.; Fransen, M. Burden of reduced work productivity among people with chronic knee pain: A systematic review. Occup. Environ. Med. 2014, 71, 651–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.S.; Farquharson, R.; Carroll, D.; Moore, A.; Phillips, C.; Taylor, R.S.; Barden, J. The Impact and Burden of Chronic Pain in the Workplace: A Qualitative Systematic Review. Pain Pract. 2012, 12, 578–589. [Google Scholar] [CrossRef]
- Kronborg, C.; Handberg, G.; Axelsen, F. Health care costs, work productivity and activity impairment in non-malignant chronic pain patients. Eur. J. Health Econ. 2009, 10, 5–13. [Google Scholar] [CrossRef] [Green Version]
- Maniadakis, N.; Gray, A. The economic burden of back pain in the UK. Pain 2000, 84, 95–103. [Google Scholar] [CrossRef]
- Odenigbo, C.; Julien, N.; Douma, N.B.; Lacasse, A. The importance of chronic pain education and awareness amongst occupational safety and health professionals. J. Pain Res. 2019, 12, 1385–1392. [Google Scholar] [CrossRef] [Green Version]
- Joypaul, S.; Kelly, F.; McMillan, S.S.; King, M.A. Multi-disciplinary interventions for chronic pain involving education: A systematic review. PLoS ONE 2019, 14, e0223306. [Google Scholar] [CrossRef]
- Geneen, L.J.; Martin, D.J.; Adams, N.; Clarke, C.; Dunbar, M.; Jones, D.; McNamee, P.; Schofield, P.; Smith, B.H. Effects of education to facilitate knowledge about chronic pain for adults: A systematic review with meta-analysis. Syst. Rev. 2015, 4, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Tegner, H.; Frederiksen, P.; Esbensen, B.A.; Juhl, C. Neurophysiological Pain Education for Patients with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Clin. J. Pain 2018, 34, 778–786. [Google Scholar] [CrossRef] [Green Version]
- Andersen, L.L.; Persson, R.; Jakobsen, M.D.; Sundstrup, E. Psychosocial effects of workplace physical exercise among workers with chronic pain: Randomized controlled trial. Medicine 2017, 96, e5709. [Google Scholar] [CrossRef]
- Skamagki, G.; King, A.; Duncan, M.; Wåhlin, C. A systematic review on workplace interventions to manage chronic musculoskeletal conditions. Physiother. Res. Int. 2018, 23, e1738. [Google Scholar] [CrossRef]
- Sundstrup, E.; Jakobsen, M.D.; Brandt, M.; Jay, K.; Persson, R.; Aagaard, P.; Andersen, L.L. Workplace strength training prevents deterioration of work ability among workers with chronic pain and work disability: A randomized controlled trial. Scand. J. Work. Environ. Health 2014, 40, 244–251. [Google Scholar] [CrossRef] [Green Version]
- Hilton, L.G.; Marshall, N.J.; Motala, A.; Taylor, S.L.; Miake-Lye, I.M.; Baxi, S.; Shanman, R.M.; Solloway, M.R.; Beroesand, J.M.; Hempel, S. Mindfulness meditation for workplace wellness: An evidence map. Work 2019, 63, 205–218. [Google Scholar] [CrossRef] [Green Version]
- Hilton, L.; Hempel, S.; Ewing, B.A.; Apaydin, E.; Xenakis, L.; Newberry, S.; Colaiaco, B.; Maher, A.R.; Shanman, R.M.; Sorbero, M.E.; et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann. Behav. Med. 2017, 51, 199–213. [Google Scholar] [CrossRef] [Green Version]
- Jay, K.; Brandt, M.; Hansen, K.; Sundstrup, E.; Jakobsen, M.D.; Schraefel, M.C.; Sjogaard, G.; Andersen, L.L. Effect of Individually Tailored Biopsychosocial Workplace Interventions on Chronic Musculoskeletal Pain and Stress Among Laboratory Technicians: Randomized Controlled Trial. Pain Physician 2015, 18, 459–471. [Google Scholar] [CrossRef]
- Caputo, G.M.; Di Bari, M.; Orellana, J.N. Group-based exercise at workplace: Short-term effects of neck and shoulder resistance training in video display unit workers with work-related chronic neck pain—A pilot randomized trial. Clin. Rheumatol. 2017, 36, 2325–2333. [Google Scholar] [CrossRef]
- Aas, R.W.; Tuntland, H.; Holte, K.A.; Røe, C.; Lund, T.; Marklund, S.; Moller, A. Workplace interventions for neck pain in workers. Cochrane Database Syst. Rev. 2011, 4, CD008160. [Google Scholar] [CrossRef]
- Bell, J.-A.; Burnett, A. Exercise for the Primary, Secondary and Tertiary Prevention of Low Back Pain in the Workplace: A Systematic Review. J. Occup. Rehabil. 2009, 19, 8–24. [Google Scholar] [CrossRef] [Green Version]
- Shojaei, S.; Tavafian, S.S.; Jamshidi, A.R.; Wagner, J. A Multidisciplinary Workplace Intervention for Chronic Low Back Pain among Nursing Assistants in Iran. Asian Spine J. 2017, 11, 419–426. [Google Scholar] [CrossRef] [Green Version]
- Slattery, B.W.; Haugh, S.; O’Connor, L.; Francis, K.; Dwyer, C.P.; O’Higgins, S.; Egan, J.; McGuire, B.E. An Evaluation of the Effectiveness of the Modalities Used to Deliver Electronic Health Interventions for Chronic Pain: Systematic Review with Network Meta-Analysis. Med. Internet Res. 2019, 21, e11086. [Google Scholar] [CrossRef] [Green Version]
- Macea, D.D.; Gajos, K.; Calil, Y.; Fregni, F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: A systematic review and meta-analysis. J. Pain 2010, 11, 917–929. [Google Scholar] [CrossRef]
- Du, S.; Liu, W.; Cai, S.; Hu, Y.; Dong, J. The efficacy of e-health in the self-management of chronic low back pain: A meta-analysis. Int. J. Nurs. Stud. 2020, 106, 103507. [Google Scholar] [CrossRef]
- Garg, S.; Garg, D.; Turin, T.C.; Chowdhury, M.F.U.; Allam, A.; Kuijpers, W.; Riva, S.; Schulz, P. Web-Based Interventions for Chronic Back Pain: A Systematic Review. J. Med. Internet Res. 2016, 18, e139. [Google Scholar] [CrossRef]
- Slater, H.; Stinson, J.N.; Jordan, J.E.; Chua, J.; Low, B.; Lalloo, C.; Pham, Q.; A Cafazzo, J.; Briggs, A.M. Evaluation of Digital Technologies Tailored to Support Young People’s Self-Management of Musculoskeletal Pain: Mixed Methods Study. J. Med. Internet Res. 2020, 22, e18315. [Google Scholar] [CrossRef]
- Minen, M.T.; Torous, J.; Raynowska, J.; Piazza, A.; Grudzen, C.; Powers, S.; Lipton, R.; Sevick, M.A. Electronic behavioral interventions for headache: A systematic review. J. Headache Pain 2016, 17, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scariot, C.A.; Heemann, A.; Padovani, S. Understanding the collaborative-participatory design. Work 2012, 41 (Suppl. S1), 2701–2705. [Google Scholar] [CrossRef] [Green Version]
- Blake, H.; Bermingham, F.; Johnson, G.; Tabner, A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int. J. Environ. Res. Public Health 2020, 17, 2997. [Google Scholar] [CrossRef]
- Blake, H.; Somerset, S.; Evans, C. Development and Fidelity Testing of the Test@Work Digital Toolkit for Employers on Workplace Health Checks and Opt-In HIV Testing. Int. J. Environ. Res. Public Health 2020, 17, 379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gartshore, E.; Briggs, L.; Blake, H. Development and evaluation of an educational training package to promote health and wellbeing. Br. J. Nurs. 2017, 21, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- ATLASSIAN Agile Coach: Kanban. How the Kanban Methodology Applies to Software Development. Available online: https://www.atlassian.com/agile/kanban (accessed on 17 November 2021).
- Hoffmann, T.; Glasziou, P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, 1687. [Google Scholar] [CrossRef] [Green Version]
- Agile Alliance, Manifesto for Agile Software Development. 2001. Available online: https://www.agilealliance.org/agile101/the-agile-manifesto/ (accessed on 4 November 2021).
- Ruiz, J.G.; Candler, C.; Teasdale, T.A. Peer Reviewing E-Learning: Opportunities, Challenges, and Solutions. Acad. Med. 2007, 82, 503–507. [Google Scholar] [CrossRef]
- The University of Nottingham. The Xerte Project. Available online: https://www.nottingham.ac.uk/xerte/index.aspx (accessed on 17 November 2021).
- Statista. Employment Rate in the United Kingdom from May 1992 to October 2021, by Age Group. Available online: https://www.statista.com/statistics/280228/uk-employment-rate-by-age-group/ (accessed on 3 December 2021).
- Greaves, S.; Somerset, S.; Abbott-Fleming, V.; Blake, H. Pain at Work (PAW) Toolkit: A Toolkit for People with Chronic or Persistent Pain at Work; Version 1; The University of Nottingham: Nottingham, UK, 2021; Available online: https://www.nottingham.ac.uk/toolkits/play_24452 (accessed on 17 November 2021).
- Fernandes, L.G.; Devan, H.; Fioratti, I.; Kamper, S.J.; Williams, C.M.; Saragiotto, B.T. At my own pace, space, and place. Pain 2021. [Google Scholar] [CrossRef]
- Bertin, P.; Fagnani, F.; Duburcq, A.; Woronoff, A.-S.; Chauvin, P.; Cukierman, G.; Tropé-Chirol, S.; Joubert, J.-M.; Kobelt, G. Impact of rheumatoid arthritis on career progression, productivity, and employability: The PRET Study. Jt. Bone Spine 2016, 83, 47–52. [Google Scholar] [CrossRef]
- Shahnasarian, M. Career Rehabilitation: Integration of Vocational Rehabilitation and Career Development in the Twenty-First Century. Career Dev. Q. 2001, 49, 275–283. [Google Scholar] [CrossRef]
- Smith, B.H.; Elliott, A.M.; Chambers, W.A.; Smith, W.C.; Hannaford, P.C.; Penny, K. The impact of chronic pain in the community. Fam. Pract. 2001, 18, 292–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Vries, H.J.; Reneman, M.F.; Groothoff, J.W.; Geertzen, J.H.B.; Brouwer, S. Factors promoting staying at work in people with chronic nonspecific musculoskeletal pain: A systematic review. Disabil. Rehabil. 2012, 34, 443–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tick, H.; Nielsen, A.; Pelletier, K.R.; Bonakdar, R.; Simmons, S.; Glick, R.; Ratner, E.; Lemmon, R.L.; Wayne, P.; Zador, V. Pain Task Force of the Academic Consortium for Integrative Medicine and Health. Evidence-Based Nonpharmacologic Strategies for Comprehensive Pain Care: The Consortium Pain Task Force White Paper. Explore 2018, 14, 177–211. [Google Scholar] [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 4, CD011279. [Google Scholar]
- Searle, A.; Spink, M.; Ho, A.; Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2015, 29, 1155–1167. [Google Scholar] [CrossRef] [PubMed]
- Arimi, S.A.; Bandpei, M.A.M.; Javanshir, K.; Rezasoltani, A.; Biglarian, A. The Effect of Different Exercise Programs on Size and Function of Deep Cervical Flexor Muscles in Patients with Chronic Nonspecific Neck Pain: A Systematic Review of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2017, 96, 582–588. [Google Scholar] [CrossRef]
- Kong, L.; Lauche, R.; Klose, P.; Bu, J.H.; Yang, X.C.; Guo, C.Q.; Dobos, G.; Cheng, Y.W. Tai Chi for Chronic Pain Conditions: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sci. Rep. 2016, 6, 25325. [Google Scholar] [CrossRef]
- Cramer, H.; Klose, P.; Brinkhaus, B.; Michalsen, A.; Dobos, G. Effects of yoga on chronic neck pain: A systematic review and meta-analysis. Clin. Rehabil. 2017, 11, 1457–1465. [Google Scholar] [CrossRef] [PubMed]
- Patti, A.; Bianco, A.; Paoli, A.; Messina, G.; Montalto, M.A.; Bellafiore, M.; Battaglia, G.; Iovane, A.; Palma, A. Effects of Pilates exercise programs in people with chronic low back pain: A systematic review. Medicine 2015, 94, e383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, C.; Kolt, G.S.; Marshall, P.; Hill, B.; Bialocerkowski, A. The effectiveness of Pilates exercise in people with chronic low back pain: A systematic review. PLoS ONE 2014, 9, e100402. [Google Scholar] [CrossRef]
- Brain, K.; Burrows, T.L.; Rollo, M.E.; Chai, L.K.; Clarke, E.D.; Hayes, C.; Hodson, F.J.; Collins, C.E. A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain. J. Hum. Nutr. Diet. 2019, 32, 198–225. [Google Scholar] [CrossRef] [PubMed]
- Ball, E.; Sharizan, E.N.S.M.; Franklin, G.; Rogozinska, E. Does mindfulness meditation improve chronic pain? A systematic review. Curr. Opin. Obstet. Gynecol. 2017, 29, 359–366. [Google Scholar] [CrossRef]
- Nelson, N.L.; Churilla, J.R. Massage Therapy for Pain and Function in Patients with Arthritis: A Systematic Review of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2017, 96, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Vickers, A.J.; Cronin, A.M.; Maschino, A.C.; Lewith, G.; MacPherson, H.; Foster, N.E.; Sherman, K.J.; Witt, C.M.; Linde, K. Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: Individual patient data meta-analysis. Arch. Intern. Med. 2012, 172, 1444–1453. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.S.; Clark, J.; Colclough, J.A.; Dale, E.; McMillan, D. Acceptance and Commitment Therapy (ACT) for Chronic Pain: A Systematic Review and Meta-Analyses. Clin. J. Pain 2017, 33, 552–568. [Google Scholar] [CrossRef]
- Veehof, M.M.; Trompetter, H.R.; Bohlmeijer, E.T.; Schreurs, K.M.G. Acceptance and mindfulness-based interventions for the treatment of chronic pain: A meta-analytic review. Cogn. Behav. Ther. 2016, 45, 5–31. [Google Scholar] [CrossRef]
- Williams, A.C.; Eccleston, C.; Morley, S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2012, 11, CD007407. [Google Scholar] [CrossRef]
- Thabrew, H.; Stasiak, K.; Hetrick, S.E.; Wong, S.; Huss, J.H.; Merry, S.N. E-Health interventions for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst. Rev. 2018, 8, CD012489. [Google Scholar] [CrossRef]
- Sander, L.B.; Paganini, S.; Terhorst, Y.; Schlicker, S.; Lin, J.; Spanhel, K.; Buntrock, C.; Ebert, D.D.; Baumeister, H. Effectiveness of a Guided Web-Based Self-help Intervention to Prevent Depression in Patients with Persistent Back Pain: The PROD-BP Randomized Clinical Trial. JAMA Psychiatry 2020, 27, e201021. [Google Scholar] [CrossRef]
- Orhan, C.; Van Looveren, E.; Cagnie, B.; Mukhtar, N.B.; Lenoir, D.; Meeus, M. Are Pain Beliefs, Cognitions, and Behaviors Influenced by Race, Ethnicity, and Culture in Patients with Chronic Musculoskeletal Pain: A Systematic Review. Physician 2018, 21, 541–558. [Google Scholar]
- Federation of Small Businesses (FSB). UK Small Business Statistics. Business Population Estimates for the UK and Regions in 2020. Available online: https://www.fsb.org.uk/uk-small-business-statistics.html (accessed on 21 November 2021).
- Arocena, P.; Núñez, I. An empirical analysis of the effectiveness of occupational health and safety management systems in SMEs. Int. Small Bus. J. 2010, 28, 398–419. [Google Scholar] [CrossRef]
- Clark, T.R. The 4 Stages of Psychological Safety: Defining the Path to Inclusion and Innovation; Berrett-Koehler: Oakland, CA, USA, 2020. [Google Scholar]
- Grant, M.; Rees, S.; Underwood, M.; Froud, R. Obstacles to returning to work with chronic pain: In-depth interviews with people who are off work due to chronic pain and employers. BMC Musculoskelet. Disord. 2019, 20, 486. [Google Scholar] [CrossRef]
- Mirpuri, S.; Gill, P.; Ocampo, A.; Roberts, N.; Narang, B.; Hwang, S.W.; Gany, F. Discrimination and Health Among Taxi Drivers in New York and Toronto. J. Community Health 2018, 43, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Sung, H.; Kim, J.-H.; Punnett, L.; Kim, S.-S. Perceived discrimination and low back pain among 28,532 workers in South Korea: Effect modification by labor union status. Soc. Sci. Med. 2017, 177, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Carney, J. A Step Toward a Cultural Transformation in the Way Pain is Perceived, Judged and Treated. Practical Bioethics: A blog of the Centre for Practical Bioethics. 2015. Available online: http://practicalbioethics.blogspot.com/2015/07/a-step-toward-cultural-transformation.html (accessed on 21 November 2021).
- Nielson, A. Journeys with Chronic Pain: Acquiring Stigma along the Way. In At the Edge of Being: The Aporia of Pain; McKenzie, H., Quintner, J., Bendelow, G., Eds.; Brill: Leiden, The Netherlands, 2012; pp. 83–97. [Google Scholar]
- Clauw, D.J.; Häuser, W.; Cohen, S.P.; Fitzcharlesf, M.A. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain 2020, 161, 1694–1697. [Google Scholar] [CrossRef]
- Puntillo, F.; Giglio, M.; Brienza, N.; Viswanath, O.; Urits, I.; Kaye, A.D.; Pergolizzi, J.; Paladini, A.; Varrassi, G. Impact of COVID-19 pandemic on chronic pain management: Looking for the best way to deliver care. Best Pr. Res. Clin. Anaesthesiol. 2020, 34, 529–537. [Google Scholar] [CrossRef]
- Nyblade, L.; Stockton, M.A.; Giger, K.; Bond, V.; Ekstrand, M.L.; Mc Lean, R.; Mitchell, E.M.H.; Nelson, L.R.E.; Sapag, J.C.; Siraprapasiri, T.; et al. Stigma in health facilities: Why it matters and how we can change it. BMC Med. 2019, 17, 25. [Google Scholar] [CrossRef]
- Kirk-Brown, A.; Van Dijk, P. An empowerment model of workplace support following disclosure, for people with MS. Mult. Scler. J. 2014, 20, 1624–1632. [Google Scholar] [CrossRef] [PubMed]




| Survey Participants (n = 274, 100%) | Total n = 274 (100%) | |||
|---|---|---|---|---|
| Male n = 150 (54%) | Female n = 121 (43.5%) | Non-Binary n = 3 (2.5%) | ||
| Age category (years) | ||||
| 18–24 | 6 (4.0%) | 5 (4.1%) | 0 (%) | 11 (4.0%) |
| 25–34 | 24 (16.0%) | 12 (10.0%) | 0 (0.0%) | 36 (13.1%) |
| 35–44 | 35 (23.3%) | 24 (19.8%) | 3 (100.0%) | 62 (22.6%) |
| 45–54 | 53 (35.3%) | 45 (37.2%) | 0 (0.0%) | 98 (35.8%) |
| 55–64 | 31 (20.7%) | 30 (24.8%) | 0 (0.0%) | 61 (22.3%) |
| 65+ | 1 (0.7%) | 5 (4.1%) | 0 (0.0%) | 6 (2.2%) |
| Work status | 141 (94.0%) | 115 (95.0%) | 3 (100.0%) | 263 (96.0%) |
| Employed (FT/PT) | 3 (2.0%) | 3 (2.5%) | 0 (0.0%) | 6 (2.2%) |
| Long-term absent from work | 1 (0.7%) | 1 (0.8%) | 0 (0.0%) | 2 (0.7%) |
| Unemployed | 1 (0.7%) | 0 (0.0%) | 0 (0.0%) | 1 (0.4%) |
| Retired | 4 (2.7%) | 2 (1.7%) | 0 (0.0%) | 6 (2.2%) |
| Other + | 141 (94.0%) | 115 (95.0%) | 3 (100.0%) | 263 (96.0%) |
| Nature of Employee Concern |
|---|
| Pain-related concerns |
| Invisibility of pain (hidden disability) Medication and side effects (e.g., drowsinesss) Focus, concentration, memory Disturbed sleep Fatigue Low energy levels Physical fitness (as a safety concern) |
| Emotional impacts |
| Shame and guilt (related to ‘difference’, perceptions of special treatment or absence) Fear (related to job security, the need for absence) Pain-related anxiety (related to flare-ups) Job-related anxiety (related to job security) Low mood or depression |
| Quality of life impacts |
| Financial impacts (related to cost of treatment or equipment, loss of income if not offering a competitive service) Social isolation No work-life balance (related to using downtime to keep up with work because of the need to pace activities) |
| Environmental concerns |
| Prolonged sitting or standing Need to carry equipment Lack of car parking near to work area Meetings booked in different buildings Access to facilities (e.g., toilets/catering on different floor or in different building) Travel to work and between sites (walking or driving) |
| Ergonomics |
| Chairs-non-adjustable/no lumbar support No adaptions in meeting rooms Requirements for safety clothing (e.g., heavy shoes) Cramped workstations Shared workspaces and equipment (e.g., need to re-adjust daily, impacts of heat or air conditioning) Repetitive work Lack of access to desk assessment Lack of access to occupational health services |
| Job-related concerns |
| Non-disclosure (feeling unable) Workload-being unable to take breaks Length of activities (such as training sessions and meetings) Number of contracted or expected hours present at work (full days) Expectations of the job (e.g., required overnight stays) Time out to attend medical appointments Safety concerns with precision work (e.g., cutting, scoring, opening chemical bottles) Work quality impacts (related to concentration) Work productivity impacts (related to keeping to timelines and deadlines set by, or expected by others) |
| Impact of line managers and peers |
| Stigma and negative attitudes Hindered career development (related to stigma or reduced opportunities) Lack of understanding about pain impacts Lack of knowledge about support available Lack of compassion and unkindness Knowing who to talk to Knowing how to communicate about pain |
| Impacts of COVID-19 + |
| Negative impacts: Long virtual meetings (related to increased use of technology) Inappropriate space for remote working (related to cramped, shared or noisy spaces) Lack of adaptions or required equipment at home Positive impacts: Increased flexibility in working hours More control over work patterns Increased comfort (related to clothing, and sitting positions) Reduction or removal of travel (related to commuting, expectations of overnight stays, travel between and within sites) Reduced medication (related to work flexibility, increased comfort and reduced travel) |
| Organisation Size + n = 107 (100%) | Total n = 107 (100%) | ||||
|---|---|---|---|---|---|
| Micro (n = 7) | Small (n = 16) | Medium (n = 22) | Large (n = 62) | ||
| Primary job role | |||||
| Worker/employee | 0 (0.0%) | 1 (6.3%) | 3 (13.6%) | 15 (24.2%) | 19 (17.8%) |
| Middle manager/team leader | 2 (28.6%) | 5 (31.3%) | 14 (63.6%) | 33 (53.2%) | 54 (50.5%) |
| Senior manager/director/chief executive | 5 (71.4%) | 10 (62.5%) | 5 (22.7%) | 14 (22.6%) | 34 (31.8%) |
| Sector | |||||
| Public | 2 (28.6%) | 4 (25.0%) | 5 (22.7%) | 34 (54.8%) | 45 (42.1%) |
| Private | 3 (42.9) | 7 (43.7%) | 14 (63.6%) | 24 (38.7%) | 48 (44.9%) |
| Third | 2 (28.6%) | 5 (31.3%) | 3 (13.6%) | 4 (6.5%) | 14 (13.1%) |
| Organisation type | |||||
| Construction | 0 (0.0%) | 2 (12.5%) | 7 (31.8%) | 15 (24.2%) | 24 (22.4%) |
| IT and internet | 2 (28.6%) | 1 (6.3%) | 1 (4.5%) | 1 (1.6%) | 5 (4.7%) |
| Manufacturing and production | 0 (0.0%) | 2 (12.5%) | 2 (9.0%) | 0 (0.0%) | 4 (3.7%) |
| Retail | 1 (14.3%) | 2 (12.5%) | 0 (0.0%) | 1 (1.6%) | 4 (3.7%) |
| Tourism | 1 (14.3%) | 1 (6.3%) | 2 (9.0%) | 0 (0.0%) | 4 (3.7%) |
| Education | 2 (28.6%) | 1 (6.3%) | 3 (13.6%) | 29 (46.8%) | 35 (32.7%) |
| Healthcare | 1 (14.3%) | 0 (0.0%) | 3 (13.6%) | 9 (14.5%) | 13 (12.1%) |
| Other | 0 (0.0%) | 7 (43.7%) | 4 (18.2%) | 7 (11.3%) | 18 (16.8%) |
| Current provision | |||||
| Disability Policies | |||||
| Yes | 3 (42.9) | 11 (68.7%) | 11 (50.0%) | 33 (53.2%) | 58 (54.2%) |
| No | 4 (57.1%) | 5 (31.3%) | 11 (50.0%) | 29 (46.8%) | 49 (45.8%) |
| Self-management | |||||
| Yes | 0 (0.0%) | 2 (12.5%) | 3 (13.6%) | 10 (16.1%) | 15 (14.0%) |
| No | 7 (100.0%) | 14 (87.5%) | 19 (86.4%) | 52 (83.9%) | 92 (86.0%) |
| Education/training | |||||
| Yes | 0 (0.0%) | 1 (6.3%) | 0 (0.0%) | 7 (11.3%) | 8 (7.5%) |
| No | 7 (100.0%) | 15 (93.7%) | 22 (100.0%) | 55 (88.7%) | 99 (92.5%) |
| Counselling service | |||||
| Yes | 2 (28.6%) | 3 (18.8%) | 5 (22.7%) | 43 (69.4%) | 53 (49.5%) |
| No | 5 (71.4%) | 13 (81.2%) | 17 (77.3%) | 19 (30.6%) | 54 (50.5%) |
| Medical assessments | |||||
| Yes | 0 (0.0%) | 3 (18.8%) | 6 (27.3%) | 18 (29.0%) | 27 (25.2%) |
| No | 7 (100.0%) | 13 (81.2%) | 16 (72.7%) | 44 (71.0%) | 80 (74.8%) |
| Occupational health | |||||
| Yes | 3 (42.9) | 7 (43.7%) | 15 (68.2%) | 52 (83.9%) | 77 (72.0%) |
| No | 4 (57.1%) | 9 (56.3%) | 7 (31.8%) | 10 (16.1%) | 30 (28.0%) |
| Private healthcare | |||||
| Yes | 0 (0.0%) | 2 (12.5%) | 9 (41.0%) | 18 (29.0%) | 29 (27.1%) |
| No | 7 (100.0%) | 14 (87.5%) | 13 (59.0%) | 44 (71.0%) | 78 (72.9%) |
| EAP helpline | |||||
| Yes | 0 (0.0%) | 1 (6.3%) | 5 (22.7%) | 28 (45.2%) | 34 (31.8%) |
| No | 7 (100.0%) | 15 (93.7%) | 17 (77.3%) | 34 (54.8%) | 73 (68.2%) |
| Physical exercise | |||||
| Yes | 1 (14.3%) | 1 (6.3%) | 0 (0.0%) | 14 (22.6%) | 16 (15.0%) |
| No | 6 (85.7%) | 15 (93.7%) | 22 (100.0%) | 48 (77.4%) | 91 (85.0%) |
| Mental health | |||||
| Yes | 3 (42.9) | 2 (12.5%) | 10 (45.5%) | 39 (62.9%) | 54 (50.5%) |
| No | 4 (57.1) | 14 (87.5%) | 12 (54.5%) | 23 (37.1%) | 53 (49.5%) |
| Physiotherapy | |||||
| Yes | 0 (0.0%) | 0 (0.0%) | 1 (4.5%) | 11 (17.7%) | 12 (11.2%) |
| No | 7 (100.0%) | 16 (100.0%) | 21 (95.5%) | 51 (82.3%) | 95 (88.8%) |
| Nature of Employer Concern |
|---|
| Organisational concerns |
| Covering staff absence in micro and small organisations Access to funds for adaptions/support (particularly SMEs +) Absence of OH provision or lengthy referral processes for OH services Challenges of managing sickness absence Balancing risks of presenteeism (particularly risks of communicable illness) Policy concerns around absence records/disciplinary measures for repeated absences Equality Act and employee statutory rights |
| Job-related concerns |
| Managing heavy workloads Requirement for manual handling Peripatetic working practices Inflexible work patterns |
| Impact of line managers and peers |
| High level of stigma around pain and disability Negative work culture around wellbeing Managers lack understanding about pain and disability Dismissive attitudes among managers Prohibitive management behaviours (preventing or delaying support) Failure to act on OH recommendations Managers disputing OH outcomes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blake, H.; Somerset, S.; Greaves, S. The Pain at Work Toolkit for Employees with Chronic or Persistent Pain: A Collaborative-Participatory Study. Healthcare 2022, 10, 56. https://doi.org/10.3390/healthcare10010056
Blake H, Somerset S, Greaves S. The Pain at Work Toolkit for Employees with Chronic or Persistent Pain: A Collaborative-Participatory Study. Healthcare. 2022; 10(1):56. https://doi.org/10.3390/healthcare10010056
Chicago/Turabian StyleBlake, Holly, Sarah Somerset, and Sarah Greaves. 2022. "The Pain at Work Toolkit for Employees with Chronic or Persistent Pain: A Collaborative-Participatory Study" Healthcare 10, no. 1: 56. https://doi.org/10.3390/healthcare10010056
APA StyleBlake, H., Somerset, S., & Greaves, S. (2022). The Pain at Work Toolkit for Employees with Chronic or Persistent Pain: A Collaborative-Participatory Study. Healthcare, 10(1), 56. https://doi.org/10.3390/healthcare10010056







