Trends in Daily Heart Rate Variability Fluctuations Are Associated with Longitudinal Changes in Stress and Somatisation in Police Officers
Abstract
:1. Introduction
1.1. Heart Rate Variability (HRV)
1.2. Daily HRV Fluctuations
1.3. Aim of the Study
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.2.1. Stress, Anxiety, Depression and Somatisation
2.2.2. Daily HRV & Daily HRV Fluctuations
2.2.3. Control Variables
2.3. Data Analysis
3. Results
4. Discussion
4.1. Associations between Daily HRV Fluctuations, Stress and Somatisation
4.2. Floor Effects in Depression and Anxiety
4.3. Strengths and Limitations
4.4. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Folkman, S.; Lazarus, R.S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- McEwen, B.S. Stress, Adaptation, and Disease: Allostasis and Allostatic Load. Ann. N. Y. Acad. Sci. 1998, 840, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Wang, S.; Zhang, J.-Q.; Li, W. Assessing the cumulative effects of stress: The association between job stress and allostatic load in a large sample of Chinese employees. Work. Stress 2007, 21, 333–347. [Google Scholar] [CrossRef]
- Collins, P.A.; Gibbs, A.C. Stress in police officers: A study of the origins, prevalence and severity of stress-related symptoms within a county police force. Occup. Med. 2003, 53, 256–264. [Google Scholar] [CrossRef] [Green Version]
- Violanti, J.M.; Fekedulegn, D.; Andrew, M.E.; Hartley, T.A.; Charles, L.E.; Miller, D.B.; Burchfiel, C.M. The impact of perceived intensity and frequency of police work occupational stressors on the cortisol awakening response (CAR): Findings from the BCOPS study. Psychoneuroendocrinology 2017, 75, 124–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magnavita, N.; Capitanelli, I.; Garbarino, S.; Pira, E. Work-related stress as a cardiovascular risk factor in police officers: A systematic review of evidence. Int. Arch. Occup. Environ. Health 2018, 91, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Garbarino, S.; Cuomo, G.; Chiorri, C.; Magnavita, N. Association of work-related stress with mental health problems in a special police force unit. BMJ Open 2013, 3, e002791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magnavita, N.; Garbarino, S. Is Absence Related to Work Stress? A Repeated Cross-Sectional Study on a Special Police Force. Am. J. Ind. Med. 2013, 56, 765–775. [Google Scholar] [CrossRef]
- De Vries, H.; Kamphuis, W.; Oldenhuis, H.; van der Schans, C.; Sanderman, R. Modelling Employee Resilience Using Wearables and Apps: A Conceptual Framework and Research Design. Int. J. Adv. Life Sci. 2019, 11, 110–117. [Google Scholar]
- Owens, A.P. The Role of Heart Rate Variability in the Future of Remote Digital Biomarkers. Front. Neurosci. 2020, 14, 582145. [Google Scholar] [CrossRef]
- Thayer, J.F.; Sternberg, E. Beyond Heart Rate Variability: Vagal Regulation of Allostatic Systems. Ann. N. Y. Acad. Sci. 2006, 1088, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [Green Version]
- Hall, M.; Vasko, R.; Buysse, D.; Ombao, H.; Chen, Q.; Cashmere, J.D.; Kupfer, D.; Thayer, J.F. Acute Stress Affects Heart Rate Variability During Sleep. Psychosom. Med. 2004, 66, 56–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuda, E.; Shibata, M.; Ogata, Y.; Ueda, N.; Yambe, T.; Yoshizawa, M.; Hayano, J. Pulse rate variability: A new biomarker, not a surrogate for heart rate variability. J. Physiol. Anthr. 2020, 39, 21. [Google Scholar] [CrossRef]
- Perpetuini, D.; Chiarelli, A.M.; Cardone, D.; Filippini, C.; Rinella, S.; Massimino, S.; Bianco, F.; Bucciarelli, V.; Vinciguerra, V.; Fallica, P.; et al. Prediction of state anxiety by machine learning applied to photoplethysmography data. PeerJ 2021, 9, e10448. [Google Scholar] [CrossRef]
- Awasthi, K.; Nanda, P.; Suma, K.V. Performance analysis of Machine Learning techniques for classification of stress levels using PPG signals. In Proceedings of the 2020 IEEE International Conference on Electronics, Computing and Communication Technologies (CONECCT), Bangalore, India, 2–4 July 2020; pp. 1–6. [Google Scholar]
- Martens, A.; Greenberg, J.; Allen, J.J.B. Self-Esteem and Autonomic Physiology: Parallels Between Self-Esteem and Cardiac Vagal Tone as Buffers of Threat. Pers. Soc. Psychol. Rev. 2008, 12, 370–389. [Google Scholar] [CrossRef] [PubMed]
- Baethge, A.; Junker, N.M.; Rigotti, T. Does work engagement physiologically deplete? Results from a daily diary study. Work. Stress 2021, 35, 283–300. [Google Scholar] [CrossRef]
- Schmid, R.F.; Thomas, J. Teachers’ ambulatory heart rate variability as an outcome and moderating variable in the job demands-resources model. Anxiety Stress. Coping 2020, 33, 387–402. [Google Scholar] [CrossRef] [PubMed]
- De Vries, H.; Kamphuis, W.; Oldenhuis, H.; van der Schans, C.; Sanderman, R. Moderation of the Stressor-Strain Process in Interns by Heart Rate Variability Measured with a Wearable and Smartphone App: Within-Subject Design Using Continuous Monitoring. JMIR Cardio 2021, 5, e28731. [Google Scholar] [CrossRef]
- Hobfoll, S.E. The Influence of Culture, Community, and the Nested-Self in the Stress Process: Advancing Conservation of Resources Theory. Appl. Psychol. 2001, 50, 337–421. [Google Scholar] [CrossRef]
- Borchini, R.; Ferrario, M.M.; Bertù, L.; Veronesi, G.; Bonzini, M.; Dorso, M.; Cesana, G. Prolonged job strain reduces time-domain heart rate variability on both working and resting days among cardiovascular-susceptible nurses. Int. J. Occup. Med. Environ. Health 2014, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Borchini, R.; Veronesi, G.; Bonzini, M.; Gianfagna, F.; Dashi, O.; Ferrario, M.M. Heart Rate Variability Frequency Domain Alterations among Healthy Nurses Exposed to Prolonged Work Stress. Int. J. Environ. Res. Public Health 2018, 15, 113. [Google Scholar] [CrossRef] [Green Version]
- Wagner, J.A.; Feinn, R.; Lampert, R.; Bermúdez-Millán, A.; Pérez-Escamilla, R. Changes in negative affect and changes in heart rate variability among low-income latinos with type 2 diabetes in a randomized, controlled stress management trial. J. Psychosom. Res. 2019, 124, 109774. [Google Scholar] [CrossRef]
- Föhr, T.; Tolvanen, A.; Myllymäki, T.; Järvelä-Reijonen, E.; Peuhkuri, K.; Rantala, S.; Kolehmainen, M.; Korpela, R.; Lappalainen, R.; Ermes, M.; et al. Physical activity, heart rate variability-based stress and recovery, and subjective stress during a 9-month study period. Scand. J. Med. Sci. Sports 2016, 27, 612–621. [Google Scholar] [CrossRef] [Green Version]
- Zhang, M.; Liu, L.; Shi, Y.; Yang, Y.; Yu, X.; Angerer, P.; Kristensen, T.S.; Li, J. Longitudinal associations of burnout with heart rate variability in patients following acute coronary syndrome: A one-year follow-up study. Gen. Hosp. Psychiatry 2018, 53, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Wekenborg, M.K.; Hill, L.K.; Thayer, J.F.; Penz, M.; Wittling, R.A.; Kirschbaum, C. The Longitudinal Association of Reduced Vagal Tone with Burnout. Psychosom. Med. 2019, 81, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Jiang, R.; Zhu, C.; Zhang, M.; Cai, H.; Hu, Z.; Ye, Y.; Liu, Y.; Sun, H.; Ma, Y.; et al. High Job Burnout Predicts Low Heart Rate Variability in the Working Population after a First Episode of Acute Coronary Syndrome. Int. J. Environ. Res. Public Health 2021, 18, 3431. [Google Scholar] [CrossRef]
- Kanthak, M.K.; Stalder, T.; Hill, L.K.; Thayer, J.F.; Penz, M.; Kirschbaum, C. Autonomic dysregulation in burnout and depression: Evidence for the central role of exhaustion. Scand. J. Work. Environ. Health 2017, 43, 475–484. [Google Scholar] [CrossRef]
- Järvelin-Pasanen, S.; Sinikallio, S.; Tarvainen, M.P. Heart rate variability and occupational stress—Systematic review. Ind. Health 2018, 56, 500–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalmers, J.A.; Quintana, D.S.; Abbott, M.J.-A.; Kemp, A.H. Anxiety Disorders are Associated with Reduced Heart Rate Variability: A Meta-Analysis. Front. Psychiatry 2014, 5, 80. [Google Scholar] [CrossRef] [Green Version]
- Kemp, A.H.; Quintana, D.S.; Gray, M.A.; Felmingham, K.L.; Brown, K.; Gatt, J.M. Impact of Depression and Antidepressant Treatment on Heart Rate Variability: A Review and Meta-Analysis. Biol. Psychiatry 2010, 67, 1067–1074. [Google Scholar] [CrossRef]
- De Jonge, P.; Mangano, D.; Whooley, M.A. Differential Association of Cognitive and Somatic Depressive Symptoms with Heart Rate Variability in Patients with Stable Coronary Heart Disease: Findings from the Heart and Soul Study. Psychosom. Med. 2007, 69, 735–739. [Google Scholar] [CrossRef] [Green Version]
- Beauchaine, T. Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Dev. Psychopathol. 2001, 13, 183–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, T.W.; Deits-Lebehn, C.; Williams, P.G.; Baucom, B.R.W.; Uchino, B.N. Toward a social psychophysiology of vagally mediated heart rate variability: Concepts and methods in self-regulation, emotion, and interpersonal processes. Soc. Pers. Psychol. Compass 2020, 14, 12516. [Google Scholar] [CrossRef]
- Perrotta, A.S.; Koehle, M.; White, M.D.; Taunton, J.E.; Warburton, D.E. Consecutive non-training days over a weekend for assessing cardiac parasympathetic variation in response to accumulated exercise stress. Eur. J. Sport Sci. 2020, 20, 1072–1082. [Google Scholar] [CrossRef]
- Flatt, A.A.; Esco, M.R. Smartphone-Derived Heart-Rate Variability and Training Load in a Women’s Soccer Team. Int. J. Sports Physiol. Perform. 2015, 10, 994–1000. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, L.; Regnard, J.; Desmarets, M.; Mauny, F.; Mourot, L.; Fouillot, J.-P.; Coulmy, N.; Millet, G. Fatigue Shifts and Scatters Heart Rate Variability in Elite Endurance Athletes. PLoS ONE 2013, 8, e71588. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R.; Nakamura, F.Y. Individual Heart Rate Variability Responses to Preseason Training in High Level Female Soccer Players. J. Strength Cond. Res. 2017, 31, 531–538. [Google Scholar] [CrossRef]
- Figueiredo, D.H.; Moreira, A.; Gonçalves, H.R.; Stanganelli, L.C. Effect of Overload and Tapering on Individual Heart Rate Variability, Stress Tolerance, and Intermittent Running Performance in Soccer Players During a Preseason. J. Strength Cond. Res. 2019, 33, 1222–1231. [Google Scholar] [CrossRef]
- Plews, D.J.; Laursen, P.B.; Kilding, A.E.; Buchheit, M. Heart rate variability in elite triathletes, is variation in variability the key to effective training? A case comparison. Graefe’s Arch. Clin. Exp. Ophthalmol. 2012, 112, 3729–3741. [Google Scholar] [CrossRef]
- Terluin, B.; Van Marwijk, H.W.; Adèr, H.J.; De Vet, H.C.; Penninx, B.W.; Hermens, M.L.; Van Boeijen, C.A.; Van Balkom, A.J.; Van Der Klink, J.J.; Ab Stalman, W. The Four-Dimensional Symptom Questionnaire (4DSQ): A validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry 2006, 6, 34. [Google Scholar] [CrossRef] [Green Version]
- Kinnunen, H.; Rantanen, A.; Kenttä, T.; Koskimäki, H. Feasible assessment of recovery and cardiovascular health: Accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG. Physiol. Meas. 2020, 41, 04NT01. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.D.; Ulman, H.K.; Tran, K.; Thompson, A.G.; Halter, M.D.; Ramadan, J.H.; Stephenson, M.; Finomore, V.S.J.; Galster, S.M.; Rezai, A.R.; et al. Assessing the Accuracy of Popular Commercial Technologies That Measure Resting Heart Rate and Heart Rate Variability. Front. Sports Act. Living 2021, 3, 37. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Lau, Z.; Chen, S.; Makowski, D. Heart Rate Variability in Psychology: A Review of HRV Indices and an Analysis Tutorial. Sensors 2021, 21, 3998. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plews, D.J.; Laursen, P.B.; Le Meur, Y.; Hausswirth, C.; Kilding, A.E.; Buchheit, M. Monitoring Training with Heart-Rate Variability: How Much Compliance Is Needed for Valid Assessment? Int. J. Sports Physiol. Perform. 2014, 9, 783–790. [Google Scholar] [CrossRef]
- Tegegne, B.S.; Man, T.; Van Roon, A.M.; Snieder, H.; Riese, H. Reference values of heart rate variability from 10-second resting electrocardiograms: The Lifelines Cohort Study. Eur. J. Prev. Cardiol. 2020, 27, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- De Zambotti, M.; Rosas, L.; Colrain, I.M.; Baker, F.C. The Sleep of the Ring: Comparison of the ŌURA Sleep Tracker Against Polysomnography. Behav. Sleep Med. 2019, 17, 124–136. [Google Scholar] [CrossRef]
- Utility, C.; Properties, P. AUDIT-C Questionnaire. Intern. Med. 2003, 163, 2–3. [Google Scholar]
- Allaire, J.J. RStudio: Integrated Development for R.; RStudio, Inc.: Boston, MA, USA. Available online: http://www.rstudio.com. (accessed on 12 February 2021).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria. Available online: http://www.R-project.org (accessed on 16 February 2021).
- Enders, C.K.; Tofighi, D. Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychol. Methods 2007, 12, 121–138. [Google Scholar] [CrossRef]
- Bates, D.; Kliegl, R.; Vasishth, S.; Baayen, H. Parsimonious Mixed Models. arXiv 2015, arXiv:1506.04967. Available online: http://arxiv.org/abs/1506.04967 (accessed on 16 July 2021).
- Matuschek, H.; Kliegl, R.; Vasishth, S.; Baayen, H.; Bates, D. Balancing Type I error and power in linear mixed models. J. Mem. Lang. 2017, 94, 305–315. [Google Scholar] [CrossRef]
- Thayer, J.F.; Åhs, F.; Fredrikson, M.; Sollers, J.J., III.; Wager, T.D. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef]
- Flatt, A.A.; Hornikel, B.; Esco, M.R. Heart rate variability and psychometric responses to overload and tapering in collegiate sprint-swimmers. J. Sci. Med. Sport 2017, 20, 606–610. [Google Scholar] [CrossRef]
- Šimkovic, M.; Träuble, B. Robustness of statistical methods when measure is affected by ceiling and/or floor effect. PLoS ONE 2019, 14, e0220889. [Google Scholar] [CrossRef]
- Frenkel, M.O.; Giessing, L.; Egger-Lampl, S.; Hutter, V.; Oudejans, R.R.; Kleygrewe, L.; Jaspaert, E.; Plessner, H. The impact of the COVID-19 pandemic on European police officers: Stress, demands, and coping resources. J. Crim. Justice 2021, 72, 101756. [Google Scholar] [CrossRef]
- Bourdillon, N.; Jeanneret, F.; Nilchian, M.; Albertoni, P.; Ha, P.; Millet, G.P. Sleep Deprivation Deteriorates Heart Rate Variability and Photoplethysmography. Front. Neurosci. 2021, 15, 642548. [Google Scholar] [CrossRef]
| Variable | Correlation | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| 1. HRV uptrend | − | |||||||
| 2. HRVsd uptrend | −0.04 | − | ||||||
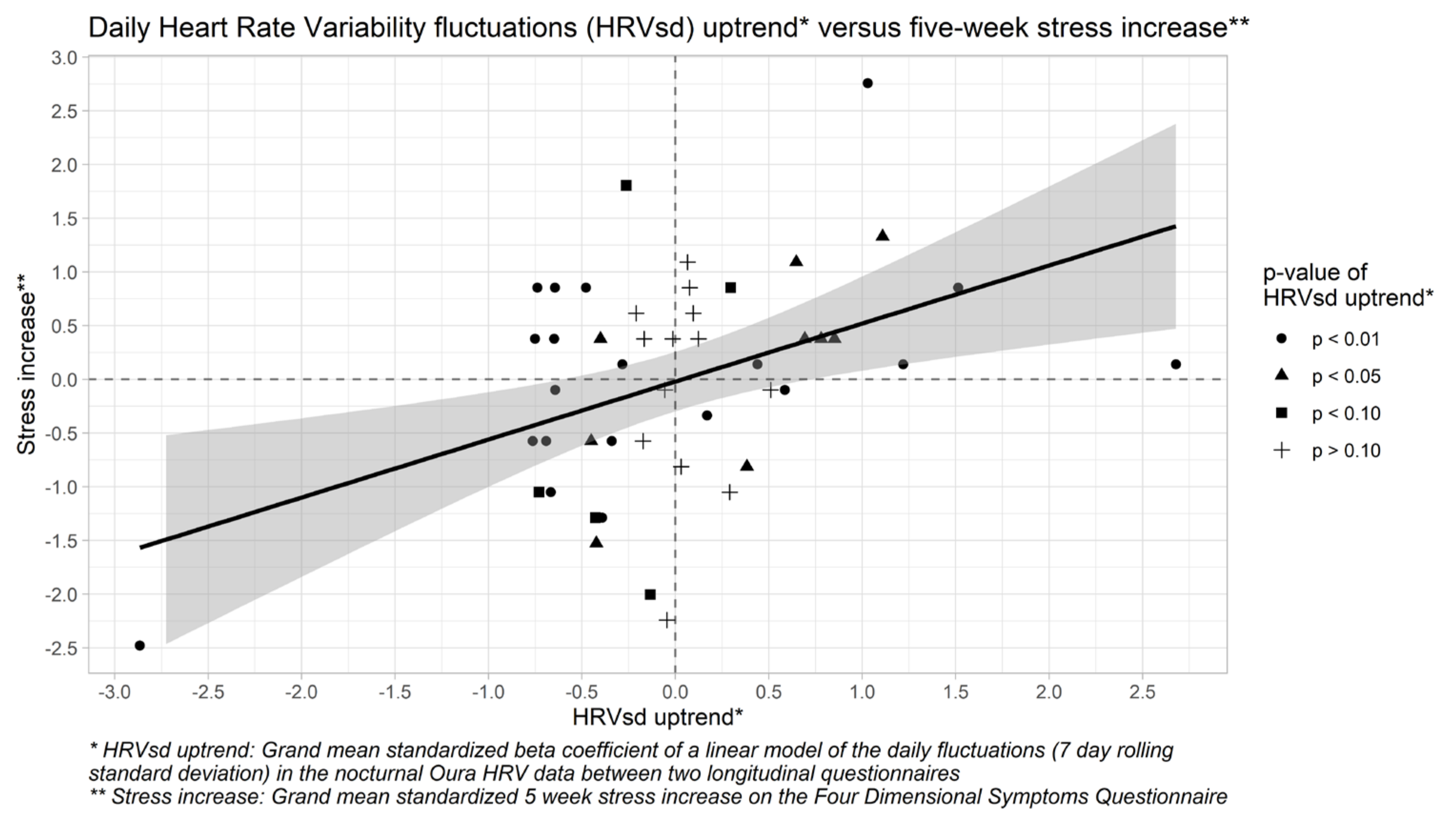
| 3. Stress increase | −0.09 | 0.43 ** | − | |||||
| 4. Anxiety increase | −0.00 | −0.04 | 0.24 | − | ||||
| 5. Depression increase | 0.06 | −0.03 | 0.31 * | 0.15 | − | |||
| 6. Somatisation increase | −0.03 | 0.42 ** | 0.56 *** | −0.03 | 0.09 | − | ||
| 7. TST uptrend | 0.01 | −0.01 | 0.11 | −0.22 | 0.10 | 0.09 | − | |
| 8. MVPA uptrend | −0.13 | 0.09 | −0.21 | −0.05 | 0.12 | −0.17 | −0.28 | − |
| 9. Alcohol use uptrend | −0.12 | −0.21 | −0.06 | 0.28 | 0.03 | −0.19 | −0.47 *** | 0.14 |
| Stress Increase | |||||
|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | |||
| Independent Variable | β | β | β | ||
| Intercept | −0.019 | −0.024 | −0.029 | ||
| TST uptrend | 0.048 | 0.075 | 0.056 | ||
| MVPA uptrend | −0.209 | −0.275 | −0.276 | ||
| Alcohol use uptrend | −0.005 | 0.100 | 0.092 | ||
| HRV uptrend | −0.098 | −0.089 | |||
| HRVsd uptrend | 0.590 | ** | 0.542 | ** | |
| HRV uptrend * HRVsd uptrend | −0.224 | ||||
| R2 | 0.047 | 0.267 | 0.291 | ||
| Adjusted R2 | −0.019 | 0.177 | 0.185 | ||
| F | 0.711 | 2.984 | * | 2.737 | * |
| ΔR2 | 0.220 | 0.024 | |||
| ΔF | 2.273 | −0.247 | |||
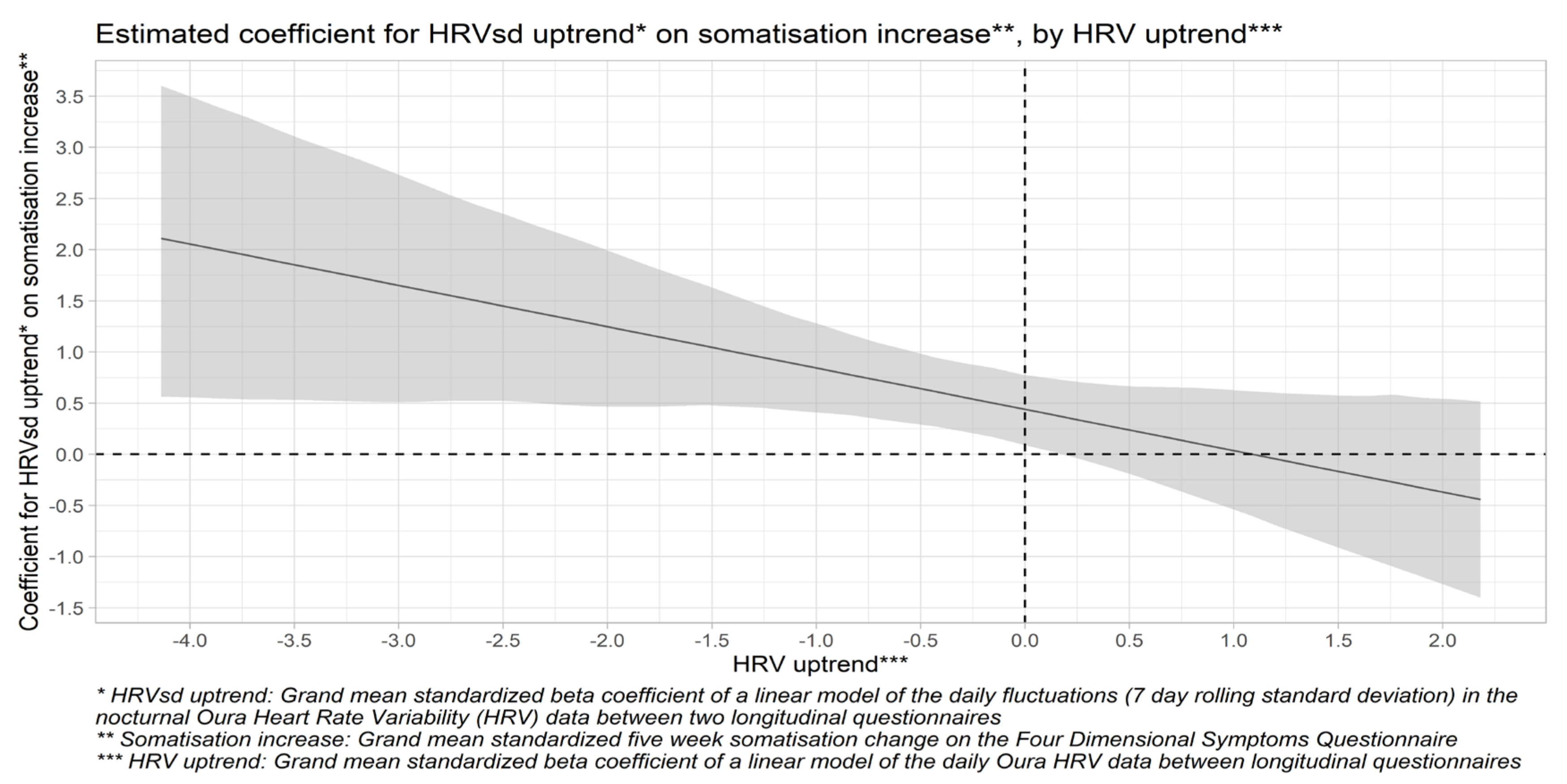
| Somatisation Increase | |||||
|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | |||
| Independent Variable | β | β | β | ||
| Intercept | 0.003 | −0.002 | −0.012 | ||
| TST uptrend | −0.051 | −0.024 | −0.058 | ||
| MVPA uptrend | −0.169 | −0.224 | −0.226 | ||
| Alcohol use uptrend | −0.191 | −0.091 | −0.107 | ||
| HRV uptrend | −0.054 | −0.038 | |||
| HRVsd uptrend | 0.530 | ** | 0.443 | * | |
| HRV uptrend * HRVsd uptrend | −0.407 | * | |||
| R2 | 0.061 | 0.234 | 0.315 | ||
| Adjusted R2 | −0.004 | 0.141 | 0.213 | ||
| F | 0.931 | 2.508 | * | 3.069 | * |
| ΔR2 | 0.173 | 0.081 | |||
| ΔF | 1.577 | 0.561 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Vries, H.; Kamphuis, W.; van der Schans, C.; Sanderman, R.; Oldenhuis, H. Trends in Daily Heart Rate Variability Fluctuations Are Associated with Longitudinal Changes in Stress and Somatisation in Police Officers. Healthcare 2022, 10, 144. https://doi.org/10.3390/healthcare10010144
de Vries H, Kamphuis W, van der Schans C, Sanderman R, Oldenhuis H. Trends in Daily Heart Rate Variability Fluctuations Are Associated with Longitudinal Changes in Stress and Somatisation in Police Officers. Healthcare. 2022; 10(1):144. https://doi.org/10.3390/healthcare10010144
Chicago/Turabian Stylede Vries, Herman, Wim Kamphuis, Cees van der Schans, Robbert Sanderman, and Hilbrand Oldenhuis. 2022. "Trends in Daily Heart Rate Variability Fluctuations Are Associated with Longitudinal Changes in Stress and Somatisation in Police Officers" Healthcare 10, no. 1: 144. https://doi.org/10.3390/healthcare10010144
APA Stylede Vries, H., Kamphuis, W., van der Schans, C., Sanderman, R., & Oldenhuis, H. (2022). Trends in Daily Heart Rate Variability Fluctuations Are Associated with Longitudinal Changes in Stress and Somatisation in Police Officers. Healthcare, 10(1), 144. https://doi.org/10.3390/healthcare10010144






