Adverse Perinatal Outcomes in COVID-19 Infected Pregnant Women: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria, Data Sources and Search Strategy
2.2. Study Selection
2.3. Data Extraction
2.4. Assessment of Risk of Bias
2.5. Data Synthesis and Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias of Included Studies
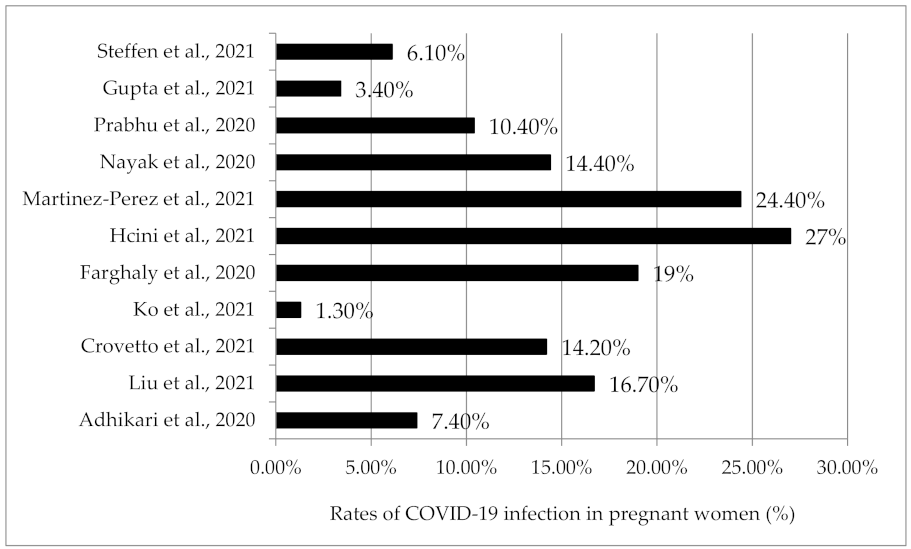
3.4. Incidence of COVID-19 Infection in Pregnant Women
3.5. Characteristics of COVID-19 Infected Pregnant Women
3.6. Summary Findings of Included Individual Studies
3.7. Adverse Perinatal Outcomes of COVID-19 Infection in Pregnancy
3.7.1. Adverse Maternal Outcomes
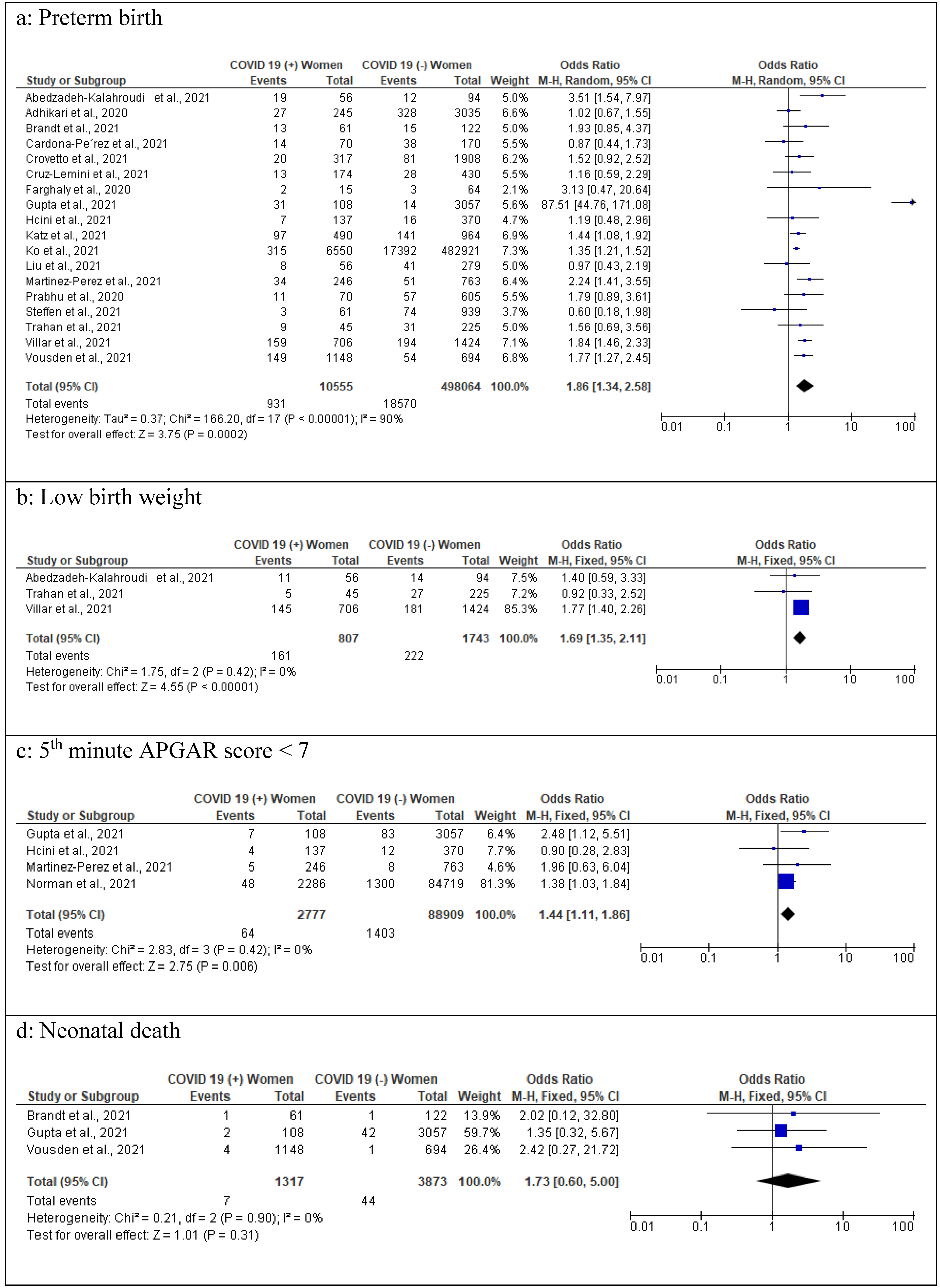
3.7.2. Adverse Fetal Outcomes
3.7.3. Adverse Neonatal Outcomes
3.8. Comorbidities among COVID-19 Pregnant Women
4. Discussion
4.1. Implications for Clinical Practice
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Situation Report—85: Coronavirus Disease 2019 (COVID-19). 2020. Available online: https://www.who.int/publications/m/item/situation-report---85 (accessed on 5 October 2021).
- Peeri, N.C.; Shrestha, N.; Rahman, M.S.; Zaki, R.; Tan, Z.; Bibi, S.; Baghbanzadeh, M.; Aghamohammadi, N.; Zhang, W.; Haque, U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int. J. Epidemiol. 2020, 49, 717–726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 4 December 2021).
- Beigi, R.H. Emerging Infectious Diseases in Pregnancy. Obstet. Gynecol. 2017, 129, 896–906. [Google Scholar] [CrossRef]
- Lapinsky, S.E. Acute respiratory failure in pregnancy. Obstet. Med. 2015, 8, 126–132. [Google Scholar] [CrossRef] [Green Version]
- WAPM (World Association of Perinatal Medicine) Working Group on COVID-19. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection. Ultrasound Obstet. Gynecol. 2021, 57, 232–241.
- Kuang, J.; Ashraf, S.; Das, U.; Bicchieri, C. Awareness, Risk Perception, and Stress during the COVID-19 Pandemic in Communities of Tamil Nadu, India. Int. J. Environ. Res. Public Health 2020, 17, 7177. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The COVID-19 Infodemic. 2021. Available online: https://www.who.int/health-topics/infodemic/the-covid-19-infodemic#tab=tab_1 (accessed on 5 December 2021).
- Sprung, C.L.; Joynt, G.M.; Christian, M.D.; Truog, R.D.; Rello, J.; Nates, J.L. Adult ICU Triage During the Coronavirus Disease 2019 Pandemic: Who Will Live and Who Will Die? Recommendations to Improve Survival. Crit. Care Med. 2020, 48, 1196–1202. [Google Scholar] [CrossRef] [PubMed]
- Breslin, N.; Baptiste, C.; Gyamfi-Bannerman, C.; Miller, R.; Martinez, R.; Bernstein, K.; Ring, L.; Landau, R.; Purisch, S.; Friedman, A.M.; et al. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am. J. Obstet. Gynecol. MFM 2020, 2, 100118. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, K.S.; Sarmento AC, A.; Martins, E.S.; Costa AP, F.; Eleutério, J., Jr.; Gonçalves, A.K. Impact of SARS-CoV-2 (COVID-19) on pregnancy: A systematic review and meta-analysis protocol. BMJ Open 2020, 10, e039933. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. Study Quality Assessment Tools; National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 2021. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 1 September 2021).
- Abedzadeh-Kalahroudi, M.; Sehat, M.; Vahedpour, Z.; Talebian, P. Maternal and neonatal outcomes of pregnant patients with COVID-19: A prospective cohort study. Int. J. Gynecol. Obstet. 2021, 153, 449–456. [Google Scholar] [CrossRef]
- Adhikari, E.H.; Moreno, W.; Zofkie, A.C.; Macdonald, L.; McIntire, D.D.; Collins, R.R.J.; Spong, C.Y. Pregnancy Outcomes Among Women With and Without Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Netw. Open 2020, 3, e2029256. [Google Scholar] [CrossRef]
- Brandt, J.S.; Hill, J.; Reddy, A.; Schuster, M.; Patrick, H.S.; Rosen, T.; Sauer, M.V.; Boyle, C.; Ananth, C.V. Epidemiology of coronavirus disease 2019 in pregnancy: Risk factors and associations with adverse maternal and neonatal outcomes. Am. J. Obstet. Gynecol. 2021, 224, 389.e1–389.e9. [Google Scholar] [CrossRef]
- Cardona-Pérez, J.A.; Villegas-Mota, I.; Helguera-Repetto, A.C.; Acevedo-Gallegos, S.; Rodríguez-Bosch, M.; Aguinaga-Ríos, M.; Coronado-Zarco, I.; León-Juárez, M.; Aguilar-Ayala, D.; Valdespino-Vázquez, M.Y.; et al. Prevalence, clinical features, and outcomes of SARS-CoV-2 infection in pregnant women with or without mild/moderate symptoms: Results from universal screening in a tertiary care center in Mexico City, Mexico. PLoS ONE 2021, 16, e0249584. [Google Scholar] [CrossRef] [PubMed]
- Crovetto, F.; Crispi, F.; Llurba, E.; Pascal, R.; Larroya, M.; Trilla, C.; Camacho, M.; Medina, C.; Dobaño, C.; Gomez-Roig, M.D.; et al. Impact of Severe Acute Respiratory Syndrome Coronavirus 2 Infection on Pregnancy Outcomes: A Population-based Study. Clin. Infect. Dis. 2021, 73, 1768–1775. [Google Scholar] [CrossRef]
- Cruz-Lemini, M.; Ferriols Perez, E.; de la Cruz Conty, M.L.; Aguilar, A.C.; Pardilla, M.B.E.; Rodríguez, P.P.; Hernando, M.M.; Acebal, L.F.; Recarte, P.P.; Mallen, M.d.M.; et al. Obstetric Outcomes of SARS-CoV-2 Infection in Asymptomatic Pregnant Women. Viruses 2021, 13, 112. [Google Scholar] [CrossRef]
- Farghaly, M.A.; Kupferman, F.; Castillo, F.; Kim, R.M. Characteristics of Newborns Born to SARS-CoV-2-Positive Mothers: A Retrospective Cohort Study. Am. J. Perinatol. 2020, 37, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Puneet, G.; Surender, K.; Sudhan, S.S. SARS-CoV-2 prevalence and maternal-perinatal outcomes among pregnant women admitted for delivery: Experience from COVID-19-dedicated maternity hospital in Jammu, Jammu and Kashmir (India). J. Med. Virol. 2021, 93, 5505–5514. [Google Scholar]
- Hcini, N.; Maamri, F.; Picone, O.; Carod, J.F.; Lambert, V.; Mathieu, M.; Carles, G.; Pomar, L. Maternal, fetal and neonatal outcomes of large series of SARS-CoV-2 positive pregnancies in peripartum period: A single-center prospective comparative study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 257, 11–18. [Google Scholar] [CrossRef]
- Katz, D.; Bateman, B.T.; Kjaer, K.; Turner, D.P.; Spence, N.Z.; Habib, A.S.; George, R.B.; Toledano, R.D.; Grant, G.; Madden, H.E.; et al. The Society for Obstetric Anesthesia and Perinatology Coronavirus Disease 2019 Registry: An Analysis of Outcomes Among Pregnant Women Delivering During the Initial Severe Acute Respiratory Syndrome Coronavirus-2 Outbreak in the United States. Anesth. Analg. 2021, 133, 462–473. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.Y.; DeSisto, C.L.; Simeone, R.M.; Ellington, S.; Galang, R.R.; Oduyebo, T.; Gilboa, S.M.; Lavery, A.M.; Gundlapalli, A.V.; Shapiro-Mendoza, C.K. Adverse Pregnancy Outcomes, Maternal Complications, and Severe Illness Among US Delivery Hospitalizations With and Without a Coronavirus Disease 2019 (COVID-19) Diagnosis. Clin. Infect. Dis. 2021, 73, S24–S31. [Google Scholar] [CrossRef]
- Liu, C.; Andrusier, M.; Silver, M.; Applewhite, L.; Clare, C.A. Effect of SARS-CoV-2 Infection on Pregnancy Outcomes in an Inner-City Black Patient Population. J. Community Health 2021, 46, 1029–1035. [Google Scholar] [CrossRef]
- Martinez-Perez, O.; Rodriguez, P.P.; Hernandez, M.M.; Pardilla, M.B.; Perez, N.P.; Hernandez, M.R.; Yarza, A.V.; Velasco, O.N.; Fernandez, P.G.; Acebal, L.F.; et al. The association between SARS-CoV-2 infection and preterm delivery: A prospective study with a multivariable analysis. BMC Pregnancy Childbirth 2021, 21, 273. [Google Scholar] [CrossRef] [PubMed]
- Nayak, A.H.; Kapote, D.S.; Fonseca, M.; Chavan, N.; Mayekar, R.; Sarmalkar, M.; Bawa, A. Impact of the Coronavirus Infection in Pregnancy: A Preliminary Study of 141 Patients. J. Obstet. Gynaecol. India 2020, 70, 256–261. [Google Scholar] [CrossRef]
- Norman, M.; Navér, L.; Söderling, J.; Ahlberg, M.; Askling, H.H.; Aronsson, B.; Byström, E.; Jonsson, J.; Sengpiel, V.; Ludvigsson, J.F.; et al. Association of Maternal SARS-CoV-2 Infection in Pregnancy With Neonatal Outcomes. JAMA 2021, 325, 2076–2086. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, M.; Cagino, K.; Matthews, K.C.; Friedlander, R.L.; Glynn, S.M.; Kubiak, J.M.; Yang, Y.J.; Zhao, Z.; Baergen, R.N.; DiPace, J.I.; et al. Pregnancy and postpartum outcomes in a universally tested population for SARS-CoV-2 in New York City: A prospective cohort study. BJOG 2020, 127, 1548–1556. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Silva, M.; Murillo-Zamora, E.; Mendoza-Cano, O.; Trujillo, X.; Huerta, M. COVID-19 mortality among pregnant women in Mexico: A retrospective cohort study. J. Glob. Health 2020, 10, 020512. [Google Scholar] [CrossRef] [PubMed]
- Steffen, H.A.; Swartz, S.R.; Jackson, J.B.; Kenne, K.A.; Ten Eyck, P.P.; Merryman, A.S.; Castaneda, C.N.; Marsden, K.; Maxwell, T.; Merrill, A.E.; et al. SARS-CoV-2 Infection during Pregnancy in a Rural Midwest All-delivery Cohort and Associated Maternal and Neonatal Outcomes. Am. J. Perinatol. 2021, 38, 614–621. [Google Scholar] [CrossRef]
- Trahan, M.-J.; Malhamé, I.; O’Farrell, P.; Mitric, C.; Desilets, J.; Bastrash, M.P.; El-Messidi, A.; Abenhaim, H.A. Obstetrical and Newborn Outcomes Among Patients With SARS-CoV-2 During Pregnancy. J. Obstet. Gynaecol. Can. 2021, 43, 888–892.e1. [Google Scholar] [CrossRef]
- Villar, J.; Ariff, S.; Gunier, R.B.; Thiruvengadam, R.; Rauch, S.; Kholin, A.; Roggero, P.; Prefumo, F.; do Vale, M.S.; Cardona-Perez, J.A.; et al. Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatr. 2021, 175, 817–826. [Google Scholar] [CrossRef]
- Vousden, N.; Bunch, K.; Morris, E.; Simpson, N.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J.; Knight, M. The incidence, characteristics and outcomes of pregnant women hospitalized with symptomatic and asymptomatic SARS-CoV-2 infection in the UK from March to September 2020: A national cohort study using the UK Obstetric Surveillance System (UKOSS). PLoS ONE 2021, 16, e0251123. [Google Scholar] [CrossRef]
- Allotey, J.; Stallings, E.; Bonet, M.; Yap, M.; Chatterjee, S.; Kew, T.; Debenham, L.; Llavall, A.C.; Dixit, A.; Zhou, D.; et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020, 370, m3320. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.Q.; Bilodeau-Bertrand, M.; Liu, S.; Auger, N. The impact of COVID-19 on pregnancy outcomes: A systematic review and meta-analysis. CMAJ 2021, 193, E540–E548. [Google Scholar] [CrossRef] [PubMed]









| Study | Country | Study Design | Study Population | Sample Size | Data Collection Period | |
|---|---|---|---|---|---|---|
| COVID-19 (+) Pregnant Women | COVID-19 (−) Pregnant Women | |||||
| Abedzadeh-Kalahroudi et al., 2021 [14] | Iran | Prospective cohort study | Single-center | 56 | 94 | March to November 2020 |
| Adhikari et al., 2020 [15] | USA | Prospective cohort study | Single-center | 252 | 3122 | 18 March to 22 August 2020 |
| Brandt et al., 2021 [16] | USA | Case–control study | Single-center | 61 | 122 | 11 March to 11 June 2020 |
| Cardona-Pe’rez et al., 2021 [17] | Mexico | Case–control study | Single-center | 70 | 170 | 22 April to 25 May 2020 |
| Crovetto et al., 2021 [18] | Spain | Prospective cohort study | Multicenter | 317 | 1908 | 15 March to 31 May 2020 |
| Cruz-Lemini et al., 2021 [19] | Spain | Prospective cohort study | Multicenter | 174 | 430 | 23 March to 31 May 2020 |
| Farghaly et al., 2020 [20] | USA | Retrospective cohort study | Single-center | 15 | 64 | March to May 2020 |
| Gupta et al., 2021 [21] | India | Retrospective cohort study | Single-center | 108 | 3057 | 1 September to 30 November 2020 |
| Hcini et al., 2021 [22] | France | Prospective cohort study | Single-center | 137 | 370 | 16 June to 16 August 2020 |
| Katz et al., 2021 [23] | USA | Case–control study | Multicenter | 490 | 964 | 19 March to 31 May 2020 |
| Ko et al., 2021 [24] | USA | Retrospective cohort study | Multicenter | 6550 | 482,921 | March to September 2020 |
| Liu et al., 2021 [25] | USA | Retrospective cohort study | Single-center | 56 | 279 | 10 April to 10 June 2020 |
| Martinez-Perez et al., 2021 [26] | Spain | Prospective cohort study | Multicenter | 246 | 763 | 23 March to 31 May 2020 |
| Nayak et al., 2020 [27] | India | Retrospective cohort study | Single-center | 141 | 836 | 1 April to 15 May 2020 |
| Norman et al., 2021 [28] | Sweden | Prospective cohort study | Nationwide | 2286 | 84,719 | 11 March 2020 to 8 March 2021. |
| Prabhu et al., 2020 [29] | USA | Prospective cohort study | Multicenter | 70 | 605 | 22 March to 20 April 2020 |
| Ríos-Silva et al., 2020 [30] | Mexico | Retrospective cohort study | Nationwide | 448 | 1216 | 28 February to 25 May 2020 |
| Steffen et al., 2021 [31] | USA | Prospective cohort study | Multicenter | 61 | 939 | 1 May to 22 September 2020 |
| Trahan et al., 2021 [32] | Canada | Cohort study | Multicenter | 45 | 225 | 22 March to 31 July 2020 |
| Villar et al., 2021 [33] | Argentina, Brazil, Egypt, France, Ghana, India, Indonesia, Italy, Japan, Mexico, Nigeria, North Macedonia, Pakistan, Russia, Spain, Switzerland, UK, US | Prospective cohort study | Multinational | 706 | 1424 | 2 March to October 2020 |
| Vousden et al., 2021 [34] | United Kingdom | Prospective cohort study | Nationwide | 1842 | 1148 | 1 March to 31 August 2020 |
| Study | Age (Years) a | Parity | Gestational Age at Delivery (Weeks) a |
|---|---|---|---|
| Abedzadeh-Kalahroudi et al., 2021 [14] | 31.6 (6.1) | Primiparous: 33.9% | 37.1 (3.1) |
| Adhikari et al., 2020 [15] | 27.0 (6.6) | Nulliparous: 29% | Range <34 wk to ≥40 wk |
| Brandt et al., 2021 [16] | 30.3 (6.4) | Median (IQR): 2 (1–3) | Mild symptomatic group: 39.0 ± 2.7; Severe symptomatic group: 34.0 ± 5.8 |
| Cardona-Pe’rez et al., 2021 [17] | Median: 26 Range: 13–45 | Median: 0; Range 0–3 | Median (IQR) 38.1 (36.3–39.3) |
| Crovetto et al., 2021 [18] | Median (IQR): 33.3 (29–37) | Nulliparous: 53% | 39.1 (2.1) |
| Cruz-Lemini et al., 2021 [19] | 32.6 | Nulliparous: 38% | 39.0 |
| Farghaly et al., 2020 [20] | Mean: 33.4 | NR | NR |
| Gupta et al., 2021 [21] | 24.7 (2.4) | Nulliparous: 41.6% | 36.6 (3.3) |
| Hcini et al., 2021 [22] | Median (IQR): 25 (21–31) | Median (IQR): 2 (1–5) | NR |
| Katz et al., 2021 [23] | 30.4 (6.2) | Parity 0: 37.5%; Parity 1: 28.3%; Parity 2+: 34.2% | 38.1 (2.6) |
| Ko et al., 2021 [24] | Median: 28.0 Range: 13–49 | NR | NR |
| Liu et al., 2021 [25] | 30.3 (6.4) | Median (IQR): 1 (0–2) | Median (IQR): 39 (38–40) |
| Martinez-Perez et al., 2021 [26] | 32.6 | Nulliparous: 38.5% | 38.6 |
| Nayak et al., 2020 [27] | Range: <20 to >30 | Primiparous: 39% | NR |
| Norman et al., 2021 [28] | 31.4 (5.0) | Nulliparous: 43.1% | 39.2 (2.1) |
| Prabhu et al., 2020 [29] | NR | NR | NR |
| Ríos-Silva et al., 2020 [30] | Median (IQR): 29 (25–33) | NR | NR |
| Steffen et al., 2021 [31] | Median (IQR): 28 (24–32) | NR | Median (IQR) 39 (37.1–39.6) |
| Trahan et al., 2021 [32] | Range: <25 to 35+ | Parity 0: 33%; Parity 1: 27%; Parity 2+: 40% | 38.9 (2.2) |
| Villar et al., 2021 [33] | 30.0 (6.1) | NR | 37.9 (3.3) |
| Vousden et al., 2021 [34] | Range: <20 to ≥35 | Primiparous: 41.2% | Median (IQR) 39 (38–40) |
| Study | The Outcome of the Study (Comparison of COVID 19 Infected and Non-Infected Pregnant Women) ‡ | |||
|---|---|---|---|---|
| Increased Risk/No Difference | Maternal Risk/s | Fetal Risk/s | Neonatal Risk/s | |
| Abedzadeh-Kalahroudi et al., 2021 [14] | Increased risk | Preeclampsia, cesarean section delivery | Fetal distress | Preterm birth, low Apgar score |
| Adhikari et al., 2020 [15] | No difference | |||
| Cardona-Pe’rez et al., 2021 [17] | Increased risk | Preeclampsia | ||
| Crovetto et al., 2021 [18] † | No difference | |||
| Cruz-Lemini et al., 2021 [19] †† | Increased risk | Pre-labor rupture of membranes | ||
| Farghaly et al., 2020 [20] | Increased risk | Cesarean section delivery | Low mean Apgar score at the fifth minute | |
| Gupta et al., 2021 [21] | Increased risk | Cesarean section delivery | Fetal distress | Preterm birth, low birth weight, low Apgar score |
| Hcini et al., 2021 [22] | Increased risk | Intra-uterine death | ||
| Katz et al., 2021 [23] | Increased risk | Preterm birth | ||
| Ko et al., 2021 [24] | Increased risk | Maternal death | Preterm birth | |
| Liu et al., 2021 [25] | No difference | |||
| Martinez-Perez et al., 2021 [26] | Increased risk | Pre-labor rupture of membranes | Preterm birth, neonatal intensive care unit admission | |
| Nayak et al., 2020 [27] | Increased risk | Cesarean section delivery | ||
| Norman et al., 2021 [28] | Increased risk | Neonatal intensive care unit admission | ||
| Prabhu et al., 2020 [29] | Increased risk | Cesarean section delivery | ||
| Ríos-Silva et al., 2020 [30] | No difference | |||
| Steffen et al., 2021 [31] | No difference | |||
| Trahan et al., 2021 [32] | No difference | |||
| Villar et al., 2021 [33] | Increased risk | Maternal death, preeclampsia | Preterm birth | |
| Vousden et al., 2021 [34] | Increased risk | Cesarean section delivery | Neonatal intensive care unit admission | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pathirathna, M.L.; Samarasekara, B.P.P.; Dasanayake, T.S.; Saravanakumar, P.; Weerasekara, I. Adverse Perinatal Outcomes in COVID-19 Infected Pregnant Women: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 203. https://doi.org/10.3390/healthcare10020203
Pathirathna ML, Samarasekara BPP, Dasanayake TS, Saravanakumar P, Weerasekara I. Adverse Perinatal Outcomes in COVID-19 Infected Pregnant Women: A Systematic Review and Meta-Analysis. Healthcare. 2022; 10(2):203. https://doi.org/10.3390/healthcare10020203
Chicago/Turabian StylePathirathna, Malshani L., Buddhini P. P. Samarasekara, Thakshila S. Dasanayake, Padmapriya Saravanakumar, and Ishanka Weerasekara. 2022. "Adverse Perinatal Outcomes in COVID-19 Infected Pregnant Women: A Systematic Review and Meta-Analysis" Healthcare 10, no. 2: 203. https://doi.org/10.3390/healthcare10020203
APA StylePathirathna, M. L., Samarasekara, B. P. P., Dasanayake, T. S., Saravanakumar, P., & Weerasekara, I. (2022). Adverse Perinatal Outcomes in COVID-19 Infected Pregnant Women: A Systematic Review and Meta-Analysis. Healthcare, 10(2), 203. https://doi.org/10.3390/healthcare10020203







