Overlap of Physical, Cognitive, and Social Frailty Affects Ikigai in Community-Dwelling Japanese Older Adults
Abstract
1. Introduction
2. Materials and Methods
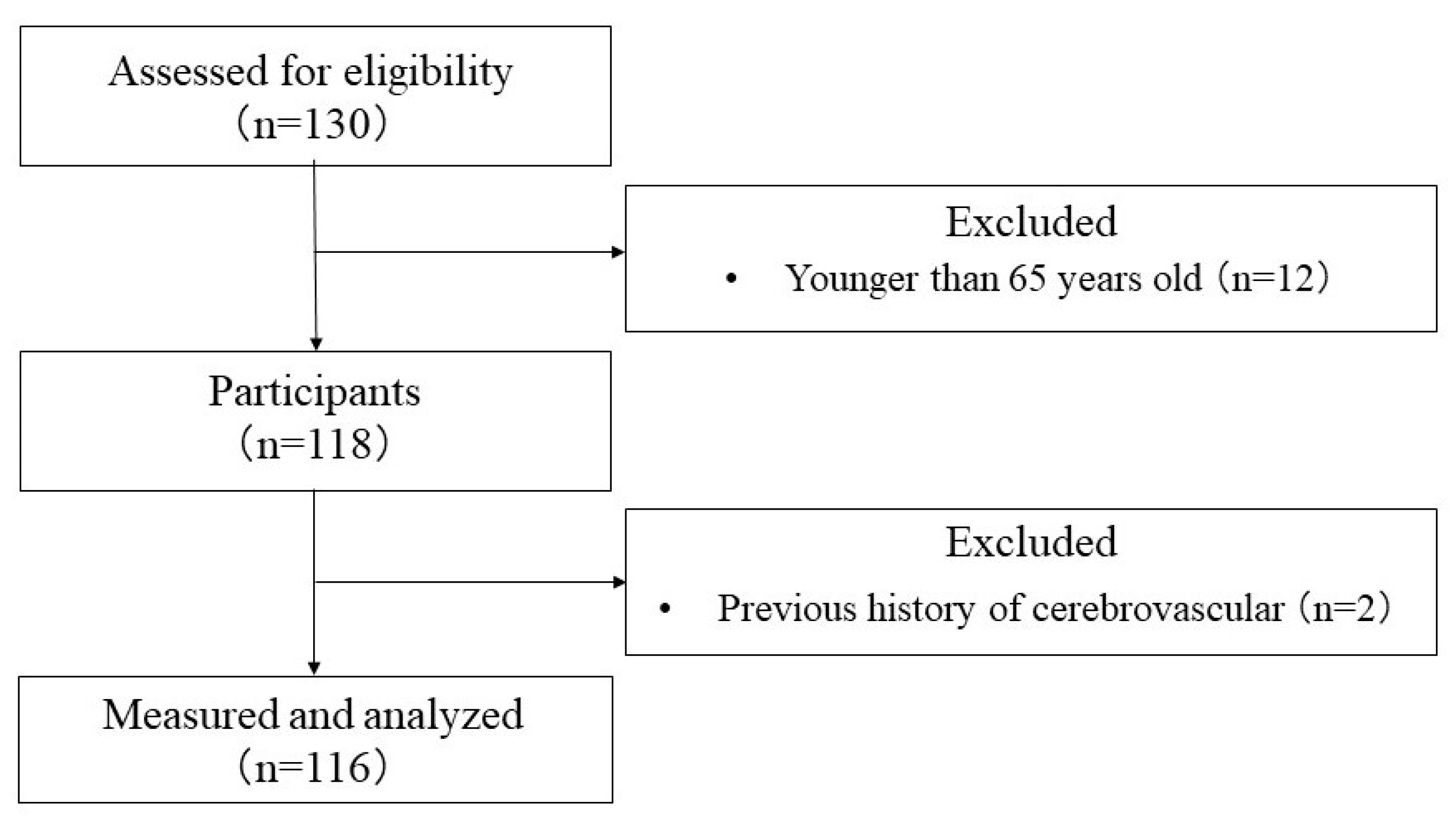
2.1. Study Design
2.2. Participants
- Persons infected or suspected of being infected with COVID-19.
- Those who had difficulty completing the questionnaire due to cognitive decline.
- Those who were certified as requiring nursing care insurance (nursing care insurance 1 or higher).
- Those who had a history of mental illness.
- Those who were undergoing orthopedic surgery or had limited mobility.
- Those who were ill and judged to be ineligible by the study physician to participate.
2.3. Sample Size Calculation
2.4. Outcomes
2.5. Data Analysis
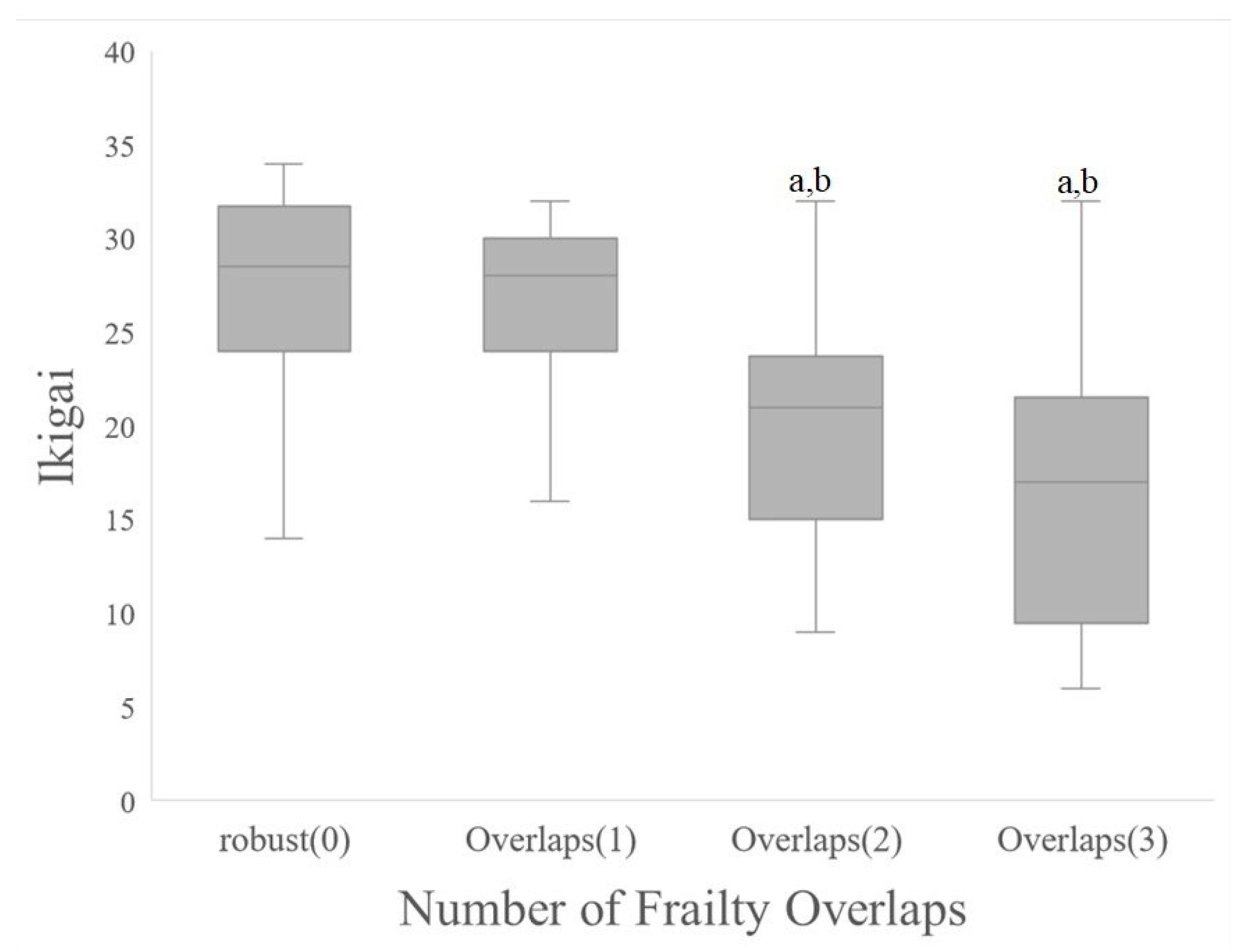
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, 146–156. [Google Scholar] [CrossRef]
- Whipple, M.O.; Hamel, A.V.; Talley, K.M.C. Fear of falling among community-dwelling older adults: A scoping review to identify effective evidence-based interventions. Geriatr. Nurs. 2018, 39, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Kojima, G.; Taniguchi, Y.; Iliffe, S.; Jivraj, S.; Walters, K. Transitions between frailty states among community-dwelling older people: A systematic review and meta-analysis. Ageing Res. Rev. 2019, 50, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.W.; Kahn, R.L. Human aging: Usual and successful. Science 1987, 237, 143–149. [Google Scholar] [CrossRef]
- Crumbaugh, J.C.; Maholic, L.T. An experimental study in existentialism: The psychometric approach to Frankl’s concept of noögenic neurosis. J. Clin. Psychol. 1964, 20, 200–207. [Google Scholar] [CrossRef]
- Lawton, M.P. The Philadelphia Geriatric Center Morale Scale: A revision. J. Gerontol. 1975, 30, 85–89. [Google Scholar] [CrossRef]
- Larson, R. Thirty years of research on the subjective well-being of older americans. J. Gerontol. 1978, 33, 109–125. [Google Scholar] [CrossRef]
- Okuzono, S.S.; Shiba, K.; Kim, E.S.; Shirai, K.; Kondo, N.; Fujiwara, T.; Kondo, K.; Lomas, T.; Trudel-Fitzgerald, C.; Kawachi, I.; et al. Ikigai and subsequent health and wellbeing among Japanese older adults: Longitudinal outcome-wide analysis. Lancet Reg. Health West Pac. 2022, 21, 100391. [Google Scholar] [CrossRef]
- Fukuzawa, A.; Katagiri, K.; Harada, K.; Masumoto, K.; Chogahara, M.; Kondo, N.; Okada, S. A Longitudinal Study of the Moderating Effects of Social Capital on the Relationships between Changes in Human Capital and Ikigai among Japanese Older Adults. Asian J. Soc. Psychol. 2019, 22, 172–182. [Google Scholar] [CrossRef]
- Roberson, D.; Davies, I.; Davidoff, J. Color categories are not universal: Replications and new evidence from a stone-age culture. J. Exp. Psychol. Gen. 2000, 129, 369–398. [Google Scholar] [CrossRef]
- Ziegelmann, J.P.; Lippke, S. Use of selection, optimization, and compensation strategies in health self-regulation: Interplay with resources and successful development. J. Aging Health 2007, 19, 500–518. [Google Scholar] [CrossRef] [PubMed]
- Tomioka, K.; Kurumatani, N.; Hosoi, H. Relationship of Having Hobbies and a Purpose in Life with Mortality, Activities of Daily Living, and Instrumental Activities of Daily Living Among Community-Dwelling Elderly Adults. J. Epidemiol. 2016, 26, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, R.; Hirano, M. Development of a Scale for Assessing the Meaning of Participation in Care Prevention Group Activities Provided by Local Governments in Japan. Int. J. Environ. Res. Public Health 2020, 17, 4499. [Google Scholar] [CrossRef]
- Kinoshita, S.; Hirooka, N.; Kusano, T.; Saito, K.; Nakamoto, H. Does Improvement in Health-Related Lifestyle Habits Increase Purpose in Life among a Health Literate Cohort? Int. J. Environ. Res. Public Health 2020, 17, 8878. [Google Scholar] [CrossRef]
- Satake, S.; Arai, H. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr. Gerontol. Int. 2020, 20, 992–993. [Google Scholar] [CrossRef]
- Solfrizzi, V.; Scafato, E.; Seripa, D.; Lozupone, M.; Imbimbo, B.P.; D’Amato, A.; Tortelli, R.; Schilardi, A.; Galluzzo, L.; Gandin, C.; et al. Reversible Cognitive Frailty, Dementia, and All-Cause Mortality. The Italian Longitudinal Study on Aging. J. Am. Med. Dir. Assoc. 2017, 18, 89.e1–89.e8. [Google Scholar] [CrossRef]
- Sugimoto, T.; Sakurai, T.; Ono, R.; Kimura, A.; Saji, N.; Niida, S.; Toba, K.; Chen, L.-K.; Arai, H. Epidemiological and clinical significance of cognitive frailty: A mini review. Ageing Res. Rev. 2018, 44, 1–7. [Google Scholar] [CrossRef]
- Shimada, H.; Makizako, H.; Lee, S.; Doi, T.; Tsutsumimoto, K.; Harada, K.; Hotta, R.; Bae, S.; Nakakubo, S.; Suzuki, T. Impact of Cognitive Frailty on Daily Activities in Older Persons. J. Nutr. Health Aging 2016, 20, 729–735. [Google Scholar] [CrossRef]
- Feng, L.; Zin Nyunt, M.S.; Gao, Q.; Feng, L.; Yap, K.B.; Ng, T.P. Cognitive Frailty and Adverse Health Outcomes: Findings from the Singapore Longitudinal Ageing Studies (SLAS). J. Am. Med. Dir. Assoc. 2017, 18, 252–258. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Tsutsumimoto, K.; Lee, S.; Doi, T.; Nakakubo, S.; Hotta, R.; Suzuki, T. Social Frailty in Community-Dwelling Older Adults as a Risk Factor for Disability. J. Am. Med. Dir. Assoc. 2015, 16, 1003.e7–1003.e11. [Google Scholar] [CrossRef]
- Seichi, A.; Hoshino, Y.; Doi, T.; Akai, M.; Tobimatsu, Y.; Iwaya, T. Development of a screening tool for risk of locomotive syndrome in the elderly: The 25-question Geriatric Locomotive Function Scale. J. Orthop. Sci. 2012, 17, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Bubela, D.J.; Magasi, S.R.; Wang, Y.C.; Gershon, R.C. Sit-to-stand test: Performance and determinants across the age-span. Isokinet. Exerc. Sci. 2010, 18, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed]
- Yoshimura, N.; Muraki, S.; Oka, H.; Tanaka, S.; Ogata, T.; Kawaguchi, H.; Akune, T.; Nakamura, K. Association between new indices in the locomotive syndrome risk test and decline in mobility: Third survey of the ROAD study. J. Orthop. Sci. 2015, 20, 896–905. [Google Scholar] [CrossRef]
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for assessing frailty status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Kondo, T.; Kamada, J. Construction of ‘the K-I Scale for the Feeling that Life is Worth Living among the Aged’ and the Definition of this Feeling. Jpn. Soc. Study Soc. Welf. 2003, 43, 93–101. [Google Scholar]
- Okura, M.; Ogita, M.; Arai, H. Self-Reported Cognitive Frailty Predicts Adverse Health Outcomes for Community-Dwelling Older Adults Based on an Analysis of Sex and Age. J. Nutr. Health Aging 2019, 23, 654–664. [Google Scholar] [CrossRef]
- Teo, N.; Gao, Q.; Nyunt, M.S.Z.; Wee, S.L.; Ng, T.P. Social Frailty and Functional Disability: Findings from the Singapore Longitudinal Ageing Studies. J. Am. Med. Dir. Assoc. 2017, 18, 637.e13–637.e19. [Google Scholar] [CrossRef]
- WHOQOL group. World Health Organization Quality of Life assessment (WHOQOL): Position paper from the world health organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]
- Shimozuma, K. History and Future Perspective of QOL Assessment Research. Jpn. J. Behav. Med. 2015, 21, 4–7. [Google Scholar]
- Gobbens, R.J.J.; van Assen, M.A.L.M. Associations between multidimensional frailty and quality of life among Dutch older people. Arch. Gerontol. Geriatr. 2017, 73, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Shin, S.H.; Scicolone, M.A.; Parmelee, P. Purpose in Life Protects Against Cognitive Decline among Older Adults. Am. J. Geriatr. Psychiatry 2019, 27, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Bell, G.; Singham, T.; Saunders, R.; John, A.; Stott, J. Positive psychological constructs and association with reduced risk of mild cognitive impairment and dementia in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2022, 77, 101594. [Google Scholar] [CrossRef] [PubMed]
- Hironaka, S.; Kugimiya, Y.; Watanabe, Y.; Motokawa, K.; Hirano, H.; Kawai, H.; Kera, T.; Kojima, M.; Fujiwara, Y.; Ihara, K.; et al. Association between oral, social, and physical frailty in community-dwelling older adults. Arch. Gerontol. Geriatr. 2020, 89, 104105. [Google Scholar] [CrossRef]
- Ament, B.H.L.; de Vugt, M.E.; Verhey, F.R.J.; Kempen, G.I.J.M. Are physically frail older persons more at risk of adverse outcomes if they also suffer from cognitive, social, and psychological frailty? Eur. J. Ageing 2014, 11, 213–219. [Google Scholar] [CrossRef] [PubMed]
| Age (years) | 75.1 ± 5.7 | |
| BMI (kg/m2) | 23.1 ± 3.1 | |
| 2-step value (2 strides/height) | 1.1 ± 0.2 | |
| Locomo5 (points) | 3.6 ± 3.6 | |
| Chair stand test (seconds) | 10.1 ± 3.8 | |
| TUG (seconds) | 6.8 ± 1.3 | |
| GDS (points) | 3.6 ± 3.1 | |
| Ikigai (points) | 22.1 ± 7.3 | |
| ADL (points) | 0.7 ± 1.1 | |
| Number of underlying diseases (persons) | None: 37, One: 58, Two: 17, Three: 2, Four: 2 | |
| Gender (persons) | Male: 23, Female: 93 | |
| Educational background (persons) | 6–9 years: 8, 10–13 years: 108 | |
| Financial comfort (persons) | Yes: 40, No: 76 | |
| Family (persons) | Living alone: 23, living together: 93 | |
| Work (persons) | Have done: 23, Have not done: 93 | |
| Married (persons) | Spouse: 74, Bereaved/separated: 38, Never married: 4 | |
| Exercise habits (persons) | Yes: 77, No: 39 | |
| Falls (persons) | Yes: 33, No: 83 | |
| Hospitalization (persons) | Yes: 22, No: 94 | |
| Physical Frailty (persons) | Robust: 43, Pre-frailty: 60, Frailty: 13 | |
| Cognitive Frailty (persons) | Robust: 77, Frailty: 39 | |
| Social frailty (persons) | Robust: 37, Pre-frail: 24, Frailty: 55 | |
| Physical Frailty (1) | ||||||
|---|---|---|---|---|---|---|
| Evaluation Item | a. Robust (n = 43) | b. Pre-Frailty (n = 60) | c. Frailty (n = 13) | p-Value | p (2) | Multiple Comparisons |
| Age | 73.0 (69.0–78.5) | 76.5 (72.0–80.0) | 77.0 (76.0–79.0) | 0.052 | ||
| BMI | 23.5 (21.8–25.0) | 22.5 (21.1–24.2) | 22.8 (20.4–23.9) | 0.412 | ||
| GDS | 2.0 (0.0–4.0) | 3.0 (2.0–7.0) | 5.0 (3.0–9.0) | 0.000 | *** | a < c, a < b |
| Number of underlying diseases | 1.0 (0.0–1.0) | 1.0 (0.0–1.0) | 1.0 (1.0–2.0) | 0.018 | * | a < c |
| 2-step value | 1.2 (1.1–1.3) | 1.1 (1.0–1.2) | 1.0 (0.9–1.1) | 0.000 | *** | a > c, a > b |
| Loco5 | 1.0 (0.0–3.0) | 3.5 (1.0–6.5) | 5.0 (3.0–6.0) | 0.000 | *** | a < b, a < c |
| 5-stance test | 8.7 (7.7–9.6) | 9.5 (8.0–12.5) | 9.5 (9.0–11.8) | 0.011 | * | a < b, a < c |
| TUG | 6.5 (5.9–7.3) | 6.6 (6.0–7.6) | 6.8 (6.5–8.2) | 0.284 | ||
| ADL | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 1.0 (0.0–2.0) | 0.042 | * | a < c |
| Self-actualization and motivation | 9.0 (7.5–12.0) | 8.0 (5.0–10.0) | 7.0 (2.0–8.0) | 0.002 | * | a > b, a > c |
| Life fulfillment | 9.0 (7.5–10.0) | 7.0 (4.0–8.5) | 7.0 (4.0–8.0) | 0.000 | *** | a > b, a > c |
| Willingness to live | 4.0 (3.0–4.0) | 3.0 (2.0–4.0) | 3.0 (2.0–4.0) | 0.008 | * | a > b |
| Sense of presence | 6.0 (5.0–6.0) | 4.0 (3.0–6.0) | 3.0 (0.0–5.0) | 0.000 | *** | a > b, a > c |
| Ikigai | 28.0 (23.0–31.0) | 19.0 (15.0–26.0) | 19.0 (10.0–23.0) | 0.000 | *** | a > b, a > c |
| Male n, % | 8, 18.6 | 11, 18.3 | 4, 30.8 | 0.578 | ||
| Have an exercise habit n, % | 34, 79.1 | 37, 61.7 | 6, 46.2 | 0.031 | * | |
| Have 10–13 years of education n, % | 42, 97.7 | 54, 90.0 | 12, 92.3 | 0.566 | ||
| Have a job n, % | 11, 25.6 | 12, 20.0 | 0, 0.0 | 0.064 | ||
| Financially well-off n, % | 17, 39.5 | 17, 28.3 | 6, 46.2 | 0.358 | ||
| Living alone n, % | 5, 11.6 | 15, 25.0 | 3, 23.1 | 0.245 | ||
| Married n, % | 33, 76.7 | 34, 56.7 | 7, 53.8 | 0.349 | ||
| Have had a fall n, % | 8, 18.6 | 18, 30.0 | 7, 53.8 | 0.034 | * | |
| Have been hospitalized n, % | 6, 14.0 | 14, 23.3 | 2, 15.4 | 0.406 | ||
| Cognitive Frailty (1) | |||||
|---|---|---|---|---|---|
| Evaluation Item | Robust (n = 77) | Frailty (n = 39) | p-Value | p (2) | |
| Age | 74.0 (70.0–78.0) | 76.0 (71.5–80.0) | 0.101 | ||
| BMI | 22.8 (21.4–25.1) | 23.3 (21.8–24.2) | 0.568 | ||
| GDS | 1.0 (0.0–3.0) | 6.0 (3.0–7.0) | 0.000 | *** | |
| Number of underlying diseases | 1.0 (0.0–1.0) | 1.0 (1.0–1.5) | 0.016 | * | |
| Falls Index | 2-step value | 1.1 (1.1–1.3) | 1.1 (1.0–1.2) | 0.105 | |
| Loco5 | 1.0 (0.0–4.0) | 4.0 (2.0–6.5) | 0.000 | *** | |
| 5-stance test | 8.8 (7.7–9.8) | 10.1 (8.5–12.5) | 0.003 | * | |
| TUG | 6.5 (6.0–7.6) | 6.6 (5.9–7.6) | 0.685 | ||
| ADL | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.544 | ||
| Ikigai Index | Self-actualization and motivation | 9.0 (7.0–11.0) | 7.0 (4.0–10.0) | 0.002 | * |
| Life fulfillment | 9.0 (7.0–10.0) | 6.0 (4.0–8.0) | 0.000 | *** | |
| Willingness to live | 4.0 (3.0–4.0) | 3.0 (2.0–4.0) | 0.000 | *** | |
| Sense of presence | 5.0 (4.0–6.0) | 4.0 (2.0–5.0) | 0.000 | *** | |
| Ikigai | 26.0 (20.0–30.0) | 19.0 (13.0–24.0) | 0.000 | *** | |
| Male n, % | 17, 22.1 | 6, 15.4 | 0.105 | ||
| Have an exercise habit n, % | 56, 72.7 | 21, 53.8 | 0.431 | ||
| Have 10–13 years of education n, % | 74, 96.1 | 34, 87.2 | 0.167 | ||
| Have a job n, % | 18, 23.4 | 5, 12.8 | 0.076 | ||
| Financially well-off n, % | 25, 32.5 | 15, 38.5 | 0.421 | ||
| Living alone n, % | 13, 16.9 | 10, 25.6 | 0.172 | ||
| Married n, % | 55, 71.4 | 19, 48.7 | 0.366 | ||
| Have had a fall n, % | 16, 20.8 | 17, 43.6 | 0.046 | * | |
| Have been hospitalized n, % | 15, 19.5 | 7, 17.9 | 0.342 | ||
| Social Frailty (1) | |||||||
|---|---|---|---|---|---|---|---|
| Evaluation Item | a. Robust (n = 37) | b. Pre-Frailty (n = 24) | c. Frailty (n = 55) | p-Value | p (2) | Multiple Comparisons | |
| Age | 74.0 (70.0–78.0) | 72.0 (69.5–77.0) | 78.0 (73.0–80.0) | 0.003 | * | a < c, b < c | |
| BMI | 23.6 (22.0–25.1) | 23.7 (21.8–24.3) | 22.4 (20.7–23.9) | 0.247 | |||
| GDS | 1.5 (0.0–3.0) | 2.0 (0.5–4.5) | 4.0 (2.0–7.5) | 0.000 | *** | a < c, b < c | |
| Number of underlying diseases | 1.0 (0.0–1.0) | 1.0 (0.0–1.0) | 1.0 (1.0–2.0) | 0.004 | * | a < c, b < c | |
| Falls Index | 2-step value | 1.2 (1.1–1.3) | 1.1 (1.1–1.2) | 1.1 (0.9–1.2) | 0.007 | * | a > c |
| Loco5 | 1.0 (0.0–2.0) | 2.0 (0.0–4.0) | 5.0 (2.0–8.0) | 0.000 | *** | a < c, b < c | |
| 5-stance test | 8.6 (7.6–9.6) | 8.9 (7.9–9.5) | 10.7 (8.3–13.3) | 0.000 | *** | a < c, b < c | |
| TUG | 6.5 (6.0–6.8) | 6.6 (5.7–8.1) | 6.6 (6.1–7.6) | 0.377 | |||
| ADL | 0.0 (0.0–0.0) | 0.0 (0.0–1.0) | 1.0 (0.0–2.0) | 0.001 | * | a < c | |
| Ikigai Index | Self-actualization and motivation | 9.0 (7.0–11.0) | 10.0 (7.0–12.0) | 7.0 (4.0–9.5) | 0.001 | * | a > c, b > c |
| Life fulfillment | 9.0 (7.0–10.0) | 8.5 (7.0–10.0) | 6.0 (4.0–8.0) | 0.000 | *** | a > c, b > c | |
| Willingness to live | 4.0 (3.0–4.0) | 4.0 (3.0–4.0) | 2.0 (2.0–4.0) | 0.000 | * | a > c, b > c | |
| Sense of presence | 6.0 (5.0–6.0) | 6.0 (4.5–6.0) | 3.0 (2.0–5.0) | 0.000 | *** | a > c, b > c | |
| Ikigai | 28.0 (23.0–30.0) | 26.0 (22.5–30.5) | 18.0 (13.0–23.0) | 0.000 | *** | a > c, b > c | |
| Male n, % | 9, 24.3 | 1, 4.2 | 13, 23.6 | 0.178 | |||
| Have an exercise habit n, % | 31, 83.8 | 13, 54.2 | 33, 60.0 | 0.029 | * | ||
| Have 10–13 years of education n, % | 35, 94.6 | 24, 100.0 | 49, 89.1 | 0.416 | |||
| Have a job n, % | 12, 32.4 | 2, 8.3 | 9, 16.4 | 0.035 | * | ||
| Financially well-off n, % | 17, 45.9 | 10, 41.7 | 13, 23.6 | 0.095 | |||
| Living alone n, % | 2, 5.4 | 0, 0.0 | 21, 38.2 | 0.000 | *** | ||
| Married n, % | 28, 75.7 | 20, 83.3 | 26, 47.3 | 0.006 | * | ||
| Have had a fall n, % | 8, 21.6 | 6, 25.0 | 19, 34.5 | 0.344 | |||
| Have been hospitalized n, % | 8, 21.6 | 4, 16.7 | 10, 18.2 | 0.814 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsujishita, S.; Nagamatsu, M.; Sanada, K. Overlap of Physical, Cognitive, and Social Frailty Affects Ikigai in Community-Dwelling Japanese Older Adults. Healthcare 2022, 10, 2216. https://doi.org/10.3390/healthcare10112216
Tsujishita S, Nagamatsu M, Sanada K. Overlap of Physical, Cognitive, and Social Frailty Affects Ikigai in Community-Dwelling Japanese Older Adults. Healthcare. 2022; 10(11):2216. https://doi.org/10.3390/healthcare10112216
Chicago/Turabian StyleTsujishita, Soma, Masaki Nagamatsu, and Kiyoshi Sanada. 2022. "Overlap of Physical, Cognitive, and Social Frailty Affects Ikigai in Community-Dwelling Japanese Older Adults" Healthcare 10, no. 11: 2216. https://doi.org/10.3390/healthcare10112216
APA StyleTsujishita, S., Nagamatsu, M., & Sanada, K. (2022). Overlap of Physical, Cognitive, and Social Frailty Affects Ikigai in Community-Dwelling Japanese Older Adults. Healthcare, 10(11), 2216. https://doi.org/10.3390/healthcare10112216






