Strategies to Engage Adolescents in Digital Health Interventions for Obesity Prevention and Management
Abstract
:1. Introduction
2. Adolescents’ and Their Digital World
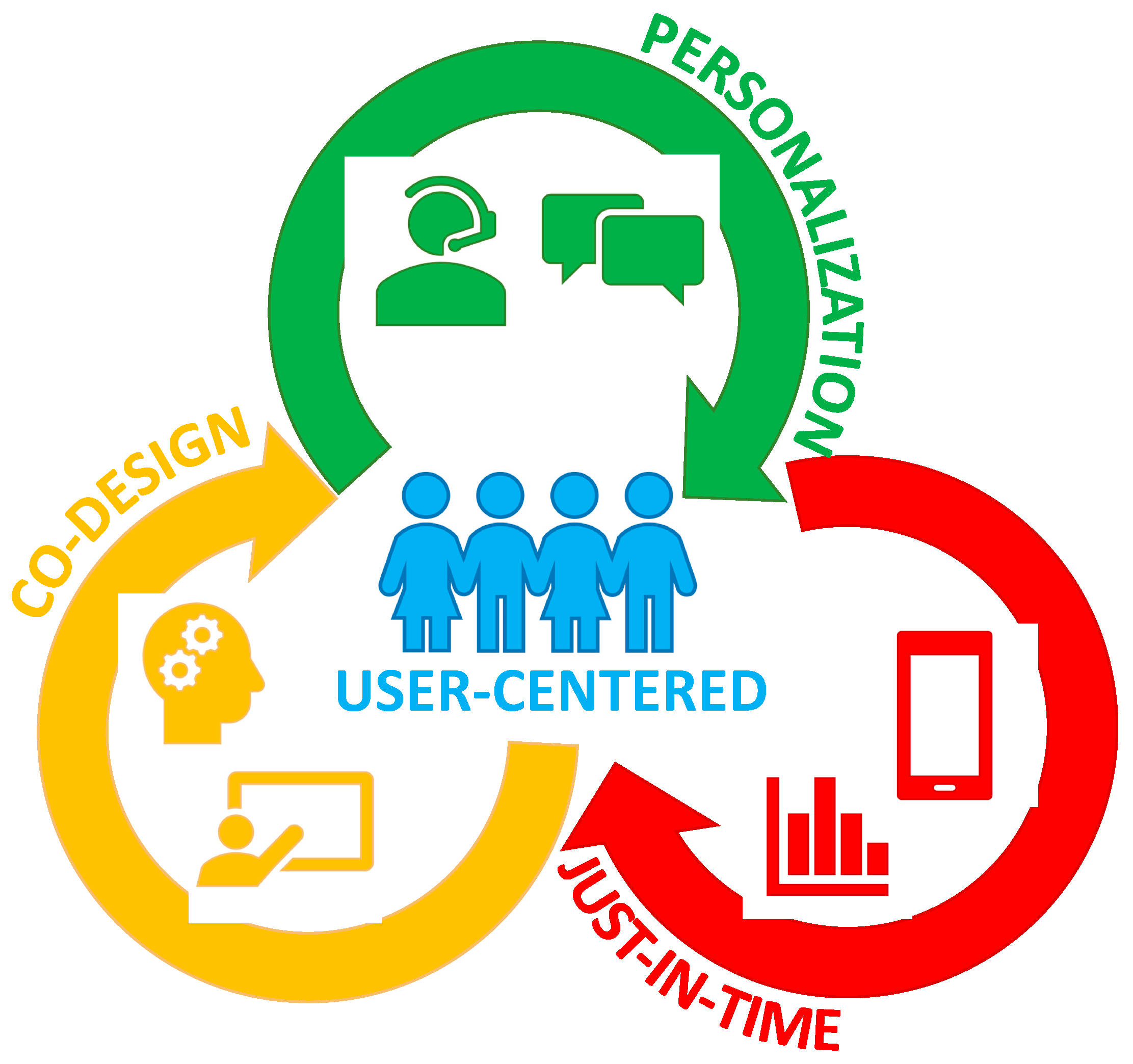
3. Three Strategies for Effective Engagement with Digital Intervention
3.1. Co-Design
3.2. Personalization
3.3. Just-in-Time-Adaptation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Health for the World’s Adolescents: A Second Chance in the Second Decade. Available online: http://apps.who.int/adolescent/second-decade/ (accessed on 12 December 2017).
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Attard, S.M.; Herring, A.H.; Howard, A.G.; Gordon-Larsen, P. Longitudinal trajectories of BMI and cardiovascular disease risk: The national longitudinal study of adolescent health. Obesity 2013, 21, 2180–2188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doak, C.M.; Visscher, T.L.; Renders, C.M.; Seidell, J.C. The prevention of overweight and obesity in children and adolescents: A review of interventions and programmes. Obes. Rev. 2006, 7, 111–136. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.F.; Leitzmann, M.F.; Ballard-Barbash, R.; Albanes, D.; Harris, T.B.; Hollenbeck, A.; Kipnis, V. Body mass and weight change in adults in relation to mortality risk. Am. J. Epidemiol. 2014, 179, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Manson, J.E.; Yuan, C.; Liang, M.H.; Grodstein, F.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Associations of weight gain from early to middle adulthood with major health outcomes later in life. JAMA 2017, 318, 255–269. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; Adair, L.S.; Nelson, M.C.; Popkin, B.M. Five-year obesity incidence in the transition period between adolescence and adulthood: The national longitudinal study of adolescent health. Am. J. Clin. Nutr. 2004, 80, 569–575. [Google Scholar] [PubMed]
- Patton, G.C.; Coffey, C.; Sawyer, S.M.; Viner, R.M.; Haller, D.M.; Bose, K.; Vos, T.; Ferguson, J.; Mathers, C.D. Global patterns of mortality in young people: A systematic analysis of population health data. Lancet 2009, 374, 881–892. [Google Scholar] [CrossRef]
- UNFPA. The Power of 1.8 Billion—Adolescents, Youth, and the Transformation of the Future; The United Nations Population Fund: New York, NY, USA, 2014. [Google Scholar]
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 4324.0.55.002—Microdata: Australian Health Survey: Nutrition and Physical Activity. Available online: http://bit.ly/2jkRRZO (accessed on 1 April 2017).
- Hardy, L.L.; Mihrshahi, S.; Drayton, B.A.; Bauman, A. NSW Schools Physical Activity and Nutrition Survey (SPANS) 2015: Full Report; NSW Department of Health: Sydney, Australia, 2016.
- Powell, L.M.; Szczypka, G.; Chaloupka, F.J. Trends in exposure to television food advertisements among children and adolescents in the united states. Arch. Pediatr. Adolesc. Med. 2010, 164, 794–802. [Google Scholar] [CrossRef] [PubMed]
- Pearson, N.; Braithwaite, R.E.; Biddle, S.J.H.; van Sluijs, E.M.F.; Atkin, A.J. Associations between sedentary behaviour and physical activity in children and adolescents: A meta-analysis. Obes. Rev. 2014, 15, 666–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandevijvere, S.; Chow, C.C.; Hall, K.D.; Umali, E.; Swinburn, B.A. Increased food energy supply as a major driver of the obesity epidemic: A global analysis. Bull. World Health Organ. 2015, 93, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O. Can a small-changes approach help address the obesity epidemic? A report of the joint task force of the American society for nutrition, institute of food technologists, and international food information council. Am. J. Clin. Nutr. 2009, 89, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Seagle, H.M.; Strain, G.W.; Makris, A.; Reeves, R.S. Position of the American Dietetic Association: Weight management. J. Am. Diet. Assoc. 2009, 109, 330–346. [Google Scholar] [PubMed]
- National Health and Medical Research Council. Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia; National Health and Medical Research Council: Melbourne, Australia, 2013.
- Müller, A.M.; Maher, C.A.; Vandelanotte, C.; Hingle, M.; Middelweerd, A.; Lopez, M.L.; DeSmet, A.; Short, C.E.; Nathan, N.; Hutchesson, M.J.; et al. Physical activity, sedentary behavior, and diet-related eHealth and mHealth Research: Bibliometric analysis. J. Med. Int. Res. 2018, 20. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Yardley, L.; West, R.; Patrick, K.; Greaves, F. Developing and evaluating digital interventions to promote behavior change in health and health care: Recommendations resulting from an international workshop. J. Med. Int. Res. 2017, 19, e232. [Google Scholar] [CrossRef] [PubMed]
- Redfern, J.; Santo, K.; Coorey, G.; Thakkar, J.; Hackett, M.; Thiagalingam, A.; Chow, C.K. Factors influencing engagement, perceived usefulness and behavioral mechanisms associated with a text message support program. PLoS ONE 2016, 11, e0163929. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Redfern, J.; Hillis, G.S.; Thakkar, J.; Santo, K.; Hackett, M.L.; Jan, S.; Graves, N.; de Keizer, L.; Barry, T.; et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: A randomized clinical trial. JAMA 2015, 314, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Lenhart, A.; Duggan, M.; Perrin, A.; Stepler, R.; Rainie, H.; Parker, K. Teens, Social Media & Technology Overview. Available online: http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/# (accessed on 6 December 2017).
- Rose, T.; Barker, M.; Maria Jacob, C.; Morrison, L.; Lawrence, W.; Strommer, S.; Vogel, C.; Woods-Townsend, K.; Farrell, D.; Inskip, H.; et al. A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J. Adolesc. Health 2017. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.; Damarell, R.; Bell, L.; Moores, C.; Miller, J. Community-Based Approaches to Adolescent Obesity; Sax Institute: Ultimo, Australia, 2017. [Google Scholar]
- Keating, S.R.; McCurry, M.K. Systematic review of text messaging as an intervention for adolescent obesity. J. Am. Assoc. Nurse Pract. 2015, 27, 714–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinbeck, K.S.; Lister, N.B.; Gow, M.L.; Baur, L.A. Treatment of adolescent obesity. Nat. Rev. Endocrinol. 2018, 14, 331–344. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Piao, M.; Byun, A.; Kim, J. A systematic review and meta-analysis of intervention for pediatric obesity using mobile technology. Stud. Health Technol. Inf. 2016, 225, 491–494. [Google Scholar]
- Chaplais, E.; Naughton, G.; Thivel, D.; Courteix, D.; Greene, D. Smartphone interventions for weight treatment and behavioral change in pediatric obesity: A systematic review. Telemed. J. E Health 2015, 21, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Wickham, C.A.; Carbone, E.T. Who’s calling for weight loss? A systematic review of mobile phone weight loss programs for adolescents. Nutr. Rev. 2015, 73, 386–398. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.A.; Sainsbury, A. Strategies to improve adherence to dietary weight loss interventions in research and real-world settings. Behav. Sci. 2017, 7. [Google Scholar] [CrossRef]
- Ahmed, S.P.; Bittencourt-Hewitt, A.; Sebastian, C.L. Neurocognitive bases of emotion regulation development in adolescence. Dev. Cogn. Neurosci. 2015, 15, 11–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peper, J.S.; Dahl, R.E. Surging hormones: Brain-Behavior interactions during puberty. Curr. Dir. Psychol. Sci. 2013, 22, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Patton, G.C.; Viner, R. Pubertal transitions in health. Lancet 2007, 369, 1130–1139. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef]
- National Health Medical Research Council (NHMRC). Australian Dietary Guidelines; NHMRC: Canberra, Australia, 2013.
- National Health and Medical Research Council. Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes; Commonwealth of Australia: Canberra, Australia, 2006.
- Skelton, J.A.; Beech, B.M. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, e273–e281. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; Straker, L.M.; McManus, A.; Fenner, A.A. Barriers and enablers for participation in healthy lifestyle programs by adolescents who are overweight: A qualitative study of the opinions of adolescents, their parents and community stakeholders. BMC Pediatr. 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Chater, A.; Lorencatto, F. Effective behaviour change techniques in the prevention and management of childhood obesity. Int. J. Obes. 2013, 37, 1287–1294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puhl, R.M.; Himmelstein, M.S. Adolescent preferences for weight terminology used by health care providers. Pediatr. Obes. 2018. [Google Scholar] [CrossRef] [PubMed]
- Roy Morgan Research. Media Release: 9 in 10 Aussie Teens Now Have a Mobile. Available online: http://bit.ly/2bbuoAX (accessed on 20 September 2017).
- Chen, J.L.; Wilkosz, M.E. Efficacy of technology-based interventions for obesity prevention in adolescents: A systematic review. Adolesc. Health Med. Ther. 2014, 5, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Turner-McGrievy, G.M.; Beets, M.W.; Moore, J.B.; Kaczynski, A.T.; Barr-Anderson, D.J.; Tate, D.F. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J. Am. Med. Inf. Assoc. 2013, 20, 513–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brannon, E.E.; Cushing, C.C. A systematic review: Is there an app for that? Translational science of pediatric behavior change for physical activity and dietary interventions. J. Pediatr. Psychol. 2015, 40, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Perski, O.; Blandford, A.; West, R.; Michie, S. Conceptualising engagement with digital behaviour change interventions: A systematic review using principles from critical interpretive synthesis. Transl. Behav. Med. 2017, 7, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and promoting effective engagement with digital behavior change interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Redfern, J.; Thiagalingam, A.; Jan, S.; Whittaker, R.; Hackett, M.L.; Mooney, J.; De Keizer, L.; Hillis, G.S.; Chow, C.K. Development of a set of mobile phone text messages designed for prevention of recurrent cardiovascular events. Eur. J. Prev. Cardiol. 2014, 21, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Cargo, M.; Mercer, S.L. The value and challenges of participatory research: Strengthening its practice. Ann. Rev. Public Health 2008, 29, 325–350. [Google Scholar] [CrossRef] [PubMed]
- Andersson, N. Community-led trials: Intervention co-design in a cluster randomised controlled trial. BMC Public Health 2017, 17, 397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagen, P.; Collin, P.; Metcalf, A.; Nicholas, M.; Rahilly, K. Participatory Design of Evidence-Based Online Youth Mental Health Promotion, Prevention, Early Intervention and Treatment; Young and Well cooperative Research Centre: Melbourne, Australia, 2012. [Google Scholar]
- Rivera, J.; McPherson, A.; Hamilton, J.; Birken, C.; Coons, M.; Iyer, S.; Agarwal, A.; Lalloo, C.; Stinson, J. Mobile apps for weight management: A scoping review. JMIR mHealth uHealth 2016, 4, e87. [Google Scholar] [CrossRef] [PubMed]
- Schoffman, D.E.; Turner-McGrievy, G.; Jones, S.J.; Wilcox, S. Mobile apps for pediatric obesity prevention and treatment, healthy eating, and physical activity promotion: Just fun and games? Transl. Behav. Med. 2013, 3, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Webb, M.J.; Wadley, G.; Sanci, L.A. Improving patient-centered care for young people in general practice with a codesigned screening app: Mixed methods study. JMIR mHealth uHealth 2017, 5, e118. [Google Scholar] [CrossRef] [PubMed]
- Hetrick, S.E.; Robinson, J.; Burge, E.; Blandon, R.; Mobilio, B.; Rice, S.M.; Simmons, M.B.; Alvarez-Jimenez, M.; Goodrich, S.; Davey, C.G. Youth codesign of a mobile phone APP to facilitate self-monitoring and management of mood symptoms in young people with major depression, suicidal ideation, and self-harm. JMIR Ment. Health 2018, 5, e9. [Google Scholar] [CrossRef] [PubMed]
- Rivera, J.; McPherson, A.C.; Hamilton, J.; Birken, C.; Coons, M.; Peters, M.; Iyer, S.; George, T.; Nguyen, C.; Stinson, J. User-centered design of a mobile APP for weight and health management in adolescents with complex health needs: Qualitative study. JMIR Form. Res. 2018, 2, e7. [Google Scholar] [CrossRef]
- Standoli, C.; Guarneri, M.; Perego, P.; Mazzola, M.; Mazzola, A.; Andreoni, G. A smart wearable sensor system for counter-fighting overweight in teenagers. Sensors 2016, 16, 1220. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cade, J.E.; Allman-Farinelli, M. The most popular smartphone Apps for weight loss: A quality assessment. JMIR mHealth uHealth 2015, 3, e104. [Google Scholar] [CrossRef] [PubMed]
- Adamson, A.J.; Mathers, J.C. Effecting dietary change. Proc. Nutr. Soc. 2004, 63, 537–547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eyles, H.C.; Mhurchu, C.N. Does tailoring make a difference? A systematic review of the long-term effectiveness of tailored nutrition education for adults. Nutr. Rev. 2009, 67, 464–480. [Google Scholar] [CrossRef] [PubMed]
- De Roos, B.; Brennan, L. Personalised interventions-a precision approach for the next generation of dietary intervention studies. Nutrients 2017, 9. [Google Scholar] [CrossRef] [PubMed]
- Steinbeck, K.; Baur, L.; Cowell, C.; Pietrobelli, A. Clinical research in adolescents: Challenges and opportunities using obesity as a model. Int. J. Obes. 2008, 33, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.; Shrewsbury, V.A.; O’Connor, J.; Steinbeck, K.S.; Hill, A.J.; Shah, S.; Kohn, M.R.; Torvaldsen, S.; Baur, L.A. Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: The Loozit randomized controlled trial. Int. J. Obes. 2013, 37, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Armanasco, A.A.; Miller, Y.D.; Fjeldsoe, B.S.; Marshall, A.L. Preventive health behavior change text message interventions: A meta-analysis. Am. J. Prev. Med. 2017, 52, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Woolford, S.J.; Barr, K.L.; Derry, H.A.; Jepson, C.M.; Clark, S.J.; Strecher, V.J.; Resnicow, K. OMG do not say LOL: Obese adolescents’ perspectives on the content of text messages to enhance weight loss efforts. Obesity 2011, 19, 2382–2387. [Google Scholar] [CrossRef] [PubMed]
- Woolford, S.J.; Clark, S.J.; Strecher, V.J.; Resnicow, K. Tailored mobile phone text messages as an adjunct to obesity treatment for adolescents. J. Telemed. Telecare 2010, 16, 458–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allman-Farinelli, M.; Partridge, S.R.; McGeechan, K.; Balestracci, K.; Hebden, L.; Wong, A.; Phongsavan, P.; Denney-Wilson, E.; Harris, M.F.; Bauman, A. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): Nine-Month outcomes of a randomized controlled trial. JMIR mHealth uHealth 2016, 4, e78. [Google Scholar] [CrossRef] [PubMed]
- Partridge, S.R.; McGeechan, K.; Hebden, L.; Balestracci, K.; Wong, A.T.; Denney-Wilson, E.; Harris, M.F.; Phongsavan, P.; Bauman, A.; Allman-Farinelli, M. Effectiveness of a mHealth lifestyle program with telephone support (TXT2BFiT) to prevent unhealthy weight gain in young adults: Randomized controlled trial. JMIR mHealth uHealth 2015, 3, e66. [Google Scholar] [CrossRef] [PubMed]
- Partridge, S.R.; Allman-Farinelli, M.; McGeechan, K.; Balestracci, K.; Wong, A.T.; Hebden, L.; Harris, M.F.; Bauman, A.; Phongsavan, P. Process evaluation of TXT2BFiT: A multi-component mHealth randomised controlled trial to prevent weight gain in young adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Santo, K.; Hyun, K.; de Keizer, L.; Thiagalingam, A.; Hillis, G.S.; Chalmers, J.; Redfern, J.; Chow, C.K. The effects of a lifestyle-focused text-messaging intervention on adherence to dietary guideline recommendations in patients with coronary heart disease: An analysis of the TEXT ME study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 45. [Google Scholar] [CrossRef] [PubMed]
- Nahum-Shani, I.; Smith, S.N.; Spring, B.J.; Collins, L.M.; Witkiewitz, K.; Tewari, A.; Murphy, S.A. Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Ann. Behav. Med. 2018, 52, 446–462. [Google Scholar] [CrossRef] [PubMed]
- Spruijt-Metz, D.; Wen, C.K.; O’Reilly, G.; Li, M.; Lee, S.; Emken, B.A.; Mitra, U.; Annavaram, M.; Ragusa, G.; Narayanan, S. Innovations in the use of interactive technology to support weight management. Curr. Obes. Rep. 2015, 4, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Schembre, S.M.; Liao, Y.; Robertson, M.C.; Dunton, G.F.; Kerr, J.; Haffey, M.E.; Burnett, T.; Basen-Engquist, K.; Hicklen, R.S. Just-in-Time feedback in diet and physical activity interventions: Systematic review and practical design framework. J. Med. Int. Res. 2018, 20, e106. [Google Scholar] [CrossRef] [PubMed]
- Turner, T.; Spruijt-Metz, D.; Wen, C.K.; Hingle, M.D. Prevention and treatment of pediatric obesity using mobile and wireless technologies: A systematic review. Pediatr. Obes. 2015, 10, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Emken, B.A.; Li, M.; Thatte, G.; Lee, S.; Annavaram, M.; Mitra, U.; Narayanan, S.; Spruijt-Metz, D. Recognition of physical activities in overweight Hispanic youth using KNOWME Networks. J. Phys. Act. Health 2012, 9, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Garcia, C.; Hardeman, R.R.; Kwon, G.; Lando-King, E.; Zhang, L.; Genis, T.; Brady, S.S.; Kinder, E. Teenagers and texting: Use of a youth ecological momentary assessment system in trajectory health research with latina adolescents. JMIR mHealth uHealth 2014, 2, e3. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Partridge, S.R.; Redfern, J. Strategies to Engage Adolescents in Digital Health Interventions for Obesity Prevention and Management. Healthcare 2018, 6, 70. https://doi.org/10.3390/healthcare6030070
Partridge SR, Redfern J. Strategies to Engage Adolescents in Digital Health Interventions for Obesity Prevention and Management. Healthcare. 2018; 6(3):70. https://doi.org/10.3390/healthcare6030070
Chicago/Turabian StylePartridge, Stephanie R., and Julie Redfern. 2018. "Strategies to Engage Adolescents in Digital Health Interventions for Obesity Prevention and Management" Healthcare 6, no. 3: 70. https://doi.org/10.3390/healthcare6030070
APA StylePartridge, S. R., & Redfern, J. (2018). Strategies to Engage Adolescents in Digital Health Interventions for Obesity Prevention and Management. Healthcare, 6(3), 70. https://doi.org/10.3390/healthcare6030070




