The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic
Abstract
:1. Introduction
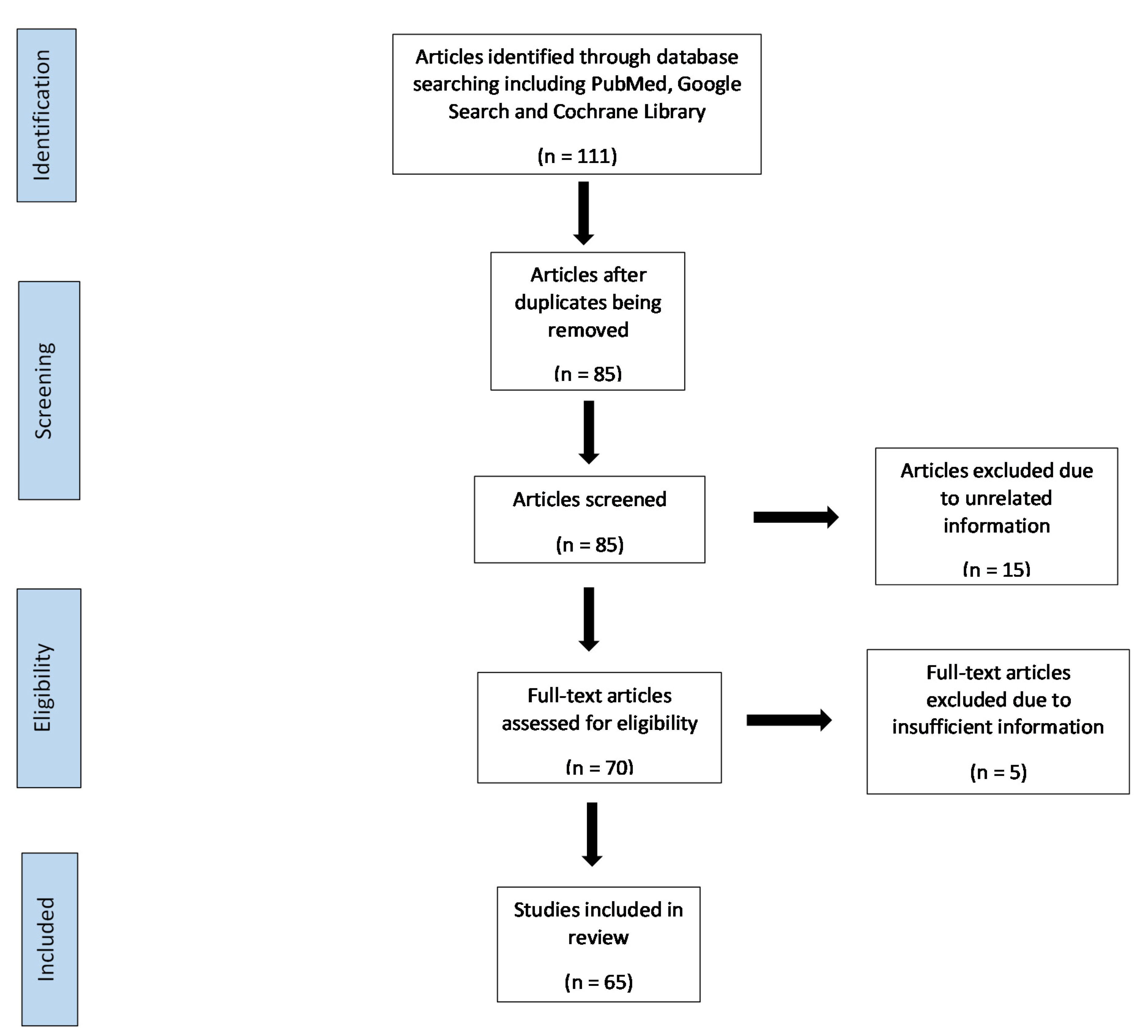
2. Method
2.1. Study Design
2.2. Literature Search Strategies
2.3. Study Eligibility Criteria–Inclusion and Exclusion Criteria
3. Results
3.1. Telehealth, COVID-19 and Breast Cancer Screening
3.2. Telehealth, COVID-19 and Breast Cancer Surgery
3.3. Teleoncology, COVID-19 and Breast Cancer
3.4. Telerehabilitation, COVID-19 and Breast Cancer
3.5. Telehealth, COVID-19, Breast Cancer and Mental Health Issues
3.6. Telehealth, COVID-19, Breast Cancer and Physical Exercise
3.7. Implementation and Satisfaction with Telehealth/Telemedicine
4. Discussion
5. Conclusions
6. Future Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth: Global Observatory for eHealth Series, Volume 2. 2010. Available online: http://apps.who.int/iris/bitstream/handle/10665/44497/9789241564144_eng.pdf;jsessionid=739641AF82AA4B3B5E5365C4889CF777?sequence=1 (accessed on 30 June 2021).
- Mahoney, M.F. Telehealth, telemedicine, and related technologic platforms: Current practice and response to the COVID-19 pandemic. J. Wound Ostomy Cont. Nurs. 2020, 47, 439–444. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Ambulatory Care Nursing; Anglea, T.; Murray, C.; Mastal, C.M.; Clelland, S. Scope and Standards of Practice for Professional Telehealth Nursing, 6th ed.; Pitman, N.J., Ed.; American Academy of Ambulatory Care Nursing: Sewell, NJ, USA, 2018. [Google Scholar]
- Allely, E.B. Synchronous and asynchronous telemedicine. J. Med. Syst. 1995, 19, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Vimalananda, V.G.; Gupte, G.; Seraj, S.M.; Orlander, J.; Berlowitz, D.; Fincke, B.G.; Simon, S.R.G. Electronic consultations (e-consults) to improve access to specialty care: A systematic review and narrative synthesis. J. Telemed. Telecare 2015, 21, 323–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palen, T.E.; Price, D.; Shetterly, S.; Wallace, K.B. Comparing virtual consults to traditional consults using an electronic health record: An observational case-control study. BMC Med. Inform. Decis. Mak. 2012, 12, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnston, S.; MacDougall, M.; McKinstry, B. The use of video consulting in general practice: Semi-structured interviews examining acceptability to patients. J. Innov. Health Inform. 2016, 23, 493–500. [Google Scholar]
- Orlando, J.F.; Beard, M.; Kumar, S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS ONE 2019, 14, e0221848. Available online: https://pubmed.ncbi.nlm.nih.gov/31469865/externalicon (accessed on 12 October 2021).
- Marzorati, C.; Renzi, C.; Russell-Edu, S.W.; Pravettoni, G. Telemedicine use among caregivers of cancer patients: Systematic review. J. Med. Internet Res. 2018, 20, e223. [Google Scholar] [CrossRef]
- Martinez, K.A.; Rood, M.; Jhangiani, N.; Kou, L.; Rose, S.; Boissy, A.; Rothberg, M.B. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. J. Gen. Internal Med. 2018, 33, 1768–1773. [Google Scholar] [CrossRef] [Green Version]
- Cox, A.; Lucas, G.; Marcu, A.; Piano, M.; Grosvenor, W.; Mold, F.; Maguire, R.; Ream, E. Cancer survivors’ experience with telehealth: A systematic review and thematic synthesis. J. Med. Internet Res. 2017, 19, e11. [Google Scholar] [CrossRef] [Green Version]
- Imaging Technology News. Telehealth to Experience Massive Growth due to COVID-19. Imaging Technology News. Park Ridge, NJ, USA, 2020. Available online: https://www.itnonline.com/content/telehealth-experience-massive-growth-due-covid-19 (accessed on 30 June 2021).
- Nouri, S.; Khoong, E.; Lyles, C.R.; Karliner, L. Addressing Equity in Telemedicine for Chronic Disease Management during the Covid-19 Pandemic. NEJM Catalyst. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123 (accessed on 30 June 2021).
- Gadzinski, A.J.; Andino, J.J.; Odisho, A.Y.; Watts, K.L.; Gore, J.L.; Ellimoottil, C. Telemedicine and eConsults for hospitalized patients during COVID-19. Urology 2020, 141, 12–14. [Google Scholar] [CrossRef]
- Chauhan, V.; Galwankar, S.; Arquilla, B.; Garg, M.; Di Somma, S.; El-Menyar, A.; Krishnan, V.; Gerber, J.; Holland, R.; Stawicki, S.P. Novel coronavirus (COVID-19): Leveraging telemedicine to optimize care while minimizing exposures and viral transmission. J. Emergencies Trauma Shock 2020, 13, 20. [Google Scholar] [CrossRef]
- Gao, Y.; Liu, R.; Zhou, Q.; Wang, X.; Huang, L.; Shi, Q.; Wang, Z.; Lu, S.; Li, W.; Ma, Y.; et al. Application of telemedicine during the coronavirus disease epidemics: A rapid review and meta-analysis. Ann. Transl. Med. 2020, 8, 626. [Google Scholar] [CrossRef] [PubMed]
- Barney, A.; Buckelew, S.; Mesheriakova, V.; Raymond-Flesch, M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: Challenges and opportunities for innovation. J. Adolesc. Health 2020, 67, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Gomez, T.; Anaya, Y.B.; Shih, K.J.; Tarn, D.M. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J. Am. Board Fam. Med. 2021, 34, S61–S70. [Google Scholar] [CrossRef]
- Hasani, S.A.; Ghafri, T.A.; Al Lawati, H.; Mohammed, J.; Al Mukhainai, A.; Al Ajmi, F.; Anwar, H. The use of telephone consultation in primary health care during COVID-19 Pandemic, Oman: Perceptions from physicians. J. Prim. Care Community Health 2020, 11, 2150132720976480. [Google Scholar] [CrossRef]
- Morgenstern-Kaplan, D.; Rocha-Haro, A.; Canales-Albarrán, S.J.; Núñez-García, E.; León-Mayorga, Y. An App-Based telemedicine program for primary care and specialist video consultations during the COVID-19 pandemic in Mexico. Telemed. J. e-Health 2021. [Google Scholar] [CrossRef]
- Garg, A.; Goyal, S.; Thati, R.; Thati, N. Implementation of telemedicine in a tertiary hospital-based ambulatory practice in Detroit during the COVID-19 pandemic: Observational study. JMIR Public Health Surveill. 2021, 7, e21327. [Google Scholar] [CrossRef]
- Drerup, B.; Espenschied, J.; Wiedemer, J.; Hamilton, L. Reduced no-show rates and sustained patient satisfaction of Telehealth during the COVID-19 pandemic. Telemed. J. e-Health 2021. [Google Scholar] [CrossRef]
- Imlach, F.; McKinlay, E.; Middleton, L.; Kennedy, J.; Pledger, M.; Russell, L.; Churchward, M.; Cumming, J.; McBride-Henry, K. Telehealth consultations in general practice during a pandemic lockdown: Survey and interviews on patient experiences and preferences. BMC Fam. Pract. 2020, 21, 269. [Google Scholar] [CrossRef]
- Catanese, S.; Pentheroudakis, G.; Douillard, J.Y.; Lordick, F. ESMO management and treatment adapted recommendations in the COVID-19 era: Pancreatic cancer. ESMO Open 2020, 5, e000804. [Google Scholar] [CrossRef]
- Paterson, C.; Bacon, R.; Dwyer, R.; Morrison, K.S.; Toohey, K.; O’Dea, A.; Slade, J.; Mortazavi, R.; Roberts, C.; Pranavan, G.; et al. The Role of telehealth during the COVID-19 pandemic across the interdisciplinary cancer team: Implications for practice. Semin. Oncol. Nurs. 2020, 36, 151090. [Google Scholar] [CrossRef]
- Morrison, K.S.; Paterson, C.; Toohey, K. The feasibility of exercise interventions delivered via telehealth for people affected by cancer: A rapid review of the literature. Semin. Oncol. Nurs. 2020, 36, 151092. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, S.; Lopez, G.; Powers-James, C.; Fellman, B.M.; Chunduru, A.; Li, Y.; Bruera, E.; Cohen, L. Integrative oncology consultations delivered via telehealth in 2020 and in-person in 2019: Paradigm shift during the COVID-19 world pandemic. Integr. Cancer Ther. 2021, 20, 1534735421999101. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, A.I.; Begley, M.; Delaney, T. Accelerating the delivery of cancer care at home during the Covid-19 pandemic. NEJM Catal. 2020. [Google Scholar] [CrossRef]
- Steindal, S.A.; Nes, A.A.G.; Godskesen, T.E. Patients’ experiences of telehealth in palliative home care: Scoping review. J. Med. Internet Res. 2020, 22, e16218. [Google Scholar] [CrossRef]
- Nelson, H.D.; Pappas, M.; Cantor, A.; Griffin, J.; Daeges, M.; Humphrey, L. Harms of breast cancer screening: Systematic review to update the 2009 U.S. Preventive Services Task Force Recommendation. Ann. Intern. Med. 2016, 164, 256–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seely, J.M.; Scaranelo, A.M.; Yong-Hing, C.; Appavoo, S.; Flegg, C.; Kulkarni, S.; Kornecki, A.; Wadden, N.; Loisel, Y.; Schofield, S.; et al. COVID-19: Safe guidelines for breast imaging during the pandemic. Can. Assoc. Radiol. J. 2020, 71, 459–469. [Google Scholar] [CrossRef]
- Salem, C.; Hajj, M.A.; Kourié, H.; Haddad, A.; Khaddage, A.; Ayoub, E.N.; Jabbour, K.; Moubarak, M.; Atallah, D. Radiology management of a ‘breast unit’ during COVID-19 pandemic: A single institution experience. Future Oncol. 2020, 16, 2917–2922. [Google Scholar] [CrossRef]
- Yin, K.; Singh, P.; Drohan, B.; Hughes, K.S. Breast imaging, breast surgery, and cancer genetics in the age of COVID-19. Cancer 2020, 126, 4466–4472. [Google Scholar] [CrossRef]
- Naidich, J.J.; Boltyenkov, A.; Wang, J.J. Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J. Am. Coll. Radiol. 2020, 17, 865–872. [Google Scholar] [CrossRef]
- Norbash, A.M.; Moore, A.V., Jr.; Recht, M.P. Early-stage radiology volume effects and considerations with the coronavirus disease 2019 (COVID-19) pandemic: Adaptations, risks, and lessons learned. J. Am. Coll. Radiol. 2020, 17, 1086–1095. [Google Scholar] [CrossRef] [PubMed]
- Smetherman, D.H. Breast cancer screening and the COVID-19 pandemic. J. Breast Imaging 2021, 3, 3–11. [Google Scholar] [CrossRef]
- Peng, S.M.; Yang, K.C.; Chan, W.P.; Wang, Y.W.; Lin, L.J.; Yen, A.M.; Smith, R.A.; Chen, T.H. Impact of the COVID-19 pandemic on a population-based breast cancer screening program. Cancer 2020, 126, 5202–5205. [Google Scholar] [CrossRef] [PubMed]
- Yong, J.H.; Mainprize, J.G.; Yaffe, M.J. The impact of episodic screening interruption: COVID-19 and population-based cancer screening in Canada. J. Med. Screen 2020. [Google Scholar] [CrossRef]
- Sharp, O.; Masud, D. Breast reconstruction with immediate autologous free tissue transfer in a peri-operative COVID-19 positive patient: A case report illustrating feasibility of aftercare. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 644–710. [Google Scholar] [CrossRef] [PubMed]
- Toss, A.; Isca, C.; Venturelli, M.; Nasso, C.; Ficarra, G.; Bellelli, V.; Armocida, C.; Barbieri, E.; Cortesi, L.; Moscetti, L.; et al. Two-month stop in mammographic screening significantly impacts on breast cancer stage at diagnosis and upfront treatment in the COVID era. ESMO Open 2021, 6, 100055. [Google Scholar] [CrossRef]
- Sonagli, M.; Cagnacci Neto, R.; Leite, F.P.M.; Makdissi, F.B.A. The use of telemedicine to retain intain breast cancer follow-up and surveillance during the COVID-19 pandemic. J. Surg. Oncol. 2021, 123, 371–374. [Google Scholar] [CrossRef]
- Johnston, K.; Smith, D.; Preston, R.; Evans, R.; Carlisle, K.; Lengren, J.; Naess, H.; Phillips, E.; Shephard, G.; Lydiard, L.; et al. From the technology came the idea: Safe implementation and operation of a high quality tele-radiology model increasing access to timely breast cancer assessment services for women in rural Australia. BMC Health Serv. Res. 2020, 20, 1103. [Google Scholar] [CrossRef]
- Greenwald, Z.R.; El-Zein, M.; Bouten, S.; Ensha, H.; Vazquez, F.L.; Franco, E.L. Mobile Screening Units for the Early Detection of Cancer: A Systematic Review. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1679–1694. [Google Scholar] [CrossRef] [Green Version]
- Marino, M.M.; Rienzo, M.; Serra, N.; Marino, N.; Ricciotti, R.; Mazzariello, L.; Leonetti, C.A.; Ceraldi, M.P.; Casamassimi, A.; Capocelli, F.; et al. Mobile screening units for the early detection of breast cancer and cardiovascular disease: A pilot telemedicine study in Southern Italy. Telemed. J. e-Health 2020, 26, 286–293. [Google Scholar] [CrossRef]
- Chung, H.L.; Parikh, J.R. Telemammography: Technical advances improve patient access in breast care. J. Breast Imaging 2020, 2, 152–156. [Google Scholar] [CrossRef]
- Lopez, F.W.; de Paredes, E.S.; Strickland, W.J., Jr.; Grizzard, W.S., Jr.; Zedler, P.A.; Roberts, K.M.; Stout, K.K. Telemammography: Interfacing between primary physicians and experts. Appl. Radiol. 2007, 36, 26–30. Available online: https://appliedradiology.com/articles/telemammography-interfacing-between-primary-physicians-and-experts (accessed on 30 June 2021).
- Leader, J.K.; Hakim, C.M.; Ganott, M.A.; Chough, D.M.; Wallace, L.P.; Clearfield, R.J.; Perrin, R.L.; Drescher, J.M.; Maitz, G.S.; Sumkin, J.H.; et al. A multisite tele-mammography system for remote management of screening mammography: An assessment of technical, operational, and clinical issues. J. Digit. Imaging 2006, 19, 216–225. [Google Scholar] [CrossRef] [Green Version]
- Syed, L.; Jabeen, S.; Manimala, S. Telemammography: A novel approach for early detection of breast cancer through wavelets based image processing and machine learning techniques. In Advances in Soft Computing and Machine Learning in Image Processing; Hassanien, A., Oliva, D., Eds.; Studies in Computational Intelligence; Springer: Cham, Switzerland, 2018; pp. 149–173. [Google Scholar]
- Ho, P.J.; Cook, A.R.; Binte Mohamed Ri, N.K.; Liu, J.; Li, J.; Hartman, M. Impact of delayed treatment in women diagnosed with breast cancer: A population-based study. Cancer Med. 2020, 9, 2435–2444. [Google Scholar] [CrossRef]
- Bleicher, R.J.; Ruth, K.; Sigurdson, E.R.; Beck, J.R.; Ross, E.; Wong, Y.N.; Patel, S.A.; Boraas, M.; Chang, E.I.; Topham, N.S.; et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. 2016, 2, 330–339. [Google Scholar] [CrossRef]
- Polverini, A.C.; Nelson, R.A.; Marcinkowski, E.; Jones, V.C.; Lai, L.; Mortimer, J.E.; Taylor, L.; Vito, C.; Yim, J.; Kruper, L. Time to treatment: Measuring quality breast cancer care. Ann. Surg. Oncol. 2016, 23, 3392–3402. [Google Scholar] [CrossRef]
- Eriksson, L.; Bergh, J.; Humphreys, K.; Wärnberg, F.; Törnberg, S.; Czene, K. Time from breast cancer diagnosis to therapeutic surgery and breast cancer prognosis: A population-based cohort study. Int. J. Cancer 2018, 143, 1093–1104. [Google Scholar] [CrossRef] [PubMed]
- Cadili, L.; DeGirolamo, K.; McKevitt, E.; Brown, C.J.; Prabhakar, C.; Pao, J.; Dingee, C.; Bazzarelli, A.; Warburton, R. COVID-19 and breast cancer at a Regional Breast Centre: Our flexible approach during the pandemic. Breast Cancer Res. Treat. 2021, 186, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Fregatti, P.; Gipponi, M.; Giacchino, M.; Sparavigna, M.; Murelli, F.; Toni, M.L.; Calabrò, M.T.; Orsino, L.; Friedman, D. Breast cancer surgery during the COVID-19 pandemic: An observational clinical study of the breast surgery clinic at Ospedale Policlinico San Martino-Genoa, Italy. In Vivo 2020, 34, 1667–1673. [Google Scholar] [CrossRef] [PubMed]
- Brenes Sánchez, J.M.; Picado, A.L.; Olivares Crespo, M.E.; García Sáenz, J.Á.; De La Plata Merlo, R.M.; De La Muela, M.H. Breast cancer management during COVID-19 pandemic in Madrid: Surgical strategy. Clin. Breast Cancer 2021, 21, e128–e135. [Google Scholar] [CrossRef] [PubMed]
- Noble, N.; Mackenzie, L.; Carey, M.; Proietto, A.; Sanson-Fisher, R.; Walker, G.; Silcock, J. Cross-sectional survey to inform the development of a telehealth support model: A feasibility study for women undergoing breast cancer surgery. Pilot Feasibility Stud. 2019, 5, 46. [Google Scholar] [CrossRef]
- Lai, L.L.; Player, H.; Hite, S.; Satyananda, V.; Stacey, J.; Sun, V.; Jones, V.; Hayter, J. Feasibility of remote occupational therapy services via telemedicine in a breast cancer recovery program. Am. J. Occup. Ther. 2021, 75, 7502205030p1–7502205030p9. [Google Scholar] [CrossRef] [PubMed]
- Pelle, F.; Cappelli, S.; Graziano, F.; Piarulli, L.; Cavicchi, F.; Magagnano, D.; De Luca, A.; De Vita, R.; Pozzi, M.; Costantini, M.; et al. Breast cancer surgery during the Covid-19 pandemic: A monocentre experience from the Regina Elena National Cancer Institute of Rome. J. Exp. Clin. Cancer Res. 2020, 39, 171. [Google Scholar] [CrossRef]
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: An International Collaborative Group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef] [Green Version]
- Colakoglu, S.; Johnson, A.; Mureau, M.A.; Douglass, S.; Kaoutzanis, C.; Chong, T.W.; Mathes, D.W.; Cohen, J.B. Telehealth: Could it be an avenue to microvascular breast reconstruction for patients with geographical barriers? J. Reconstr. Microsurg. 2021, 37, 597–601. [Google Scholar]
- Hazin, R.; Qaddoumi, I. Teleoncology: Current and future applications for improving cancer care globally. Lancet Oncol. 2010, 11, 204–210. [Google Scholar] [CrossRef] [Green Version]
- Sirintrapun, S.J.; Lopez, A.M. Telemedicine in cancer care. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 540–545. [Google Scholar] [CrossRef]
- Sabesan, S.; Kelly, J. Are teleoncology models merely about avoiding long distance travel for patients? Eur. J. Cancer Care 2014, 23, 745–749. [Google Scholar] [CrossRef]
- Sabesan, S. Medical models of tele-oncology: Current status and future directions. Asia Pac. J. Clin. Oncol. 2014, 10, 200–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sabesan, S.; Simcox, K.; Marr, I. Medical oncology clinics through videoconferencing: An acceptable telehealth model for rural patients and health workers. Intern. Med. J. 2012, 42, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Onesti, C.E.; Rugo, H.S.; Generali, D.; Peeters, M.; Zaman, K.; Wildiers, H.; Harbeck, N.; Martin, M.; Cristofanilli, M.; Cortes, J.; et al. Oncological care organization during COVID-19 outbreak. ESMO Open 2020, 5, e000853. [Google Scholar] [CrossRef]
- Orazem, M.; Oblak, I.; Spanic, T.; Ratosa, I. Telemedicine in radiation oncology post-COVID-19 pandemic: There is no turning back. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, 411–415. [Google Scholar] [CrossRef]
- Yildiz, F.; Oksuzoglu, B. Tele-oncology or telemedicine for oncology patients during the COVID-19 pandemic: The new normal for breast cancer survivors? Future Oncol. 2020, 16, 2191–2195. [Google Scholar] [CrossRef] [PubMed]
- Vecchione, L.; Stintzing, S.; Pentheroudakis, G.; Douillard, J.Y.; Lordick, F. ESMO management and treatment adapted recommendations in the COVID-19 era: Colorectal cancer. ESMO Open 2020, e000826. [Google Scholar] [CrossRef] [PubMed]
- American Society for Radiation Oncology. COVID-19′s Impact on Radiation Oncology. Initial Results of a Nationwide Physician Survey. Available online: https://www.astro.org/ASTRO/media/ASTRO/News%20and%20Publications/PDFs/ASTROCOVID19Survey1-ExecSummary.pdf (accessed on 30 June 2021).
- Khairat, S.; Meng, C.; Xu, Y.; Edson, B.; Gianforcaro, R. Interpreting COVID-19 and virtual care trends: Cohort study. J. Med. Internet Res. Public Health Surveill. 2020, 6, e18811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tashkandi, E.; Zeeneldin, A.; AlAbdulwahab, A.; Elemam, O.; Elsamany, S.; Jastaniah, W.; Abdullah, S.; Alfayez, M.; Jazieh, A.R.; Al-Shamsi, H.O. Virtual management of patients with cancer during the COVID-19 pandemic: Web-Based questionnaire study. J. Med. Internet Res. 2020, 22, e19691. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.J.; Liang, W.T.; Liu, Q.; He, R.; Chen, Q.C.; Li, Q.F.; Zhang, Y.; Du, X.D.; Pan, Y.; Liu, S.; et al. Use of a remote oncology pharmacy service platform for patients with cancer during the COVID-19 pandemic: Implementation and user acceptance evaluation. J. Med. Internet Res. 2021, 23, e24619. [Google Scholar] [CrossRef] [PubMed]
- Berlin, A.; Lovas, M.; Truong, T.; Melwani, S.; Liu, J.; Zhihui, A.L.; Badzynski, A.; Carpenter, M.B.; Virtanen, C.; Morley, L.; et al. Implementation and outcomes of virtual care across a tertiary cancer center during COVID-19. JAMA Oncol. 2021, 7, 597–602. [Google Scholar] [CrossRef]
- Loree, J.M.; Dau, H.; Rebić, N.; Howren, A.; Gastonguay, L.; McTaggart-Cowan, H.; Gill, S.; Raghav, K.; De Vera, M.A. Virtual oncology appointments during the initial wave of the COVID-19 pandemic: An international survey of patient perspectives. Curr. Oncol. 2021, 28, 671–677. [Google Scholar] [CrossRef]
- Zimmerman, B.S.; Seidman, D.; Berger, N.; Cascetta, K.P.; Nezolosky, M.; Trlica, K.; Ryncarz, A.; Keeton, C.; Moshier, E.; Tiersten, A. Patient perception of telehealth services for breast and gynecologic oncology care during the COVID-19 pandemic: A single center survey-based study. J. Breast Cancer 2020, 23, 542–552. [Google Scholar] [CrossRef]
- Hasson, S.P.; Waissengrin, B.; Shachar, E.; Hodruj, M.; Fayngor, R.; Brezis, M.; Nikolaevski-Berlin, A.; Pelles, S.; Safra, T.; Geva, R.; et al. Rapid implementation of telemedicine during the COVID-19 pandemic: Perspectives and preferences of patients with cancer. Oncologist 2021, 26, e679–e685. [Google Scholar] [CrossRef]
- Bizot, A.; Heudel, P.E.; Karimi, M.; Levy, C.; Vanlemmens, L.; Uzan, C.; Deluche, E.; Genet, D.; Saghatchian, M.; Giacchetti, S.; et al. 1710P International multicentric evaluation of breast cancer patients’ satisfaction and experience with oncology telemedicine visits (TV) during the COVID-19 outbreak. Ann. Oncol. 2020, 31, S1006. [Google Scholar] [CrossRef]
- Miller, C.; Kaltman, R.D.; Leon, A.; Gesteira, A.; Duffy, S.; Burgess, P.B. Telemedicine usability for cancer care during the COVID-19 pandemic. J. Clin. Oncol. 2020, 38, 265. [Google Scholar] [CrossRef]
- Brennan, D.M.; Mawson, S.; Brownsell, S. Tele-rehabilitation: Enabling the remote delivery of healthcare, rehabilitation, and self-management. Stud. Health Technol. Inform. 2009, 145, 231–248. [Google Scholar] [PubMed]
- McCue, M.; Fairman, A.; Pramuka, M. Enhancing quality of life through tele-rehabilitation. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Malliaras, P.; Cridland, K.; Hopmans, R.; Ashton, S.; Littlewood, C.; Page, R.; Harris, I.; Skouteris, H.; Haines, T. Internet and tele-rehabilitation-delivered management of rotator cuff-related shoulder pain (INTEL Trial): Randomized controlled pilot and feasibility trial. JMIR mHealth uHealth 2020, 8, e24311. [Google Scholar] [CrossRef]
- Malik, A.A.; Kiran, T. Psychological problems in breast cancer patients: A Review. Chemotherapy 2013, 2, 115. [Google Scholar] [CrossRef] [Green Version]
- Falcicchio, C.; Di Lallo, D.; Fabi, A.; Bonucci, A.; Perrone, M.; Pace, A.; Corti, A.; Giacomelli, L.; Pugliese, P. Use of rehabilitation pathways in women with breast cancer in the first 12 months of the disease: A retrospective study. BMC Cancer 2021, 21, 311. [Google Scholar] [CrossRef]
- Dávid, L.; Sebastian Rutkowski, M. Breast cancer rehabilitation. Klin. Onkol. 2021, 34, 14–19. [Google Scholar]
- Kilgour, R.D.; Jones, D.H.; Keyserlingk, J.R. Effectiveness of a self-administered, home-based exercise rehabilitation program for women following a modified radical mastectomy and axillary node dissection: A preliminary study. Breast Cancer Res. Treat. 2008, 109, 285–295. [Google Scholar] [CrossRef]
- Galiano-Castillo, N.; Cantarero-Villanueva, I.; Fernández-Lao, C.; Ariza-García, A.; Díaz-Rodríguez, L.; Del-Moral-Ávila, R.; Arroyo-Morales, M. Telehealth system: A randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer 2016, 122, 3166–3174. [Google Scholar] [CrossRef]
- Cheville, A.L.; Moynihan, T.; Herrin, J.; Loprinzi, C.; Kroenke, K. Effect of collaborative telerehabilitation on functional impairment and pain among patients with advanced-stage cancer: A randomized clinical trial. JAMA Oncol. 2019, 5, 644–652. [Google Scholar] [CrossRef]
- Helm, E.E.; Kempski, K.A.; Galantino, M.L.A. Effect of disrupted rehabilitation services on distress and quality of life in breast cancer survivors during the COVID-19 pandemic. Rehabil. Oncol. 2020, 38, 153–158. [Google Scholar] [CrossRef]
- de Rezende, L.F.; Francisco, V.E.; Franco, R.L. Tele-rehabilitation for patients with breast cancer through the COVID-19 pandemic. Breast Cancer Res. Treat. 2021, 185, 257–259. [Google Scholar] [CrossRef] [PubMed]
- Mella-Abarca, W.; Barraza-Sánchez, V.; Ramírez-Parada, K. Tele-rehabilitation for people with breast cancer through the COVID-19 pandemic in Chile. Ecancermedicalscience 2020, 14, 1085. [Google Scholar] [CrossRef]
- Tavoli, A.; Mohagheghi, M.A.; Moztazeri, A.; Roshan, R.; Tavoli, Z.; Omidvari, S. Anxiety and depression in patients with gastrointestinal cancer: Does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007, 7, 28. [Google Scholar] [CrossRef] [Green Version]
- Kissane, D.W.; Clarke, D.M.; Ikin, J.; Bloch, S.; Smith, G.C.; Vitetta, L.; McKenzie, D.P. Psychological morbidity and quality of life in Australian women with early-stage breast cancer: A cross-sectional survey. Med. J. Aust. 1998, 169, 192–196. [Google Scholar] [CrossRef]
- Moyer, A. Psychosocial outcomes of breast-conserving surgery versus mastectomy: A meta-analytic review. Health Psychol. 1997, 16, 284–293. [Google Scholar] [CrossRef]
- Gallagher, J.; Parle, M.; Cairns, D. Appraisal and psychological distress six months after diagnosis of breast cancer. Br. J. Health Psychol. 2002, 7, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Mendes-Santos, C.; Weiderpass, E.; Santana, R.; Andersson, G. A guided internet-delivered individually-tailored ACT-influenced cognitive behavioral intervention to improve psychosocial outcomes in breast cancer survivors (iNNOVBC): Study protocol. Internet Interv. 2019, 17, 100236. [Google Scholar] [CrossRef] [PubMed]
- Abrahams, H.J.G.; Gielissen, M.F.M.; Donders, R.R.; Goedendorp, M.M.; van der Wouw, A.J.; Verhagen, C.A.H.H.V.M.; Knoop, H. The efficacy of Internet-based cognitive behavioral therapy for severely fatigued survivors of breast cancer compared with care as usual: A randomized controlled trial. Cancer 2017, 123, 3825–3834. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.Y.; Guan, B.S.; Li, Z.K.; Li, X.Y. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: A meta-analysis. J. Telemed. Telecare 2018, 24, 157–167. [Google Scholar] [CrossRef]
- Myers, J.S.; Cook-Wiens, G.; Baynes, R.; Jo, M.Y.; Bailey, C.; Krigel, S.; Klemp, J.; Asher, A. Emerging from the Haze: A multicenter, controlled pilot study of a multidimensional, psychoeducation-based cognitive rehabilitation intervention for breast cancer survivors delivered with telehealth conferencing. Arch. Phys. Med. Rehabil. 2020, 101, 948–959. [Google Scholar] [CrossRef]
- Bargon, C.A.; Batenburg, M.C.T.; van Stam, L.E.; Mink van der Molen, D.R.; van Dam, I.E.; van der Leij, F.; Baas, I.O.; Ernst, M.F.; Maarse, W.; Vermulst, N.; et al. Impact of the COVID-19 pandemic on patient-reported outcomes of breast cancer patients and survivors. JNCI Cancer Spectr. 2020, 5, pkaa104. [Google Scholar] [CrossRef] [PubMed]
- Swainston, J.; Chapman, B.; Grunfeld, E.A.; Derakshan, N. COVID-19 lockdown and its adverse impact on psychological health in breast cancer. Front. Psychol. 2020, 11, 2033. [Google Scholar] [CrossRef] [PubMed]
- Hulbert-Williams, N.J.; Leslie, M.; Hulbert-Williams, L.; Smith, E.; Howells, L.; Pinato, D.J. Evaluating the impact of COVID-19 on supportive care needs, psychological distress and quality of life in UK cancer survivors and their support network. Eur. J. Cancer Care 2021, e13442. [Google Scholar] [CrossRef]
- Schade, E.C.; Elkaddoum, R.; Kourie, H.R. The psychological challenges for oncological patients in times of COVID-19 pandemic: Telemedicine, a solution? Future Oncol. 2020, 16, 2265–2268. [Google Scholar] [CrossRef]
- Eng, L.; Pringle, D.; Su, J.; Shen, X.; Mahler, M.; Niu, C.; Charow, R.; Tiessen, K.; Lam, C.; Halytskyy, O. Patterns, perceptions, and perceived barriers to physical activity in adult cancer survivors. Support Care Cancer 2018, 26, 3755–3763. [Google Scholar] [CrossRef]
- Tarasenko, Y.; Linder, D.; Miller, E. Muscle-strengthening and aerobic activities and mortality among 3+ year cancer survivors in the U.S. Cancer Causes Control 2018, 29, 475–484. [Google Scholar] [CrossRef]
- Garcia, D.; Thomson, C. Physical activity and cancer survivorship. Nutr. Clin. Pract. 2014, 29, 768–779. [Google Scholar] [CrossRef]
- Campbell, K.; Winters-Stone, K.; Wiskemann, J.; May, A.; Schwartz, A.; Courneya, K.; Zucker, D.; Matthews, C.; Ligibel, J.; Gerber, L.; et al. Exercise guidelines for cancer survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cormie, P.; Zopf, E.; Zhang, X.; Schmitz, K. The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol. Rev. 2017, 39, 71–92. [Google Scholar] [CrossRef] [PubMed]
- Aapro, M.; Bossi, P.; Dasari, A.; Fallowfield, L.; Gascón, P.; Geller, M.; Jordan, K.; Kim, J.; Martin, K.; Porzig, S. Digital health for optimal supportive care in oncology: Benefits, limits, and future perspectives. Support Care Cancer 2020, 28, 4589–4612. [Google Scholar] [CrossRef] [PubMed]
- Chung, I.Y.; Jung, M.; Park, Y.R.; Cho, D.; Chung, H.; Min, Y.H.; Park, H.J.; Lee, M.; Lee, S.B.; Chung, S.; et al. Exercise promotion and distress reduction using a mobile app-based community in breast cancer survivors. Front. Oncol. 2020, 9, 1505. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Garcia, A.; Lozano-Lozano, M.; Galiano-Castillo, N.; Postigo-Martin, P.; Arroyo-Morales, M.; Cantarero-Villanueva, I. A web-based exercise system (e-CuidateChemo) to counter the side effects of chemotherapy in patients with breast cancer: Randomized controlled trial. J. Med. Internet Res. 2019, 21, e14418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, J.L.; Rosen, A.B.; Wilson, F.A. The effect of telehealth interventions on quality of life of cancer patients: A systematic review and meta-analysis. Telemed. J. e-Health 2018, 24, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Larson, J.L.; Rosen, A.B.; Wilson, F.A. The effect of telehealth interventions on quality of life of cancer survivors: A systematic review and meta-analysis. Health Inform. J. 2020, 26, 1060–1078. [Google Scholar] [CrossRef] [Green Version]
- Blackwood, J.; Huang, M.H. The use of telehealth interventions to improve physical activity in adult cancer survivors: A systematic review. Rehabil. Oncol. 2018, 8, 355. Available online: https://www.epistemonikos.org/en/documents/c1a2ac3bca3c02a945ab5f3b1b8820bf1cdf013c (accessed on 30 June 2021).
- Wangwatcharakul, W.; Kapol, N.; Bunchuailua, W. The effectiveness of telemedicine for breast cancer disease management: A systematic review and meta-analysis. Thai Bull. Pharm. Sci. 2018, 13, 145–161. [Google Scholar]
- Newton, R.U.; Hart, N.H.; Clay, T. Keeping patients with cancer exercising in the age of COVID-19. JCO Oncol. Pract. 2020, 16, 656–664. [Google Scholar] [CrossRef]
- Bland, K.A.; Bigaran, A.; Campbell, K.L.; Trevaskis, M.; Zopf, E.M. Exercising in isolation? The role of telehealth in exercise oncology during the COVID-19 pandemic and beyond. Phys. Ther. 2020, 100, 1713–1716. [Google Scholar] [CrossRef] [PubMed]
- Tsang-Wright, F.; Tasoulis, M.K.; Roche, N.; MacNeill, F. Breast cancer surgery after the COVID-19 pandemic. Future Oncol. 2020, 16, 2687–2690. [Google Scholar] [CrossRef]
- Warner, E.T.; Restrepo, E.; Benjamin, C.; Fairley, R.; Roudebush, L.; Eshraghi, L.; Hertz, C.; Du, S.; Carfang, L. Abstract S11-02: Patient-reported impact of the COVID-19 pandemic on breast cancer screening, diagnosis, and treatment: A national survey. Clin. Cancer Res. 2020, 26 (Suppl. 18), S11-02. [Google Scholar] [CrossRef]
- Lorgelly, P.K.; Adler, A. Impact of a global pandemic on health technology assessment. Appl. Health Econ. Health Policy 2020, 18, 339–343. [Google Scholar] [CrossRef]
- Darcourt, J.G.; Aparicio, K.; Dorsey, P.M.; Ensor, J.E.; Zsigmond, E.M.; Wong, S.T.; Ezeana, C.F.; Puppala, M.; Heyne, K.E.; Geyer, C.E.; et al. Analysis of the implementation of telehealth visits for care of patients with cancer in Houston during the COVID-19 pandemic. JCO Oncol. Pract. 2021, 17, e36–e43. [Google Scholar] [CrossRef]
- Gutkin, P.M.; Prionas, N.D.; Minneci, M.O.; Allen, E., 3rd; Balazy, K.E.; Rahimy, E.; Chang, D.T.; Horst, K.C. Telemedicine in radiation oncology: Is it here to stay? Impacts on patient care and resident education. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, 416–420. [Google Scholar] [CrossRef]
- Patt, D.A.; Wilfong, L.; Toth, S.; Broussard, S.; Kanipe, K.; Hammonds, J.; Allen, V.; Mautner, B.; Campbell, N.; Dubey, A.K.; et al. Telemedicine in community cancer care: How technology helps patients with cancer navigate a pandemic. JCO Oncol. Pract. 2021, 17, e11–e15. [Google Scholar] [CrossRef]
- Onesti, C.E.; Tagliamento, M.; Curigliano, G.; Harbeck, N.; Bartsch, R.; Wildiers, H.; Tjan-Heijnen, V.; Martin, M.; Rottey, S.; Generali, D.; et al. Expected medium- and long-term impact of the COVID-19 outbreak in oncology. JCO Glob. Oncol. 2021, 7, 162–172. [Google Scholar] [CrossRef]
- Isautier, J.M.; Copp, T.; Ayre, J.; Cvejic, E.; Meyerowitz-Katz, G.; Batcup, C.; Bonner, C.; Dodd, R.; Nickel, B.; Pickles, K.; et al. People’s experiences and satisfaction with telehealth during the COVID-19 pandemic in Australia: Cross-sectional survey study. J. Med. Internet Res. 2020, 22, e24531. [Google Scholar] [CrossRef]
- Shaverdian, N.; Gillespie, E.F.; Cha, E.; Kim, S.Y.; Benvengo, S.; Chino, F.; Kang, J.J.; Li, Y.; Atkinson, T.M.; Lee, N.; et al. Impact of telemedicine on patient satisfaction and perceptions of care quality in radiation oncology. J. Natl. Compr. Canc. Netw. 2021, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ignatowicz, A.; Atherton, H.; Bernstein, C.J.; Bryce, C.; Court, R.; Sturt, J.; Griffiths, F. Internet videoconferencing for patient-clinician consultations in long-term conditions: A review of reviews and applications in line with guidelines and recommendations. Digit. Health 2019, 5, 2055207619845831. [Google Scholar] [CrossRef] [Green Version]
- Pareek, P.; Vishnoi, J.R.; Kombathula, S.H.; Vyas, R.K.; Misra, S. Teleoncology: The youngest pillar of oncology. JCO Glob. Oncol. 2020, 6, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.A.; Brennan, F.P.; Gardiner, M.D. Cancer rehabilitation and palliative care-Exploring the synergies. J. Pain Symptom Manag. 2020, 60, 1239–1252. [Google Scholar] [CrossRef] [PubMed]
- Freer, P.E. The impact of the COVID-19 pandemic on breast imaging. Radiol. Clin. N. Am. 2021, 59, 1–11. [Google Scholar] [CrossRef]
- White, L.A.; Krousel-Wood, M.A.; Mather, F. Technology meets healthcare: Distance learning and telehealth. Ochsner J. 2001, 3, 22–29. [Google Scholar]
- Jiménez-Rodríguez, D.; Santillán García, A.; Montoro Robles, J.; Rodríguez Salvador, M.; Muñoz Ronda, F.J.; Arrogante, O. Increase in video consultations during the COVID-19 pandemic: Healthcare professionals’ perceptions about their implementation and adequate management. Int. J. Environ. Res. Public Health 2020, 17, 5112. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, M.J.; Filart, R.; Burgess, L.P.; Lee, I.; Poropatich, R.K. Developing next-generation telehealth tools and technologies: Patients, systems, and data perspectives. Telemed. J. e-Health 2010, 16, 93–95. [Google Scholar] [CrossRef] [Green Version]
- Jiang, C.Y.; El-Kouri, N.T.; Elliot, D.; Shields, J.; Caram, M.E.V.; Frankel, T.L.; Ramnath, N.; Passero, V.A. Telehealth for cancer care in veterans: Opportunities and challenges revealed by COVID. JCO Oncol. Pract. 2021, 17, 22–29. [Google Scholar] [CrossRef]
- Elliott, V.L. Department of Veterans Affairs (VA): A Primer on Telehealth (R45834). Available online: https://crsreports.congress.gov/product/pdf/R/R45834 (accessed on 26 July 2019).

| Health Care Technological Tool | Study Design–Number of Participants | Objective of the Study | Main Findings | References |
|---|---|---|---|---|
| Telehealth | Retrospective study of 1351 subjects (842 in-person and 509 telehealth) | To assess the feasibility of conducting integrative oncology consultations via telehealth during the COVID-19 pandemic (2020) | Increased physical activity among cancer patients in the telehealth group compared with those in the in-person group. | Narayanan et al., 2020 [27] |
| Telemedicine | Retrospective study of 77 cancer patients at Oncology Center in Brazil | To observe the use of telemedicine appointments at Oncology Centre | Telemedicine appointments for breast cancer follow-up (46.8%), breast cancer screening (26%) and benign breast disease evaluation (13%). | Sonagli et al., 2021 [41] |
| Telemedicine | Prospective study of 26 female breast cancer patients | To evaluate the viability and acceptance of occupational therapy services using a telemedicine model | Videoconferencing telemedicine for both perioperative and post-operative sessions were practical, effective and satisfactory and could be used for rehabilitative services. | Lai et al., 2021 [57] |
| Telehealth | Prospective study of 235 breast reconstruction surgery patients | To investigate the use of video telehealth to provide consultation to patients after breast reconstruction | Eighty eight (37.4%) of the 235 breast cancer patients received consultation via telehealth visit relating to post-surgical wound healing. | Colakoglu et al., 2021 [60] |
| Telehealth | A self-administrated electronic survey of 222 medical oncologist including those treating breast cancer patients | To evaluate the views of oncologists on virtual management of patients and the priority of prescribing anti-cancer treatments | Clinical oncologists have a high level of awareness of virtual management but 50% did not favor virtual prescription of chemotherapy and 45% prefer to manage cases virtually. | Tashkandi et al., 2020 [73] |
| Telehealth | Questionnaire-based study of 215 respondents with breast or gynecological cancer; 74 participated in telehealth visit | To assess the perceptions of the utility of telehealth among cancer patients in an outpatient breast/ gynecological centre | Majority (92%) was highly satisfied, 73% reported better access to care, 82% improved health and 92% saved time due to the telehealth services. | Zimmerman et al., 2020 [77] |
| Telehealth | Study involved 172 patients with the majority presenting with gastrointestinal malignancies (9.5%) with 14.5% breast cancer patients | To evaluate patients’ perspectives and preferences regarding telemedicine | High patient satisfaction and perception of the technology as safe and effective. | Hasson et al., 2021 [78] |
| Telehealth | A study involving 1244 breast cancer patients from 18 centers from Italy and France | To assess the levels of satisfaction of clinicians and patients who agreed to video visits | High satisfaction with telehealth visits during the COVID-19 pandemic, and the technology was feasible regardless of the mode. | Bizot et al., 2020 [79] |
| Telemedicine | Survey of 105 patients (38%) | To assess usability of virtual cancer care delivery for patients and providers across | Telemedicine adoption and use in clinical care of cancer patients was perceived to be safe and favorable by physicians and patients. | Miller et al., 2020 [80] |
| Healthcare Technological Tool | Study Design–Number of Participants | Objective of the Study | Main Findings | References |
|---|---|---|---|---|
| Teleoncology | Descriptive cross-sectional study of 421 cancer patients | The use of teleoncology (video call) at a tertiary care comprehensive oncology center | Majority of patients (64.1%) who were contacted using telemedicine had breast cancer. Teleoncology facilitated remote communication and 32.1% of patients required no further intervention. | Yildiz and Oksuzoglu, 2020 [69] |
| Teleoncology | Internet-based cross-sectional survey of 381 participants (21% breast cancer patients) | To evaluate the perspective and satisfaction of cancer patients with virtual appointment | Sixty two percent of the respondents reported having had a virtual oncology appointment, 82% had high satisfaction and there was significant use of videoconferencing. | Loree et al., 2021 [76] |
| Telerehabilitation | Survey of 15 women with primary complaints of shoulder stiffness, pain, and lymphedema | To evaluate distress and quality of life of breast cancer patients receiving care for breast cancer–related impairments during closure of rehabilitation services due to COVID-19. | Increased distress due to the closure of rehabilitation services due to the COVID-19 pandemic which was associated with decreased quality of life and physical activity. There were improvements following restart of rehabilitation service and offering of telehealth to one-third of the breast cancer survivors. | Helm et al., 2020 [90] |
| Telerehabilitation | Study of breast cancer survivors that require rehabilitation as part of their care | To implement telerehabilitation as an initial option for continued care to breast cancer patients | The physical therapy telerehabilitation program provides a range of movement modality, a multicomponent exercise program and aerobic exercises that could be performed in a home environment. | de Rezende et al., 2021 [91] |
| Telerehabilitation | Study of breast cancer survivors that attend a Chilean hospital | To implement a model of telerehabilitation | High level of approval and satisfaction by breast cancer patients, clinicians and physiotherapists. | Mella-Abarca et al., 2020 [92] |
| Telerehabilitation | Study conducted over approximately 3 months comprising 118 breast cancer patients | To implement a model of telerehabilitation in a public referral hospital | Majority (63%) of the 226 events were conducted via telerehabilitation. These include pre-operative checks, follow-up appointments and prevention of lymphedema. | Mella-Abarca et al., 2020 [92] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGrowder, D.A.; Miller, F.G.; Vaz, K.; Anderson Cross, M.; Anderson-Jackson, L.; Bryan, S.; Latore, L.; Thompson, R.; Lowe, D.; McFarlane, S.R.; et al. The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic. Healthcare 2021, 9, 1401. https://doi.org/10.3390/healthcare9101401
McGrowder DA, Miller FG, Vaz K, Anderson Cross M, Anderson-Jackson L, Bryan S, Latore L, Thompson R, Lowe D, McFarlane SR, et al. The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic. Healthcare. 2021; 9(10):1401. https://doi.org/10.3390/healthcare9101401
Chicago/Turabian StyleMcGrowder, Donovan A., Fabian G. Miller, Kurt Vaz, Melisa Anderson Cross, Lennox Anderson-Jackson, Sophia Bryan, Lyndon Latore, Rory Thompson, Dwight Lowe, Shelly R. McFarlane, and et al. 2021. "The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic" Healthcare 9, no. 10: 1401. https://doi.org/10.3390/healthcare9101401
APA StyleMcGrowder, D. A., Miller, F. G., Vaz, K., Anderson Cross, M., Anderson-Jackson, L., Bryan, S., Latore, L., Thompson, R., Lowe, D., McFarlane, S. R., & Dilworth, L. (2021). The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic. Healthcare, 9(10), 1401. https://doi.org/10.3390/healthcare9101401






