Spatial Variability of Geriatric Depression Risk in a High-Density City: A Data-Driven Socio-Environmental Vulnerability Mapping Approach
Abstract
:1. Introduction
2. Data and Methods
2.1. Data Collection
2.2. Measures
2.3. Analytic Approach
2.4. Socio-Environmental Vulnerability Index: Development and Validation
3. Results
3.1. Data Summary
3.2. Geriatric Depression Risk
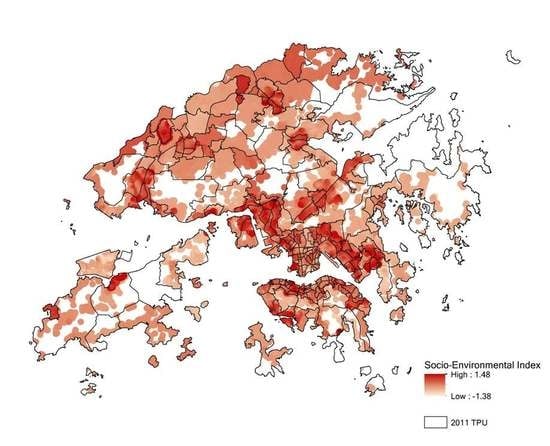
3.3. Socio-Environmental Vulnerability Index
4. Discussion
4.1. Advantage of the Cross-Sectional Analysis
4.2. Relationship between Geriatric Depression and Local Environment
4.3. Connection with Local Geriatric Studies
4.4. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Alexopoulos, G.S. Depression in the elderly. Lancet 2005, 365, 1961–1970. [Google Scholar] [CrossRef]
- Almeida, O.P.; Almeida, S.A. Short versions of the geriatric depression scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int. J. Geriatr. Psychiatry 1999, 14, 858–865. [Google Scholar] [CrossRef]
- Copeland, J.R.; Dewey, M.E.; Wood, N.; Searle, R.; Davidson, I.A.; McWilliam, C. Range of mental illness among the elderly in the community. Prevalence in Liverpool using the GMS-AGECAT package. Br. J. Psychiatry 1987, 150, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Kay, D.W.K.; Henderson, A.S.; Scott, R.; Wilson, J.; Rickwood, D.; Grayson, D.A. Dementia and depression among the elderly living in the Hobart community: The effect of the diagnostic criteria on the prevalence rates. Psychol. Med. 1985, 15, 771–788. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Hawkins, A.; Graham, N.; Blizard, B.; Mann, A. The Gospel Oak Study: Prevalence rates of dementia, depression and activity limitation among elderly residents in inner London. Psychol. Med. 1990, 20, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.E.; Shema, S.J.; Kaplan, G.A.; Strawbridge, W.J. Sleep complaints and depression in an aging cohort: A prospective perspective. Am. J. Psychiatry 2000, 157, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Chau, J.P.C.; Thompson, D.R.; Chang, A.M.; Woo, J.; Twinn, S.; Cheung, S.K.; Kwok, T. Depression among Chinese stroke survivors six months after discharge from a rehabilitation hospital. J. Clin. Nurs. 2010, 19, 3042–3050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, S.Y.; Lau, E.M.; Lynn, H.; Leung, P.C.; Woo, J.; Cummings, S.R.; Orwoll, E. Depression and bone mineral density: Is there a relationship in elderly Asian men? Results from Mr. Os (Hong Kong). Osteoporos. Int. 2005, 16, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.; Woo, J.; Lynn, H.S.; Leung, J.; Tang, Y.N.; Leung, P.C. Risk of depression in patients with chronic respiratory diseases: Results from two large cohort studies in Chinese elderly from Hong Kong. Int. J. Geriatr. Psychiatry 2006, 21, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.Y.; Mercer, S.W.; Woo, J.; Leung, J. The influence of multi-morbidity and self-reported socio-economic standing on the prevalence of depression in an elderly Hong Kong population. BMC Public Health 2008, 8, 119. [Google Scholar] [CrossRef] [PubMed]
- Firdaus, G. Built environment and health outcomes: Identification of contextual risk factors for mental well-being of older adults. Ageing Int. 2017, 42, 62–77. [Google Scholar] [CrossRef]
- Harlow, S.D.; Goldberg, E.L.; Comstock, G.W. A longitudinal study of risk factors for depressive symptomatology in elderly widowed and married women. Am. J. Epidemiol. 1991, 134, 526–538. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, G.J.; Kelman, H.R.; Thomas, C. The emergence of depressive symptoms in late life: The importance of declining health and increasing disability. J. Community Health 1990, 15, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Luppa, M.; Sikorski, C.; Luck, T.; Ehreke, L.; Konnopka, A.; Wiese, B.; Weyerer, S.; König, H.-H.; Riedel-Heller, S.G. Age and gender-specific prevalence of depression in latest-life—Systematic review and meta-analysis. J. Affect. Disord. 2012, 136, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Østbye, T.; Kristjansson, B.; Hill, G.; Newman, S.C.; Brouwer, R.N.; McDowell, I. Prevalence and predictors of depression in elderly Canadians: The Canadian Study of Health and Aging. Chronic Dis. Inj. Can. 2005, 26, 93. [Google Scholar]
- Sugiyama, T.; Leslie, E.; Giles-Corti, B.; Owen, N. Associations of neighbourhood greenness with physical and mental health: Do walking, social coherence and local social interaction explain the relationships? J. Epidemiol. Community Health 2008, 62, 1203–1210. [Google Scholar] [CrossRef]
- Van den Berg, A.E.; Maas, J.; Verheij, R.A.; Groenewegen, P.P. Green space as a buffer between stressful life events and health. Soc. Sci. Med. 2010, 70, 1203–1210. [Google Scholar] [CrossRef] [PubMed]
- Guite, H.F.; Clark, C.; Ackrill, G. The impact of the physical and urban environment on mental well-being. Public Health 2006, 120, 1117–1126. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W. The built environment and mental health. J. Urban Health 2003, 80, 536–555. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W.; Lepore, S.J.; Allen, K.M. Cross-cultural differences in tolerance for crowding: Fact or fiction? J. Personal. Soc. Psychol. 2000, 79, 204. [Google Scholar] [CrossRef]
- Evans, G.W.; Wells, N.M.; Moch, A. Housing and mental health: A review of the evidence and a methodological and conceptual critique. J. Soc. Issues 2003, 59, 475–500. [Google Scholar] [CrossRef]
- Gifford, R. The consequences of living in high-rise buildings. Archit. Sci. Rev. 2007, 50, 2–17. [Google Scholar] [CrossRef]
- Bao, J.; Li, X.; Yu, C. The construction and validation of the heat vulnerability index, a review. Int. J. Environ. Res. Public Health 2015, 12, 7220–7234. [Google Scholar] [CrossRef] [PubMed]
- Cutter, S.L. The vulnerability of science and the science of vulnerability. Ann. Assoc. Am. Geogr. 2003, 93, 1–12. [Google Scholar] [CrossRef]
- Morrow, B.H. Identifying and mapping community vulnerability. Disasters 1999, 23, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; O’Neill, M.S.; Gronlund, C.J.; Brines, S.J.; Brown, D.G.; Diez-Roux, A.V.; Schwartz, J. Mapping community determinants of heat vulnerability. Environ. Health Perspect. 2009, 117, 1730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bell, N.; Hayes, M.V. The Vancouver Area Neighbourhood Deprivation Index (VANDIX): A census-based tool for assessing small-area variations in health status. Can. J. Public Health 2012, 103, S28–S32. [Google Scholar] [PubMed]
- Chateau, D.; Metge, C.; Prior, H.; Soodeen, R.A. Learning from the census: The Socio-economic Factor Index (SEFI) and health outcomes in Manitoba. Can. J. Public Health 2012, 103, S23–S27. [Google Scholar] [PubMed]
- Chau, P.H.; Gusmano, M.K.; Cheng, J.O.; Cheung, S.H.; Woo, J. Social vulnerability index for the older people—Hong Kong and New York City as examples. J. Urban Health 2014, 91, 1048–1064. [Google Scholar] [CrossRef] [PubMed]
- Kihal-Talantikite, W.; Padilla, C.M.; Lalloue, B.; Rougier, C.; Defrance, J.; Zmirou-Navier, D.; Deguen, S. An exploratory spatial analysis to assess the relationship between deprivation, noise and infant mortality: An ecological study. Environ. Health 2013, 12, 109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padilla, C.M.; Deguen, S.; Lalloue, B.; Blanchard, O.; Beaugard, C.; Troude, F.; Navier, D.Z.; Vieira, V.M. Cluster analysis of social and environment inequalities of infant mortality: A spatial study in small areas revealed by local disease mapping in France. Sci. Total Environ. 2013, 454, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Pampalon, R.; Hamel, D.; Gamache, P.; Philibert, M.D.; Raymond, G.; Simpson, A. An area-based material and social deprivation index for public health in Québec and Canada. Can. J. Public Health 2012, 103, S17–S22. [Google Scholar] [PubMed]
- Pampalon, R.; Hamel, D.; Gamache, P.; Simpson, A.; Philibert, M.D. Validation of a deprivation index for public health: A complex exercise illustrated by the Quebec index. Chronic Dis. Inj. Can. 2014, 34, 12–22. [Google Scholar] [PubMed]
- Aminipouri, M.; Knudby, A.; Ho, H.C. Using multiple disparate data sources to map heat vulnerability: Vancouver case study. Can. Geogr. 2016, 60, 356–368. [Google Scholar] [CrossRef]
- Buscail, C.; Upegui, E.; Viel, J.F. Mapping heatwave health risk at the community level for public health action. Int. J. Health Geogr. 2012, 11, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, H.C.; Knudby, A.; Huang, W. A Spatial Framework to Map Heat Health Risks at Multiple Scales. Int. J. Environ. Res. Public Health 2015, 12, 16110–16123. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.C.; Knudby, A.; Walker, B.B.; Henderson, S.B. Delineation of spatial variability in the temperature-mortality relationship on extremely hot days in Greater Vancouver, Canada. Environ. Health Perspect. 2017, 125, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Morelli, X.; Rieux, C.; Cyrys, J.; Forsberg, B.; Slama, R. Air pollution, health and social deprivation: A fine-scale risk assessment. Environ. Res. 2016, 147, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Morrison, S.; Fordyce, F.M.; Scott, E.M. An initial assessment of spatial relationships between respiratory cases, soil metal content, air quality and deprivation indicators in Glasgow, Scotland, UK: Relevance to the environmental justice agenda. Environ. Geochem. Health 2014, 36, 319–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padilla, C.M.; Kihal-Talantikit, W.; Vieira, V.M.; Deguen, S. City-specific spatiotemporal infant and neonatal mortality clusters: Links with socioeconomic and air pollution spatial patterns in France. Int. J. Environ. Res. Public Health 2016, 13, 624. [Google Scholar] [CrossRef] [PubMed]
- Sabel, C.E.; Wilson, J.G.; Kingham, S.; Tisch, C.; Epton, M. Spatial implications of covariate adjustment on patterns of risk: Respiratory hospital admissions in Christchurch, New Zealand. Soc. Sci. Med. 2007, 65, 43–59. [Google Scholar] [CrossRef] [PubMed]
- Thach, T.Q.; Zheng, Q.; Lai, P.C.; Wong, P.P.Y.; Chau, P.Y.K.; Jahn, H.J.; Plass, D.; Katzschner, L.; Kraemer, A.; Wong, C.M. Assessing spatial associations between thermal stress and mortality in Hong Kong: A small-area ecological study. Sci. Total Environ. 2015, 502, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, C.J.; Chapman, L.; Thornes, J.E.; Baker, C.J. Including the urban heat island in spatial heat health risk assessment strategies: A case study for Birmingham, UK. Int. J. Health Geogr. 2011, 10, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, B.B.; Schuurman, N.; Hameed, S.M. A GIS-based spatiotemporal analysis of violent trauma hotspots in Vancouver, Canada: Identification, contextualisation and intervention. BMJ Open 2014, 4, e003642. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.S.; Ho, H.C.; Yang, L.; Shi, W.; Yang, J.; Chan, T.C. Spatial variability of excess mortality during prolonged dust events in a high-density city: A time-stratified spatial regression approach. Int. J. Health Geogr. 2017, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Auluck, A.; Walker, B.B.; Hislop, G.; Lear, S.A.; Schuurman, N.; Rosin, M. Population-based incidence trends of oropharyngeal and oral cavity cancers by sex among the poorest and underprivileged populations. BMC Cancer 2014, 14, 316. [Google Scholar] [CrossRef] [PubMed]
- Auluck, A.; Walker, B.B.; Hislop, G.; Lear, S.A.; Schuurman, N.; Rosin, M. Socio-economic deprivation: A significant determinant affecting stage of oral cancer diagnosis and survival. BMC Cancer 2016, 16, 569. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.B.; Schuurman, N.; Auluck, A.; Lear, S.A.; Rosin, M. Suburbanisation of oral cavity cancers: Evidence from a geographically-explicit observational study of incidence trends in British Columbia, Canada, 1981–2010. BMC Public Health 2015, 15, 785. [Google Scholar] [CrossRef] [PubMed]
- Kwok, T.C.Y.; Su, Y.; Khoo, C.C.; Leung, J.; Kwok, A.; Orwoll, E.; Woo, J.; Leung, P.C. Predictors of non-vertebral fracture in older Chinese males and females: Mr. OS and Ms. OS (Hong Kong). J. Bone Miner. Metab. 2016, 3, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Nichol, J.; Lee, C.M. Urban vegetation monitoring in Hong Kong using high resolution multispectral images. Int. J. Remote Sens. 2005, 26, 903–918. [Google Scholar] [CrossRef]
- Nichol, J.; Wong, M.S.; Fung, C.; Leung, K.K. Assessment of urban environmental quality in a subtropical city using multispectral satellite images. Environ. Plan. B Plan. Des. 2006, 33, 39–58. [Google Scholar] [CrossRef]
- Planning Department. Urban Climatic Map and Standards for Wind Environment: Feasibility Study (No. 1); Technical Input Report; Planning Department: Hong Kong, 2008.
- De Craen, A.J.; Heeren, T.J.; Gussekloo, J. Accuracy of the 15-item geriatric depression scale (GDS-15) in a community sample of the oldest old. Int. J. Geriatr. Psychiatry 2003, 18, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.B.; Chiu, H.F.; Kowk, W.Y.; Leung, C.M. Chinese elderly and the GDS short form: A preliminary study. Clin. Gerontol. J. Aging Ment. Health 1993, 14, 37–42. [Google Scholar]
- Chau, J.; Martin, C.R.; Thompson, D.R.; Chang, A.M.; Woo, J. Factor structure of the Chinese version of the Geriatric Depression Scale. Psychol. Health Med. 2006, 11, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Marschner, I. Glm2: Fitting Generalized Linear Models. Available online: https://cran.r-project.org/web/packages/glm2/index.html (accessed on 8 July 2017).
- Forsell, Y. Predictors for depression, anxiety and psychotic symptoms in a very elderly population: Data from a 3-year follow-up study. Soc. Psychiatry Psychiatr. Epidemiol. 2000, 35, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Watkin, V.; Milne, B.; Manela, M.V.; Katona, C. Who becomes depressed? The Islington community study of older people. J. Affect. Disord. 2000, 58, 125–133. [Google Scholar] [CrossRef]
- Miles, R.; Coutts, C.; Mohamadi, A. Neighborhood urban form, social environment, and depression. J. Urban Health 2012, 89, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.; Verheij, R.A.; Groenewegen, P.P.; De Vries, S.; Spreeuwenberg, P. Green space, urbanity, and health: How strong is the relation? J. Epidemiol. Community Health 2006, 60, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Reijneveld, S.A.; Verheij, R.A.; de Bakker, D.H. The impact of area deprivation on differences in health: Does the choice of the geographical classification matter? J. Epidemiol. Community Health 2000, 54, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Dai, D.; Zhang, Y.; Lynch, C.A.; Miller, T.; Shakir, M. Childhood drowning in Georgia: A geographic information system analysis. Appl. Geogr. 2013, 37, 11–22. [Google Scholar] [CrossRef]
- Lee, K.M.; Wong, H.; Law, K.Y. Social polarisation and poverty in the global city the case of Hong Kong. China Rep. 2007, 43, 1–30. [Google Scholar] [CrossRef]
- Lehman, A.F. The well-being of chronic mental patients: Assessing their quality of life. Arch. Gen. Psychiatry 1983, 40, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Nutsford, D.; Pearson, A.L.; Kingham, S. An ecological study investigating the association between access to urban green space and mental health. Public Health 2013, 127, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.A.; James, P.; Rudolph, K.E.; Wu, C.D.; Schwartz, B.S. Greenness and birth outcomes in a range of Pennsylvania communities. Int. J. Environ. Res. Public Health 2016, 13, 311. [Google Scholar] [CrossRef] [PubMed]
- Wilker, E.H.; Wu, C.D.; McNeely, E.; Mostofsky, E.; Spengler, J.; Wellenius, G.A.; Mittleman, M.A. Green space and mortality following ischemic stroke. Environ. Res. 2014, 133, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Gong, F.; Lau, K.; Ng, E. Exploring association between neighbourhood green space and physical activity of elderly in high density cities. In Proceedings of the 36th International Conference on Passive and Low Energy Architecture, Los Angeles, CA, USA, 11–13 July 2016. [Google Scholar]
- Burton, E.J.; Mitchell, L.; Stride, C.B. Good places for ageing in place: Development of objective built environment measures for investigating links with older people’s wellbeing. BMC Public Health 2011, 11, 839. [Google Scholar] [CrossRef] [PubMed]
- Chi, I.; Yip, P.S.; Chiu, H.F.; Chou, K.L.; Chan, K.S.; Kwan, C.W.; Conwell, Y.; Caine, E. Prevalence of depression and its correlates in Hong Kong’s Chinese older adults. Am. J. Geriatr. Psychiatry 2005, 13, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.C.W.; Wong, C.S.M.; Wang, M.J.; Chan, W.C.; Chen, E.Y.H.; Ng, R.M.K.; Hung, H.-F.; Cheung, E.F.-C.; Sham, P.-C.; Chiu, H.F.-K.; et al. Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: The Hong Kong Mental Morbidity Survey (HKMMS). Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1379–1388. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.F.; Chung, J.W.; Wong, T.K.; Huang, C.M. Comparison of the prevalence and risk factors for depressive symptoms among elderly nursing home residents in Taiwan and Hong Kong. Int. J. Geriatr. Psychiatry 2005, 20, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Chi, I.; Chou, K.L. Social support and depression among elderly Chinese people in Hong Kong. Int. J. Aging Hum. Dev. 2001, 52, 231–252. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.T.; Lum, T.; Lam, L.C.; Fung, H.H. Hong Kong: Embracing a fast aging society with limited welfare. Gerontologist 2013, 53, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.C.; Lam, L.C.W.; Chen, E.Y.H. Hong Kong: Recent development of mental health services. BJPsych Adv. 2015, 21, 71–72. [Google Scholar] [CrossRef]
- Rushton, G. Public health, GIS, and spatial analytic tools. Ann. Rev. Public Health 2003, 24, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.R.; Richardson, E.A.; Mitchell, R.J.; Shortt, N.K. Environmental justice and health: The implications of the socio-spatial distribution of multiple environmental deprivation for health inequalities in the United Kingdom. Trans. Inst. Br. Geogr. 2010, 35, 522–539. [Google Scholar] [CrossRef]
- Pearce, J.R.; Richardson, E.A.; Mitchell, R.J.; Shortt, N.K. Environmental justice and health: A study of multiple environmental deprivation and geographical inequalities in health in New Zealand. Soc. Sci. Med. 2011, 73, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.C.; Knudby, A.; Sirovyak, P.; Xu, Y.; Hodul, M.; Henderson, S.B. Mapping maximum urban air temperature on hot summer days. Remote Sens. Environ. 2014, 154, 38–45. [Google Scholar] [CrossRef]
- Sun, Y.J.; Wang, J.F.; Zhang, R.H.; Gillies, R.R.; Xue, Y.; Bo, Y.C. Air temperature retrieval from remote sensing data based on thermodynamics. Theor. Appl. Climatol. 2005, 80, 37–48. [Google Scholar] [CrossRef]
- Kloog, I.; Nordio, F.; Coull, B.A.; Schwartz, J. Incorporating local land use regression and satellite aerosol optical depth in a hybrid model of spatiotemporal PM2.5 exposures in the Mid-Atlantic states. Environ. Sci. Technol. 2012, 46, 11913–11921. [Google Scholar] [CrossRef] [PubMed]



| Variables | Case (n = 364) | Control (n = 3566) | p-Value |
|---|---|---|---|
| Social Vulnerability | |||
| Older Ages (Age ≥ 80) | 15.4% | 9.5% | <0.05 |
| Living Alone | 19.8% | 12.9% | <0.05 |
| Low Education | 78.6% | 65.5% | <0.05 |
| Non-married | 39.6% | 28.1% | <0.05 |
| Male | 45.6% | 50.5% | 0.07 |
| Environmental Vulnerability | |||
| Pct. Residential | 33.8 ± 9.7 | 32.5 ± 10.4 | <0.05 |
| Pct. Vegetation | 24.6 ± 21.3 | 23.3 ± 21.2 | 0.28 |
| Average Building Height (m) | 33.8 ± 8.5 | 33.9 ± 9.1 | 0.84 |
| Variation of Building Height (m) | 32.1 ± 8.6 | 31.2 ± 9.3 | 0.06 |
| Variables | OA | LA | LE | NM | Male | %Res | %Veg | ABH | SDBH |
|---|---|---|---|---|---|---|---|---|---|
| Older Ages (OA) | 1 | ||||||||
| Living Alone (LA) | 0.13 | 1 | |||||||
| Low Education (LE) | 0.06 | 0.06 | 1 | ||||||
| Not Married (NM) | 0.21 | 0.55 | 0.19 | 1 | |||||
| Male | −0.03 | −0.19 | −0.27 | −0.38 | 1 | ||||
| Pct. Residential (%Res) | 0.03 | 0.08 | 0.07 | 0.06 | −0.05 | 1 | |||
| Pct. Vegetation (%Veg) | 0.01 | −0.03 | 0.07 | 0.03 | −0.04 | −0.21 | 1 | ||
| Avg Build Height (ABH) | −0.02 | 0.06 | 0.03 | 0.07 | −0.02 | −0.04 | 0.12 | 1 | |
| Std Build Height (SDBH) | −0.01 | 0.03 | 0.03 | 0.07 | −0.03 | −0.04 | 0.20 | 0.82 | 1 |
| Variables | Crude ORs | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| Older Ages: Age ≥ 80 | 1.74 (1.28, 2.36) * | 1.29 (0.93, 1.80) | 1.26 (0.91, 1.75) | |
| Living Alone | 1.66 (1.26, 2.19) * | 1.27 (0.91, 1.78) | 1.31 (0.93, 1.85) | |
| Low Education | 1.94 (1.49, 2.51) * | 1.63 (1.24, 2.16) * | 1.60 (1.21, 2.12) * | |
| Not Married | 1.67 (1.34, 2.09) * | 1.28 (0.95, 1.72) | 1.24 (0.92, 1.67) | |
| Male | 0.82 (0.66, 1.02) | 1.11 (0.85, 1.46) | 1.13 (0.86, 1.48) | |
| Pct. Residential | 1.01 (1.00, 1.02) * | 1.01 (1.00, 1.02) * | 1.01 (1.00, 1.02) * | |
| Pct. Vegetation | 1.00 (0.998, 1.01) | 1.00 (0.996, 1.01) | 1.00 (0.995, 1.01) | |
| Avg Build Height | 1.00 (0.99, 1.00) | 0.98 (0.96, 0.99) * | 0.98 (0.96, 0.99) * | |
| Std Build Height | 1.01 (0.999, 1.02) | 1.03 (1.01, 1.04) * | 1.03 (1.01, 1.04) * |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, H.C.; Lau, K.K.-L.; Yu, R.; Wang, D.; Woo, J.; Kwok, T.C.Y.; Ng, E. Spatial Variability of Geriatric Depression Risk in a High-Density City: A Data-Driven Socio-Environmental Vulnerability Mapping Approach. Int. J. Environ. Res. Public Health 2017, 14, 994. https://doi.org/10.3390/ijerph14090994
Ho HC, Lau KK-L, Yu R, Wang D, Woo J, Kwok TCY, Ng E. Spatial Variability of Geriatric Depression Risk in a High-Density City: A Data-Driven Socio-Environmental Vulnerability Mapping Approach. International Journal of Environmental Research and Public Health. 2017; 14(9):994. https://doi.org/10.3390/ijerph14090994
Chicago/Turabian StyleHo, Hung Chak, Kevin Ka-Lun Lau, Ruby Yu, Dan Wang, Jean Woo, Timothy Chi Yui Kwok, and Edward Ng. 2017. "Spatial Variability of Geriatric Depression Risk in a High-Density City: A Data-Driven Socio-Environmental Vulnerability Mapping Approach" International Journal of Environmental Research and Public Health 14, no. 9: 994. https://doi.org/10.3390/ijerph14090994
APA StyleHo, H. C., Lau, K. K.-L., Yu, R., Wang, D., Woo, J., Kwok, T. C. Y., & Ng, E. (2017). Spatial Variability of Geriatric Depression Risk in a High-Density City: A Data-Driven Socio-Environmental Vulnerability Mapping Approach. International Journal of Environmental Research and Public Health, 14(9), 994. https://doi.org/10.3390/ijerph14090994