A Face-Aging Smoking Prevention/Cessation Intervention for Nursery School Students in Germany: An Appearance-Focused Interventional Study
Abstract
:1. Introduction
1.1. Smoking Prevention/Cessation Interventions in German Nursing Schools
1.2. Theoretical Considerations on Photoaging Interventions in Adolescence
2. Materials and Methods
2.1. Study Design, Participants, and Setting
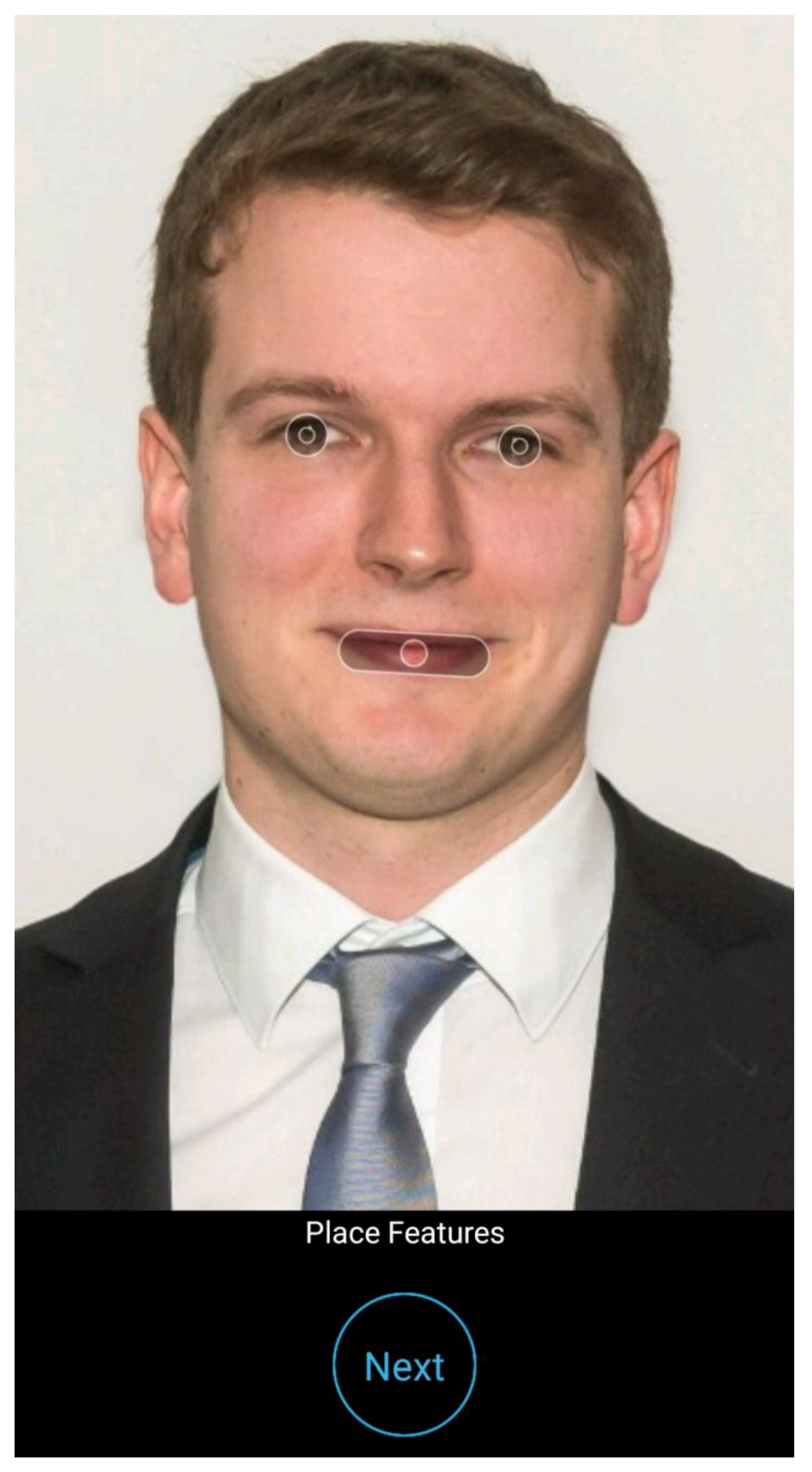
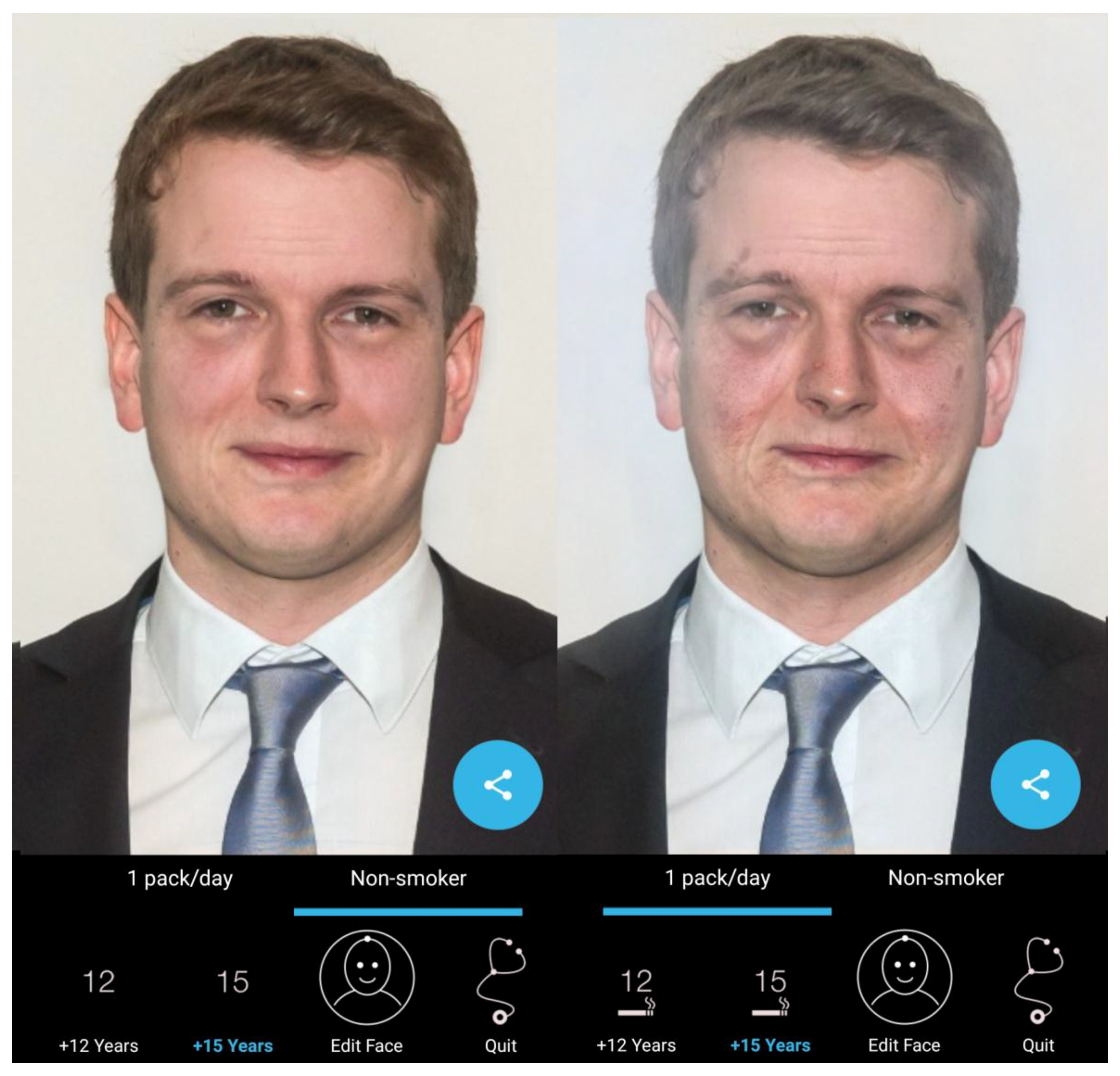
2.2. Intervention
2.3. Post-Intervention Survey
- (1)
- Change in motivation: (one item) “My 3D-selfie motivates me not to smoke”)
- (2)
- Perceived reactions of the peer group/the subjective norm: (four items) “My classmates think I look better as a non-smoker”, “The reactions of my classmates motivate me not to smoke” and “I think I can motivate coworkers with the Smokerface App to remain abstinent/to quit”
- (3)
- Future app use and sharing: (three items) “I plan to try this app again in the future,” “I want to install the Smokerface app on my phone,” and “I plan to show this app to other people”
- (4)
- Global feedback: (four items) “The intervention was fun,” “I learned new benefits of non-smoking,” “The app results are realistic”; “The time of the intervention was enough for everyone to morph their face”
2.4. Data Analysis
3. Results
3.1. Participants
3.2. Perceptions of the Intervention
3.2.1. Motivation Not to Smoke
3.2.2. Perceived Subjective Norm during the Intervention
3.2.3. App Reuse and Sharing
3.2.4. Global Feedback
3.2.5. How Can Nursery Students Best Be Motivated Not to Smoke?
- the need for a stronger focus on pathologies in the prevention curriculum (n = 27);
- the need to change of external factors should be discussed (n = 24; e.g., the need for a lower nurse to patient ratio at work, stress reduction, and a replacement for smoking breaks to be used by non-smokers; interestingly, these breaks were described as a major motivation for starting to smoke at work);
- interventions should take place earlier, such as early in secondary school n = 8);
- prevention programs do not help and/or that it was impossible to prevent smoking in nursing students (n = 7);
- the advantages of quitting should be discussed and quitting advice should be offered (n = 6);
- nobody should interfere with personal decisions to smoke (n = 5); and
- finally, there were several non-categorizable statements (n = 15), including Smokerface, emphasizing that quitting saves money, placing a stronger focus on smokers instead of nonsmokers, giving more motivation to quit, recommending prevention programs, and some statements of “I do not know.”
4. Discussion
4.1. Principal Considerations
4.2. Interpretation of Likert-Scale-Measurements from This Study
4.3. Interpretation of the Qualitative Feedback
4.4. Implications for Future Research
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Petrescu, D.; Vasiljevic, M.; Pepper, J.; Ribisl, K.; Marteau, T. What Is the Impact of E-Cigarette Adverts on Children’s Perceptions of Tobacco Smoking? An Experimental Study. Available online: https://tobaccocontrol.bmj.com/content/early/2016/08/12/tobaccocontrol-2016-052940?utm_source=trendmd&utm_medium=cpc&utm_campaign=bmjopen&trendmd-shared=1&utm_content=Journalcontent&utm_term=TrendMDPhase4 (accessed on 1 August 2018).
- Jha, P.; Peto, R. Global Effects of Smoking, of Quitting, and of Taxing Tobacco. N. Eng. J. Med. 2014, 370, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Batra, A.; Petersen, K.U.; Hoch, E.; Andreas, S.; Bartsch, G.; Gohlke, H.; Jähne, A.; Kröger, C.; Lindinger, P.; Mühlig, S. S3 Guideline “Screening, Diagnostics, and Treatment of Harmful and Addictive Tobacco Use”. SUCHT 2016. [Google Scholar] [CrossRef]
- Raupach, T.; Falk, J.; Vangeli, E.; Schiekirka, S.; Rustler, C.; Grassi, M.C.; Pipe, A.; West, R. Structured smoking cessation training for health professionals on cardiology wards: A prospective study. Eur. J. Prev. Cardiol. 2014, 21, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Balmford, J.; Leifert, J.A.; Jaehne, A. “Tobacco dependence treatment makes no sense because”…: Rebuttal of commonly-heard arguments against providing tobacco dependence treatment in the hospital setting. BMC Public Health 2014, 14, 1182. [Google Scholar] [CrossRef] [PubMed]
- Strobel, L.; Schneider, N.; Krampe, H.; Beißbarth, T.; Pukrop, T.; Anders, S.; West, R.; Aveyard, P.; Raupach, T. German medical students lack knowledge of how to treat smoking and problem drinking. Addiction 2012, 107, 1878–1882. [Google Scholar] [CrossRef] [PubMed]
- Raupach, T.; Merker, J.; Hasenfuß, G.; Andreas, S.; Pipe, A. Knowledge gaps about smoking cessation in hospitalized patients and their doctors. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.; Aitchison, P.; Harris, F.; Ozakinci, G.; Radley, A.; Bauld, L.; Entwistle, V.; Munro, A.; Haw, S.; Culbard, B. Barriers and facilitators to smoking cessation in a cancer context: A qualitative study of patient, family and professional views. BMC Cancer 2017, 17, 348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balmford, J.; Leifert, J.A.; Schulz, C.; Elze, M.; Jaehne, A. Implementation and effectiveness of a hospital smoking cessation service in Germany. Patient Educ. Couns. 2014, 94, 103–109. [Google Scholar] [CrossRef] [PubMed]
- La Torre, G.; Gualano, M.R.; Saulle, R.; Bontempi, C. Smoking Among Health Professionals. In Smoking Prevention and Cessation; Springer: Berlin, Germany, 2013; pp. 215–239. [Google Scholar]
- Bühler, A.; Schulze, K.; Rustler, C.; Scheifhacken, S.; Schweizer, I.; Bonse-Rohmann, M. Geschlechtsbezogene Analyse des Tabakkonsums bei Auszubildenden in Pflegeberufen. Sucht 2016. [Google Scholar] [CrossRef]
- Hoebel, J.; Kuntz, B.; Kroll, L.E.; Finger, J.D.; Zeiher, J.; Lange, C.; Lampert, T. Trends in absolute and relative educational inequalities in adult smoking since the early 2000s: The case of Germany. Nicotine Tobacco Res. 2017, 20, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, B.; Hoebel, J.; Lampert, T. Bildungsunterschiede im Tabakkonsum und Rauchausstieg junger Erwachsener. Ergebnisse der Studie “Gesundheit in Deutschland aktuell” (GEDA) 2009 und 2010. Das Gesundheitswesen 2014, 76, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, B.; Lampert, T. Smoking and passive smoke exposure among adolescents in Germany: Prevalence, trends over time, and differences between social groups. Dtsch. Ärzteblatt Int. 2016, 113, 23. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, B.; Waldhauer, J.; Moor, I.; Rathmann, K.; Richter, M.; Orth, B.; Piontek, D.; Kraus, L.; Zeiher, J.; Lampert, T. Zeitliche Entwicklung von Bildungsunterschieden im Rauchverhalten von Jugendlichen in Deutschland. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2018, 61, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, B.; Zeiher, J.; Hoebel, J.; Lampert, T. Soziale Ungleichheit, Rauchen und Gesundheit. Suchttherapie 2016, 17, 115–123. [Google Scholar] [CrossRef]
- Montano, D.E.; Kasprzyk, D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In Health Behavior: Theory, Research and Practice; John Wiley & Sons: Hoboken, NJ, USA, 2015; pp. 95–124. [Google Scholar]
- Brinker, T.J.; Holzapfel, J.; Baudson, T.G.; Sies, K.; Jakob, L.; Baumert, H.M.; Heckl, M.; Cirac, A.; Suhre, J.L.; Mathes, V. Photoaging smartphone app promoting poster campaign to reduce smoking prevalence in secondary schools: The Smokerface Randomized Trial: Design and baseline characteristics. BMJ Open 2016, 6, e014288. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Seeger, W. Photoaging Mobile Apps: A Novel Opportunity for Smoking Cessation? J. Med. Internet Res. 2015, 17, e186. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Seeger, W.; Buslaff, F. Photoaging Mobile Apps in School-Based Tobacco Prevention: The Mirroring Approach. J. Med. Internet Res. 2016, 18, e183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brinker, T.J.; Stamm-Balderjahn, S.; Seeger, W.; Groneberg, D.A. Education Against Tobacco (EAT): A quasi-experimental prospective evaluation of a programme for preventing smoking in secondary schools delivered by medical students: A study protocol. BMJ Open 2014, 4, e004909. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Stamm-Balderjahn, S.; Seeger, W.; Klingelhöfer, D.; Groneberg, D.A. Education Against Tobacco (EAT): A quasi-experimental prospective evaluation of a multinational medical-student-delivered smoking prevention programme for secondary schools in Germany. BMJ Open 2015, 5, e008093. [Google Scholar] [CrossRef] [PubMed]
- Xavier, L.E.D.F.; Bernardes-Souza, B.; Lisboa, O.C.; Seeger, W.; Groneberg, D.A.; Tran, T.-A.; Fries, F.N.; Corrêa, P.C.R.P.; Brinker, T.J. A Medical Student–Delivered Smoking Prevention Program, Education Against Tobacco, for Secondary Schools in Brazil: Study Protocol for a Randomized Trial. JMIR Res. Protoc. 2017, 6, e16. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Owczarek, A.D.; Seeger, W.; Groneberg, D.A.; Brieske, C.M.; Jansen, P.; Klode, J.; Stoffels, I.; Schadendorf, D.; Izar, B. A Medical Student-Delivered Smoking Prevention Program, Education Against Tobacco, for Secondary Schools in Germany: Randomized Controlled Trial. J. Med. Internet Res. 2017, 19, e199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faria, B.L.; Brieske, C.M.; Cosgarea, I.; Omlor, A.J.; Fries, F.N.; de Faria, C.O.M.; Lino, H.A.; Oliveira, A.C.C.; Lisboa, O.C.; Klode, J. A smoking prevention photoageing intervention for secondary schools in Brazil delivered by medical students: Protocol for a randomised trial. BMJ Open 2017, 7, e018589. [Google Scholar] [PubMed]
- Vitzthum, K.; Koch, F.; Groneberg, D.A.; Kusma, B.; Mache, S.; Marx, P.; Hartmann, T.; Pankow, W. Smoking behaviour and attitudes among German nursing students. Nurse Educ. Pract. 2013, 13, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Baudson, T.G.; Weber, K.E.; Freund, P.A. More Than Only Skin Deep: Appearance Self-Concept Predicts Most of Secondary School Students’ Self-Esteem. Front. Psychol. 2016, 7, 1568. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Büchele, G.; Jähnke, A.G.; Weiland, S.K. A cluster-randomized trial on smoking cessation in German student nurses. Prev. Med. 2006, 42, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Bühler, A.; Schulze, K.; Rustler, C.; Scheifhacken, S.; Schweizer, I.; Bonse-Rohmann, M. Tobacco prevention and reduction with nursing students: A non-randomized controlled feasibility study. Nurse Educ. Today 2017, 48, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Heckl, M.; Gatzka, M.; Heppt, M.V.; Rodrigues, H.R.; Schneider, S.; Sondermann, W.; e Silva, C.D.A.; Kirchberger, M.C.; Klode, J. A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study. JMIR mHealth uHealth 2018, 6, e60. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Faria, B.L.; Gatzka, M.; de Faria, O.M.; Heppt, M.V.; Kirchberger, M.C.; Schadendorf, D.; Nakamura, Y.; Buslaff, F.; Lisboa, O.C. A skin cancer prevention photoageing intervention for secondary schools in Brazil delivered by medical students: Protocol for a randomised controlled trial. BMJ Open 2018, 8, e018299. [Google Scholar] [CrossRef] [PubMed]
- Brinker, T.J.; Brieske, C.M.; Schaefer, C.M.; Buslaff, F.; Gatzka, M.; Petri, M.P.; Sondermann, W.; Schadendorf, D.; Stoffels, I.; Klode, J. Photoaging Mobile Apps in School-Based Melanoma Prevention: Pilot Study. J. Med. Internet Res. 2017, 19, e319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiwa, M.; Burford, O.; Parsons, R. Preliminary findings of how visual demonstrations of changes to physical appearance may enhance weight loss attempts. Eur. J. Public Health 2015, 25, 283–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brinker, T.J.; Enk, A.; Gatzka, M.; Nakamura, Y.; Sondermann, W.; Omlor, A.J.; Petri, M.P.; Karoglan, A.; Seeger, W.; Klode, J. A Dermatologist’s Ammunition in the War Against Smoking: A. Photoaging App. J. Med. Internet Res. 2017, 19, e326. [Google Scholar] [CrossRef] [PubMed]
- Burford, O.; Jiwa, M.; Carter, O.; Parsons, R.; Hendrie, D. Internet-Based Photoaging Within Australian Pharmacies to Promote Smoking Cessation: Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e64. [Google Scholar] [CrossRef] [PubMed]
- Weiss, C.; Hanebuth, D.; Coda, P.; Dratva, J.; Heintz, M.; Stutz, E.Z. Aging images as a motivational trigger for smoking cessation in young women. Int. J. Environ. Res. Public Health 2010, 7, 3499–3512. [Google Scholar] [CrossRef] [PubMed]
- Abroms, L.C.; Westmaas, J.L.; Bontemps-Jones, J.; Ramani, R.; Mellerson, J. A content analysis of popular smartphone apps for smoking cessation. Am. J. Prev. Med. 2013, 45, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Haskins, B.L.; Lesperance, D.; Gibbons, P.; Boudreaux, E.D. A systematic review of smartphone applications for smoking cessation. Transl. Behav. Med. 2017, 7, 292–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bricker, J.B.; Mull, K.E.; Kientz, J.A.; Vilardaga, R.; Mercer, L.D.; Akioka, K.J.; Heffner, J.L. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend. 2014, 143, 87–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buller, D.B.; Borland, R.; Bettinghaus, E.P.; Shane, J.H.; Zimmerman, D.E. Randomized trial of a smartphone mobile application compared to text messaging to support smoking cessation. Telemed. e-Health 2014, 20, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Powell, A.C.; Torous, J.; Chan, S.; Raynor, G.S.; Shwarts, E.; Shanahan, M.; Landman, A.B. Interrater reliability of mHealth app rating measures: Analysis of top depression and smoking cessation apps. JMIR mHealth uHealth 2016, 4, e15. [Google Scholar] [CrossRef] [PubMed]
- BinDhim, N.F.; McGeechan, K.; Trevena, L. Who uses smoking cessation apps? A feasibility study across three countries via smartphones. JMIR mHealth uHealth 2014, 2, e4. [Google Scholar] [CrossRef] [PubMed]
- McClure, J.B.; Hartzler, A.L.; Catz, S.L. Design considerations for smoking cessation apps: Feedback from nicotine dependence treatment providers and smokers. JMIR mHealth uHealth 2016, 4, e17. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Noh, G.-Y.; Park, D.-J. Smoking cessation apps for smartphones: Content analysis with the self-determination theory. J. Med. Internet Res. 2014, 16, e44. [Google Scholar] [CrossRef] [PubMed]
- Ferron, J.C.; Brunette, M.F.; Geiger, P.; Marsch, L.A.; Adachi-Mejia, A.M.; Bartels, S.J. Mobile phone apps for smoking cessation: Quality and usability among smokers with psychosis. JMIR Hum. Factors 2017, 4, e7. [Google Scholar] [CrossRef] [PubMed]
- Iacoviello, B.M.; Steinerman, J.R.; Klein, D.B.; Silver, T.L.; Berger, A.G.; Luo, S.X.; Schork, N.J. Clickotine, a personalized smartphone app for smoking cessation: Initial evaluation. JMIR mHealth uHealth 2017, 5, e56. [Google Scholar] [CrossRef] [PubMed]
- Ubhi, H.K.; Michie, S.; Kotz, D.; Wong, W.C.; West, R. A mobile app to aid smoking cessation: Preliminary evaluation of SmokeFree28. J. Med. Internet Res. 2015, 17, e17. [Google Scholar] [CrossRef] [PubMed]
- Ubhi, H.K.; Kotz, D.; Michie, S.; van Schayck, O.C.; Sheard, D.; Selladurai, A.; West, R. Comparative analysis of smoking cessation smartphone applications available in 2012 versus 2014. Addict. Behav. 2016, 58, 175–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thornton, L.; Quinn, C.; Birrell, L.; Guillaumier, A.; Shaw, B.; Forbes, E.; Deady, M.; Kay-Lambkin, F. Free smoking cessation mobile apps available in Australia: A quality review and content analysis. Aust. N. Z. J. Public Health 2017, 41, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Xu, J.; Su, C.; Fu, X.; Bricker, J. Content Analysis of Smartphone Apps for Smoking Cessation in China: Empirical Study. JMIR mHealth uHealth 2017, 5, e93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, E.Y.; Heffner, J.L.; Copeland, W.K.; Mull, K.E.; Bricker, J.B. Get with the program: Adherence to a smartphone app for smoking cessation. Addict. Behav. 2016, 63, 120–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baskerville, N.B.; Dash, D.; Wong, K.; Shuh, A.; Abramowicz, A. Perceptions Toward a Smoking Cessation App Targeting LGBTQ+ Youth and Young Adults: A Qualitative Framework Analysis of Focus Groups. JMIR Public Health Surveill. 2016, 2, e165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassandra, M.; Lintunen, T.; Kettunen, T.; Vanhala, M.; Toivonen, H.-M.; Kinnunen, K.; Heikkinen, R. Effectiveness of a mobile phone app for adults that uses physical activity as a tool to manage cigarette craving after smoking cessation: A study protocol for a randomized controlled trial. JMIR Res. Protoc. 2015, 4, e125. [Google Scholar] [PubMed]
- Hoeppner, B.B.; Hoeppner, S.S.; Seaboyer, L.; Schick, M.R.; Wu, G.W.; Bergman, B.G.; Kelly, J.F. How smart are smartphone apps for smoking cessation? A. content analysis. Nicot. Tob. Res. 2015, 18, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- McClure, J.B.; Anderson, M.L.; Bradley, K.; An, L.C.; Catz, S.L. Evaluating an adaptive and interactive mHealth smoking cessation and medication adherence program: A randomized pilot feasibility study. JMIR mHealth uHealth 2016, 4, e94. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.; Cha, E.M. Using a mobile app to promote smoking cessation in hospitalized patients. JMIR mHealth uHealth 2016, 4, e59. [Google Scholar] [CrossRef] [PubMed]
- BinDhim, N.F.; McGeechan, K.; Trevena, L. Smartphone Smoking Cessation Application (SSC App) trial: A multicountry double-blind automated randomised controlled trial of a smoking cessation decision-aid ‘app’. BMJ Open 2018, 8, e017105. [Google Scholar] [PubMed]
- Baskerville, N.B.; Struik, L.L.; Hammond, D.; Guindon, G.E.; Norman, C.D.; Whittaker, R.; Burns, C.M.; Grindrod, K.A.; Brown, K.S. Effect of a mobile phone intervention on quitting smoking in a young adult population of smokers: Randomized controlled trial study protocol. JMIR Research Protoc. 2015, 4, e10. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, B.; Bartlett, Y.K.; Tooley, E.; Armitage, C.J.; Wearden, A. Prevalence and frequency of mHealth and eHealth use among US and UK smokers and differences by motivation to quit. J. Med. Internet Res. 2015, 17, e164. [Google Scholar] [CrossRef] [PubMed]
- Naughton, F.; Hopewell, S.; Lathia, N.; Schalbroeck, R.; Brown, C.; Mascolo, C.; McEwen, A.; Sutton, S. A context-sensing mobile phone app (Q sense) for smoking cessation: A mixed-methods study. JMIR mHealth uHealth 2016, 4, e106. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Yang, F.; Haigh, M.M. Let me take a selfie: Exploring the psychological effects of posting and viewing selfies and groupies on social media. Telemat. Inform. 2017, 34, 274–283. [Google Scholar] [CrossRef]
- Barry, C.T.; Reiter, S.R.; Anderson, A.C.; Schoessler, M.L.; Sidoti, C.L. “Let Me Take Another Selfie”: Further Examination of the Relation Between Narcissism, Self-Perception, and Instagram Posts. Psychol. Popul. Media Cult. 2017. [Google Scholar] [CrossRef]
- Brown, T. #Let Me Take a Selfie: Social Media’s Influence on Teenage Girls. 2015. Available online: http://mcstor.library.milligan.edu/handle/11558/138 (accessed on 3 August 2018).
- Paris, C.M.; Pietschnig, J. ‘But First, Let Me Take a Selfie’: Personality Traits as Predictors of Travel Selfie Taking and Sharing Behaviors. 2015. Available online: https://scholarworks.umass.edu/cgi/viewcontent.cgi?article=1138&context=ttra (accessed on 3 August 2018).
- Hu, Y.; Manikonda, L.; Kambhampati, S. What We Instagram: A First Analysis of Instagram Photo Content and User Types. In Proceedings of the International AAAI Conference on Weblogs and Social Media (ICWSM), Ann Arbor, MI, USA, 2–4 June 2014. [Google Scholar]
- Van De Ven, M.O.; Engels, R.C.; Otten, R.; Van Den Eijnden, R.J. A longitudinal test of the theory of planned behavior predicting smoking onset among asthmatic and non-asthmatic adolescents. J. Behav. Med. 2007, 30, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; McLellan, J.; Perera, R. Effectiveness of school-based smoking prevention curricula: Systematic review and meta-analysis. BMJ Open 2015, 5, e006976. [Google Scholar] [CrossRef] [PubMed]
- De Kleijn, M.J.; Farmer, M.M.; Booth, M.; Motala, A.; Smith, A.; Sherman, S.; Assendelft, W.J.; Shekelle, P. Systematic review of school-based interventions to prevent smoking for girls. Syst. Rev. 2015, 4, 109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, X.; Alexander, R.L.; Simpson, S.A.; Goates, S.; Nonnemaker, J.M.; Davis, K.C.; McAfee, T. A cost-effectiveness analysis of the first federally funded antismoking campaign. Am. J. Prev. Med. 2015, 48, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.C.; Duke, J.; Shafer, P.; Patel, D.; Rodes, R.; Beistle, D. Perceived effectiveness of antismoking ads and association with quit attempts among smokers: Evidence from the tips from former smokers campaign. Health Commun. 2017, 32, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Neff, L.J.; Patel, D.; Davis, K.; Ridgeway, W.; Shafer, P.; Cox, S. Peer Reviewed: Evaluation of the National Tips From Former Smokers Campaign: The 2014 Longitudinal Cohort. Prev. Chronic Dis. 2016, 13, E42. [Google Scholar]
- Romer, D.; Ferguson, S.G.; Strasser, A.A.; Evans, A.T.; Tompkins, M.K.; Macisco, J.; Fardal, M.; Tusler, M.; Ellen, P. Effects of pictorial warning labels for cigarettes and quit-efficacy on emotional responses, smoking satisfaction, and cigarette consumption. Ann. Behav. Med. 2017, 52, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Mead, E.L.; Cohen, J.E.; Kennedy, C.E.; Gallo, J.; Latkin, C.A. The role of theory-driven graphic warning labels in motivation to quit: A qualitative study on perceptions from low-income, urban smokers. BMC Public Health 2015, 15, 92. [Google Scholar] [CrossRef] [PubMed]


| Do You Smoke? | How Often Do You Smoke? | Sum | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | Daily | Not Daily, But at Least Once A Week | Less than Once A Week | Not at All | ||
| Total | 52/26.4% | 145/73.6% | 46/23.3% | 6/3.0% | 15/7.6% | 130/66.0% | 197 |
| Male | 12/37.5% | 20/62.5% | 12/37.5% | 0/0% | 2/6.3% | 18/56.3% | 32 |
| Female | 40/24.2% | 125/75.8% | 34/20.6% | 6/3.6% | 13/7.9% | 112/67.9% | 165 |
| 1st year | 14/37.5% | 24/62.5% | 13/34.2% | 2/5.3% | 4/10.5% | 19/50.0% | 38 |
| 2nd year | 19/19.2% | 80/80.8% | 18/18.1% | 1/1.0% | 5/5.1% | 75/75.8% | 99 |
| 3rd year | 18/30.0% | 42/70.0% | 15/25.0% | 3/5.0% | 6/10.0% | 36/60.0% | 60 |
| 5-Point-Likert-Scales | Total | Smokers | Nonsmokers | Year 1 | Year 2–3 | Male | Female |
|---|---|---|---|---|---|---|---|
| The participation on AirPlay-Mirroring was fun 4: 1–2/4–5 | 143/73.3% 10/5.1% | 40/78.4% 2/3.9% | 103/71.5% 8/5.6% | 27/71.1% 1/2.6% | 116/73.9% 9/5.7% | 25/78.1% 0/0% | 118/72.4% 10/6.1% |
| My classmates think that I look better as a non-smoker in the long term 2: 1–2/4–5 | 141/73.4% 13/6.8% | 32/62.7% 7/13.7% | 109/77.3% 6/4.3% | 26/68.4% 5/13.2% | 115/74.7% 8/5.2% | 24/75.0% 1/3.1% | 117/73.1% 12/7.5% |
| The time sufficed so that everyone could encourage their face with the Smokerface App at least once 4: 1–2/4–5 | 191/97.0% 2/1.0% | 50/96.2% 1/1.9% | 141/97.2% 1/0.7% | 35/92.1% 3/7.9% | 156/98.1% 2/1.3% | 32/100% 0/0% | 159/96.4% 2/1.2% |
| I want to try the Smokerface App again after this hour 3: 1–2/4–5 | 43/21.8% 78/39.6% | 12/23.1% 18/34.6% | 31/21.4% 60/41.4% | 10/26.3% 14/36.8% | 33/20.8% 64/40.3% | 5/15.6% 11/34.8% | 38/23.0% 67/40.6% |
| Now I am more aware of the advantages of non-smoking than in the past 4: 1–2/4–5 | 70/35.5% 47/23.9% | 19/36.5% 15/28.8% | 51/35.2% 32/22.1% | 15/39.5% 12 31.6% | 55/34.6% 35/22.0% | 15/46.9% 8/25.0% | 55/33.3% 39/23.6% |
| I will install the Smokerface App on my mobile phone 3: 1–2/4–5 | 21/10.7% 127/64.8% | 7/13.5% 25/48.1% | 14/9.7% 102/70.8% | 3/8.1% 23/62.2% | 18/11.3% 104/65.4% | 4/12.5% 19/59.4% | 17/10.4% 108/65.9% |
| I will show the Smokerface App to other persons 3: 1–2/4–5 | 75/38.3% 56/28.6% | 20/38.5% 15/28.8% | 55/38.2% 41/28.5% | 13/34.2% 13/34.2% | 62/39.2% 43/27.2% | 10/31.3% 6/18.8% | 65/39.6% 50/30.5% |
| The animation of my face in the Smokerface App motivates me not to smoke 1: 1–2/4–5 | 81/42.0% 50/25.9% | 12/23.5% 23/45.1% | 69/48.6% 27/19.0% | 11/28.9% 12/31.6% | 70/45.2% 38/24.5% | 12/37.5% 11/34.4% | 69/42.9% 39/24.2% |
| Reactions of classmates during mirroring motivates me not to smoke 2: 1–2/4–5 | 67/34.7% 57/29.5% | 8/15.7% 26/51.0% | 59/41.5% 31/21.8% | 8/21.1% 15/39.5% | 59/38.1% 42/7.1% | 8/25.0% 12/37.5% | 59/36.6% 45/28% |
| The app results are realistic 4: 1–2/4–5 | 79/40.5% 47/24.1% | 16/31.4% 16/31.4% | 63/43.8% 31/21.5% | 12/32.4% 13/35.1% | 67/42.4% 34/21.5% | 14/43.8% 7/21.9% | 65/39.9% 40/24.5% |
| With the Smokerface App I can motivate coworkers to stay nonsmokers 2: 1–2/4–5 | 59/30.1% 63/32.1% | 17/33.3% 16/31.4% | 42/29% 47/32.4% | 8/21.1% 11/28.9% | 51/32.3% 52/32.9% | 11/34.4% 8/25.0% | 48/29.3% 55/33.5% |
| With the Smokerface App I can motivate coworkers to top smoking 2: 1–2/4–5 | 29/14.8% 99/50.5% | 4/7.8% 30/58.8% | 25/17.2% 69/47.6% | 6/15.8% 20/52.6% | 23/14.6% 79/50.0% | 4/12.5% 13/40.6% | 25/15.2% 86/52.4% |
| Items | Agreement of Nursery Students | Agreement of 7th Graders |
|---|---|---|
| The intervention was fun | 143/195, 73.3% | 77/125, 61.6% |
| Motivated me not to smoke | 81/193, 42.0% | 79/125, 63.2% |
| Learned new benefits of non-smoking | 70/198, 35.3%, | 81/125, 64.8% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brinker, T.J.; Alfitian, J.; Seeger, W.; Groneberg, D.A.; Von Kalle, C.; Enk, A.H.; Herth, F.J.F.; Kreuter, M.; Bauer, C.M.; Gatzka, M.; et al. A Face-Aging Smoking Prevention/Cessation Intervention for Nursery School Students in Germany: An Appearance-Focused Interventional Study. Int. J. Environ. Res. Public Health 2018, 15, 1656. https://doi.org/10.3390/ijerph15081656
Brinker TJ, Alfitian J, Seeger W, Groneberg DA, Von Kalle C, Enk AH, Herth FJF, Kreuter M, Bauer CM, Gatzka M, et al. A Face-Aging Smoking Prevention/Cessation Intervention for Nursery School Students in Germany: An Appearance-Focused Interventional Study. International Journal of Environmental Research and Public Health. 2018; 15(8):1656. https://doi.org/10.3390/ijerph15081656
Chicago/Turabian StyleBrinker, Titus J., Jonas Alfitian, Werner Seeger, David A. Groneberg, Christof Von Kalle, Alexander H. Enk, Felix J. F. Herth, Michael Kreuter, Claudia M. Bauer, Martina Gatzka, and et al. 2018. "A Face-Aging Smoking Prevention/Cessation Intervention for Nursery School Students in Germany: An Appearance-Focused Interventional Study" International Journal of Environmental Research and Public Health 15, no. 8: 1656. https://doi.org/10.3390/ijerph15081656
APA StyleBrinker, T. J., Alfitian, J., Seeger, W., Groneberg, D. A., Von Kalle, C., Enk, A. H., Herth, F. J. F., Kreuter, M., Bauer, C. M., Gatzka, M., & Suhre, J. L. (2018). A Face-Aging Smoking Prevention/Cessation Intervention for Nursery School Students in Germany: An Appearance-Focused Interventional Study. International Journal of Environmental Research and Public Health, 15(8), 1656. https://doi.org/10.3390/ijerph15081656






