Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China
Abstract
:1. Introduction
2. Revisiting Health Disparity and Institutions of Healthcare Resources Distribution
2.1. Health Disparity and the Uneven Distribution of Healthcare Resources
2.2. China’s Healthcare Institutions: From Central Planning to Radical Marketization
3. Data and Methodology
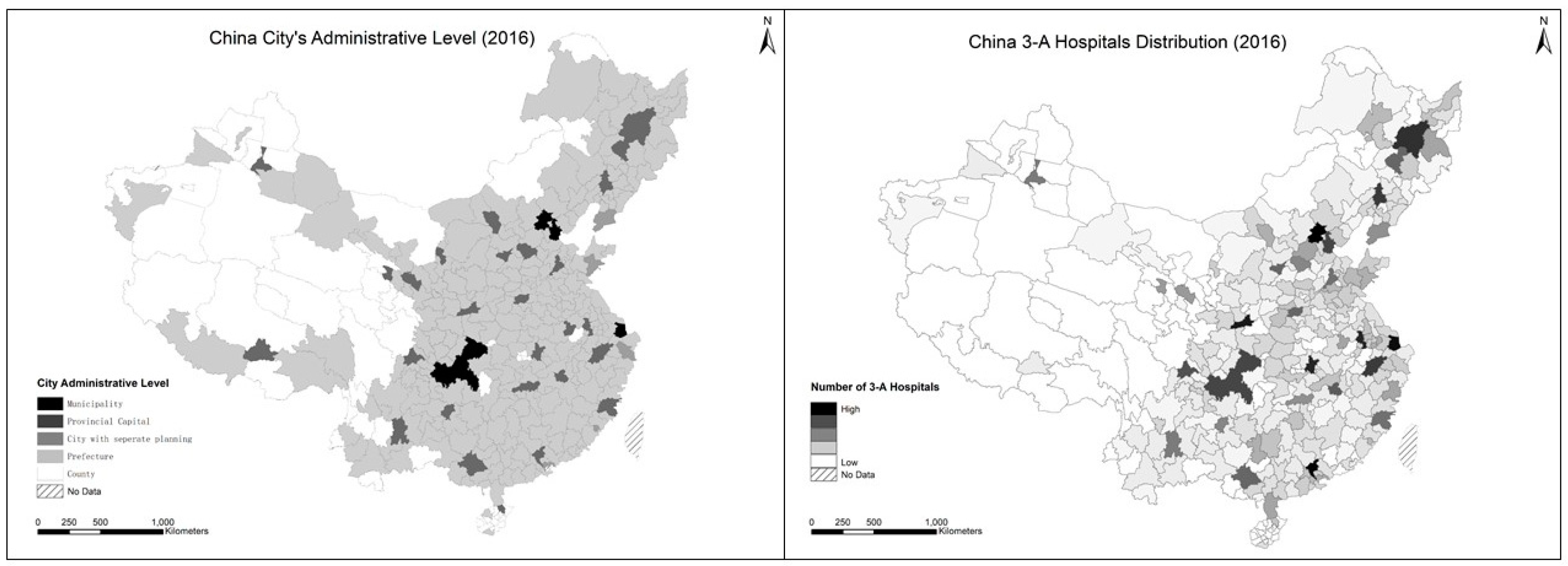
3.1. Developing an Integrated Database of High-Quality Hospitals
3.2. Modeling a Comprehensive Evaluation Framework
3.3. Measuring Uneven Distribution of High-Quality Healthcare Resources
3.3.1. Inequality Measurement Methods
3.3.2. Inequality Decomposition by Subgroups
4. Empirical Results and Major Findings
4.1. Determinants of 3-A Hospitals’ Performance
4.2. 3-A Hospitals Scores Distribution and GE() Values at Multiple Scales
4.3. Interpreting the Unevenness at Different Scales
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chang, J. Chinese Spur Medical-Tourism Growth in the US. China Daily USA. 2015. Available online: http://usa.chinadaily.com.cn/epaper/2015-08/07/content_21527300.htm (accessed on 20 April 2019).
- Liu, Y.; Rao, K.; Wu, J.; Gakidou, E. China’s health system performance. Lancet 2008, 372, 1914–1923. [Google Scholar] [CrossRef]
- Tang, S.; Meng, Q.; Chen, L.; Bekedam, H.; Evans, T.; Whitehead, M. Tackling the challenges to health equity in China. Lancet 2008, 372, 1493–1501. [Google Scholar] [CrossRef]
- Zhang, X.; Kanbur, R. Spatial inequality in education and health care in China. China Econ. Rev. 2005, 16, 189–204. [Google Scholar] [CrossRef] [Green Version]
- State Council, Central Committee of CPC. Outline of the Plan for “Healthy China 2030”. 2016. Available online: https://china.lexiscn.com/law/law-english-1-2961294-T.html (accessed on 15 April 2019).
- State Council of China. China to Continue Improving Fairness, Accessibility of Health Service: Minister. Official Website of the State Council of China; 2017. Available online: http://english.gov.cn/state_council/ministries/2017/05/23/content_281475664671834.htm (accessed on 11 July 2019).
- Liu, M.; Zhang, Q.; Lu, M.; Kwon, C.; Quan, H. Rural and urban disparity in health services utilization in China. Med Care 2007, 45, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Gottlieb, L. The social determinants of health: Its time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. 2), 19–31. [Google Scholar] [CrossRef]
- Rich, R.F.; Elkins, C.L. Health disparities. In Encyclopedia of Health Services Research; Mullner, R., Ed.; Sage: Los Angeles, CA, USA, 2009; Available online: http://sk.sagepub.com.eproxy.lib.hku.hk/reference/healthservices/n174.xml (accessed on 10 July 2019).
- Braveman, P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014, 129 (Suppl. 2), 5–8. [Google Scholar] [CrossRef]
- Eriksson, T.; Pan, J.; Qin, X. The intergenerational inequality of health in China. China Econ. Rev. 2014, 31, 392–409. [Google Scholar] [CrossRef] [Green Version]
- Guo, H. Research on the Equity of Rural and Urban Residents Basic Medical Insurance Scheme: The Case of Chengdu; Southwest University of Finance and Economics Press: Chengdu, China, 2014. (In Chinese) [Google Scholar]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Health & Human Services. Healthy People 2010: Understanding and Improving Health; U.S. Department of Health & Human Services: Washington, DC, USA, 2000; 63p.
- World Health Organ; Commission on Social Determinants of Health. CSDH Final Report: Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- U.S. Department of Health & Human Services. Healthy People 2020 Framework; U.S. Department of Health & Human Services: Washington, DC, USA, 2011. Available online: http://www.healthypeople.gov/2020/Co (accessed on 9 July 2019).
- U.S. Department of Health & Human Services. Healthy People 2000: National Health Promotion and Disease Prevention Objectives; U.S. Department of Health & Human Services: Washington, DC, USA, 1991.
- U.K. Department of Health and Social Care. Tackling Health Inequalities: A Programme for Action; U.K. Department of Health and Social Care: London, UK, 2003.
- Bleich, S.N.; Jarlenski, M.P.; Bell, C.N.; Laveist, T.A. Health inequalities: Trends, progress, and policy. Annu. Rev. Public Health 2012, 33, 7–40. [Google Scholar] [CrossRef]
- Doorslaer, E.V. Inequalities in access to medical care by income in developed countries. Can. Med Assoc. J. 2006, 174, 177–183. [Google Scholar] [CrossRef] [Green Version]
- Yip, W.; Hsiao, W. Chinas health care reform: A tentative assessment. China Econ. Rev. 2009, 20, 613–619. [Google Scholar] [CrossRef]
- La Foucade, A.; Scott, E. Equity in health. In The SAGE Encyclopedia of World Poverty; Odekon, M., Ed.; SAGE: Thousand Oaks, CA, USA, 2015; Available online: http://sk.sagepub.com.eproxy.lib.hku.hk/reference/healthservices/n174.xml (accessed on 11 July 2019).
- Evandrou, M.; Falkingham, J.; Feng, Z.; Vlachantoni, A. Individual and province inequalities in health among older people in China: Evidence and policy implications. Health Place 2014, 30, 134–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miao, J.; Wu, X. Urbanization, socioeconomic status and health disparity in China. Health Place 2016, 42, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A. Spatial analysis of disparities in LDL-C testing for older diabetic adults: A socio-environmental framework focusing on race, poverty, and health access in Mississippi. Appl. Geogr. 2014, 55, 248–256. [Google Scholar] [CrossRef]
- Wang, L. Unequal spatial accessibility of integration-promoting resources and immigrant health: A mixed-methods approach. Appl. Geogr. 2018, 92, 140–149. [Google Scholar] [CrossRef]
- Zhang, W.; Wu, Y. Individual educational attainment, neighborhood-socioeconomic contexts, and self-rated health of middle-aged and elderly Chinese: Exploring the mediating role of social engagement. Health Place 2017, 44, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Gulliford, M.; Morgan, M. Access to Health Care; Routledge: London, UK, 2003. [Google Scholar]
- Jacobs, B.; Ir, P.; Bigdeli, M.; Annear, P.L.; Van Damme, W. Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012, 27, 288–300. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Appl. Geogr. 2014, 54, 182–188. [Google Scholar] [CrossRef]
- Yin, C.; He, Q.; Liu, Y.; Chen, W.; Gao, Y. Inequality of public health and its role in spatial accessibility to medical facilities in China. Appl. Geogr. 2018, 92, 50–62. [Google Scholar] [CrossRef]
- Pei, X.; Rodriguez, E. Provincial income inequality and self-reported health status in China during 1991–1997. J. Epidemiol. Community Health 2006, 60, 1065–1069. [Google Scholar] [CrossRef]
- Yip, W.C.; Hsiao, W.C.; Chen, W.; Hu, S.; Ma, J.; Maynard, A. Early appraisal of Chinas huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef]
- Ding, M.; Zhang, X.; Liu, G. Research on the Reform of Social Governance of China, 1st ed.; China Economic Publishing House: Beijing, China, 2009; pp. 52–54. (In Chinese) [Google Scholar]
- Mertha, A.C. Chinas “Soft” centralization: Shifting Tiao/Kuai authority relations. China Q. 2005, 184, 791–810. Available online: https://www.cambridge.org/core/journals/china-quarterly/article/chinas-soft-centralization-shifting-tiaokuai-authority-relations/70295A675B87106E598FB0F9864A75EC (accessed on 19 July 2019). [CrossRef]
- Nundy, M. Transformation of health insurance schemes in China: Lessons for access. China Rep. 2014, 50, 31–43. [Google Scholar] [CrossRef]
- Jin, J.; Wang, J.; Ma, X.; Wang, Y.; Li, R. Equality of medical health resource allocation in China based on the Gini coefficient method. Iran. J. Public Health 2015, 44, 445–457. [Google Scholar] [PubMed]
- Sun, J.; Luo, H. Evaluation on equality and efficiency of health resources allocation and health services utilization in China. Int. J. Equity Health 2017, 16, 127. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Xu, Y.; Ren, J.; Sun, L.; Liu, C. Inequality in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef] [PubMed]
- Cowell, F.A. Estimation of inequality indices. In Handbook of Income Inequality Measurement; Springer: Dordrecht, The Netherlands, 1999; pp. 123–143. [Google Scholar]
- Cowell, F.A.; Kuga, K. Additivity and the entropy concept: An axiomatic approach to inequality measurement. J. Econ. Theory 1981, 25, 131–143. Available online: https://www.sciencedirect.com/science/article/pii/002205318190020X (accessed on 27 July 2004). [CrossRef]
- Toyoda, T. Inequalities of income distributions: Their comparisons and inequality measures. Kokumin Keizai 1975, 134, 15–41. [Google Scholar]
- Jansen, P.W.; Mensah, F.K.; Nicholson, J.M.; Wake, M. Family and neighbourhood socioeconomic inequalities in childhood trajectories of BMI and overweight: Longitudinal study of Australian children. PLoS ONE 2013, 8, e69676. [Google Scholar] [CrossRef]
- Jenkins, S.P. Estimation and Interpretation of Measures of Inequality, Poverty, and Social Welfare Using Stata. North American Stata Users’ Group Meetings 2006. 2008. Available online: https://ideas.repec.org/p/boc/asug06/16.html (accessed on 10 July 2019).
- World Bank Poverty Manual—pofunmare.files.wordpress.com. Available online: https://pofunmare.files.wordpress.com/2015/08/world-bank-poverty-manual.pdf (accessed on 11 July 2019).
- Biewen, M.; Jenkins, S.P. Variance estimation for generalized entropy and Atkinson inequality indices: The complex survey data case*. Oxf. Bull. Econ. Stat. 2006, 68, 371–383. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1468-0084.2006.00166.x (accessed on 10 July 2019). [CrossRef]
- Ma, J.; Lu, M.; Quan, H. From a national, centrally planned health system to a system based on the market: Lessons from China. Health Aff. 2008, 27, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Haughton, H.; Khandker, S. Handbook on Poverty and Inequality; The World Bank: Washington, DC, USA, 2009; ISBN 9780821376133. Available online: http://siteresources.worldbank.org/INTPA/Resources/429966-1259774805724/Poverty_Inequality_Handbook_FrontMatter.pdf (accessed on 11 July 2019).
- Zhu, J.S. Breaking down the institutional barriers for the allocation of medical resources guided by medical insurance. China Health Insur. 2017, 12, 12–15. Available online: http://www.cqyuzhong.com/UploadFile/news/20172915113140738.pdf (accessed on 9 July 2019). (In Chinese).
- Xue, D. Defect and improvement of the administration management in health care system: From the perspective of medical resource allocation efficiency and equity. Chin. Hosp. Manag. 2013, 33, 1–3. (In Chinese) [Google Scholar]
- Kanbur, R. Chapter 13 Income distribution and development. In Handbook of Income Distribution; Elsevier: Amsterdam, The Netherlands, 2000; pp. 791–841. [Google Scholar]
- Wang, X.; Wei, W.; Ma, C.; Zhou, D.; Wang, S.; Feng, Z. Reasons and destination features of medical personnel flow in township hospitals in Hubei province. Chin. J. Public Health 2014, 30, 1312–1314. Available online: http://html.rhhz.net/ZGGGWS/html/20141025.htm (accessed on 11 July 2019). (In Chinese).
- Wu, S.; Liu, X.; Jiang, X.; Huang, Q.; Yuan, Z. Turnover of healthcare technical personnel in township health centers of Jangxi province. Chin. J. Public Health 2017, 33, 1048–1050. Available online: http://html.rhhz.net/ZGGGWS/html/20170704.htm (accessed on 12 July 2019). (In Chinese).
- Gu, X. The transformation in public finance and the return of government’s responsibility for healthcare financing. Soc. Sci. China 2010, 2010, 103–120. Available online: http://kns.cnki.net.eproxy.lib.hku.hk//KXReader/Detail?TIMESTAMP=636983844539036250&DBCODE=CJFD&TABLEName=CJFD2010&FileName=ZSHK201002008&RESULT=1&SIGN=tc%2f3JUXxGx69%2blzA7b1AUvGpsEo%3d (accessed on 10 July 2019). (In Chinese).
- Du, C.; Zhu, H.P. The evolutionary logic in urban China’s healthcare and medical system. Soc. Sci. China 2016, 2016, 66–89. Available online: http://big5.oversea.cnki.net.eproxy.lib.hku.hk/kcms/detail/detail.aspx?dbCode=cjfd&QueryID=37&CurRec=4&filename=ZSHK201608004&dbname=CJFDLAST2016&uid=WEEvREcwSlJHSldRa1Fhb09jT0pjQnpiNUFtQmhqUmRVTkNNcDR2eVkrdz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4IQMovwHtwkF4VYPoHbKxJw!! (accessed on 10 July 2019). (In Chinese).
- Yu, Y.X.; Yang, D.K. Theoretical and empirical research on equity of healthcare resource allocation in China. Reform Econ. Syst. 2008, 2008, 160–163. Available online: http://www.cqvip.com/qk/91904x/200806/29122406.html (accessed on 12 June 2019). (In Chinese).
- Wu, S.; Fu, Y.; Shen, H.; Liu, F. Using ranked weights and Shannon entropy to modify regional sustainable society index. Sustain. Cities Soc. 2018, 41, 443–448. Available online: https://www.sciencedirect.com/science/article/pii/S2210670717312441 (accessed on 23 May 2019). [CrossRef]


| Variable Details in Equation (1) | Category | Data Source |
|---|---|---|
| y: 379 Ailibi 3A hospital score | Ailibi-2016-ranking | |
| var1: No. of total staff (person) | Hospitals’ official websites. For missing information and data, we visit other websites such as www.haodf.com and https://www.jobmd.cn/ | |
| var2: city2016 permanent population (unit: 10,000 person) | China City Statistical Yearbook 2017 | |
| var3: city 2016 disposable income (yuan) | ||
| var4: ownership |
| Hospitals’ official websites |
| var5: medical treatment style |
| Hospitals’ official websites |
| var6: church & charity initiated |
| Hospitals’ official websites |
| var7: university affiliation |
| Hospitals’ official websites |
| var8: NHFPC direct administration |
| NHFPC website |
| var9: provincial HFPC direct administration |
| Websites of the Health and Family Planning Commission of each province |
| var10: municipality HFPC direct administration |
| http://wjw.beijing.gov.cn/ http://wsjk.tj.gov.cn/html/wsjn/portal/index/index.htm http://wsjkw.sh.gov.cn/index.html http://wsjkw.cq.gov.cn/ |
| var11: prefecture bureau of Health and Family Planning Commission administration |
| Authors’ summary |
| var12: military affiliation |
| https://www.yaofangwang.com/yiyuan/ |
| var13: city administrative level |
| China City Statistical Yearbook 2017 |
| Linear regression Number of obs = 368 F(21, 346) = 29.16 Prob > F = 0.0000 R-squared = 0.5959 Root MSE = 115.83 Robust | |||||
|---|---|---|---|---|---|
| y | Standard Error | t | P > t | (95% Confidence Interval) | |
| var1 | 0.0436 | 0.0080 | 5.50 | 0.000 *** | 0.0280–0.0592 |
| var2 | 0.0356 | 0.0203 | 1.75 | 0.081 * | −0.0044–0.0755 |
| var3 | 0.0042 | 0.0008 | 5.39 | 0.000 *** | 0.0027–0.0058 |
| var4 = 1 | 105.3848 | 32.6609 | 3.23 | 0.001 *** | 41.1459–169.6237 |
| var5 = | |||||
| 2 | −105.664 | 18.3378 | −5.76 | 0.000 *** | −141.7317–−69.5964 |
| 3 | −142.515 | 40.0669 | −3.56 | 0.000 *** | −221.3204–−63.7096 |
| var6 = 1 | 44.8862 | 16.5621 | 2.71 | 0.007 *** | 12.3111–77.4613 |
| var12 = 1 | 171.0338 | 59.9637 | 2.85 | 0.005 *** | 53.0946–288.9731 |
| var9 = 1 | 23.8974 | 32.1457 | 0.74 | 0.458 | −39.3281–87.1230 |
| var10 = 1 | 13.3541 | 38.2681 | 0.35 | 0.727 | −61.9132–88.6215 |
| var8 * var7 | |||||
| 0 1 | −94.1936 | ||||
| 1 0 | 60.0584 | 34.6160 | −2.72 | 0.007 *** | −162.278–−26.1093 |
| 1 1 | 0 (omitted) | 38.9043 | 1.54 | 0.124 | −16.4603–136.577 |
| var11 * var7 | |||||
| 0 1 | −67.3168 | ||||
| 1 0 | 159.3906 | 32.0474 | −2.10 | 0.036 * | −130.3491–−4.2845 |
| 1 1 | 0 (omitted) | 39.2444 | 4.06 | 0.000 *** | 82.2029–236.5783 |
| var13 * var7 | |||||
| 1 1 | 257.8345 | 64.8942 | 3.97 | 0.000 *** | 130.1978–385.4712 |
| 2 0 | 59.5823 | 59.4744 | 1.00 | 0.317 | −57.3946–176.5593 |
| 2 1 | 283.7637 | 72.0074 | 3.94 | 0.000 *** | 142.1364–425.391 |
| 3 0 | −24.1865 | 66.7344 | −0.36 | 0.717 | −155.4427–107.0697 |
| 3 1 | 300.5646 | 96.5215 | 3.11 | 0.002 *** | 110.7219–490.4072 |
| 4 0 | −25.5099 | 65.3923 | −0.39 | 0.697 | −154.1263–103.1066 |
| 4 1 | 270.0733 | 80.1628 | 3.37 | 0.001 *** | 112.4057–427.741 |
| _cons | 63.0924 | 77.3488 | 0.82 | 0.415 | −89.0406–215.2255 |
| City’s Aggregated 3-A Hospital Score | Average 3-A Hospitals Score Per 10,000 People | |||||
|---|---|---|---|---|---|---|
| Ranking | City Name | City Administrative Level | Province | City Name | City Administrative Level | Province |
| 1 | Beijing | Municipality | Beijing | Xining | Provincial capital | Qinghai |
| 2 | Guangzhou | Provincial capital | Guangdong | Urumqi | Autonomous capital | Xinjiang |
| 3 | Shanghai | Municipality | Shanghai | Nanchang | Provincial capital | Jiangxi |
| 4 | Nanjing | Provincial capital | Jiangsu | Nanjing | Provincial capital | Jiangsu |
| 5 | Wuhan | Provincial capital | Hubei | Taiyuan | Provincial capital | Shanxi |
| 6 | Xi’an | Provincial capital | Shaanxi | Shenyang | Provincial capital | Liaoning |
| 7 | Hangzhou | Provincial capital | Zhejiang | Xi’an | Provincial capital | Shaanxi |
| 8 | Shenyang | Provincial capital | Liaoning | Lhasa | Autonomous capital | Tibet |
| 9 | Chengdu | Provincial capital | Sichuan | Beijing | Municipality | Beijing |
| 10 | Harbin | Provincial capital | Heilongjiang | Guangzhou | Provincial capital | Guangdong |
| Grouping at City Level N = Observation, aw: Analytical Weight | Theil’s L GE(0) | Theil’s T GE(1) |
|---|---|---|
| City (N = 308, aw: city population) | 0.337 | 0.330 |
| Subgroups by city administrative level (N = 308, aw: city population) | Theil’s L GE(0) | Theil’s T GE(1) |
| 2-Provincial capital 3-Sub-provincial leveled city 4-Prefecture | 0.055 0.091 0.184 | 0.052 0.098 0.175 |
| GE_W(α) GE_B(α) | 47.52% 52.47% | 35.93% 64.07% |
| 32 Provinces | GE(0) | GE(1) | 7 Regions | GE(0) | GE(1) | 3 Zones | GE(0) | GE(1) |
|---|---|---|---|---|---|---|---|---|
| Total | 0.34 | 0.32 | Total | 0.34 | 0.32 | Total | 0.34 | 0.32 |
| 1-Heilongjiang | 0.28 | 0.18 | 1-NE | 0.32 | 0.25 | 1-Eastern China | 0.28 | 0.27 |
| 2-Jilin | 0.38 | 0.32 | 2-NC | 0.39 | 0.36 | 2-Central China | 0.37 | 0.35 |
| 3-Liaoning | 0.30 | 0.27 | 3-EC | 0.25 | 0.25 | 3-Western China | 0.37 | 0.38 |
| 4-Beijing | 0 | 0 | 4-CC | 0.38 | 0.38 | |||
| 5-Tianjin | 0 | 0 | 5-SC | 0.26 | 0.26 | |||
| 6-Hebei | 0.18 | 0.15 | 6-SW | 0.28 | 0.28 | |||
| 7-Shanxi | 0.43 | 0.47 | 7-NW | 0.42 | 0.37 | |||
| 8-Inner Mongolia | 0.34 | 0.36 | ||||||
| 9-Shanghai | 0 | 0 | ||||||
| 10-Jiangsu | 0.37 | 0.36 | ||||||
| 11-Zhejiang | 0.19 | 0.21 | ||||||
| 12-Anhui | 0.19 | 0.18 | Note: 1-NE comprises provinces No. 1~3; 2-NC comprises provinces No. 4~8; 3-EC comprises provinces No. 9~14; 4-CC comprises provinces No. 15~18; 5-SC comprises provinces No. 19~21; 6-SW comprises provinces No. 22~26; 7-NW comprises provinces No. 27~32. | Note: 1-Eastern China comprises provinces No. 3, 4, 5, 6, 9, 10, 11, 13, 14, 19, 20 and 21; 2-Central China comprises provinces No. 1, 2, 8, 12, 15, 16, 17 and 18; 3-Western China comprises provinces No. 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 and 32. | ||||
| 13-Fujian | 0.27 | 0.26 | ||||||
| 14-Shandong | 0.18 | 0.18 | ||||||
| 15-Henan | 0.35 | 0.30 | ||||||
| 16-Hubei | 0.34 | 0.32 | ||||||
| 17-Hunan | 0.26 | 0.28 | ||||||
| 18-Jiangxi | 0.52 | 0.57 | ||||||
| 19-Guangdong | 0.24 | 0.26 | ||||||
| 20-Hainan | 0.002 | 0.002 | ||||||
| 21-Guangxi | 0.27 | 0.25 | ||||||
| 22-Chongqing | 0 | 0 | ||||||
| 23-Sichuan | 0.28 | 0.26 | ||||||
| 24-Guizhou | 0.41 | 0.46 | ||||||
| 25-Yunnan | 0.31 | 0.34 | ||||||
| 26-Tibet | 0 | 0 | ||||||
| 27-Shaanxi | 0.43 | 0.39 | ||||||
| 28-Gansu | 0.33 | 0.34 | ||||||
| 29-Qinghai | 0 | 0 | ||||||
| 30-Ningxia | 0 | 0 | ||||||
| 31-Xinjiang | 0.43 | 0.33 | ||||||
| 32-XPCC | 0 | 0 | ||||||
| GE_W() GE_B() | 80.36% 19.64% | 76.13% 23.87% | GE_W() GE_B() | 92.82% 7.18% | 92.52% 7.47% | GE_W() GE_B() | 97.43% 2.56% | 97.35% 2.65% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, M.; He, S.; Wu, D.; Zhu, H.; Webster, C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. Int. J. Environ. Res. Public Health 2019, 16, 2813. https://doi.org/10.3390/ijerph16162813
Yu M, He S, Wu D, Zhu H, Webster C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. International Journal of Environmental Research and Public Health. 2019; 16(16):2813. https://doi.org/10.3390/ijerph16162813
Chicago/Turabian StyleYu, Meng, Shenjing He, Dunxu Wu, Hengpeng Zhu, and Chris Webster. 2019. "Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China" International Journal of Environmental Research and Public Health 16, no. 16: 2813. https://doi.org/10.3390/ijerph16162813
APA StyleYu, M., He, S., Wu, D., Zhu, H., & Webster, C. (2019). Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. International Journal of Environmental Research and Public Health, 16(16), 2813. https://doi.org/10.3390/ijerph16162813






