Risk Factors for Acute Rheumatic Fever: Literature Review and Protocol for a Case-Control Study in New Zealand
Abstract
:1. Introduction
2. Epidemiology and Impact of ARF in New Zealand
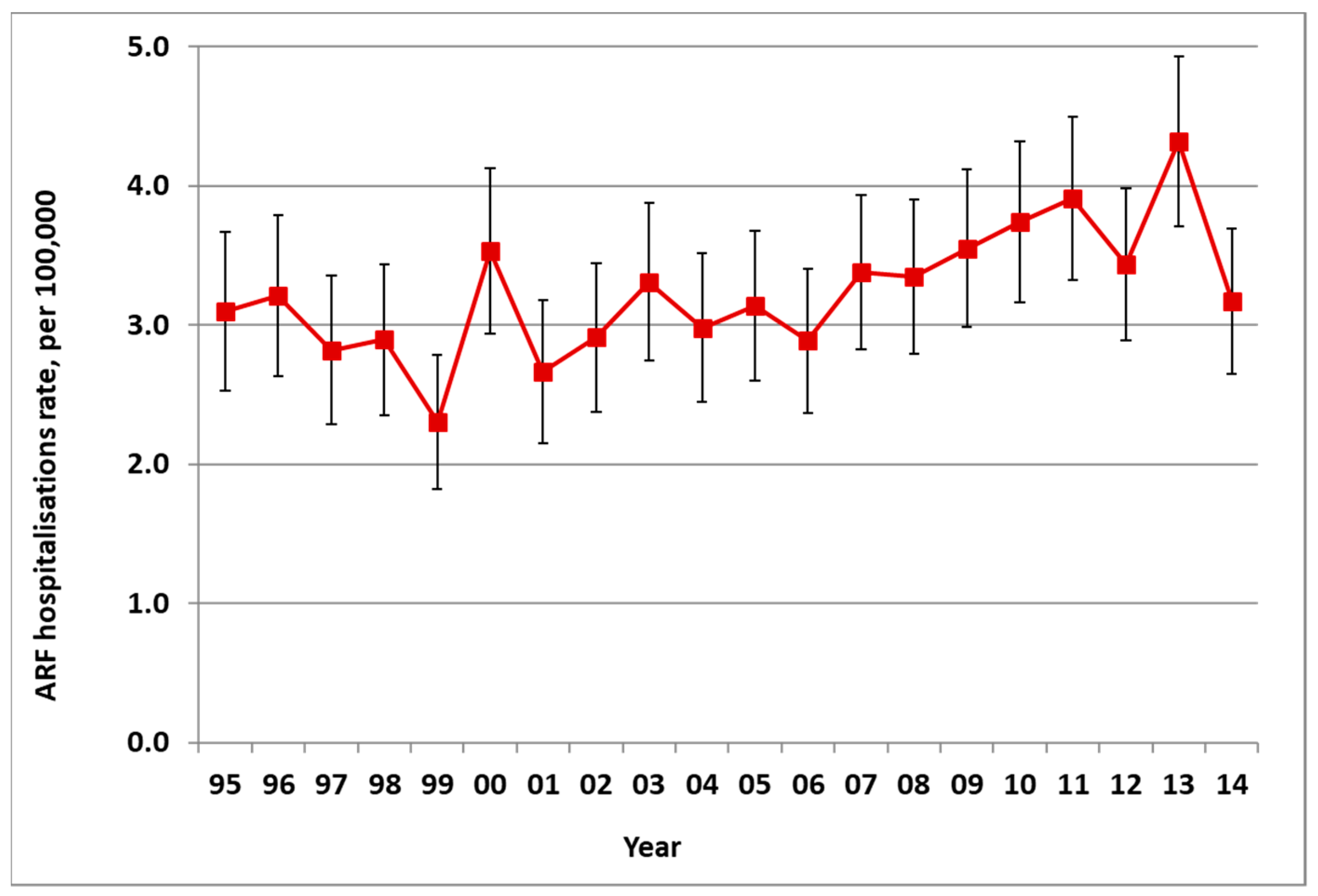
2.1. Incidence of ARF
2.2. Distribution of ARF
2.2.1. Geographic Distribution
2.2.2. Age and Sex Distribution
2.2.3. Ethnic Distribution
2.2.4. Distribution by Deprivation
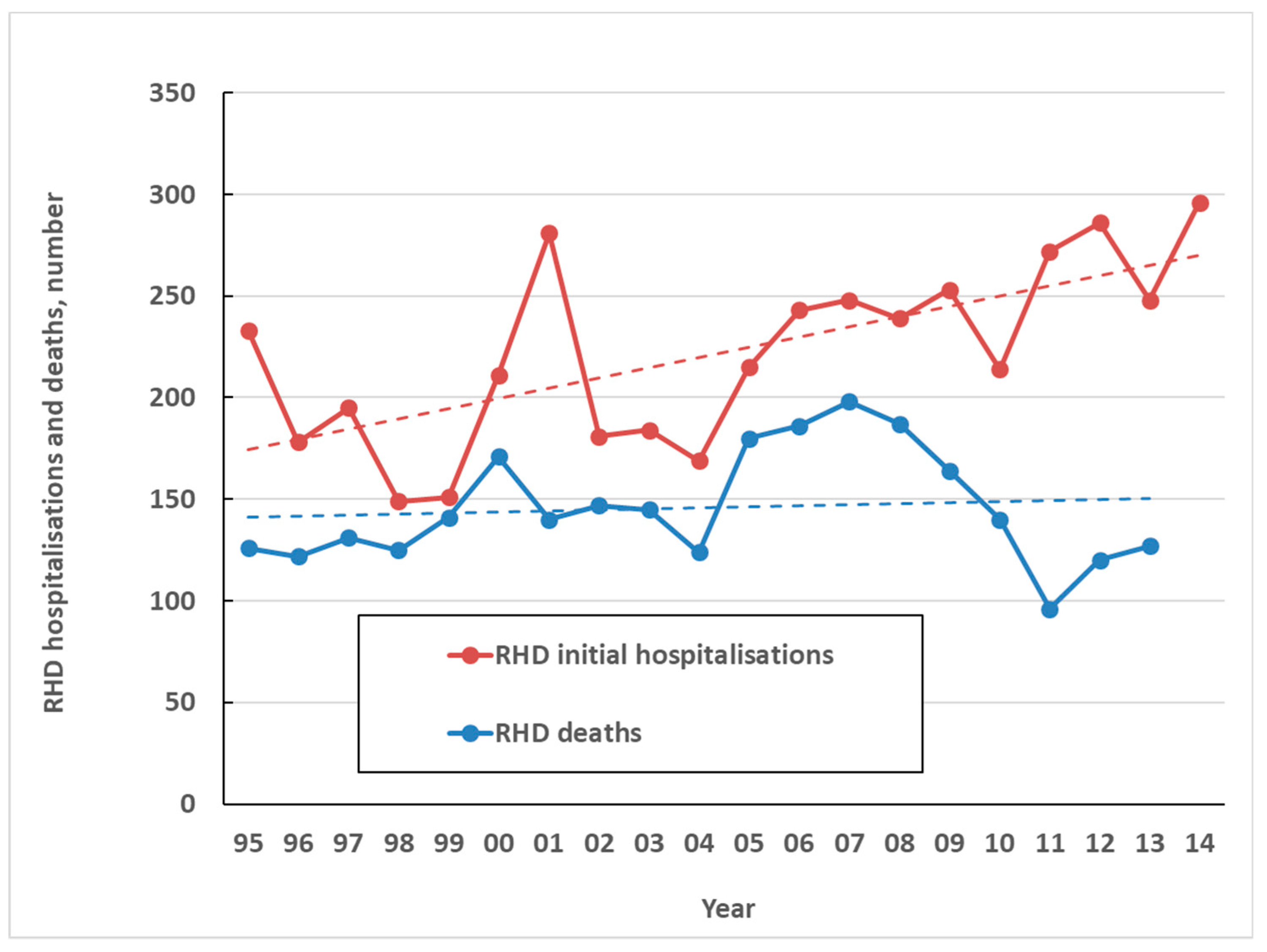
2.3. Impact on RHD, RHD Mortality and Healthcare Costs
3. Existing Knowledge about Risk and Protective Factors for ARF and RHD
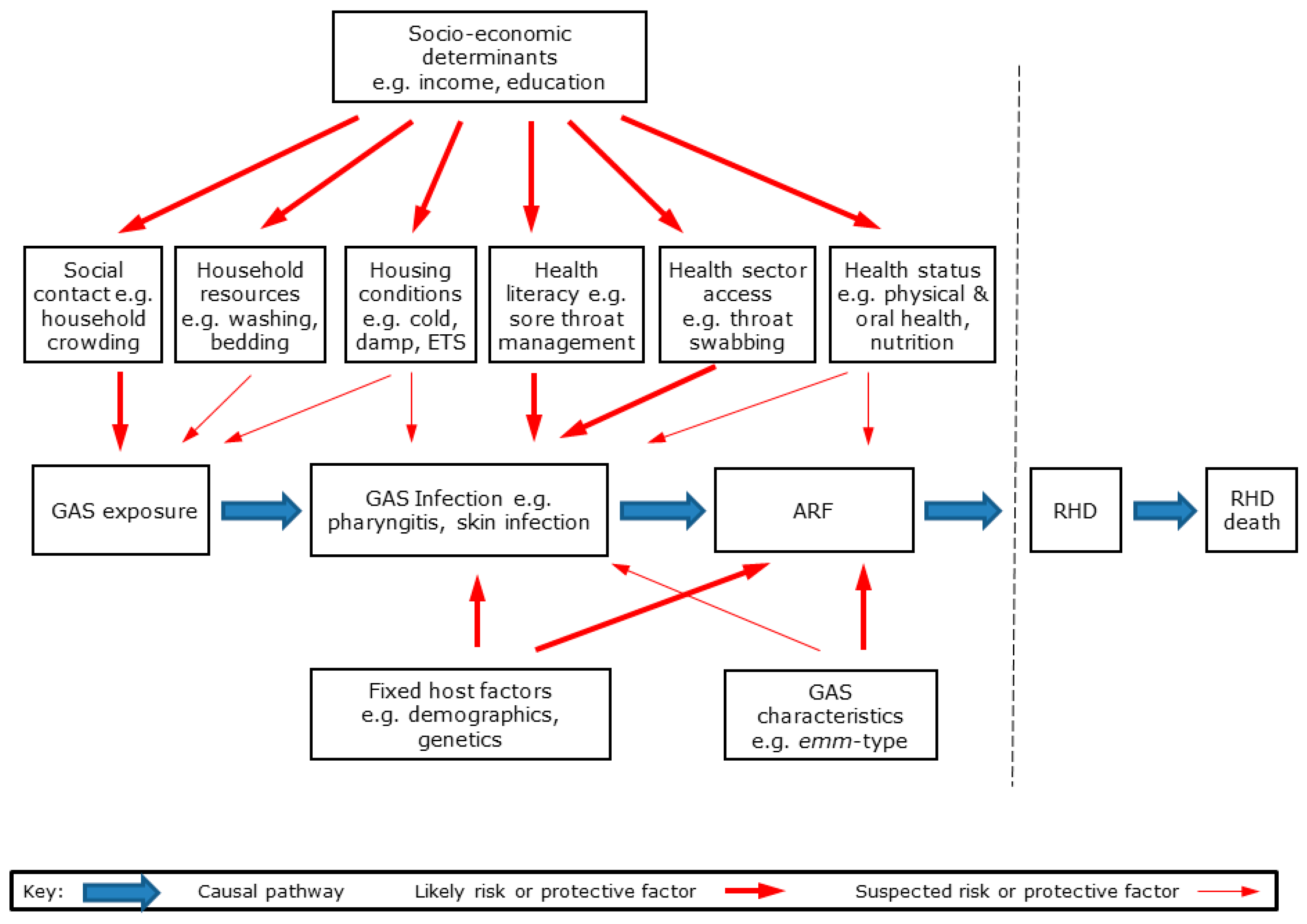
3.1. Causal Pathway for GAS Exposure, ARF and RHD
- Preceding GAS infections of throat and skin, which may initiate ARF;
- Environmental risk factors, notably the number of social contacts, household crowding and bed sharing, household resources, including those for washing, teeth cleaning, and laundry, housing conditions, including damp, and cold, environmental tobacco smoke (ETS) exposure, exposure to biting insects and skin injuries;
- Healthcare factors, notably health literacy and healthcare access;
- Health and nutrition factors, including health status, oral health status and services, nutrition;
- Social determinants, including income, education and housing tenure;
- Predisposing host factors, including demographic, inherited and early development;
- Organism factors, including molecular typing data.
3.2. Knowledge of Risk and Protective Factors for ARF from Previous Epidemiological Studies
3.3. Preceding GAS Infection of Throat and Skin as the Initiator of ARF
3.4. Environmental Risk Factors for ARF
3.4.1. Number of Social Contacts
3.4.2. Household Crowding, Including Bed Sharing
3.4.3. Household Resources, including those for Washing and Laundry
3.4.4. Housing Conditions, including Tenure, Damp and Cold
3.4.5. Environmental Tobacco Smoke Exposure
3.4.6. Exposure to Animals, Biting Insects and Skin Injuries
3.5. Healthcare Access and Risk of ARF
3.5.1. Health Literacy
3.5.2. Healthcare Access
3.6. Health Status, Nutrition and Risk of ARF
3.6.1. Health Status
3.6.2. Oral Health Status and Services
3.6.3. Nutrition
3.7. Wider Modifiable Social Determinants, including Income and Education
3.8. Predisposing Host Factors that Are Inherited or Act during Early Development
3.8.1. Demographic Risk Factors
3.8.2. Ancestry and Genetic Factors
3.8.3. Pregnancy and Birth
3.8.4. Autoimmunity
3.9. Organism Factors, including Infectious Co-Factors
3.9.1. Exposure to Group A Streptococcus (GAS)
3.9.2. Exposure to Potential Infectious Co-factors
4. Study Aims and Research Questions
- Identify potentially modifiable environmental risk factors for ARF, notably household crowding and bed-sharing, poor housing conditions, and ETS.
- Establish whether access to healthcare, including sore throat treatment and related health literacy, is protective for ARF.
- Establish whether current or recent skin infection is associated with an increased risk of ARF.
- Establish whether poor oral health is associated with an increased risk of ARF.
- Identify potentially modifiable host and nutritional factors for ARF, such as vitamin D deficiency, anaemia and high consumption of sugar-sweetened beverages.
- Contribute to identifying immunological factors associated with an increased risk of ARF.
- Establish whether a positive family history and the HLA-DRB1 locus or other plausible genetic markers are associated with ARF.
- Establish whether specific GAS organisms are associated with ARF.
- Are there modifiable environmental exposures contributing to an increased risk of ARF, notably household crowding, bed sharing, poor indoor environments (e.g., cold, damp, mouldy), fuel poverty, tobacco smoke exposure, limited resources for washing and teeth cleaning, inadequate protection from insect bites and fleas?
- Are there modifiable host and nutritional factors contributing to an increased risk of ARF, notably vitamin D deficiency, high consumption of sugar-sweetened beverages, low consumption of fruit and vegetables?
- Is ARF associated with skin infections, which might suggest the need to treat such infections as part of ARF prevention programmes?
- Are there knowledge, attitudes and behaviours associated with a decreased risk of ARF, notably health literacy around treatment of sore throats and skin infections?
- Is good access to health services protective for ARF?
- Is there a large proportion of ARF cases with a history of sore throat who did not receive treatment for this, suggesting the potential for improved pharyngitis treatment?
- Is participating in school-based sore throat management programme protective of ARF?
- Does the distribution of GAS emm-types that we observe to be associated with ARF differ from those emm-types circulating in the wider child population?
- Are there specific immunological markers of increased susceptibility to ARF?
- Is family history of ARF/RHD a risk factor for ARF?
- Do environmental exposures interact with inherited factors (e.g., HLA-DRB1 locus) in a non-additive (multiplicative) way to explain disease distribution?
5. Study Design
5.1. Study Population
5.2. Cases
5.2.1. Case Recruitment
5.2.2. Case Inclusion and Exclusion Criteria
5.2.3. Case Review
5.3. Controls
5.3.1. Matched Controls
5.3.2. Community Controls
6. Data Sources and Specimen Collection
6.1. Study Questionnaire
6.1.1. Content
6.1.2. Pre-testing and Pilot Testing
6.1.3. Selection of Proxy Interview Subject for Children
6.1.4. Selection of Housing Environment for Children
6.1.5. Selection of Time-period
6.1.6. Household Composition
6.2. Biological Specimens
6.3. Linked Health Information
6.4. Data Collection
6.4.1. Interviewer Selection, Training and Quality Assurance
6.4.2. Interviews
6.4.3. Specimen Collection
6.4.4. Specimen Storage
6.5. Steering Committees and Ethical Review
7. Data Analysis
7.1. Approach to Data Analysis
7.1.1. Descriptive Analysis
7.1.2. Primary Exposure Analysis
7.1.3. Secondary Exposure Analysis
7.1.4. Population Attributable Fraction (PAF)
7.2. Study Sample and Power
7.3. Study Operation
8. Dissemination
9. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- New Zealand Ministry of Health. Progress on the Better Public Services Rheumatic Fever Target Wellington. Available online: http://www.health.govt.nz/about-ministry/what-we-do/strategic-direction/betterpublic-services/progress-better-public-services-rheumatic-fever-target (accessed on 9 April 2017).
- Carapetis, J.R.; Zuhlke, L.J. Global research priorities in rheumatic fever and rheumatic heart disease. Ann. Pediatric Cardiol. 2011, 4, 4–12. [Google Scholar] [CrossRef]
- Health Research Council of New Zealand. Rheumatic Fever Research Partnership; Health Research Council of New Zealand: Auckland, New Zealand, 2013.
- Allison, V.D.; Gunn, W. The Epidemiology of Streptococcal Infections. Proc. R. Soc. Med. 1932, 25, 927–944. [Google Scholar] [CrossRef]
- Carapetis, J.R.; Beaton, A.; Cunningham, M.W.; Guilherme, L.; Karthikeyan, G.; Mayosi, B.M.; Sable, C.; Steer, A.; Wilson, N.; Wyber, R.; et al. Acute rheumatic fever and rheumatic heart disease. Nat. Rev. Dis. Primers 2016, 2, 15084. [Google Scholar] [CrossRef] [PubMed]
- Bright, P.D.; Mayosi, B.M.; Martin, W.J. An immunological perspective on rheumatic heart disease pathogenesis: More questions than answers. Heart 2016, 102, 1527–1532. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.R.; Voss, L.M.; Walker, S.J.; Lennon, D. Acute rheumatic fever in Auckland, New Zealand: Spectrum of associated group A streptococci different from expected. Pediatric Infect. Dis. J. 1994, 13, 264–269. [Google Scholar] [CrossRef] [PubMed]
- McDonald, M.; Currie, B.J.; Carapetis, J.R. Acute rheumatic fever: A chink in the chain that links the heart to the throat? Lancet Infect. Dis. 2004, 4, 240–245. [Google Scholar] [CrossRef]
- Parks, T.; Smeesters, P.R.; Steer, A.C. Streptococcal skin infection and rheumatic heart disease. Curr. Opin. Infect. Dis. 2012, 25, 145–153. [Google Scholar] [CrossRef]
- Lennon, D.; Stewart, J.; Farrell, E.; Palmer, A.; Mason, H. School-based prevention of acute rheumatic fever: A group randomized trial in New Zealand. Pediatric Infect. Dis. J. 2009, 28, 787–794. [Google Scholar] [CrossRef]
- O’Sullivan, L.; Moreland, L.J.; Webb, R.H.; Upton, A.; Wilson, N.J. Acute rheumatic fever following Group a Steptococcus pyoderma and Group G Streptococcus pharyngitis. Pediatric Infect. Dis. J. 2017, 34, 692–694. [Google Scholar] [CrossRef]
- Kaplan, M.H.; Bolande, R.; Rakita, L.; Blair, J. Presence of Bound Immunoglobulins and Complement in the Myocardium in Acute Rheumatic Fever. Association with Cardiac Failure. N. Engl. J. Med. 1964, 271, 637–645. [Google Scholar] [CrossRef]
- Saphir, O. The Aschoff nodule. Am. J. Clin. Pathol. 1959, 31, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.; Kosanke, S.; Terrence Dunn, S.; Jankelow, D.; Duran, C.M.; Cunningham, M.W. Pathogenic mechanisms in rheumatic carditis: Focus on valvular endothelium. J. Infect. Dis. 2001, 183, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Lennon, D.R. Acute Rheumatic Fever. In Feigin & Cherry’s Textbook of Pediatric Infectious Diseases, 7th ed.; Cherry, J., Demmler-Harrison, G.J., Kaplan, S.L., Steinbach, W.J., Hotez, P., Eds.; Saunders: Philadelphia, PA, USA, 2013; Volume 1, pp. 401–418. [Google Scholar]
- Spinetto, H.; Lennon, D.; Horsburgh, M. Rheumatic fever recurrence prevention: A nurse-led programme of 28-day penicillin in an area of high endemnicity. J. Paediatr. Child Health 2011, 47, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Bryant, P.A.; Robins-Browne, R.; Carapetis, J.R.; Curtis, N.; Bryant, P.A.; Robins-Browne, R.; Carapetis, J.R.; Curtis, N. Some of the people, some of the time: Susceptibility to acute rheumatic fever. Circulation 2009, 119, 742–753. [Google Scholar] [CrossRef]
- Thornley, C.; McNicholas, A.; Baker, M.; Lennon, D. Rheumatic fever registers in New Zealand. N. Z. Public Health Rep. 2001, 8, 41–44. [Google Scholar]
- Watkins, D.A.; Johnson, C.O.; Colquhoun, S.M.; Karthikeyan, G.; Beaton, A.; Bukhman, G.; Forouzanfar, M.H.; Longenecker, C.T.; Mayosi, B.M.; Mensah, G.A.; et al. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015. N. Engl. J. Med. 2017, 377, 713–722. [Google Scholar] [CrossRef]
- Steer, A.C. Historical aspects of rheumatic fever. J. Paediatr. Child Health 2015, 51, 21–27. [Google Scholar] [CrossRef]
- Milne, R.J.; Lennon, D.R.; Stewart, J.M.; Vander Hoorn, S.; Scuffham, P.A. Incidence of acute rheumatic fever in New Zealand children and youth. J. Paediatr. Child Health 2012, 48, 685–691. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Rheumatic Heart Disease and Acute Rheumatic Fever in Australia: 1996–2012. Cardiovascular Disease Series. Cat. No. CVD 60; Australian Institute of Health and Welfare: Canberra, Australia, 2013.
- Jaine, R.; Baker, M.; Venugopal, K. Epidemiology of acute rheumatic fever in New Zealand 1996–2005. J. Paediatr. Child Health 2008, 44, 564–571. [Google Scholar] [CrossRef]
- Webb, R.; Wilson, N. Rheumatic fever in New Zealand. J. Paediatr. Child Health 2013, 49, 179–184. [Google Scholar] [CrossRef]
- Oliver, J.; Pierse, N.; Baker, M.G. Estimating rheumatic fever incidence in New Zealand using multiple data sources. Epidemiol. Infect. 2015, 143, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.K.; Stanley, J.; Baker, M.G.; Wilson, N.J.; Sarfati, D. Estimating the risk of acute rheumatic fever in New Zealand by age, ethnicity and deprivation. Epidemiol. Infect. 2016, 144, 3058–3067. [Google Scholar] [CrossRef] [PubMed]
- Siriett, V.; Crengle, S.; Lennon, D.; Stonehouse, M.; Cramp, G. The epidemiology of rheumatic fever in the Tairawhiti/Gisborne region of New Zealand: 1997–2009. N. Z. Med. J. 2012, 125, 8–15. [Google Scholar] [PubMed]
- Robin, A.; Mills, C.; Tuck, R.; Lennon, D. The epidemiology of acute rheumatic fever in Northland, 2002–2011. N. Z. Med. J. 2013, 126, 46–52. [Google Scholar] [PubMed]
- Pennock, V.; Bell, A.; Moxon, T.A.; Reed, P.; Maxwell, F.; Lennon, D. Retrospective epidemiology of acute rheumatic fever: A 10-year review in the Waikato District Health Board area of New Zealand. N. Z. Med. J. 2014, 127, 26–37. [Google Scholar] [PubMed]
- Moxon, T.A.; Reed, P.; Jelleyman, T.; Anderson, P.; Leversha, A.; Jackson, C.; Lennon, D. Is a rheumatic fever register the best surveillance tool to evaluate rheumatic fever control in the Auckland region? N. Z. Med. J. 2017, 130, 48–62. [Google Scholar] [PubMed]
- Baker, M.G.; Telfar Barnard, L.; Kvalsvig, A.; Verrall, A.; Zhang, J.; Keall, M.; Wilson, N.; Wall, T.; Howden-Chapman, P. Increasing incidence of serious infectious diseases and inequalities in New Zealand: A national epidemiological study. Lancet 2012, 379, 1112–1119. [Google Scholar] [CrossRef]
- New Zealand Ministry of Health. HISO 10001:2017 Ethnicity Data Protocols; Ministry of Health: Wellington, New Zealand, 2017.
- Atkinson, J.; Salmond, C.; Crampton, P. NZDep2013 Index of Deprivation; Department of Public Health, University of Otago: Wellington, New Zealand, 2014. [Google Scholar]
- Salmond, C.E.; Crampton, P. Development of New Zealand’s deprivation index (NZDep) and its uptake as a national policy tool. Can. J. Public Health 2012, 103 (Suppl. 2), 7–11. [Google Scholar]
- Milne, R.J.; Lennon, D.; Stewart, J.M.; Vander Hoorn, S.; Scuffham, P.A. Mortality and hospitalisation costs of rheumatic fever and rheumatic heart disease in New Zealand. J. Paediatr. Child Health 2012, 48, 692–697. [Google Scholar] [CrossRef]
- Oliver, J.; Pierse, N.; Baker, M.G. Improving rheumatic fever surveillance in New Zealand: Results of a surveillance sector review. BMC Public Health 2014, 14, 528. [Google Scholar] [CrossRef]
- Kerdemelidis, M.; Lennon, D.R.; Arroll, B.; Peat, B.; Jarman, J. The primary prevention of rheumatic fever. J. Paediatr. Child Health 2010, 46, 534–548. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, P.M.; Pereira, R.R.; Guilherme, L. Understanding rheumatic fever. Rheumatol. Int. 2012, 32, 1113–1120. [Google Scholar] [CrossRef] [PubMed]
- Entine, M. A survey of dental diseases as a diagnostic aid in rheumatic fever. J. Am. Dent. Assoc. 1949, 38, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Grave, P.E. Social and environmental factors in the aetiology of rheumatic fever. Med. J. Aust. 1957, 44, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Coburn, A.F. The concept of egg yolk as a dietary inhibitor to rheumatic susceptibility. Lancet 1960, 1, 867–870. [Google Scholar] [CrossRef]
- Adanja, B.; Vlajinac, H.; Jarebinski, M. Socioeconomic factors in the etiology of rheumatic fever. J. Hyg. Epidemiol. Microbiol. Immunol. 1988, 32, 329–335. [Google Scholar]
- Vlajinac, H.; Adanja, B.; Jarebinski, M. Socio-economic factors and rheumatic fever occurrence. Differences between patients with and without frequent sore throat. J. Hyg. Epidemiol. Microbiol. Immunol. 1989, 33, 471–476. [Google Scholar]
- Bahr, G.M.; Eales, L.J.; Nye, K.E.; Majeed, H.A.; Yousof, A.M.; Behbehani, K.; Rook, G.A. An association between Gc (vitamin D-binding protein) alleles and susceptibility to rheumatic fever. Immunology 1989, 67, 126–128. [Google Scholar]
- Vlajinac, H.; Adanja, B.; Marinkovic, J.; Jarebinski, M. Influence of socio-economic and other factors on rheumatic fever occurrence. Eur. J. Epidemiol. 1991, 7, 702–704. [Google Scholar] [CrossRef]
- Adanja, B.J.; Vlajinac, H.D.; Marinkovic, J.P.; Jarebinski, M.S. Rheumatic fever and diet. Isr. J. Med. Sci. 1991, 27, 161–163. [Google Scholar]
- Thomas, D.R.; Salmon, R.L.; Kench, S.M.; Meadows, D.; Coleman, T.J.; Morgan-Capner, P.; Morgan, K.L. Zoonotic illness—Determining risks and measuring effects: Association between current animal exposure and a history of illness in a well characterised rural population in the UK. J. Epidemiol. Community Health 1994, 48, 151–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaman, M.M.; Yoshiike, N.; Chowdhury, A.H.; Jalil, M.Q.; Mahmud, R.S.; Faruque, G.M.; Rouf, M.A.; Haque, K.M.; Tanaka, H. Socio-economic deprivation associated with acute rheumatic fever. A hospital-based case-control study in Bangladesh. Paediatr. Perinat. Epidemiol. 1997, 11, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Zaman, M.M.; Yoshiike, N.; Chowdhury, A.H.; Nakayama, T.; Yokoyama, T.; Faruque, G.M.; Rouf, M.A.; Haque, S.; Tanaka, H. Nutritional factors associated with rheumatic fever. J. Trop. Pediatric 1998, 44, 142–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaman, M.M.; Yoshiike, N.; Rouf, M.A.; Haque, S.; Chowdhury, A.H.; Nakayama, T.; Tanaka, H. Association of rheumatic fever with serum albumin concentration and body iron stores in Bangladeshi children: Case-control study. BMJ 1998, 317, 1287–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berdeli, A.; Celik, H.A.; Ozyurek, R.; Aydin, H.H. Involvement of immunoglobulin FcgammaRIIA and FcgammaRIIIB gene polymorphisms in susceptibility to rheumatic fever. Clin. Biochem. 2004, 37, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Berdeli, A.; Celik, H.A.; Ozyurek, R.; Dogrusoz, B.; Aydin, H.H. TLR-2 gene Arg753Gln polymorphism is strongly associated with acute rheumatic fever in children. J. Mol. Med. 2005, 83, 535–541. [Google Scholar] [CrossRef]
- Berdeli, A.; Tabel, Y.; Celik, H.A.; Ozyurek, R.; Dogrusoz, B.; Aydin, H.H. Lack of association between TNF α gene polymorphism at position-308 and risk of acute rheumatic fever in Turkish patients. Scand. J. Rheumatol. 2006, 35, 44–47. [Google Scholar] [CrossRef]
- Kurahara, D.K.; Grandinetti, A.; Galario, J.; Reddy, D.V.; Tokuda, A.; Langan, S.; Tanabe, B.; Yamamoto, K.S.; Yamaga, K.M.; Kurahara, D.K.; et al. Ethnic differences for developing rheumatic fever in a low-income group living in Hawaii. Ethn. Dis. 2006, 16, 357–361. [Google Scholar]
- Hounie, A.G.; Pauls, D.L.; do Rosario-Campos, M.C.; Mercadante, M.T.; Diniz, J.B.; De Mathis, M.A.; De Mathis, M.E.; Chacon, P.; Shavitt, R.G.; Curi, M.; et al. Obsessive-compulsive spectrum disorders and rheumatic fever: A family study. Biol. Psychiatry 2007, 61, 266–272. [Google Scholar] [CrossRef]
- Seixas, A.A.; Hounie, A.G.; Fossaluza, V.; Curi, M.; Alvarenga, P.G.; De Mathis, M.A.; De Mathis, M.E.; Vallada, H.; Pauls, D.; de Braganca Pereira, C.A.; et al. Anxiety disorders and rheumatic Fever: Is there an association? CNS Spectr. 2008, 13, 1039–1046. [Google Scholar] [CrossRef]
- Messias-Reason, I.J.; Schafranski, M.D.; Kremsner, P.G.; Kun, J.F. Ficolin 2 (FCN2) functional polymorphisms and the risk of rheumatic fever and rheumatic heart disease. Clin. Exp. Immunol. 2009, 157, 395–399. [Google Scholar] [CrossRef]
- Walker, K.G.; Cooper, M.; McCabe, K.; Hughes, J.; Mathiassen, W.; Lawrenson, J.; Wilmshurst, J.M. Markers of susceptibility to acute rheumatic fever: The B-cell antigen D8/17 is not robust as a marker in South Africa. Cardiol. Young 2011, 21, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Col-Araz, N.; Pehlivan, S.; Baspinar, O.; Oguzkan-Balci, S.; Sever, T.; Balat, A. Role of cytokine gene (IFN-gamma, TNF-alpha, TGF-beta1, IL-6, and IL-10) polymorphisms in pathogenesis of acute rheumatic fever in Turkish children. Eur. J. Pediatric 2012, 171, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Riaz, B.K.; Selim, S.; Karim, M.N.; Chowdhury, K.N.; Chowdhury, S.H.; Rahman, M.R. Risk factors of rheumatic heart disease in Bangladesh: A case-control study. J. Health Popul. Nutr. 2013, 31, 70–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thornley, S.; Marshall, R.J.; Bach, K.; Koopu, P.; Reynolds, G.; Sundborn, G.; Ei, W.L. Sugar, dental caries and the incidence of acute rheumatic fever: A cohort study of Maori and Pacific children. J. Epidemiol. Community Health 2017, 71, 364–370. [Google Scholar] [CrossRef]
- Thornley, S.; Marshall, R.; Jarrett, P.; Sundborn, G.; Reynolds, E.; Schofield, G. Scabies is strongly associated with acute rheumatic fever in a cohort study of Auckland children. J. Paediatr. Child Health 2018, 54, 625–632. [Google Scholar] [CrossRef]
- McLaren, M.J.; Hawkins, D.M.; Koornhof, H.J.; Bloom, K.R.; Bramwell-Jones, D.M.; Cohen, E.; Gale, G.E.; Kanarek, K.; Lachman, A.S.; Lakier, J.B.; et al. Epidemiology of rheumatic heart disease in black shcoolchildren of Soweto, Johannesburg. BMJ 1975, 3, 474–478. [Google Scholar] [CrossRef] [Green Version]
- Caughey, D.E.; Douglas, R.; Wilson, W.; Hassall, I.B. HL-A antigens in Europeans and Maoris with rheumatic fever and rheumatic heart disease. J. Rheumatol. 1975, 2, 319–322. [Google Scholar]
- Anabwani, G.M.; Amoa, A.B.; Muita, A.K. Epidemiology of rheumatic heart disease among primary school children in western Kenya. Int. J. Cardiol. 1989, 23, 249–252. [Google Scholar] [CrossRef]
- Coggon, D.; Barker, D.J.; Inskip, H.; Wield, G. Housing in early life and later mortality. J. Epidemiol. Community Health 1993, 47, 345–348. [Google Scholar] [CrossRef] [Green Version]
- Longo-Mbenza, B.; Bayekula, M.; Ngiyulu, R.; Kintoki, V.E.; Bikangi, N.F.; Seghers, K.V.; Lukoki, L.E.; Mandundu, M.F.; Manzanza, M.; Nlandu, Y. Survey of rheumatic heart disease in school children of Kinshasa town. Int. J. Cardiol. 1998, 63, 287–294. [Google Scholar] [CrossRef]
- Oli, K.; Porteous, J. Prevalence of rheumatic heart disease among school children in Addis Ababa. East Afr. Med. J. 1999, 76, 601–605. [Google Scholar] [PubMed]
- Rizvi, S.F.; Khan, M.A.; Kundi, A.; Marsh, D.R.; Samad, A.; Pasha, O. Status of rheumatic heart disease in rural Pakistan. Heart 2004, 90, 394–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, H.T.; Tsai, C.H.; Tsai, F.J. Association between angiotensin I-converting enzyme gene insertion/deletion polymorphism and risk of rheumatic heart disease. Jpn. Heart J. 2004, 45, 949–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steer, A.C.; Kado, J.; Wilson, N.; Tuiketei, T.; Batzloff, M.; Waqatakirewa, L.; Mulholland, E.K.; Carapetis, J.R. High prevalence of rheumatic heart disease by clinical and echocardiographic screening among children in Fiji. J. Heart Valve Dis. 2009, 18, 327–336. [Google Scholar] [PubMed]
- Azevedo, P.M.; Bauer, R.; Caparbo Vde, F.; Silva, C.A.; Bonfa, E.; Pereira, R.M. Interleukin-1 receptor antagonist gene (IL1RN) polymorphism possibly associated to severity of rheumatic carditis in a Brazilian cohort. Cytokine 2010, 49, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.; Ramakrishnan, S.; Roy, A.; Seth, S.; Krishnan, A.; Misra, P.; Kalaivani, M.; Bhargava, B.; Flather, M.D.; Poole-Wilson, P.P. Prevalence and outcome of subclinical rheumatic heart disease in India: The RHEUMATIC (Rheumatic Heart Echo Utilisation and Monitoring Actuarial Trends in Indian Children) study. Heart 2011, 97, 2018–2022. [Google Scholar] [CrossRef]
- Ba-Saddik, I.A.; Munibari, A.A.; Al-Naqeeb, M.S.; Parry, C.M.; Hart, C.A.; Cuevas, L.E.; Coulter, J.B.S. Prevalence of rheumatic heart disease among school-children in Aden, Yemen. Ann. Trop. Paediatr. 2011, 31, 37–46. [Google Scholar] [CrossRef]
- Dobson, J.; Steer, A.C.; Colquhoun, S.; Kado, J. Environmental factors and rheumatic heart disease in Fiji. Pediatric Cardiol. 2012, 33, 332–336. [Google Scholar] [CrossRef]
- Okello, E.; Kakande, B.; Sebatta, E.; Kayima, J.; Kuteesa, M.; Mutatina, B.; Nyakoojo, W.; Lwabi, P.; Mondo, C.K.; Odoi-Adome, R.; et al. Socioeconomic and environmental risk factors among rheumatic heart disease patients in Uganda. PLoS ONE 2012, 7, e43917. [Google Scholar] [CrossRef] [Green Version]
- Eriksson, J.G.; Kajantie, E.; Phillips, D.I.; Osmond, C.; Thornburg, K.L.; Barker, D.J. The developmental origins of chronic rheumatic heart disease. Am. J. Hum. Biol. 2013, 25, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Rehman, S.; Akhtar, N.; Saba, N.; Munir, S.; Ahmed, W.; Mohyuddin, A.; Khanum, A. A study on the association of TNF-α (−308), IL-6 (−174), IL-10 (−1082) and IL-1Ra(VNTR) gene polymorphisms with rheumatic heart disease in Pakistani patients. Cytokine 2013, 61, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Mirabel, M.; Fauchier, T.; Bacquelin, R.; Tafflet, M.; Germain, A.; Robillard, C.; Rouchon, B.; Marijon, E.; Jouven, X. Echocardiography screening to detect rheumatic heart disease: A cohort study of schoolchildren in French Pacific Islands. Int. J. Cardiol. 2015, 188, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, P.M.; Merriman, T.R.; Topless, R.K.; Wilson, N.J.; Crengle, S.; Lennon, D.R. Association study involving polymorphisms in IL-6, IL-1RA, and CTLA4 genes and rheumatic heart disease in New Zealand population of Maori and Pacific ancestry. Cytokine 2016, 85, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Gray, L.A.; D’Antoine, H.A.; Tong, S.Y.C.; McKinnon, M.; Bessarab, D.; Brown, N.; Remenyi, B.; Steer, A.; Syn, G.; Blackwell, J.M.; et al. Genome-wide analysis of genetic risk factors for rheumatic heart disease in Aboriginal Australians provides support for pathogenic molecular mimicry. J. Infect. Dis. 2017, 216, 1460–1470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parks, T.; Mirabel, M.M.; Kado, J.; Auckland, K.; Nowak, J.; Rautanen, A.; Mentzer, A.J.; Marijon, E.; Jouven, X.; Perman, M.L.; et al. Association between a common immunoglobulin heavy chain allele and rheumatic heart disease risk in Oceania. Nat. Commun. 2017, 8, 14946. [Google Scholar] [CrossRef] [PubMed]
- Gordis, L.; Lilienfeld, A.; Rodriguez, R. Studies in the epidemiology and preventability of rheumatic fever. II. Socio-economic factors and the incidence of acute attacks. J. Chronic Dis. 1969, 21, 655–666. [Google Scholar] [CrossRef]
- Jaine, R.; Baker, M.; Venugopal, K. Acute rheumatic fever associated with household crowding in a developed country. Pediatric Infect. Dis. J. 2011, 30, 315–319. [Google Scholar] [CrossRef]
- Dajani, A.S. Current status of nonsuppurative complications of group A streptococci. Pediatric Infect. Dis. J. 1991, 10, 25–27. [Google Scholar] [CrossRef]
- Catanzaro, F.J.; Rammelkamp, C.H., Jr.; Chamovitz, R. Prevention of rheumatic fever by treatment of streptococcal infections. II. Factors responsible for failures. N. Engl. J. Med. 1958, 259, 53–57. [Google Scholar] [CrossRef]
- McDonald, M.I.; Towers, R.J.; Andrews, R.M.; Benger, N.; Currie, B.J.; Carapetis, J.R. Low rates of streptococcal pharyngitis and high rates of pyoderma in Australian aboriginal communities where acute rheumatic fever is hyperendemic. Clin. Infect. Dis. 2006, 43, 683–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, A.C.; Mahe, A.; Hay, R.J.; Andrews, R.M.; Steer, A.C.; Tong, S.Y.; Carapetis, J.R. The Global Epidemiology of Impetigo: A Systematic Review of the Population Prevalence of Impetigo and Pyoderma. PLoS ONE 2015, 10, e0136789. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; Smeesters, P.R.; Steer, A.C.; Steemson, J.D.; Ng, A.C.; Proft, T.; Fraser, J.D.; Baker, M.G.; Morgan, J.; Carter, P.E.; et al. M-Protein Analysis of Streptococcus pyogenes Isolates Associated with Acute Rheumatic Fever in New Zealand. J. Clin. Microbiol. 2015, 53, 3618–3620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Sullivan, C.E.; Baker, M.G.; Zhang, J. Increasing hospitalizations for serious skin infections in New Zealand children, 1990–2007. Epidemiol. Infect. 2011, 139, 1794–1804. [Google Scholar] [CrossRef] [Green Version]
- Tupai-Firestone, R.; Tsai, J.Y.; Anderson, P.; Broome, L.; McKee, T.; Lennon, D.R. Antimicrobial stewardship using pharmacy data for the nurse-led school-based clinics in Counties Manukau District Health Board for management of group A streptococcal pharyngitis and skin infection. N. Z. Med. J. 2016, 129, 29–38. [Google Scholar]
- Anderson, P.; King, J.; Moss, M.; Light, P.; McKee, T.; Farrell, E.; Stewart, J.; Lennon, D. Nurse-led school-based clinics for rheumatic fever prevention and skin infection management: Evaluation of Mana Kidz programme in Counties Manukau. N. Z. Med. J. 2016, 129, 37–46. [Google Scholar]
- O’Sullivan, C.E.; Baker, M.G. Proposed epidemiological case definition for serious skin infection in children. J. Paediatr. Child Health 2010, 46, 176–183. [Google Scholar] [CrossRef]
- Romani, L.; Steer, A.C.; Whitfeld, M.J.; Kaldor, J.M. Prevalence of scabies and impetigo worldwide: A systematic review. Lancet Infect. Dis. 2015, 15, 960–967. [Google Scholar] [CrossRef]
- Fischer, K.; Holt, D.; Currie, B.; Kemp, D. Scabies: Important clinical consequences explained by new molecular studies. Adv. Parasitol. 2012, 79, 339–373. [Google Scholar]
- Richardson, M.; Elliman, D.; Maguire, H.; Simpson, J.; Nicoll, A. Evidence base of incubation periods, periods of infectiousness and exclusion policies for the control of communicable diseases in schools and preschools. Pediatric Infect. Dis. J. 2001, 20, 380–391. [Google Scholar] [CrossRef]
- Danchin, M.H.; Rogers, S.; Kelpie, L.; Selvaraj, G.; Curtis, N.; Carlin, J.B.; Nolan, T.M.; Carapetis, J.R. Burden of acute sore throat and group A streptococcal pharyngitis in school-aged children and their families in Australia. Pediatrics 2007, 120, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, C. Evolution: The Triumph of an Idea; HarperCollins: New York, NY, USA, 2001; Volume 1. [Google Scholar]
- Stolleman, G.H. Factors determining the attack rate of rheumatic fever. JAMA 1961, 177, 823–828. [Google Scholar] [CrossRef]
- Schneider, W.F.; Chapman, S.; Schulz, V.B.; Krause, R.M.; Lancefield, R.C. Prevention of streptococcal pharyngitis among military personnel and their civilian dependents by mass prophylaxis. N. Engl. J. Med. 1964, 270, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Gray, G.C.; Callahan, J.D.; Hawksworth, A.W.; Fisher, C.A.; Gaydos, J.C. Respiratory diseases among US military personnel: Countering emerging threats. Emerg. Infect. Dis. 1999, 5, 379. [Google Scholar] [CrossRef]
- Baker, M.; McNicholas, A.; Garrett, N.; Jones, N.; Stewart, J.; Koberstein, V.; Lennon, D. Household crowding a major risk factor for epidemic meningococcal disease in Auckland children. Pediatric Infect. Dis. J. 2000, 19, 983–990. [Google Scholar] [CrossRef]
- Grant, C.C.; Emery, D.; Milne, T.; Coster, G.; Forrest, C.B.; Wall, C.R.; Scragg, R.; Aickin, R.; Crengle, S.; Leversha, A.; et al. Risk factors for community-acquired pneumonia in pre-school-aged children. J. Paediatr. Child Health 2012, 48, 402–412. [Google Scholar] [CrossRef]
- Baker, M.; Das, D.; Venugopal, K.; Howden-Chapman, P. Tuberculosis associated with household crowding in a developed country. J. Epidemiol. Community Health 2008, 62, 715–721. [Google Scholar] [CrossRef]
- Ransome, O.J.; Roode, H.; Spector, I.; Reinach, S.G. Pharyngeal carriage of group A beta-haemolytic streptococci in coloured and Indian schoolchildren. S. Afr. Med. J. 1983, 64, 779–781. [Google Scholar]
- Nandi, S.; Kumar, R.; Ray, P.; Vohra, H.; Ganguly, N.K. Group A streptococcal sore throat in a periurban population of northern India: A one-year prospective study. Bull. World Health Organ. 2001, 79, 528–533. [Google Scholar]
- Tay, L.; Chay, S.O. A three-year streptococcal survey among Singapore school children. Part I—Carriership of streptococci. Ann. Acad. Med. Singap. 1981, 10, 14–24. [Google Scholar]
- Faruq, Q.O.; Rashid, A.K.; Ahmed, J.; Waiz, A.; Haque, K.M.; Rouf, M.A.; Khan, S.M.; Khan, T.N. Prevalence of streptococcal sorethroat in the school children of Dhaka. Bangladesh Med. Res. Counc. Bull. 1995, 21, 87–94. [Google Scholar] [PubMed]
- Likitnukul, S.; Prapphal, N.; Tatiyakavee, K.; Nunthapisud, P.; Chumdermpadetsuk, S. Risk factors of streptococcal colonization in school age children. Southeast Asian J. Trop. Med. Public Health 1994, 25, 664–671. [Google Scholar] [PubMed]
- Spitzer, J.; Hennessy, E.; Neville, L. High group A streptococcal carriage in the Orthodox Jewish community of north Hackney. Br. J. Gen. Pract. 2001, 51, 101–105. [Google Scholar] [PubMed]
- McDonald, M.I.; Towers, R.J.; Andrews, R.; Benger, N.; Fagan, P.; Currie, B.J.; Carapetis, J.R. The dynamic nature of group A streptococcal epidemiology in tropical communities with high rates of rheumatic heart disease. Epidemiol. Infect. 2008, 136, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Oliver, J.R.; Pierse, N.; Stefanogiannis, N.; Jackson, C.; Baker, M.G. Acute rheumatic fever and exposure to poor housing conditions in New Zealand: A descriptive study. J. Paediatr. Child Health 2017, 53, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Schwebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bygdeman, S.; Jacobsson, E.; Myrback, K.E.; Wallmark, G. Hemolytic streptococci among infants in a maternity department. Report of an outbreak. Scand. J. Infect. Dis. 1978, 10, 45–49. [Google Scholar] [CrossRef]
- Claesson, B.E.; Claesson, U.L. An outbreak of endometritis in a maternity unit caused by spread of group A streptococci from a showerhead. J. Hosp. Infect. 1985, 6, 304–311. [Google Scholar] [CrossRef]
- Wagenvoort, J.H.; Penders, R.J.; Davies, B.I.; Lutticken, R. Similar environmental survival patterns of Streptococcus pyogenes strains of different epidemiologic backgrounds and clinical severity. Eur. J. Clin. Microbiol. Infect. Dis. 2005, 24, 65–67. [Google Scholar] [CrossRef]
- Luby, S.P.; Agboatwalla, M.; Feikin, D.R.; Painter, J.; Billhimer, W.; Altaf, A.; Hoekstra, R.M. Effect of handwashing on child health: A randomised controlled trial. Lancet 2005, 366, 225–233. [Google Scholar] [CrossRef]
- Carapetis, J.R.; Johnston, F.; Nadjamerrek, J.; Kairupan, J. Skin sores in Aboriginal children. J. Paediatr. Child Health 1995, 31, 563. [Google Scholar] [CrossRef] [PubMed]
- Buckett, N.R.; Marston, N.J.; Saville-Smith, K.; Jowett, J.H.; Jones, M.S. Preliminary BRANZ 2010 House Condition Survey Report, 2nd ed.; BRANZ Study Report 240; BRANZ: Porirua, New Zealand, 2011. [Google Scholar]
- Rushdy, A.A.; Cooke, R.P.; Iversen, A.M.; Pickering, B.J. Boarding school outbreak of group A streptococcal pharyngitis. Commun. Dis. Rep. CDR Rev. 1995, 5, 106–108. [Google Scholar]
- Shorter, C.; Crane, J.; Pierse, N.; Barnes, P.; Kang, J.; Wickens, K.; Douwes, J.; Stanley, T.; Taubel, M.; Hyvarinen, A.; et al. Indoor visible mold and mold odor are associated with new-onset childhood wheeze in a dose-dependent manner. Indoor Air 2018, 28, 6–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pierse, N.; Arnold, R.; Keall, M.; Howden-Chapman, P.; Crane, J.; Cunningham, M.; Heating, H.; Health Study Group. Modelling the effects of low indoor temperatures on the lung function of children with asthma. J. Epidemiol. Community Health 2013, 67, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Craig, E.; Anderson, P.; Jackson, G.; Jackson, C. Measuring potentially avoidable and ambulatory care sensitive hospitalisations in New Zealand children using a newly developed tool. N. Z. Med. J. 2012, 125, 38–50. [Google Scholar] [PubMed]
- Vanker, A.; Gie, R.P.; Zar, H.J. The association between environmental tobacco smoke exposure and childhood respiratory disease: A review. Expert Rev. Respir. Med. 2017, 11, 661–673. [Google Scholar] [CrossRef]
- Brook, I. The impact of smoking on oral and nasopharyngeal bacterial flora. J. Dent. Res. 2011, 90, 704–710. [Google Scholar] [CrossRef]
- Greene, C.E. Infectious Diseases of the Dog and Cat, 4th ed.; Elsevier/Saunders: St Louis, MO, USA, 2013. [Google Scholar]
- Biberstein, E.L.; Brown, C.; Smith, T. Serogroups and biotypes among beta-hemolytic streptococci of canine origin. J. Clin. Microbiol. 1980, 11, 558–561. [Google Scholar]
- Pichichero, M.E.; Casey, J.R. Systematic review of factors contributing to penicillin treatment failure in Streptococcus pyogenes pharyngitis. JAMA Otolaryngol. Head Neck Surg. 2007, 137, 851–857. [Google Scholar] [CrossRef]
- Falck, G. Group A streptococci in household pets’ eyes—A source of infection in humans? Scand. J. Infect. Dis. 1997, 29, 469–471. [Google Scholar] [CrossRef]
- Wilson, K.S.; Maroney, S.A.; Gander, R.M. The family pet as an unlikely source of group A beta-hemolytic streptococcal infection in humans. Pediatric Infect. Dis. J. 1995, 14, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Arya, R.K. Awareness about sore-throat, rheumatic fever and rheumatic heart disease in a rural community. Indian J. Public Health 1992, 36, 63–67. [Google Scholar] [PubMed]
- Iyengar, S.D.; Grover, A.; Kumar, R.; Ganguly, N.K.; Wahi, P.L. Participation of health workers, school teachers and pupils in the control of rheumatic fever: Evaluation of a training programme. Indian Pediatric 1992, 29, 875–881. [Google Scholar]
- Harre, N.; Thomas, D.; Brown, K.; Raza, F.; Lennon, D. Communicating information about sore throats and rheumatic fever to South Auckland high-school students. N. Z. Med. J. 2000, 113, 215–217. [Google Scholar]
- World Health Organization Technical Report Series. Rheumatic Fever and Rheumatic Heart Disease; Report of a WHO Expert Consultation Geneva, 29 October–1 November 2001; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Robertson, K.A.; Volmink, J.A.; Mayosi, B.M. Towards a uniform plan for the control of rheumatic fever and rheumatic heart disease in Africa—The Awareness Surveillance Advocacy Prevention (A.S.A.P.) Programme. S. Afr. Med. J. 2006, 96, 241. [Google Scholar]
- Allen, L.B.; Allen, M.; Lesa, R.F.; Richardson, G.E.; Eggett, D.L. Rheumatic fever in Samoa: Education as prevention. Pac. Health Dialog 2011, 17, 107–118. [Google Scholar]
- Jack, S.J.; Williamson, D.A.; Galloway, Y.; Pierse, N.; Zhang, J.; Oliver, J.; Milne, R.J.; Mackereth, G.; Jackson, C.M.; Steer, A.C.; et al. Primary prevention of rheumatic fever in the 21st century: Evaluation of a national programme. Int. J. Epidemiol. 2018, 47, 1585–1593. [Google Scholar] [CrossRef]
- Nordet, P.; Lopez, R.; Duenas, A.; Sarmiento, L. Prevention and control of rheumatic fever and rheumatic heart disease: The Cuban experience (1986–1996–2002). Cardiovasc. J. Afr. 2008, 19, 135–140. [Google Scholar]
- Bach, J.F.; Chalons, S.; Forier, E.; Elana, G.; Jouanelle, J.; Kayemba, S.; Delbois, D.; Mosser, A.; Saint-Aime, C.; Berchel, C. 10-year educational programme aimed at rheumatic fever in two French Caribbean islands. Lancet 1996, 347, 644–648. [Google Scholar] [CrossRef]
- Ramsey, L.S.; Watkins, L.; Engel, M.E. Health education interventions to raise awareness of rheumatic fever: A systematic review protocol. Syst. Rev. 2013, 2, 58. [Google Scholar] [CrossRef] [Green Version]
- Chang, C. Cutting edge issues in rheumatic fever. Clin. Rev. Allergy Immunol. 2012, 42, 213–237. [Google Scholar] [CrossRef] [PubMed]
- Andrulis, D.P. Access to care is the centerpiece in the elimination of socioeconomic disparities in health. Ann. Intern. Med. 1998, 129, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Gordis, L. Effectiveness of comprehensive-care programs in preventing rheumatic fever. N. Engl. J. Med. 1973, 289, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Arguedas, A.; Mohs, E. Prevention of rheumatic fever in Costa Rica. J. Pediatric 1992, 121, 569–572. [Google Scholar] [CrossRef]
- Eltohami, E.A.; Hajar, H.A.; Folger, G.M., Jr. Acute rheumatic fever in an Arabian Gulf country—Effect of climate, advantageous socioeconomic conditions, and access to medical care. Angiology 1997, 48, 481–489. [Google Scholar] [CrossRef]
- Jatrana, S.; Crampton, P. Primary health care in New Zealand: Who has access? Health Policy 2009, 93, 1–10. [Google Scholar] [CrossRef]
- Robertson, K.A.; Volmink, J.A.; Mayosi, B.M. Antibiotics for the primary prevention of acute rheumatic fever: A meta-analysis. BMC Cardiovasc. Disord. 2005, 5, 11. [Google Scholar] [CrossRef] [Green Version]
- Spinks, A.; Glasziou, P.P.; Del Mar, C.B. Antibiotics for sore throat. Cochrane Database Syst. Rev. 2013, 11, CD000023. [Google Scholar] [CrossRef] [Green Version]
- Lennon, D.; Anderson, P.; Kerdemelidis, M.; Farrell, E.; Mahi, S.C.; Percival, T.; Jansen, D.; Stewart, J. First Presentation Acute Rheumatic Fever is Preventable in a Community Setting: A School Based Intervention. Pediatric Infect. Dis. J. 2017, 36, 1113–1118. [Google Scholar] [CrossRef]
- el-Daher, N.T.; Hijazi, S.S.; Rawashdeh, N.M.; al-Khalil, I.A.; Abu-Ektaish, F.M.; Abdel-Latif, D.I. Immediate vs. delayed treatment of group A beta-hemolytic streptococcal pharyngitis with penicillin V. Pediatric Infect. Dis. J. 1991, 10, 126–130. [Google Scholar] [CrossRef]
- Pichichero, M.E.; Disney, F.A.; Talpey, W.B.; Green, J.L.; Francis, A.B.; Roghmann, K.J.; Hoekelman, R.A. Adverse and beneficial effects of immediate treatment of Group A beta-hemolytic streptococcal pharyngitis with penicillin. Pediatric Infect. Dis. J. 1987, 6, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.A.; Randolph, M.F.; DeMeo, K.K.; Kaplan, E.L. Lack of impact of early antibiotic therapy for streptococcal pharyngitis on recurrence rates. J. Pediatric 1990, 117, 853–858. [Google Scholar] [CrossRef]
- New Zealand Ministry of Health Progress on the Better Public Services Rheumatic Fever Target. Available online: http://www.health.govt.nz/about-ministry/what-we-do/strategic-direction/better-public-services/progress-better-public-services-rheumatic-fever-target (accessed on 1 April 2017).
- Currie, B.J.; McCarthy, J.S. Permethrin and ivermectin for scabies. N. Engl. J. Med. 2010, 362, 717–725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tasani, M.; Tong, S.Y.; Andrews, R.M.; Holt, D.C.; Currie, B.J.; Carapetis, J.R.; Bowen, A.C. The Importance of Scabies Coinfection in the Treatment Considerations for Impetigo. Pediatric Infect. Dis. J. 2016, 35, 374–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeoh, D.K.; Bowen, A.C.; Carapetis, J.R. Impetigo and scabies—Disease burden and modern treatment strategies. J. Infect. 2016, 72, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Price, W.A. Nutrition and Physical Degeneration: A Comparison of Primitive and Modern Diets and Their Effects, 6th ed.; Keats Publishing: New Canaan, CT, USA, 2003. [Google Scholar]
- Burton, J.P.; Drummond, B.K.; Chilcott, C.N.; Tagg, J.R.; Thomson, W.M.; Hale, J.D.F.; Wescombe, P. Influence of the probiotic Streptococcus salivarius strain M18 on indices of dental health in children: A randomized double-blind, placebo-controlled trial. J. Med. Microbiol. 2013, 62, 875–884. [Google Scholar] [CrossRef]
- Strom, B.L.; Abrutyn, E.; Berlin, J.A.; Kinman, J.L.; Feldman, R.S.; Stolley, P.D.; Levison, M.E.; Korzeniowski, O.M.; Kaye, D. Risk factors for infective endocarditis: Oral hygiene and nondental exposures. Circulation 2000, 102, 2842–2848. [Google Scholar] [CrossRef]
- He, J.; Li, Y.; Cao, Y.; Xue, J.; Zhou, X. The oral microbiome diversity and its relation to human diseases. Folia Microbiol. 2015, 60, 69–80. [Google Scholar] [CrossRef]
- Saiman, L.; Prince, A.; Gersony, W.M. Pediatric infective endocarditis in the modern era. J. Pediatric 1993, 122, 847–853. [Google Scholar] [CrossRef]
- Webb, R.; Voss, L.; Roberts, S.; Hornung, T.; Rumball, E.; Lennon, D. Infective endocarditis in New Zealand children 1994–2012. Pediatric Infect. Dis. J. 2014, 33, 437–442. [Google Scholar] [CrossRef]
- Thornley, S.; Sundborn, G.; Schmidt-Uili, S.M. Rheumatic fever in New Zealand: What are the teeth trying to tell us? Pac. Health Dialog 2014, 20, 7–10. [Google Scholar] [PubMed]
- Chassy, B.M.; Beall, J.R.; Bielawski, R.M.; Porter, E.V.; Donkersloot, J.A. Occurrence and distribution of sucrose-metabolizing enzymes in oral streptococci. Infect. Immun. 1976, 14, 408–415. [Google Scholar] [PubMed]
- Shelburne, S.A.; Keith, D.; Horstmann, N.; Sumby, P.; Davenport, M.T.; Graviss, E.A.; Brennan, R.G.; Musser, J.M. A direct link between carbohydrate utilization and virulence in the major human pathogen group A Streptococcus. Proc. Natl. Acad. Sci. USA 2008, 105, 1698–1703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Congiu, G.; Campus, G.; Luglie, P.F. Early Childhood Caries (ECC) Prevalence and Background Factors: A Review. Oral Health Prev. Dent. 2014, 12, 71–76. [Google Scholar]
- Rafael da Silveira Moreira. Epidemiology of Dental Caries in the World, Oral Health Care—Pediatric, Research, Epidemiology and Clinical Practices; InTech: Rijeka, Croatia, 2012. [Google Scholar]
- Carapetis, J.R.; Steer, A.C.; Mulholland, E.K.; Weber, M. The global burden of group A streptococcal diseases. Lancet Infect. Dis. 2005, 5, 685–694. [Google Scholar] [CrossRef]
- Hewison, M. Vitamin D and immune function: An overview. Proc. Nutr. Soc. 2012, 71, 50–61. [Google Scholar] [CrossRef] [Green Version]
- Nseir, W.; Mograbi, J.; Abu-Rahmeh, Z.; Mahamid, M.; Abu-Elheja, O.; Shalata, A. The association between vitamin D levels and recurrent group A streptococcal tonsillopharyngitis in adults. Int. J. Infect. Dis. 2012, 16, 735–738. [Google Scholar] [CrossRef] [Green Version]
- Reid, D.; Morton, R.; Salkeld, L.; Bartley, J. Vitamin D and tonsil disease--preliminary observations. Int. J. Pediatric Otorhinolaryngol. 2011, 75, 261–264. [Google Scholar] [CrossRef]
- Utter, J.; Denny, S.; Teevale, T.; Peiris-John, R.; Dyson, B. Prevalence and Recent Trends in Overweight, Obesity, and Severe Obesity among New Zealand Adolescents. Child Obes. 2015, 11, 585–589. [Google Scholar] [CrossRef]
- Rajput, N.; Tuohy, P.; Mishra, S.; Smith, A.; Taylor, B. Overweight and obesity in 4-5-year-old children in New Zealand: Results from the first 4 years (2009–2012) of the B4School Check programme. J. Paediatr. Child Health 2015, 51, 334–343. [Google Scholar] [CrossRef]
- Salmond, C.; Crampton, P.; King, P.; Waldegrave, C. NZiDep: A New Zealand index of socioeconomic deprivation for individuals. Soc. Sci. Med. 2006, 62, 1474–1485. [Google Scholar] [CrossRef] [PubMed]
- Vendsborg, P.; Hansen, L.F.; Olesen, K.H. Decreasing incidence of a history of acute rheumatic fever in chronic rheumatic heart disease. Cardiologia 1968, 53, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Gordis, L. The virtual disappearance of rheumatic fever in the United States: Lessons in the rise and fall of disease. T. Duckett Jones memorial lecture. Circulation 1985, 72, 1155–1162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carapetis, J.R. Rheumatic heart disease in Asia. Circulation 2008, 118, 2748–2753. [Google Scholar] [CrossRef] [Green Version]
- Omurzakova, N.A.; Yamano, Y.; Saatova, G.M.; Mirzakhanova, M.I.; Shukurova, S.M.; Kydyralieva, R.B.; Jumagulova, A.S.; Seisenbaev, A.; Nishioka, K.; Nakajima, T. High incidence of rheumatic fever and rheumatic heart disease in the republics of Central Asia. Int. J. Rheum. Dis. 2009, 12, 79–83. [Google Scholar] [CrossRef]
- White, H.; Walsh, W.; Brown, A.; Riddell, T.; Tonkin, A.; Jeremy, R.; Brieger, D.; Zeitz, C.; Kritharides, L. Rheumatic heart disease in indigenous populations. Heart Lung Circ. 2010, 19, 273–281. [Google Scholar] [CrossRef]
- Steer, A.C.; Carapetis, J.R.; Nolan, T.M.; Shann, F. Systematic review of rheumatic heart disease prevalence in children in developing countries: The role of environmental factors. J. Paediatr. Child Health 2002, 38, 229–234. [Google Scholar] [CrossRef]
- Stollerman, G.H. Rheumatic Fever and Streptococcal Infection; Grune & Stratton: New York, NY, USA, 1975. [Google Scholar]
- Coburn, A. Observations on the mechanism of rheumatic fever. Lancet 1936, 228, 1025–1030. [Google Scholar] [CrossRef]
- Engel, M.E.; Stander, R.; Vogel, J.; Adeyemo, A.A.; Mayosi, B.M. Genetic susceptibility to acute rheumatic fever: A systematic review and meta-analysis of twin studies. PLoS ONE 2011, 6, e25326. [Google Scholar] [CrossRef] [Green Version]
- Stanhope, J.M. New Zealand trends in rheumatic fever: 1885–1971. N. Z. Med. J. 1975, 82, 297–299. [Google Scholar]
- Nepom, G.T.; Erlich, H. MHC class-II molecules and autoimmunity. Annu. Rev. Immunol. 1991, 9, 493–525. [Google Scholar] [CrossRef] [PubMed]
- Padyukov, L.; Silva, C.; Stolt, P.; Alfredsson, L.; Klareskog, L. A gene-environment interaction between smoking and shared epitope genes in HLA-DR provides a high risk of seropositive rheumatoid arthritis. Arthritis Rheum. 2004, 50, 3085–3092. [Google Scholar] [CrossRef] [PubMed]
- Too, C.L.; Yahya, A.; Murad, S.; Dhaliwal, J.S.; Larsson, P.T.; Muhamad, N.A.; Abdullah, N.A.; Mustafa, A.N.; Klareskog, L.; Alfredsson, L.; et al. Smoking interacts with HLA-DRB1 shared epitope in the development of anti-citrullinated protein antibody-positive rheumatoid arthritis: Results from the Malaysian Epidemiological Investigation of Rheumatoid Arthritis (MyEIRA). Arthritis Res. Ther. 2012, 14, 89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boechat Nde, O.; Ogusku, M.M.; Boechat, A.L.; Sadahiro, A. Interaction between smoking and HLA-DRB1*04 gene is associated with a high cardiovascular risk in Brazilian Amazon patients with rheumatoid arthritis. PLoS ONE 2012, 7, e41588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, B.A.; Bang, S.Y.; Chowdhury, M.; Lee, H.S.; Kim, J.H.; Charles, P.; Venables, P.; Bae, S.C. Smoking, the HLA-DRB1 shared epitope and ACPA fine-specificity in Koreans with rheumatoid arthritis: Evidence for more than one pathogenic pathway linking smoking to disease. Ann. Rheum. Dis. 2013, 73, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Bang, S.Y.; Lee, H.S.; Lee, K.W.; Bae, S.C. Interaction of HLA-DRB1 *09:01 and *04:05 with Smoking Suggests Distinctive Mechanisms of Rheumatoid Arthritis Susceptibility Beyond the Shared Epitope. J. Rheumatol. 2013, 40, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, H.T.; Labouriau, R.; Jensen, E.S.; Mortensen, P.B.; Schonheyder, H.C. Fetal growth, maternal prenatal smoking, and risk of invasive meningococcal disease: A nationwide case-control study. Int. J. Epidemiol. 2004, 33, 816–820. [Google Scholar] [CrossRef]
- Melville, J.M.; Moss, T.J. The immune consequences of preterm birth. Front. Neurosci. 2013, 7, 79. [Google Scholar] [CrossRef] [Green Version]
- Yuan, W.; Basso, O.; Sorensen, H.T.; Olsen, J. Indicators of fetal growth and infectious disease in childhood—A birth cohort with hospitalization as outcome. Eur. J. Epidemiol. 2001, 17, 829–834. [Google Scholar] [CrossRef]
- Selling, K.E.; Carstensen, J.; Finnstrom, O.; Josefsson, A.; Sydsjo, G. Hospitalizations in adolescence and early adulthood among Swedish men and women born preterm or small for gestational age. Epidemiology 2008, 19, 63–70. [Google Scholar] [CrossRef]
- Mahon, B.E.; Ehrenstein, V.; Norgaard, M.; Pedersen, L.; Rothman, K.J.; Sorensen, H.T. Perinatal risk factors for hospitalization for pneumococcal disease in childhood: A population-based cohort study. Pediatrics 2007, 119, e804–e812. [Google Scholar] [CrossRef] [PubMed]
- Goldacre, M.J.; Wotton, C.J.; Maisonneuve, J.J. Maternal and perinatal factors associated with subsequent meningococcal, Haemophilus or enteroviral meningitis in children: Database study. Epidemiol. Infect. 2014, 142, 371–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, M.W. Rheumatic fever revisited. Nat. Rev. Cardiol. 2014, 11, 123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tandon, R.; Sharma, M.; Chandrashekhar, Y.; Kotb, M.; Yacoub, M.H.; Narula, J. Revisiting the pathogenesis of rheumatic fever and carditis. Nat. Rev. Cardiol. 2013, 10, 171–177. [Google Scholar] [CrossRef]
- Martin, W.J.; Steer, A.C.; Smeesters, P.R.; Keeble, J.; Inouye, M.; Carapetis, J.; Wicks, I.P. Post-infectious group A streptococcal autoimmune syndromes and the heart. Autoimmun. Rev. 2015, 14, 710–725. [Google Scholar] [CrossRef]
- Raynes, J.M.; Frost, H.R.; Williamson, D.A.; Young, P.G.; Baker, E.N.; Steemson, J.D.; Loh, J.M.; Proft, T.; Dunbar, P.R.; Atatoa Carr, P.E.; et al. Serological Evidence of Immune Priming by Group A Streptococci in Patients with Acute Rheumatic Fever. Front. Microbiol. 2016, 7, 1119. [Google Scholar] [CrossRef]
- Gewitz, M.H.; Baltimore, R.S.; Tani, L.Y.; Sable, C.A.; Shulman, S.T.; Carapetis, J.; Remenyi, B.; Taubert, K.A.; Bolger, A.F.; Beerman, L.; et al. Revision of the Jones Criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: A scientific statement from the American Heart Association. Circulation 2015, 131, 1806–1818. [Google Scholar] [CrossRef] [Green Version]
- Shulman, S.T.; Stollerman, G.; Beall, B.; Dale, J.B.; Tanz, R.R. Temporal changes in streptococcal M protein types and the near-disappearance of acute rheumatic fever in the United States. Clin. Infect. Dis. 2006, 42, 441–447. [Google Scholar] [CrossRef] [Green Version]
- Shulman, S.; Bisno, A. Non Suppurative Post Streptococcal Sequelae. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 8th ed.; Bennett, J.E., Dolin, R., Blaser, M.J., Eds.; Elsevier/Saunders: Philadelphia, PA, USA, 2015. [Google Scholar]
- Johnson, D.R.; Stevens, D.L.; Kaplan, E.L. Epidemiologic analysis of group A streptococcal serotypes associated with severe systemic infections, rheumatic fever, or uncomplicated pharyngitis. J. Infect. Dis. 1992, 166, 374–382. [Google Scholar] [CrossRef]
- Carapetis, J.R.; McDonald, M.; Wilson, N.J. Acute rheumatic fever. Lancet 2005, 366, 155–168. [Google Scholar] [CrossRef]
- Erdem, G.; Mizumoto, C.; Esaki, D.; Reddy, V.; Kurahara, D.; Yamaga, K.; Abe, L.; Johnson, D.; Yamamoto, K.; Kaplan, E.L. Group A streptococcal isolates temporally associated with acute rheumatic fever in Hawaii: Differences from the continental United States. Clin. Infect. Dis. 2007, 45, e20–e24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pruksakorn, S.; Sittisombut, N.; Phornphutkul, C.; Pruksachatkunakorn, C.; Good, M.F.; Brandt, E. Epidemiological analysis of non-M-typeable group A Streptococcus isolates from a Thai population in northern Thailand. J. Clin. Microbiol. 2000, 38, 1250–1254. [Google Scholar] [PubMed]
- Williamson, D.A.; Smeesters, P.R.; Steer, A.C.; Morgan, J.; Davies, M.; Carter, P.; Upton, A.; Tong, S.Y.; Fraser, J.; Moreland, N.J. Comparative M-protein analysis of Streptococcus pyogenes from pharyngitis and skin infections in New Zealand: Implications for vaccine development. BMC Infect. Dis. 2016, 16, 561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williamson, D.A.; Ritchie, S.R.; Lennon, D.; Roberts, S.A.; Stewart, J.; Thomas, M.G.; Baker, M.G. Increasing Incidence and Sociodemographic Variation in Community-Onset Staphylococcus Aureus Skin and Soft Tissue Infections in New Zealand Children. Pediatric Infect. Dis. J. 2013, 32, 923–925. [Google Scholar] [CrossRef] [PubMed]
- Olgunturk, R.; Okur, I.; Cirak, M.Y.; Oguz, A.D.; Akalin, N.; Turet, S.; Tunaoglu, S. The role of viral agents in aetiopathogenesis of acute rheumatic fever. Clin. Rheumatol. 2011, 30, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Doyle, H.; Pierse, N.; Tiatia, R.; Williamson, D.; Baker, M.; Crane, J. The effect of the oral probiotic Streptococcus salivarius (K12) on Group A Streptococcus pharyngitis: A pragmatic trial in schools. Pediatric Infect. Dis. J. 2017, 37, 619–623. [Google Scholar] [CrossRef]
- Heart Foundation of New Zealand. New Zealand Guidelines for Rheumatic Fever: Diagnosis, Management and Secondary Prevention of Acute Rheumatic Fever and Rheumatic Heart Disease: 2014 Update; Heart Foundation of New Zealand: Auckland, New Zealand, 2014. [Google Scholar]
- Jack, S.; Moreland, N.J.; Meagher, J.; Fittock, M.; Galloway, Y.; Ralph, A.P. Streptococcal Serology in Acute Rheumatic Fever Patients: Findings from Two High-income, High Burden Settings. Pediatric Infect. Dis. J. 2018, 38, 1–6. [Google Scholar] [CrossRef]
- Burke, R.J.; Chang, C. Diagnostic criteria of acute rheumatic fever. Autoimmun. Rev. 2014, 13, 503–507. [Google Scholar] [CrossRef]
- Dajani, A.S.; Ayoub, E.; Bierman, F.Z. Guidelines for the diagnosis of rheumatic fever: Jones criteria, 1992 update. JAMA 1992, 268, 2069–2073. [Google Scholar] [CrossRef]
- Wilson, N.J.; Voss, L.; Morreau, J.; Stewart, J.; Lennon, D. New Zealand guidelines for the diagnosis of acute rheumatic fever: Small increase in the incidence of definite cases compared to the American Heart Association Jones criteria. N. Z. Med. J. 2013, 126, 50–59. [Google Scholar]
- New Zealand Ministry of Health. Methodology Report 2015/16: New Zealand Health Survey; New Zealand Ministry of Health: Wellington, New Zealand, 2016.
- New Zealand Ministry of Health. New Zealand Health Survey Methodology Report; Ministry of Health: Wellington, New Zealand, 2012.
- Huang, Q.S.; Turner, N.; Baker, M.G.; Williamson, D.A.; Wong, C.; Webby, R.; Widdowson, M.A. Southern Hemisphere Influenza and Vaccine Effectiveness Research and Surveillance. Influenza Respir. Viruses 2015, 9, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Adolescent Health Research Group Youth’12 National Health and Wellbeing Survey of New Zealand Secondary School Students: Questionnaire. Available online: https://www.fmhs.auckland.ac.nz/assets/fmhs/faculty/ahrg/docs/youth12-questionnaire.pdf (accessed on 31 March 2017).
- Kelly, A.; Denning-Kemp, G.; Geiringer, K.; Abdulhamid, A.; Albabtain, A.; Beard, M.; Brimble, J.; Campbell, A.; Feng, S.; Haminudin, M.; et al. Exposure to harmful housing conditions is common in children admitted to Wellington Hospital. N. Z. Med. J. 2013, 126, 108–126. [Google Scholar] [PubMed]
- Athey, K.R.; Coleman, J.E.; Reitman, A.P.; Tang, J. Two experiments showing the effect of the interviewer’s racial background on responses to questionnaires concerning racial issues. J. Appl. Psychol. 1960, 44, 244–246. [Google Scholar] [CrossRef]
- Greenland, S.; Daniel, R.; Pearce, N. Outcome modelling strategies in epidemiology: Traditional methods and basic alternatives. Int. J. Epidemiol. 2016, 45, 565–575. [Google Scholar] [CrossRef] [Green Version]
- Rockhill, B.; Newman, B.; Weinberg, C. Use and misuse of population attributable fractions. Am. J. Public Health 1998, 88, 15–19. [Google Scholar] [CrossRef] [Green Version]





| Diagnosis | Requirements | Category |
|---|---|---|
| Initial Episode of ARF | Chorea, or 2 major or 1 major and 2 minor manifestations plus evidence of a preceding GAS infection * | Definite ARF |
| Initial Episode of ARF | 1 major and 2 minor with the inclusion of evidence of a preceding GAS infection* as a minor manifestation (Jones, 1956) | Probable ARF |
| Initial Episode of ARF | Strong clinical suspicion of ARF, but insufficient signs and symptoms to fulfil diagnosis of definite or probable ARF | Possible ARF |
| Recurrent ARF | ARF in a case with known past history of ARF or RHD | Recurrent ARF (not eligible for study) |
| Inclusion |
| • Definite and probable ARF using NZ criteria (Table 1); |
| • Recruited within four weeks of hospital admission; |
| • Aged under 20 years at time of diagnosis; |
| • Normally resident in study area (one of the 11 North Island DHBs in the study). |
| Exclusion |
| • Cases presenting only with chorea or indolent carditis; |
| • Cases with a previous diagnosis of ARF (i.e., recurrent ARF) or RHD; |
| • Cases outside age group, study area or hospitalised more than four weeks prior to recruitment. |
| Specimen | Measurement(s) of Interest |
|---|---|
| Throat Swab | Presence/absence of GAS; emm-gene typing |
| Nasal (Anterior Nares) Swab | Presence/absence of S. aureus |
| Blood Samples | Vitamin D; serum ferritin levels; Immunophenotypic-profiling DNA for genetic testing |
| Head Hair (–2cm Long, Proximal Section) | Nicotine exposure |
| Data Sources and Linking Method | Measurement(s) of Interest |
|---|---|
| National Minimum Dataset (NMDS) held by the NZ Ministry of Health, linked via NHI | Previous hospitalisations (dates, diagnostic codes) total and for infectious diseases (respiratory, skin) |
| Maternity Collections held by the NZ Ministry of Health, linked via NHI | Early life exposures, e.g., Low birth weight, pre-term delivery, Apgar score |
| Clinical data held by DHBs on ARF cases, linked via NHI | Clinical information for case review (clinical record, laboratory results, cardiac ultrasound) Height, weight and BMI |
| Dental records held by DHBs and other service providers, linked via name | Decayed, Missing, Filled Teeth (dmft/DMFT) scores obtained from dental service providers |
| Housing records from a national housing and valuation database, linked via address | Age and floor area of the house |
| Census data and NZDep, linked via home address | NZDep of home meshblock, Population and density of home meshblock |
| NZ Ministry of Education schools data, linked via school name | School size |
| Record of schools participating in RFPP held by NZ Ministry of Health, linked via school name | Attendance at a school that provided a school-based throat swabbing programme at the time of illness or interview |
| Controls | Date recruited and interviewed for NZHS Height, weight, BMI |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, M.G.; Gurney, J.; Oliver, J.; Moreland, N.J.; Williamson, D.A.; Pierse, N.; Wilson, N.; Merriman, T.R.; Percival, T.; Murray, C.; et al. Risk Factors for Acute Rheumatic Fever: Literature Review and Protocol for a Case-Control Study in New Zealand. Int. J. Environ. Res. Public Health 2019, 16, 4515. https://doi.org/10.3390/ijerph16224515
Baker MG, Gurney J, Oliver J, Moreland NJ, Williamson DA, Pierse N, Wilson N, Merriman TR, Percival T, Murray C, et al. Risk Factors for Acute Rheumatic Fever: Literature Review and Protocol for a Case-Control Study in New Zealand. International Journal of Environmental Research and Public Health. 2019; 16(22):4515. https://doi.org/10.3390/ijerph16224515
Chicago/Turabian StyleBaker, Michael G, Jason Gurney, Jane Oliver, Nicole J Moreland, Deborah A Williamson, Nevil Pierse, Nigel Wilson, Tony R Merriman, Teuila Percival, Colleen Murray, and et al. 2019. "Risk Factors for Acute Rheumatic Fever: Literature Review and Protocol for a Case-Control Study in New Zealand" International Journal of Environmental Research and Public Health 16, no. 22: 4515. https://doi.org/10.3390/ijerph16224515
APA StyleBaker, M. G., Gurney, J., Oliver, J., Moreland, N. J., Williamson, D. A., Pierse, N., Wilson, N., Merriman, T. R., Percival, T., Murray, C., Jackson, C., Edwards, R., Foster Page, L., Chan Mow, F., Chong, A., Gribben, B., & Lennon, D. (2019). Risk Factors for Acute Rheumatic Fever: Literature Review and Protocol for a Case-Control Study in New Zealand. International Journal of Environmental Research and Public Health, 16(22), 4515. https://doi.org/10.3390/ijerph16224515







