Obstetricians’ and Gynecologists’ Communication Practices around Smoking Cessation in Pregnancy, Secondhand Smoke and Sudden Infant Death Syndrome (SIDS): A Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measures
2.2. Data Analysis
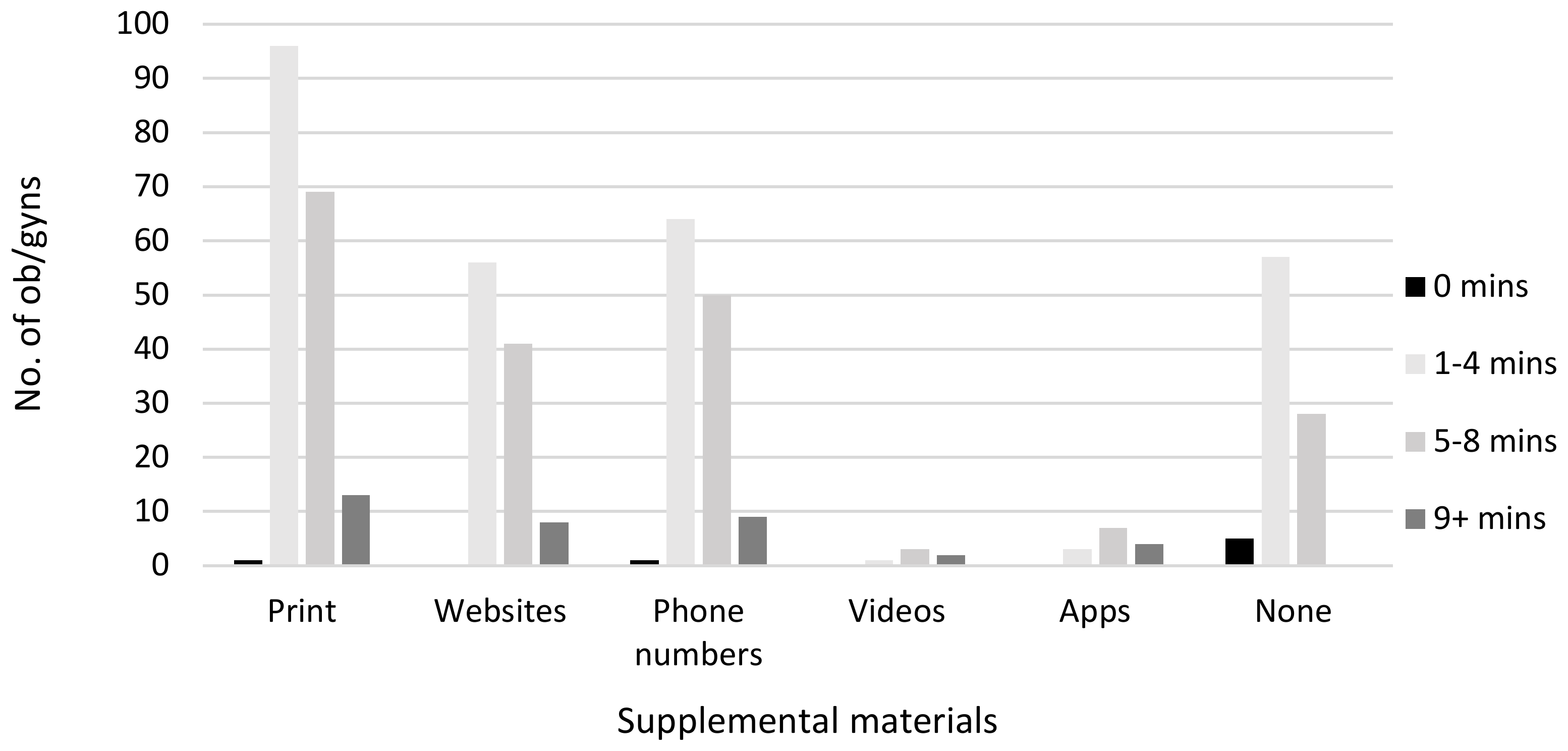
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mathews, T.J.; MacDorman, M. Infant mortality statistics from the 2010 period linked birth/infant death data set. In National Vital Statistics Reports; National Center for Health Statistics: Hyattsville, MD, USA, 2013; Volume 62, No 9. [Google Scholar]
- Anderson, H.R.; Cook, D.G. Passive smoking and sudden infant death syndrome: Review of the epidemiological evidence. Thorax 1997, 52, 1003–1009. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, E.A.; Milerad, J. Smoking and the sudden infant death syndrome. Rev. Environ. Health 2006, 21, 81–104. [Google Scholar] [CrossRef]
- Anderson, T.M.; Lavista Ferres, J.M.; You Ren, S.; Moon, R.Y.; Goldstein, R.D.; Ramirez, J.M.; Mitchell, E.A. Maternal smoking before and during pregnancy and the risk of Sudden Unexpected Infant Death. Pediatrics 2019, 143, e20183325. [Google Scholar] [CrossRef] [Green Version]
- Slotkin, T.A.; Lappi, S.E.; McCook, E.C.; Lorber, B.A.; Seidler, F.J. Loss of neonatal hypoxia tolerance after prenatal nicotine exposure: Implications for sudden infant death syndrome. Brain Res. Bull. 1995, 38, 69–75. [Google Scholar] [CrossRef]
- Horne, R.S.C. Sudden infant death syndrome: Current perspectives. Intern. Med. J. 2019, 49, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.S.; Franco, P.; Adamson, T.M.; Groswasser, J.; Kahn, A. Influences of maternal cigarette smoking on infant arousability. Early Hum. Dev. 2004, 79, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Kinney, H.C.; Filiano, J.J. Brainstem research in sudden infant death syndrome. Pediatrician 1988, 15, 240–250. [Google Scholar] [PubMed]
- U.S Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Available online: https://www.ncbi.nlm.nih.gov/books/NBK44324/ (accessed on 17 March 2020).
- Mathews, T.J.; MacDorman, M.F.; Thoma, M.E. Infant mortality statistics from the 2013 period linked birth/infant death data set. In National Vital Statistics Reports; National Center for Health Statistics: Hyattsville, MD, USA, 2015; Volume 64, No 9. [Google Scholar]
- Bartick, M.; Tomori, C. Sudden infant death and social justice: A syndemics approach. Matern. Child Nutr. 2019, e2652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, R.Y.; AAP Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: Evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics 2016, 138, e20162940. [Google Scholar] [CrossRef] [Green Version]
- Stiffer, D.; Ayres, B.; Fauvergue, C.; Cullen, D. Sudden infant death and sleep practices in the black community. J. Spec. Ped. Nurs. 2018, 23, e12213. [Google Scholar] [CrossRef] [PubMed]
- Drope, J.; Liber, A.C.; Cahn, Z.; Stoklosa, M.; Kennedy, R.; Douglas, C.E.; Henson, R.; Drope, J. Who’s still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer 2018, 68, 106–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ostfeld, B.M.; Esposito, L.; Perl, H.; Hegyi, T. Concurrent risks in sudden infant death syndrome. Pediatrics 2010, 125, 447–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, R.Y.; Gingras, J.L.; Erwin, R. Physician beliefs and practices regarding SIDS and SIDS risk reduction. Clin. Pediatr. 2002, 41, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Tracy, E.E.; Haas, S.; Lauria, M.R. Newborn care and safety: The black box of obstetric practices and residency training. Obstet. Gynecol. 2012, 120, 643–646. [Google Scholar] [CrossRef] [PubMed]
- Eron, N.B.; Dygert, K.M.; Squillace, C.; Webster, N.J.; Andrianos, A.; Crockett, E.G.; Consenstein, L. The physician’s role in reducing SIDS. Health Promot. Pract. 2011, 12, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Moon, R.Y.; Hauck, F.R.; Colson, E.R. Safe infant sleep interventions: What is the evidence for successful behavior change? Curr. Pediatric Rev. 2016, 12, 67–75. [Google Scholar] [CrossRef] [Green Version]
- United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Vital Statistics, Natality public-use data 2016–2018, on CDC WONDER Online Database, September 2019. Available online: http://wonder.cdc.gov/natality-expanded-current.html (accessed on 17 March 2020).
- Weisband, Y.L.; Gallo, M.F.; Klebanoff, M.; Shoben, A.; Norris, A.H. Who uses a midwife for prenatal care and for birth in the United States? A secondary analysis of Listening to Mothers III. Women Health Issues 2018, 28, 89–96. [Google Scholar] [CrossRef]
- Ryan, H.; Trosclair, A.; Gfroerer, J. Adult current smoking: Differences in definitions and prevalence estimates—NHIS and NSDUH, 2008. J. Environ. Public Health 2012, 918368. [Google Scholar] [CrossRef]
- Mostafa, N.; Momen, M. Effect of physicians′ smoking status on their knowledge, attitude, opinions and practices of smoking cessation in a University Hospital in Egypt. J. Egypt Public Health Assoc. 2017, 92, 96–106. [Google Scholar] [CrossRef]
- Fiore, M.C.; Jaén, C.R.; Baker, T.B.; Bailey, W.C.; Benowitz, N.L.; Curry, S.J.; Dorfman, S.F.; Froelicher, E.S.; Goldstein, M.G.; Healton, C.G.; et al. Treating Tobacco Use and Dependence: 2008 Update: Clinical Practice Guideline; Department of Health and Human Services, Public Health Service: Rockville, MD, USA, 2008. [Google Scholar]
- Nabi-Burza, E.; Drehmer, J.E.; Hipple Walters, B.; Rigotti, N.A.; Ossip, D.J.; Levy, D.E.; Klein, J.D.; Regan, S.; Gorzkowski, J.A.; Winickoff, J.P. Treating parents for tobacco Use in the pediatric setting: The clinical effort against secondhand smoke exposure cluster randomized clinical trial. JAMA Pediatr. 2019, 173, 931–939. [Google Scholar] [CrossRef]
- Winickoff, J.P.; Nabi-Burza, E.; Chang, Y.; Finch, S.; Regan, S.; Wasserman, R.; Ossip, D.; Woo, H.; Klein, J.; Dempsey, J.; et al. Implementation of a parental tobacco control intervention in pediatric practice. Pediatrics 2013, 132, 109–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulos, M.N.; Brewer, A.C.; Karimkhani, C.; Buller, D.B.; Dellavalle, R.P. Mobile medical and health apps: State of the art, concerns, regulatory control and certification. Online J. Public Health Inform. 2014, 5, 229. [Google Scholar] [PubMed] [Green Version]
- International Data Corporation. Smartphone OS Market Share, 2017. Q1. 2017. Available online: https://www.idc.com/promo/smartphone-market-share/oswebcite (accessed on 10 January 2020).
- Cisco. Cisco Visual Networking Index: Global Mobile Data Traffic Forecast Update, 2017–2022 White Paper. 2016. Available online: https://tinyurl.com/y2lwempdwebcite (accessed on 10 January 2020).
- Waring, M.E.; Moore, S.T.; Xiao, R.S.; Lombardini, L.M.; Allison, J.J.; Rosal, M.C.; Pagoto, S.L. Pregnant women′s interest in a website or mobile application for healthy gestational weight gain. Sex Reprod. Healthc. 2014, 5, 182–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goetz, M.; Müller, M.; Matthies, L.M.; Hansen, J.; Doster, A.; Szabo, A.; Pauluschke-Fröhlich, J.; Abele, H.; Sohn, C.; Wallwiener, M.; et al. Perceptions of patient engagement applications during pregnancy: A qualitative assessment of the patient’s perspective. JMIR Mhealth Uhealth. 2017, 26, e73. [Google Scholar] [CrossRef]
- Guerra-Reyes, L.; Christie, V.M.; Prabhakar, A.; Harris, A.L.; Siek, K.A. Postpartum health information seeking using mobile phones: Experiences of low-income mothers. Matern. Child Health J. 2016, 20, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Simply Put: A Guide for Creating Easy-to-Understand Materials [Handbook]. April 2009. Available online: https://www.cdc.gov/healthliteracy/pdf/simply_put.pdf (accessed on 10 January 2020).
- Ashford, K.B.; Hahn, E.; Hall, L.; Rayens, M.K.; Noland, M. Postpartum smoking relapse and secondhand smoke. Public Health Rep. 2009, 124, 515–526. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. American Academy of Pediatrics Announces New Safe Sleep Recommendations to Protect Against SIDS, Sleep-Related Infant Deaths. Available online: https://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/American-Academy-of-Pediatrics-Announces-New-Safe-Sleep-Recommendations-to-Protect-Against-SIDS.aspx (accessed on 17 March 2020).
- Notley, C.; Blyth, A.; Craig, J.; Edwards, A.; Holland, R. Postpartum smoking relapse—A thematic synthesis of qualitative studies. Addiction 2015, 110, 1712–1723. [Google Scholar] [CrossRef]
- Reid, K.M.; Taylor, M.G. Social support, stress, and maternal postpartum depression: A comparison of supportive relationships. Soc. Sci. Res. 2015, 54, 246–262. [Google Scholar] [CrossRef]
- Baker, B.; Yang, I. Social media as social support in pregnancy and the postpartum. Sex Reprod. Healthc. 2018, 17, 31–34. [Google Scholar] [CrossRef]
- Lee, S.Y.; Sirieix, C.M.; Nattie, E.; Li, A. Pre- and early postnatal nicotine exposure exacerbates autoresuscitation failure in serotonin-deficient rat neonates. J. Physiol. 2018, 596, 5977–5991. [Google Scholar] [CrossRef] [Green Version]
- Liebrechts-Akkerman, G.; Lao, O.; Liu, F.; van Sleuwen, B.E.; Engelberts, A.C.; L’hoir, M.P.; Tiemeier, H.W.; Kayser, M. Postnatal parental smoking: An important risk factor for SIDS. Eur. J. Pediatr. 2011, 170, 1281–1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Lee, N.L.; Burstyn, I. Smoking and use of electronic cigarettes (vaping) in relation to preterm birth and small-for-gestational-age in a 2016 U.S. national sample. Prev. Med. 2020, 134, 106041. [Google Scholar] [CrossRef] [PubMed]
- Malloy, M.H. Size for gestational age at birth: Impact on risk for sudden infant death and other causes of death, USA 2002. Arch. Dis. Child. Fetal Neonatal Ed. 2007, 92, F473–F478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDonnell, B.P.; Dicker, P.; Regan, C.L. Electronic cigarettes and obstetric outcomes: A prospective observational study. BJOG 2020. [Google Scholar] [CrossRef]
- Feeney, A.; Britton, G. Counseling women on smoking relapse prevention during postpartum. MCN Am. J. Matern. Child Nurs. 2016, 41, 287–292. [Google Scholar] [CrossRef]


| Measures | Never | Rarely | Some of the Time | Most of the Time | Always |
|---|---|---|---|---|---|
| Ask your patients if they smoke | 0 (0) | 4 (1.3) | 11 (3.5) | 62 (19.6) | 239 (75.6) |
| Advise smokers to quit | 1 (0.3) | 3 (0.9) | 16 (5.1) | 88 (27.8) | 208 (65.8) |
| Ask smokers if they are interested in quitting | 2 (0.6) | 12 (3.8) | 50 (15.8) | 106 (33.5) | 146 (46.2) |
| Encourage smokers to set a quit date | 14 (4.4) | 57 (18) | 105 (33.2) | 78 (24.7) | 62 (19.6) |
| Discuss medication options (nicotine replacement therapy) | 11 (3.5) | 60 (19) | 117 (37) | 79 (25) | 48 (15.2) |
| Refer interested smokers to cessation treatment | 32 (10.1) | 65 (20.6) | 81 (25.6) | 69 (21.8) | 68 (21.5) |
| Follow up with a letter or call | 138 (43.7) | 118 (37.3) | 33 (10.4) | 18 (5.7) | 8 (2.5) |
| Age Subgroup | Prevalence and Odds of Discussing Medication Options (Nicotine Replacement Therapy) for Cessation Treatment at Least Some of the Time * | Prevalence and Odds of at Least Somewhat Agreeing that Lack of Time Is a Barrier to Providing Cessation Treatment | Prevalence and Odds of Recommending Smokers Switch to E-Cigarettes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years old | % | AOR | 95% CI | p-Value | % | AOR | 95% CI | p-Value | % | AOR | 95% CI | p-Value | |||
| 33–49 | 71.2 | ref | 84.9 | 6.28 | 2.50 | 15.80 | <0.001 | 8.7 | ref | ||||||
| 50–65 | 83.8 | 2.38 | 1.24 | 4.57 | <0.01 | 79.4 | 3.72 | 1.61 | 8.59 | <0.01 | 20.6 | 2.82 | 1.29 | 6.17 | <0.01 |
| 66+ | 85.3 | 2.73 | 0.92 | 8.08 | 0.069 | 52.9 | ref | 8.8 | 0.96 | 0.24 | 3.83 | 0.949 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sontag, J.M.; Singh, B.; Ostfeld, B.M.; Hegyi, T.; Steinberg, M.B.; Delnevo, C.D. Obstetricians’ and Gynecologists’ Communication Practices around Smoking Cessation in Pregnancy, Secondhand Smoke and Sudden Infant Death Syndrome (SIDS): A Survey. Int. J. Environ. Res. Public Health 2020, 17, 2908. https://doi.org/10.3390/ijerph17082908
Sontag JM, Singh B, Ostfeld BM, Hegyi T, Steinberg MB, Delnevo CD. Obstetricians’ and Gynecologists’ Communication Practices around Smoking Cessation in Pregnancy, Secondhand Smoke and Sudden Infant Death Syndrome (SIDS): A Survey. International Journal of Environmental Research and Public Health. 2020; 17(8):2908. https://doi.org/10.3390/ijerph17082908
Chicago/Turabian StyleSontag, Jennah M., Binu Singh, Barbara M. Ostfeld, Thomas Hegyi, Michael B. Steinberg, and Cristine D. Delnevo. 2020. "Obstetricians’ and Gynecologists’ Communication Practices around Smoking Cessation in Pregnancy, Secondhand Smoke and Sudden Infant Death Syndrome (SIDS): A Survey" International Journal of Environmental Research and Public Health 17, no. 8: 2908. https://doi.org/10.3390/ijerph17082908






