Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Research Team Settlement
2.4. Interventions
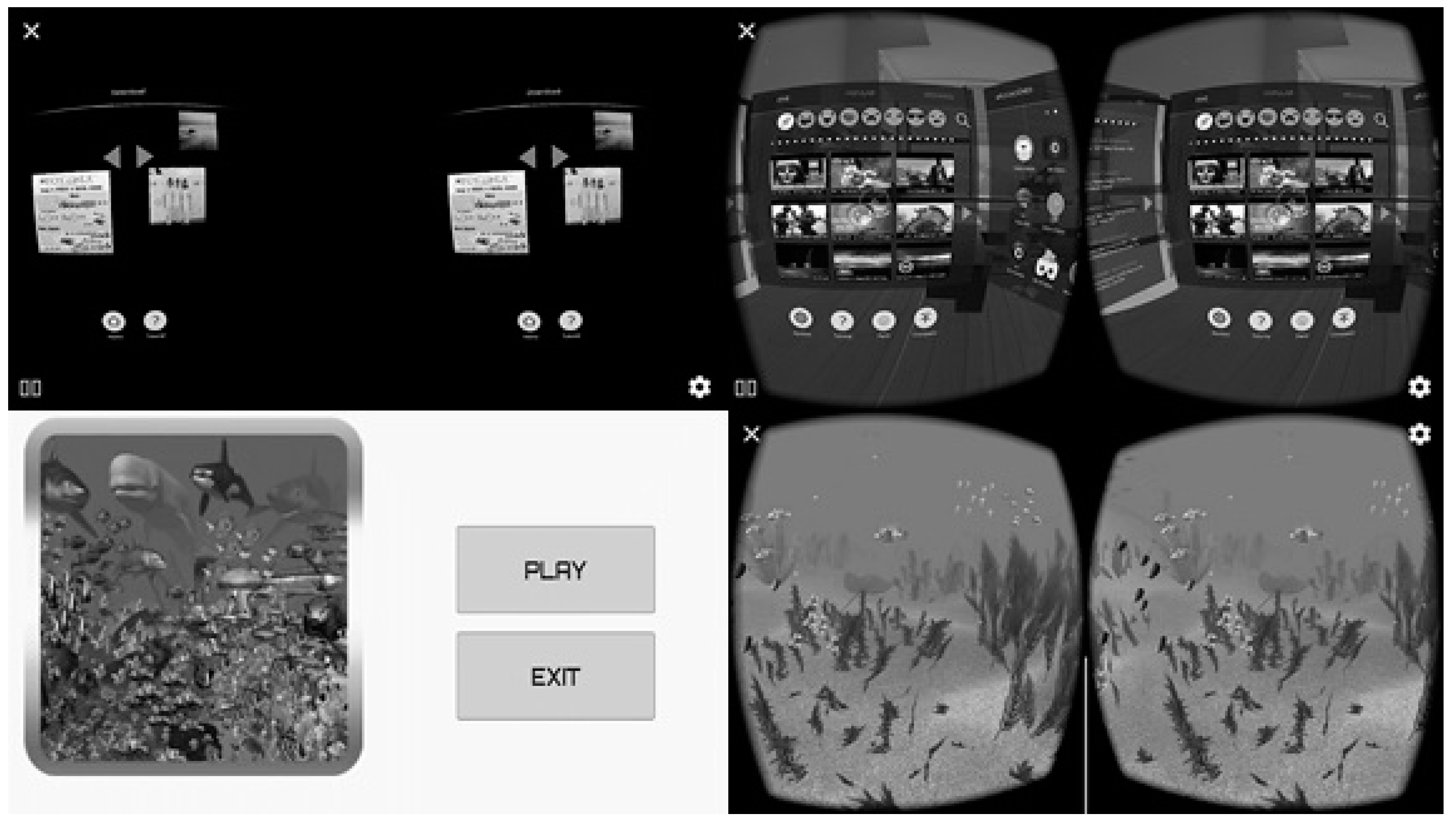
2.4.1. Virtual Reality Treatment
2.4.2. Neck Exercises
2.5. Outcome Measures
2.5.1. Primary Outcomes
Visual Analog Scale (VAS)
Conditioned Pain Modulation
Temporal Summation
2.5.2. Secondary Outcomes
Active Cervical Range of Movement
Neck Disability Index (NDI)
Pain Catastrophizing
Pain-Related Fear of Movement/(Re)Injury
Fear-Avoidance Beliefs
Pain Pressure Thresholds
Pain-Related Anxiety
2.6. Procedure
2.7. Sample Size Calculation and Randomization
2.8. Statistical Analysis
3. Results
3.1. Variables
3.1.1. Neck Pain Intensity
3.1.2. Conditioned Pain Modulation
3.1.3. Temporal Summation
3.1.4. Range of Motion
3.1.5. Neck Disability Index
3.1.6. Pain Catastrophizing
3.1.7. Pain Kinesiophobia
3.1.8. Fear-Avoidance Beliefs
3.1.9. Pressure Pain Threshold
3.1.10. Anxiety
4. Discussion
4.1. Clinical Implications
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Haldeman, S.; Carroll, L.; Cassidy, J.D. Findings from the bone and joint decade 2000 to 2010 task force on neck pain and its associated disorders. J. Occup. Environ. Med. 2010, 52, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Safari, S.; Kolahi, A.; Hoy, D.; Buchbinder, R.; Mansournia, M.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Smith, E.; Sepidarkish, M.; et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: Systematic analysis of the Global Burden of Disease Study 2017. BMJ 2020, 368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoy, D.; March, L.; Woolf, A.; Blyth, F.; Brooks, P.; Smith, E.; Vos, T.; Barendregt, J.; Blore, J.; Murray, C.; et al. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Palacios-Ceña, D.; Alonso-Blanco, C.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Jiménez-García, R.; Fernández-de-las-Peñas, C. Prevalence of neck and low back pain in community—Dwelling adults in Spain: An updated population-based national study (2009/10–2011/12). Eur. Spine J. 2015, 24, 482–492. [Google Scholar] [CrossRef]
- Saavedra-Hernández, M.; Castro-Sánchez, A.M.; Cuesta-Vargas, A.I.; Cleland, J.; Fernández-de-las-Peñas, C.; Arroyo-Morales, M. The contribution of previous episodes of pain, pain intensity, physical impairment, and pain-related fear to disability in patients with chronic mechanical neck pain. Am. J. Phys. Med. Rehabil. 2012, 91, 1070–1076. [Google Scholar] [CrossRef]
- Bahat, H.S.; Weiss, P.; Sprecher, E. Do neck kinematics correlate with pain intensity, neck disability or with fear of motion? Man. Ther. 2014, 19, 252–258. [Google Scholar] [CrossRef]
- Rudolfsson, T.; Björklund, M.; Djupsjöbacka, M. Range of motion in the upper and lower cervical spine in people with chronic neck pain. Man. Ther. 2012, 17, 53–59. [Google Scholar] [CrossRef]
- Lee, H.; Nicholson, L.L.; Adams, R.D. Neck muscle endurance, self-report, and range of motion data from subjects with treated and untreated neck pain. J. Manip. Physiol. Ther. 2005, 28, 25–32. [Google Scholar] [CrossRef]
- Beltran-Alacreu, H.; López-de-Uralde-Villanueva, I.; Calvo-Lobo, C.; Fernández-Carnero, J.; Touche, R. La Clinical features of patients with chronic non-specific neck pain per disability level: A novel observational study. Rev. Assoc. Med. Bras. 2018. [Google Scholar] [CrossRef] [Green Version]
- Tsang, S.M.H.; Szeto, G.P.Y.; Lee, R.Y.W. Movement coordination and differential kinematics of the cervical and thoracic spines in people with chronic neck pain. Clin. Biomech. 2013, 28, 610–617. [Google Scholar] [CrossRef]
- Johnston, V.; Jull, G.; Souvlis, T.; Jimmieson, N.L. Neck movement and muscle activity characteristics in female office workers with neck pain. Spine 2008, 33, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Lin, R.-F.; Chang, J.-J.; Lu, Y.-M.; Huang, M.-H.; Lue, Y.-J. Correlations between quality of life and psychological factors in patients with chronic neck pain. Kaohsiung J. Med. Sci. 2010, 26, 13–20. [Google Scholar] [CrossRef] [Green Version]
- Fowler, C.A.; Ballistrea, L.M.; Mazzone, K.E.; Martin, A.M.; Kaplan, H.; Kip, K.E.; Murphy, J.L.; Winkler, S.L. A virtual reality intervention for fear of movement for Veterans with chronic pain: Protocol for a feasibility study. Pilot Feasibility Stud. 2019, 5, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hudes, K. The Tampa Scale of Kinesiophobia and neck pain, disability and range of motion: A narrative review of the literature. J. Can. Chiropr. Assoc. 2011, 55, 222–232. [Google Scholar]
- Leeuw, M.; Goossens, M.E.J.B.; Linton, S.J.; Crombez, G.; Boersma, K.; Vlaeyen, J.W.S. The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. J. Behav. Med. 2007, 30, 77–94. [Google Scholar] [CrossRef] [Green Version]
- López-De-Uralde-Villanueva, I.; Notario-Pérez, R.; Del Corral, T.; Ramos-Díaz, B.; Acuyo-Osorio, M.; La Touche, R. Functional limitations and associated psychological factors in military personnel with chronic nonspecific neck pain with higher levels of kinesiophobia. Work 2017, 58, 287–297. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-García, D.; Gil-Martínez, A.; López-López, A.; Lopez-de-Uralde-Villanueva, I.; La Touche, R.; Fernández-Carnero, J. Chronic Neck Pain and Cervico-Craniofacial Pain Patients Express Similar Levels of Neck Pain-Related Disability, Pain Catastrophizing, and Cervical Range of Motion. Pain Res. Treat. 2016. [Google Scholar] [CrossRef] [Green Version]
- Itoh, K.; Katsumi, Y.; Hirota, S.; Kitakoji, H. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement. Ther. Med. 2007, 15, 172–179. [Google Scholar] [CrossRef]
- Lopez-de-Uralde-Villanueva, I.; Beltran-Alacreu, H.; Fernandez-Carnero, J.; Kindelan-Calvo, P.; La Touche, R. Widespread Pressure Pain Hyperalgesia in Chronic Nonspecific Neck Pain with Neuropathic Features: A Descriptive Cross-Sectional Study. Pain Physician 2016, 19, 77–88. [Google Scholar]
- Muñoz-García, D.; López-de-Uralde-Villanueva, I.; Beltran-Alacreu, H.; La Touche, R.; Fernández-Carnero, J. Patients with concomitant chronic neck pain and myofascial pain in masticatory muscles have more widespread pain and distal hyperalgesia than patients with only chronic neck pain. Pain Med. 2017, 18, 526–537. [Google Scholar] [CrossRef] [Green Version]
- Piña-Pozo, F.; Heredia-Rizo, A.M.; Madeleine, P.; Escobio-Prieto, I.; Luque-Carrasco, A.; Oliva-Pascual-Vaca, Á. Local and Widespread Pressure Pain Hyperalgesia Is Not Side Specific in Females with Unilateral Neck Pain that Can Be Reproduced during Passive Neck Rotation. J. Clin. Med. 2019, 8, 1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarig Bahat, H.; Croft, K.; Carter, C.; Hoddinott, A.; Sprecher, E.; Treleaven, J. Remote kinematic training for patients with chronic neck pain: A randomised controlled trial. Eur. Spine J. 2018, 27, 1309–1323. [Google Scholar] [CrossRef] [PubMed]
- Sarig-Bahat, H.; Takasaki, H.; Chen, X.; Betor, Y.; Treleaven, J. Cervical kinematic training with and without an interactive virtual reality device for chronic neck pain—A pilot randomized clinical trial. Man. Ther. 2015, 20, 68–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahern, M.M.; Dean, L.V.; Stoddard, C.C.; Agrawal, A.; Kim, K.; Cook, C.E.; Narciso Garcia, A. The Effectiveness of Virtual Reality in Patients with Spinal Pain: A Systematic Review and Meta-Analysis. Pain Pract. 2020, 20, 656–675. [Google Scholar] [CrossRef] [PubMed]
- Matheve, T.; Bogaerts, K.; Timmermans, A. Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: A randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 55. [Google Scholar] [CrossRef] [PubMed]
- Gumaa, M.; Youssef, A.R. Is Virtual Reality Effective in Orthopedic Rehabilitation? A Systematic Review and Meta-Analysis. Phys. Ther. 2019, 99, 1304–1325. [Google Scholar] [CrossRef] [Green Version]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340. [Google Scholar] [CrossRef]
- World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA J. Am. Med. Assoc. 2013, 310, 2191–2194. [CrossRef] [Green Version]
- Serrano-Atero, M.S.; Caballero, J.; Cañas, A.; García-Saura, P.L.; Serrano-Álvarez, C.; Prieto, J. Valoración del dolor (I). REVISIÓN 2002, 9, 94–108. [Google Scholar]
- Antolinez, L. Escala Visual Análoga, Universidad de Pamplona; Facultad de Salud. Departamento de Psicología: Pamplona, Colombia, 2014. [Google Scholar]
- Collins, S.L.; Moore, R.A.; McQuay, H.J. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain 1997, 72, 95–97. [Google Scholar] [CrossRef]
- Lee, J.S.; Hobden, E.; Stiell, I.G.; Wells, G.A. Clinically important change in the visual analog scale after adequate pain control. Acad. Emerg. Med. 2003, 10, 1128–1130. [Google Scholar] [CrossRef]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Vierck, C.J. Psychological and neural mechanisms of pain, by Donald D. Price; Raven Press, 1988, 253 pp. Synapse 1989, 4, 96. [Google Scholar] [CrossRef]
- Yarnitsky, D.; Sprecher, E.; Zaslansky, R.; Hemli, J.A. Multiple session experimental pain measurement. Pain 1996, 67, 327–333. [Google Scholar] [CrossRef]
- Smith, A.; Pedler, A. Conditioned pain modulation is affected by occlusion cuff conditioning stimulus intensity, but not duration. Eur. J. Pain 2018, 22, 94–102. [Google Scholar] [CrossRef] [Green Version]
- Cathcart, S.; Winefield, A.H.; Rolan, P.; Lushington, K. Reliability of temporal summation and diffuse noxious inhibitory control. Pain Res. Manag. 2009, 14, 433–438. [Google Scholar] [CrossRef] [Green Version]
- Yarnitsky, D. Role of endogenous pain modulation in chronic pain mechanisms and treatment. Pain 2015, 156, S24–S31. [Google Scholar] [CrossRef]
- Yoo, W.-G.; An, D.-H. The relationship between the active cervical range of motion and changes in head and neck posture after continuous VDT work. Ind. Health 2009, 47, 183–188. [Google Scholar] [CrossRef] [Green Version]
- Prushansky, T.; Dvir, Z. Cervical Motion Testing: Methodology and Clinical Implications. J. Manipulative Physiol. Ther. 2008, 31, 503–508. [Google Scholar] [CrossRef]
- Audette, I.; Dumas, J.-P.; Côté, J.N.; De Serres, S.J. Validity and between-day reliability of the cervical range of motion (CROM) device. J. Orthop. Sports Phys. Ther. 2010, 40, 318–323. [Google Scholar] [CrossRef]
- Andrade Ortega, J.A.; Delgado Martínez, A.D.; Almécija Ruiz, R. Validation of the Spanish version of the Neck Disability Index. Spine 2010, 35, E114–E118. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement properties of the neck disability index: A systematic review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vernon, H. The Neck Disability Index: State-of-the-art, 1991–2008. J. Manip. Physiol. Ther. 2008, 31, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Hains, F.; Waalen, J.; Mior, S. Psychometric properties of the neck disability index. J. Manip. Physiol. Ther. 1998, 21, 75–80. [Google Scholar]
- Olmedilla, A.; Ortega, E.; Abenza, L. Validación de la escala de catastrofismo ante el dolor (Pain Catastrophizing Scale) en deportistas españoles./Validation of the Pain Catastrophizing Scale in Spanish athletes./Validação da escala de catastrofismo diante da dor (pain catastrophizing scale) em esportistas espanhóis. Cuad. Psicol. del Deport. 2013, 13, 83–94. [Google Scholar] [CrossRef] [Green Version]
- García Campayo, J.; Rodero, B.; Alda, M.; Sobradiel, N.; Montero, J.; Moreno, S. Validation of the Spanish version of the Pain Catastrophizing Scale in fibromyalgia. Med. Clin. 2008, 131, 487–492. [Google Scholar] [CrossRef]
- Gómez-Pérez, L.; López-Martínez, A.E.; Ruiz-Párraga, G.T. Psychometric Properties of the Spanish Version of the Tampa Scale for Kinesiophobia (TSK). J. Pain 2011, 12, 425–435. [Google Scholar] [CrossRef]
- Woby, S.R.; Roach, N.K.; Urmston, M.; Watson, P.J. Psychometric properties of the TSK-11: A shortened version of the Tampa Scale for Kinesiophobia. Pain 2005, 117, 137–144. [Google Scholar] [CrossRef]
- Lee, K.C.; Chiu, T.T.W.; Lam, T.H. The role of fear-avoidance beliefs in patients with neck pain: Relationships with current and future disability and work capacity. Clin. Rehabil. 2007, 21, 812–821. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Muriel, A.; Medina, J.M.; Abraira, V.; Sánchez, M.D.C.; Jaúregui, J.O. Psychometric characteristics of the Spanish version of the FAB questionnaire. Spine 2006, 31, 104–110. [Google Scholar] [CrossRef]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Zayfert, C.; Gross, R.T. The Pain Anxiety Symptoms Scale: Development and validation of a scale to measure fear of pain. Pain 1992, 50, 67–73. [Google Scholar] [CrossRef]
- McCracken, L.M.; Dhingra, L. A short version of the pain anxiety symptoms scale (PASS-20): Preliminary development and validity. Pain Res. Manag. 2002, 7, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Roelofs, J.; McCracken, L.M.; Peters, M.L.; Crombez, G.; van Breukelen, G.; Vlaeyen, J.W.S. Psychometric evaluation of the pain anxiety symptoms scale (PASS) in chronic pain patients. J. Behav. Med. 2004, 27, 167–183. [Google Scholar] [CrossRef] [PubMed]
- Abrams, M.P.; Carleton, R.N.; Asmundson, G.J.G. An Exploration of the Psychometric Properties of the PASS-20 with a Nonclinical Sample. J. Pain 2007, 8, 879–886. [Google Scholar] [CrossRef]
- López-Martínez, A.; Esteve-Zarazaga, R.; Ramírez-Maestre, C. The Spanish version of the Pain Anxiety Symptoms Scale (PASS-20): Preliminary data on its reliability, validity and factorial structure. Eur. J. Pain Suppl. 2011, 5, 256. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Cohen, J. Statistical power analysis for the behavioral sciences. Stat. Power Anal. Behav. Sci. 1988, 2, 567. [Google Scholar]
- Hayashi, K.; Aono, S.; Shiro, Y.; Ushida, T. Effects of Virtual Reality-Based Exercise Imagery on Pain in Healthy Individuals. Biomed Res. Int. 2019. [Google Scholar] [CrossRef]
- Gold, J.I.; Belmont, K.A.; Thomas, D.A. The neurobiology of virtual reality pain attenuation. Cyberpsychol. Behav. 2007, 10, 536–544. [Google Scholar] [CrossRef] [Green Version]
- Mallari, B.; Spaeth, E.K.; Goh, H.; Boyd, B.S. Virtual reality as an analgesic for acute and chronic pain in adults: A systematic review and meta-analysis. J. Pain Res. 2019, 12, 2053–2085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiederhold, B.K.; Gao, K.; Sulea, C.; Wiederhold, M.D. Virtual reality as a distraction technique in chronic pain patients. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.W.; Hsu, H.H.; Hou, Y.R.; Chiu, Y.L.; Sung, W.H. Immediate effects of virtual reality mental practice in subjects with low back pain: A pilot study. Ann. Phys. Rehabil. Med. 2018, 61, e483. [Google Scholar] [CrossRef]
- Lin, H.-T.; Li, Y.-I.; Hu, W.-P.; Huang, C.-C.; Du, Y.-C. A Scoping Review of the Efficacy of Virtual Reality and Exergaming on Patients of Musculoskeletal System Disorder. J. Clin. Med. 2019, 8, 791. [Google Scholar] [CrossRef] [Green Version]
- Morales Tejera, D.; Fernandez-Carnero, J.; Suso-Martí, L.; Cano-de-la-Cuerda, R.; Lerín-Calvo, A.; Remón-Ramiro, L.; La Touche, R. Comparative study of observed actions, motor imagery and control therapeutic exercise on the conditioned pain modulation in the cervical spine: A randomized controlled trial. Somatosens. Mot. Res. 2020. [Google Scholar] [CrossRef]
- Harvie, D.S.; Smith, R.T.; Moseley, G.L.; Meulders, A.; Michiels, B.; Sterling, M. Illusion-enhanced Virtual Reality Exercise for Neck Pain: A Replicated Single Case Series. Clin. J. Pain 2020, 36, 101–109. [Google Scholar] [CrossRef]
- Cuenca-Martínez, F.; La Touche, R.; León-Hernández, J.V.; Suso-Martí, L. Mental practice in isolation improves cervical joint position sense in patients with chronic neck pain: A randomized single-blind placebo trial. PeerJ 2019. [Google Scholar] [CrossRef] [Green Version]
- Spiegel, B.; Fuller, G.; Lopez, M.; Dupuy, T.; Noah, B.; Howard, A.; Albert, M.; Tashjian, V.; Lam, R.; Ahn, J.; et al. Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE 2019. [CrossRef] [Green Version]
- Dascal, J.; Reid, M.; Ishak, W.W.; Spiegel, B.; Recacho, J.; Rosen, B.; Danovitch, I. Virtual reality and medical inpatients: A systematic review of randomized, controlled trials. Innov. Clin. Neurosci. 2017, 14, 14–21. [Google Scholar]
- Hapidou, E.G.; Obrien, M.A.; Pierrynowski, M.R.; de las Heras, E.; Patel, M.; Patla, T. Fear and Avoidance of Movement in People with Chronic Pain: Psychometric Properties of the 11-item Tampa Scale for Kinesiophobia (TSK-11). Physiother. Can. 2012, 64, 235–241. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz Yelvar, G.D.; Çırak, Y.; Dalkılınç, M.; Parlak Demir, Y.; Guner, Z.; Boydak, A. Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial. Eur. Spine J. 2017, 26, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-Martínez, F.; Suso-Martí, L.; León-Hernández, J.V.; Touche, R. The role of movement representation techniques in the motor learning process: A neurophysiological hypothesis and a narrative review. Brain Sci. 2020, 10, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Variable | VR Group (n = 22) Mean ± SD (CI) | Control Group (n = 22) Mean ± SD (CI) | p-Value * |
|---|---|---|---|
| Age (years) | 32.72 ± 11.63 (27.56–37.88) | 26.68 ± 9.21 (22.59–30.76) | p = 0.063 |
| Male | 11 (50%) † | 10 (45.5%) | p = 0.763 ‡ |
| Female | 11 (50%) † | 12 (54.5%) | |
| VAS | 4.97 ± 1.88 (4.20–5.74) | 4.27 ± 1.3 (3.28–4.75) | p = 0.063 |
| CPM | 0.53 ± 0.74 (0.14–0.98) | 0.67 ± 0.94 (0.14–0.97) | p = 0.667 |
| TS + | –0.54 ± 1.31 (−1.75–−0.23) | −1.00 ± 1.42 (−2.04–−0.71) | p = 0.380 |
| F/E(ROM) | 110.22 ± 19.19 (101.71–118.73) | 116.13 ± 22.34 (106.22–126.04) | p = 0.352 |
| Lateroflexion (ROM) Rotation (ROM) | 79.54 ± 20.61 (70.40–88.68) | 87.21 ± 17.96 (79.24–95.17) | p = 0.196 |
| 114.10 ± 18.97 (105.69–122.52) | 118.48 ± 15.19 (111.74–125.22) | p = 0.403 | |
| NDI | 13.72 ± 6.68 (10.76–16.69) | 14.09 ± 9.32 (9.95–18.22) | p = 0.883 |
| PCS | 17.36 ± 11.49 (12.26–22.45) | 11.95 ± 9.39 (7.79–16.11) | p = 0.095 |
| Kinesiophobia | 22.90 ± 7.11 (19.75–26.06) | 21.40 ± 6.63 (18.46–24.35) | p = 0.474 |
| FAQ | 28.25 ± 16.43 (21.58–34.91) | 25.68 ± 13.02 (19.32–32.03) | p = 0.576 |
| PPT Right (kg/cm2) | 2.85 ± 1.59 (2.13–3.58) | 2.95 ± 1.09 (2.45–3.44) | p = 0.828 |
| PPT Left (kg/cm2) | 3.88 ± 2.13 (2.93–4.83) | 3.86 ± 1.69 (3.09–4.63) | p = 0.974 |
| PASS-20 | 27.52 ± 20.52 (19.31–35.73) | 26.59 ± 16.50 (18.57–34.61) | p = 0.870 |
| Variables | Times of Measurement | VR Group (n = 22) Mean ± SD (CI) | Control Group (n = 22) Mean ± SD (CI) | p-Value | Effect Size Cohen’s Method |
|---|---|---|---|---|---|
| VAS | Baseline | 4.97 ± 1.88 (4.20–5.74) | 4.27 ± 1.35 (3.57–4.97) | p = 0.063 | 0.27 |
| Post-treatment | 2.67 ± 1.91 † (1.90–3.44) | 3.11 ± 1.47 † (2.38–3.84) | p = 0.409 | 0.12 | |
| Follow-up 1 Month | 2.77 ± 2.04 † (1.91–3.63) | 1.88 ± 1.74 † (1.07–2.70) | p = 0.137 | 0.31 | |
| Follow-up 3 months | 2.17 ± 1.99 † (1.24–3.10) | 1.72 ± 2.09 † (0.84–2.61) | p = 0.484 | 0.10 | |
| CPM (µs) | Baseline | 0.53 ± 0.74 (0.14–0.98) | 0.67 ± 0.94 (0.14–0.97) | p = 0.667 | 0.70 |
| Post-treatment | 0.85 ± 0.65 (0.39–1.27) | 1.16 ± 1.11 (0.47–1.33) | p = 0.361 | 0.14 | |
| Follow-up 1 Month | 0.89 ± 0.91 (0.36–1.20) | 0.75 ± 0.91 (0.23–1.04) | p = 0.682 | 0.06 | |
| Follow-up 3 months | 0.88 ± 0.79 (0.41–1.14) | 0.62 ± 0.68 (0.18–0.89) | p = 0.335 | 0.15 | |
| TS | Baseline | −0.54 ± 1.31 (−1.75–−0.23) | −1.00 ± 1.42 (−2.04–−0.71) | p = 0.380 | 0.11 |
| Post-treatment | −0.75 ± 1.53 (−1.61–0.10) | −1.14 ± 1.49 (−1.89–−0.38) | p = 0.493 | 0.10 | |
| Follow-up 1 Month | −0.37 ± 1.52 (−1.28–0.53) | −1.69 ± 1.65 (−2.48–−0.89) | p = 0.034 * | 0.57 | |
| Follow-up 3 months | −0.30 ± 1.97 (−5.42–4.81) | −3.54 ± 11.79 (−8.01–0.93) | p = 0.338 | 0.15 | |
| F/E(ROM) | Baseline | 110.22 ± 19.19 (101.26–119.19) | 116.13 ± 22.34 (107.17–125.09) | p = 0.352 | 0.15 |
| Post-treatment | 112.01 ± 19.05 (103.19–120.83) | 116.92 ± 21.84 (108.10–125.74) | p = 0.431 | 0.12 | |
| Follow-up 1 Month | 113.18 ± 24.13 (103.97–122.38) | 117.63 ± 18.23 (108.43–126.84) | p = 0.494 | 0.10 | |
| Follow-up 3 months | 112.03 ± 23.99 (101.64–122.41) | 117.60 ± 24.27 (107.22–127.99) | p = 0.448 | 0.11 | |
| Lateroflexion (ROM) | Baseline | 79.54 ± 20.61 (70.96–88.12) | 87.21 ± 17.96 (78.78–95.63) | p = 0.196 | 0.23 |
| Post-treatment | 80.28 ± 22.25 (70.96–89.06) | 89.07 ± 20.04 (79.96–98.18) | p = 0.181 | 0.26 | |
| Follow-up 1 Month | 82.85 ± 21.91 (74.25–91.46) | 89.06 ± 16.94 (80.65–97.46) | p = 0.304 | 0.17 | |
| Follow-up 3 months | 84.93 ± 21.47 (76.46–93.40) | 86.42 ± 16.79 (78.14–94.69) | p = 0.801 | 0.05 | |
| Rotation (ROM) | Baseline | 114.10 ± 18.97 (107.66–123.24) | 118.48 ± 15.19 (111.05–125.91) | p = 0.403 | 0.08 |
| Post-treatment | 117.31 ± 23.64 (108.37–126.26) | 122.07 ± 15.49 (113.54–130.60) | p = 0.441 | 0.11 | |
| Follow-up 1 Month | 122.15 ± 19.42 (114.10–130.19) | 122.34 ± 16.17 (114.68–130.01) | p = 0.971 | 0.05 | |
| Follow-up 3 months | 121.90 ± 18.49 (114.21–129.58) | 124.30 ± 15.55 (116.97–131.63) | p = 0.650 | 0.07 | |
| NDI | Baseline | 13.72 ± 6.68 (9.66–16.72) | 14.09 ± 9.32 (10.64–17.54) | p = 0.883 | 0.06 |
| Post-treatment | 6.90 ± 6.28 (4.33–9.47) | 7.45 ± 5.36 (4.94–9.96) | p = 0.759 | 0.06 | |
| Follow-up 1 Month | 5.57 ± 6.32 (2.97–8.16) | 5.95 ± 5.43 (3.41–8.49) | p = 0.832 | 0.05 | |
| Follow-up 3 months | 4.95 ± 6.60 (2.44–7.46) | 5.77 ± 4.67 (3.31–8.22) | p = 0.640 | 0.07 | |
| PCS | Baseline | 17.36 ± 11.49 (12.20–21.41) | 11.95 ± 9.39 (7.45–16.45) | p = 0.095 | |
| Post-treatment | 8.52 ± 9.77 (4.97–12.07) | 6.40 ± 5.98 (2.94–9.87) | p = 0.395 | ||
| Follow-up 1 Month | 6.33 ± 10.06 (2.89–9.77) | 3.72 ± 4.72 (0.37–7.08) | p = 0.280 | ||
| Follow-up 3 months | 4.95 ± 8.08 (1.31–8.58) | 4.86 ± 8.40 (1.31–8.41) | p = 0.136 | ||
| Kinesiophobia | Baseline | 22.90 ± 7.11 (19.74–25.87) | 21.40 ± 6.63 (18.41–24.40) | p = 0.474 | 0.09 |
| Post-treatment | 18.90 ± 10.73 (14.84–22.96) | 18.36 ± 7.48 (14.39–22.33) | p = 0.848 | 0.05 | |
| Follow-up 1 Month | 14.85 ± 10.08 † (10.90–18.08) | 17.54 ± 7.75 (13.68–21.40) | p = 0.331 | 0.16 | |
| Follow-up 3 months | 12.09 ± 7.77 † (8.86–15.33) | 17.50 ± 6.89 (14.33–20.66) | p< 0.05 * | 0.65 | |
| FAQ | Baseline | 28.25 ± 16.43 (21.58–34.91) | 25.68 ± 13.02 (19.32–32.03) | p = 0.576 | |
| Post-treatment | 20.55 ± 16.78 (13.18–27.91) | 18.81 ± 15.84 (11.79–25.84) | p = 0.733 | ||
| Follow-up 1 Month | 18.95 ± 20.19 (11.31–26.58) | 15.84 ± 13.24 (8.58–23.14) | p = 0.558 | ||
| Follow-up 3 months | 12.30 ± 13.48 (6.00–18.59) | 16.59 ± 14.32 (10.58–22.59) | p = 0.325 | ||
| PPT Right (Kg/cm2) | Baseline | 2.85 ± 1.59 (2.38–3.64) | 2.95 ± 1.09 (2.35–3.55) | p = 0.828 | 0.05 |
| Post-treatment | 3.09 ± 1.33 (2.56–3.61) | 3.12 ± 0.90 (2.62–3.62) | p = 0.932 | 0.05 | |
| Follow-up 1 Month | 3.43 ± 1.44 (2.83–4.03) | 3.35 ± 1.14 (2.78–3.92) | p = 0.854 | 0.05 | |
| Follow-up 3 months | 3.53 ± 1.27 (2.96–4.01) | 3.28 ± 1.17 (2.74–3.83) | p = 0.525 | 0.09 | |
| PPT Left (Kg/cm2) | Baseline | 3.38 ± 2.13 (3.20–4.94) | 3.86 ± 1.69 (3.01–4.71) | p = 0.974 | 0.06 |
| Post-treatment | 4.77 ± 2.38 (3.83–5.70) | 4.07 ± 1.70 (3.15–4.98) | p = 0.284 | 0.18 | |
| Follow-up 1 Month | 3.55 ± 0.96 (3.04–4.05) | 3.58 ± 1.25 (3.09–4.08) | p = 0.920 | 0.05 | |
| Follow-up 3 months | 3.78 ± 0.97 (3.29–4.27) | 3.40 ± 1.17 (2.92–3.88) | p = 0.266 | 0.19 | |
| PASS-20 | Baseline | 27.52 ± 20.52 (19.31–35.73) | 26.59 ± 16.50 (18.57–34.61) | p = 0.870 | 0.05 |
| Post-treatment | 17.33 ± 16.71 (10.97–23.69) | 17.86 ± 11.85 (11.65–24.07) | p = 0.905 | 0.05 | |
| Follow-up 1 Month | 14.09 ± 17.44 (7.48–20.70) | 16.04 ± 12.20 (9.59–22.50) | p = 0.672 | 0.07 | |
| Follow-up 3 months | 12.33 ± 16.09 (6.23–18.43) | 15.90 ± 11.30 (9.94–21.87) | p = 0.402 | 0.13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tejera, D.M.; Beltran-Alacreu, H.; Cano-de-la-Cuerda, R.; Leon Hernández, J.V.; Martín-Pintado-Zugasti, A.; Calvo-Lobo, C.; Gil-Martínez, A.; Fernández-Carnero, J. Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 5950. https://doi.org/10.3390/ijerph17165950
Tejera DM, Beltran-Alacreu H, Cano-de-la-Cuerda R, Leon Hernández JV, Martín-Pintado-Zugasti A, Calvo-Lobo C, Gil-Martínez A, Fernández-Carnero J. Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial. International Journal of Environmental Research and Public Health. 2020; 17(16):5950. https://doi.org/10.3390/ijerph17165950
Chicago/Turabian StyleTejera, David Morales, Hector Beltran-Alacreu, Roberto Cano-de-la-Cuerda, Jose Vicente Leon Hernández, Aitor Martín-Pintado-Zugasti, César Calvo-Lobo, Alfonso Gil-Martínez, and Josué Fernández-Carnero. 2020. "Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial" International Journal of Environmental Research and Public Health 17, no. 16: 5950. https://doi.org/10.3390/ijerph17165950
APA StyleTejera, D. M., Beltran-Alacreu, H., Cano-de-la-Cuerda, R., Leon Hernández, J. V., Martín-Pintado-Zugasti, A., Calvo-Lobo, C., Gil-Martínez, A., & Fernández-Carnero, J. (2020). Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial. International Journal of Environmental Research and Public Health, 17(16), 5950. https://doi.org/10.3390/ijerph17165950








