Lifestyle Habits and Mental Health in Light of the Two COVID-19 Pandemic Waves in Sweden, 2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measures
2.3. Statistical Analyses
3. Results
3.1. Working, Commuting Situation, and Type of Sitting at Home
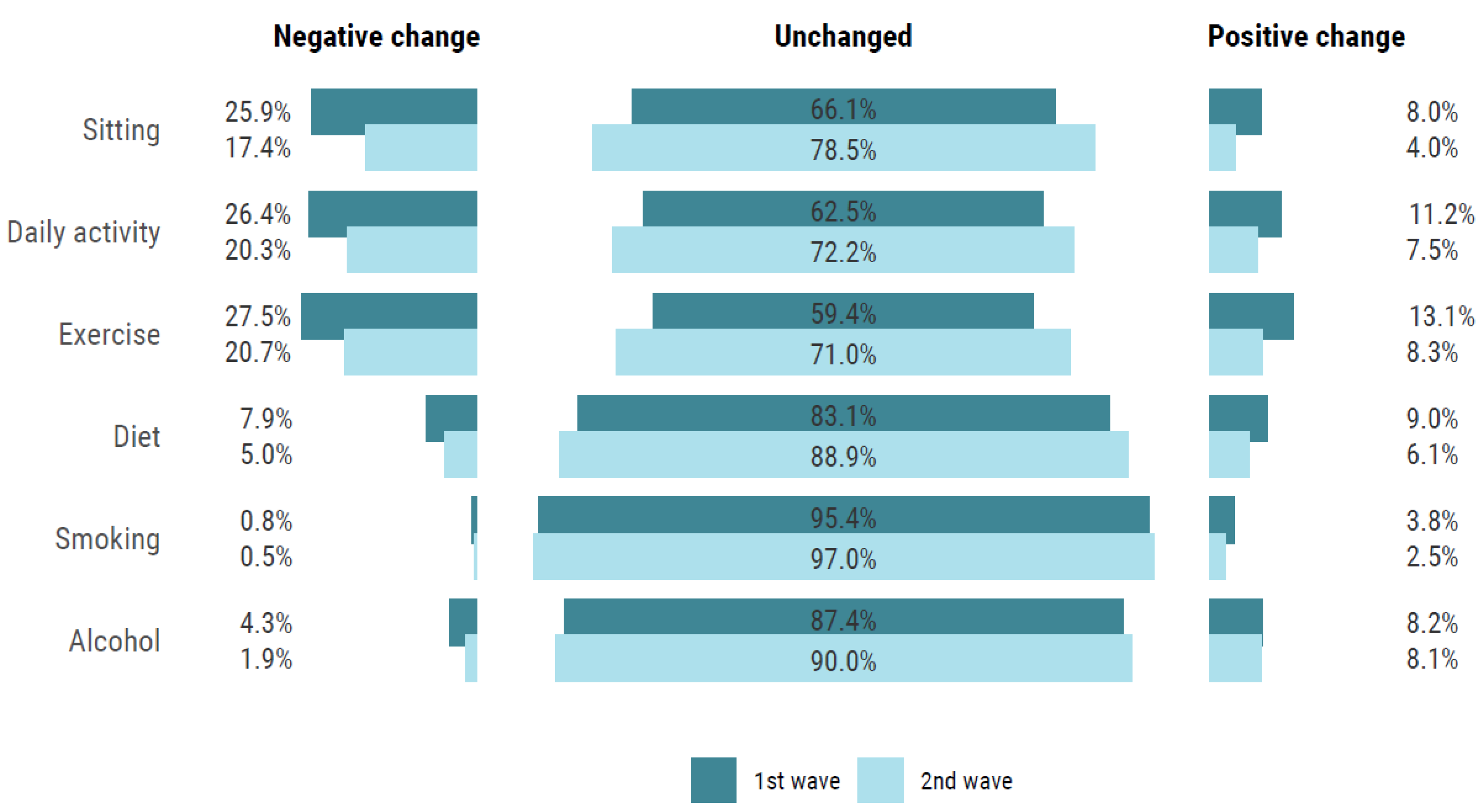
3.2. Perceived Changes in Lifestyle Habits
3.3. Mental Health Experiences
3.4. Type of Sitting and Change in Lifestyle Habits in Relation to Mental Ill-Health
4. Discussion
4.1. Changes in Lifestyle Habits in Sweden Compared to Other Countries
4.2. Changes in Mental Health in Sweden Compared to Other Countries
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Sitting | □ Increased | □ Unchanged | □ Decreased |
| Daily activity | □ Decreased | □ Unchanged | □ Increased |
| Exercise | □ Decreased | □ Unchanged | □ Increased |
| Diet | □ Worsened | □ Unchanged | □ Improved |
| Alcohol intake | □ Increased | □ Unchanged | □ Decreased |
| Smoking | □ Increased | □ Unchanged | □ Decreased |
Appendix B
| HPA Year 2019 | HPA Year 2020 | Difference | |
|---|---|---|---|
| n | 20,864 | 11,844 | |
| Sex (women) | 39% | 41% | 0.005 |
| Age (year) | 44.4 (11.8) | 45.6 (11.4) | <0.001 |
| Estimated VO2max (ml/min/kg) | 35.9 (9.8) | 35.9 (9.8) | 0.781 |
| BMI (kg/m2) | 26.4 (4.6) | 26.5 (4.7) | 0.021 |
| Exercise (Never/irregular) | 30% | 26% | <0.001 |
| Sitting at work (All the time/75% of the time) | 38% | 36% | <0.001 |
| Sitting in leisure (All the time/75% of the time) | 10% | 9% | 0.174 |
| University degree | 28% | 29% | 0.036 |
| Occupation group (Blue collar) | 31% | 29% | 0.003 |
| Diet (Very poor/poor) | 5% | 4% | <0.001 |
| Alcohol risk consumption (AUDIT-C score >3 women, >4 men) | 34% | 34% | 0.220 |
| Daily smoker (≥1 cig/day) | 7% | 6% | 0.003 |
| Overall stress (Very often/often) | 13% | 12% | 0.001 |
| Perceived symptoms of anxiety and depression (Very often/often) | 8% | 8% | 0.623 |
| Data presented as mean (SD) or percentage |
| Alcohol Intake (n = 2790) | Decreased | Increased |
|---|---|---|
| Women vs. Men | 0.70 (0.45–1.09) | 1.13 (0.83–1.53) |
| 18–59 years vs. 60–78 years | 2.31 (0.93–5.79) | 2.00 (1.13–3.57) |
| University vs. non-university | 1.09 (0.69–1.72) | 1.12 (0.82–1.53) |
| White collar vs. Blue collar | 2.16 (1.06–4.40) | 0.99 (0.66–1.48) |
| April–June vs. July–September | 2.22 (1.36–3.63) | 1.08 (0.76–1.55) |
| October–December vs. July–September | 0.94 (0.53–1.67) | 1.10 (0.79–1.54) |
| No alcohol risk consumption vs. Alcohol risk consumption | 0.16 (0.08–0.31) | 0.92 (0.68–1.23) |
References
- Kesaniemi, Y.K.; Danforth, E., Jr.; Jensen, M.D.; Kopelman, P.G.; Lefèbvre, P.; A Reeder, B. Dose-response issues concerning physical activity and health: An evidence-based symposium. Med. Sci. Sports Exerc. 2001, 33 (Suppl. 6), S351–S358. [Google Scholar] [CrossRef]
- Klatsky, A.L. Alcohol and cardiovascular diseases: Where do we stand today? J. Intern. Med. 2015, 278, 238–250. [Google Scholar] [CrossRef] [Green Version]
- Mente, A.; De Koning, L.; Shannon, H.S.; Anand, S.S. A Systematic Review of the Evidence Supporting a Causal Link Between Dietary Factors and Coronary Heart Disease. Arch. Intern. Med. 2009, 169, 659–669. [Google Scholar] [CrossRef] [Green Version]
- Godtfredsen, N.S.; Prescott, E. Benefits of smoking cessation with focus on cardiovascular and respiratory comorbidities. Clin. Respir. J. 2011, 5, 187–194. [Google Scholar] [CrossRef]
- Ng, Q.X.; Ho, C.Y.X.; Chan, H.W.; Yong, B.Z.J.; Yeo, W.-S. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: A systematic review. Complement. Ther. Med. 2017, 34, 123–128. [Google Scholar] [CrossRef]
- Rodriguez-Ayllon, M.; Cadenas-Sánchez, C.; Estévez-López, F.; Muñoz, N.E.; Mora-Gonzalez, J.; Migueles, J.H.; Molina-García, P.; Henriksson, H.; Mena-Molina, A.; Martínez-Vizcaíno, V.; et al. Role of Physical Activity and Sedentary Behavior in the Mental Health of Preschoolers, Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 1383–1410. [Google Scholar] [CrossRef] [PubMed]
- Cheval, B.; Sivaramakrishnan, H.; Maltagliati, S.; Fessler, L.; Forestier, C.; Sarrazin, P.; Orsholits, D.; Chalabaev, A.; Sander, D.; Ntoumanis, N.; et al. Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland. J. Sports Sci. 2020, 2020, 1–6. [Google Scholar] [CrossRef]
- Constandt, B.; Thibaut, E.; De Bosscher, V.; Scheerder, J.; Ricour, M.; Willem, A. Exercising in Times of Lockdown: An Analysis of the Impact of COVID-19 on Levels and Patterns of Exercise among Adults in Belgium. Int. J. Environ. Res. Public Health 2020, 17, 4144. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef] [PubMed]
- Bin Zarah, A.; Enriquez-Marulanda, J.; Andrade, J.M. Relationship between Dietary Habits, Food Attitudes and Food Security Status among Adults Living within the United States Three Months Post-Mandated Quarantine: A Cross-Sectional Study. Nutrients 2020, 12, 3468. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Poelman, M.P.; Gillebaart, M.; Schlinkert, C.; Dijkstra, S.C.; Derksen, E.; Mensink, F.; Hermans, R.C.; Aardening, P.; de Ridder, D.; de Vet, E. Eating behavior and food purchases during the COVID-19 lockdown: A cross-sectional study among adults in the Netherlands. Appetite 2021, 157, 105002. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Błaszczyk-Bębenek, E.; Jagielski, P.; Bolesławska, I.; Jagielska, A.; Nitsch-Osuch, A.; Kawalec, P. Nutrition Behaviors in Polish Adults before and during COVID-19 Lockdown. Nutrients 2020, 12, 3084. [Google Scholar] [CrossRef]
- Zajacova, A.; Jehn, A.; Stackhouse, M.; Denice, P.; Ramos, H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: A cross-sectional analysis. Can. J. Public Health 2020, 111, 953–962. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.D.; Hammarberg, K.; Kirkman, M.; Nguyen, H.T.M.; Fisher, J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J. Affect. Disord. 2020, 277, 810–813. [Google Scholar] [CrossRef]
- Cancello, R.; Soranna, D.; Zambra, G.; Zambon, A.; Invitti, C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int. J. Environ. Res. Public Health 2020, 17, 6287. [Google Scholar] [CrossRef]
- Elbay, R.Y.; Kurtulmuş, A.; Arpacıoğlu, S.; Karadere, E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020, 290, 113130. [Google Scholar] [CrossRef]
- Duncan, G.E.; Avery, A.R.; Seto, E.; Tsang, S. Perceived change in physical activity levels and mental health during COVID-19: Findings among adult twin pairs. PLoS ONE 2020, 15, e0237695. [Google Scholar] [CrossRef]
- Jacob, L.; Tully, M.A.; Barnett, Y.; Lopez-Sanchez, G.F.; Butler, L.; Schuch, F.; López-Bueno, R.; McDermott, D.; Firth, J.; Grabovac, I.; et al. The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Ment. Health Phys. Act. 2020, 19, 100345. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Hallgren, M.; Owen, N.; Stubbs, B.; Zeebari, Z.; Vancampfort, D.; Schuch, F.; Bellocco, R.; Dunstan, D.; Lagerros, Y.T. Passive and mentally-active sedentary behaviors and incident major depressive disorder: A 13-year cohort study. J. Affect. Disord. 2018, 241, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Salkovskis, P.M.; A Rimes, K.; Warwick, H.M.C.; Clark, D.M. The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol. Med. 2002, 32, 843–853. [Google Scholar] [CrossRef]
- Vander Elst, T.D.W.H.; De Cuyper, N. The Job Insecurity Scale: A psychometric evaluation across five European countries. Eur. J. Work Organ. Psychol. 2014, 23, 364–380. [Google Scholar] [CrossRef]
- Statistics Sweden. Levnadsförhållanden 1980–2016—Ett Urval av Indikatorer Living [Conditions 1980–2016—A Selection of Indicators]. Available online: https://www.scb.se/publikation/33620 (accessed on 2 March 2018). (In Swedish)
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Astrand, I. Aerobic work capacity in men and women with special reference to age. Acta Physiol. Scand. Suppl. 1960, 49, 1–92. [Google Scholar]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De La Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Stastistics Sweden. Standard för Svensk Yrkesklassificering (SSYK) [Standard for Swedish Occupational Classification (SSYK)]. Available online: http://www.scb.se/dokumentation/klassifikationer-och-standarder/standard-for-svenskyrkesklassificering-ssyk/ (accessed on 18 March 2020). (In Swedish)
- Public health Agency of Sweden. Bekräftade fall i Sverige—Daglig Uppdatering [Confirmed Cases in Sweden -Daily Uppdate]. Available online: https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/bekraftade-fall-i-sverige/ (accessed on 3 December 2020). (In Swedish).
- Wickham, H.A.M.; Bryan, J.; Chang, W.; D’Agostino McGowan, L.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; Kuhn, M.; et al. Welcome to the Tidyverse. J. Open Source Softw. 2019, 4, 43. [Google Scholar] [CrossRef]
- Public Health Agency of Sweden. Hälsorapport Maj 2020 [Health report May 2020]. Available online: https://halsorapport.se/sv/resultat/resultat-maj-2020/ (accessed on 4 January 2021). (In Swedish).
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef]
- Hallgren, M.; Nguyen, T.-T.-D.; Owen, N.; Vancampfort, D.; Dunstan, D.W.; Wallin, P.; Andersson, G.; Ekblom-Bak, E. Associations of sedentary behavior in leisure and occupational contexts with symptoms of depression and anxiety. Prev. Med. 2020, 133, 106021. [Google Scholar] [CrossRef]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef]
- Stastistics Sweden. En Av Tre Jobbar Hemifrån [One out of Three Works from Home]. Available online: https://www.scb.se/om-scb/nyheter-och-pressmeddelanden/en-tre-av-jobbar-hemifran/ (accessed on 4 February 2021). (In Swedish)
- Jackson, S.E.; Garnett, C.; Shahab, L.; Oldham, M.; Brown, J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: An analysis of 2019–2020 data. Addiction 2020. [Google Scholar] [CrossRef]
- Amarantou, V.; Kazakopoulou, S.; Chatzoudes, D.; Chatzoglou, P. Resistance to change: An em-pirical investigation of its antecedents. J. Organ. Chang. Manag. 2018, 31, 1. [Google Scholar]
- Abramson, J.L.; Vaccarino, V. Relationship Between Physical Activity and Inflammation Among Apparently Healthy Middle-aged and Older US Adults. Arch. Intern. Med. 2002, 162, 1286–1292. [Google Scholar] [CrossRef] [Green Version]
- Smith, L.; Jacob, L.; Yakkundi, A.; McDermott, D.; Armstrong, N.C.; Barnett, Y.; López-Sánchez, G.F.; Martin, S.; Butler, L.; A Tully, M. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: A cross-sectional study of UK-based respondents. Psychiatry Res. 2020, 291, 113138. [Google Scholar] [CrossRef]
- Ainsworth, B.; Cahalin, L.; Buman, M.; Ross, R. The Current State of Physical Activity Assessment Tools. Prog. Cardiovasc. Dis. 2015, 57, 387–395. [Google Scholar] [CrossRef]
- Olsson, S.J.G.; Ekblom, Ö.; Andersson, E.; Börjesson, M.; Kallings, L.V. Categorical answer modes provide superior validity to open answers when asking for level of physical activity: A cross-sectional study. Scand. J. Public Health 2016, 44, 70–76. [Google Scholar] [CrossRef] [PubMed]

| Title | HPA + COVID-19 Data | Only HPA Data | p-Value |
|---|---|---|---|
| n | 5599 | 6232 | |
| Sex (women) | 50% | 33% | <0.001 |
| Age (year) | 46.3 (11.0) | 44.9 (11.6) | <0.001 |
| Estimated VO2max (ml/min/kg) | 36.0 (9.4) | 35.8 (10.0) | 0.518 |
| BMI (kg/m2) | 26.1 (4.5) | 26.7 (4.8) | <0.001 |
| Exercise habits (never/irregular) | 24% | 27% | <0.001 |
| Sitting at work (all the time/75% of the time) | 45% | 30% | <0.001 |
| Sitting in leisure (all the time/75% of the time) | 10% | 9% | 0.101 |
| University degree | 35% | 23% | <0.001 |
| Occupation group (blue collar) | 18% | 39% | <0.001 |
| Diet habits (very poor/poor) | 4% | 4% | 0.060 |
| Alcohol abuse (AUDIT-C score >4 women, >5 men) | 35% | 33% | 0.017 |
| Daily smoker (≥1 cig/day) | 3% | 7% | <0.001 |
| Overall stress (very often/often) | 13% | 11% | 0.001 |
| Perceived symptoms of anxiety and depression (very often/often) | 9% | 7% | 0.002 |
| Total | Men | Women | 18–59 Years | 60–78 Years | White-Collar | Blue-Collar | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Do you work from home? | ||||||||||
| All the time | 10% | 10% | 10% | 10% | 8% | 12% | 1% | |||
| Partly | 26% | 27% | 25% | 27% | 20% | 30% | 5% | |||
| My occupation requires that I am at work | 49% | 47% | 52% | 48% | 58% | 41% | 90% | |||
| I can work at home, but chose to be at work | 15% | 17% | 13% | p < 0.001 | 15% | 15% | p < 0.001 | 18% | 4% | p < 0.001 |
| How have your commuting habits to and from work changed due to the COVID-19 pandemic? | ||||||||||
| Same as before | 74% | 75% | 73% | 74% | 76% | 70% | 91% | |||
| Changed | 11% | 9% | 12% | 10% | 12% | 12% | 5% | |||
| Stopped commuting | 15% | 16% | 15% | p = 0.004 | 16% | 12% | p = 0.010 | 18% | 4% | p < 0.001 |
| If changed, how have they changed? | ||||||||||
| Bus/train to active commuting | 26% | 21% | 30% | 26% | 29% | 26% | 19% | |||
| Bus/train to car | 54% | 57% | 52% | 55% | 51% | 55% | 57% | |||
| Car to active commuting | 8% | 12% | 6% | 8% | 11% | 9% | 8% | |||
| Car to bus/train | 2% | 0% | 3% | 2% | 1% | 2% | 0% | |||
| Active commuting to car | 8% | 9% | 8% | 8% | 7% | 8% | 11% | |||
| Active commuting to bus/train | 2% | 1% | 2% | p = 0.009 | 2% | 1% | p = 0.930 | 1% | 5% | p = 0.232 |
| Type of sitting at home | ||||||||||
| Mentally passive (min/day) | 119 (78) | 127 (82) | 112 (73) | p < 0.001 | 119 (77) | 122 (84) | p = 0.424 | 115 (74) | 134 (87) | p < 0.001 |
| Mentally active (min/day) | 131 (174) | 124 (167) | 139 (179) | p = 0.001 | 134 (177) | 114 (143) | p = 0.002 | 144 (182) | 70 (107) | p < 0.001 |
| Socializing (min/day) | 82 (68) | 84 (68) | 81 (68) | p = 0.006 | 83 (69) | 79 (62) | p = 0.173 | 81 (64) | 85 (83) | p = 0.145 |
| Negative Change in Lifestyle Habits OR (95% CI) | Positive Change in Lifestyle Habits OR (95% CI) | |
|---|---|---|
| Clustering of change in lifestyle habits § | Negative change in 2 or more vs. less | Positive change in 2 or more vs. less |
| Women vs. Men | 1.25 (1.03–1.52) | 1.12 (0.91–1.38) |
| 18–59 y vs. 60–78 y | 1.33 (0.97–1.83) | 1.99 (1.34–2.95) |
| University vs. non-university | 1.30 (1.07–1.58) | 1.10 (0.89–1.36) |
| White collar vs. Blue collar | 1.67 (1.21–2.30) | 1.74 (1.25–2.43) |
| April–June vs. July–September | 1.99 (1.55–2.55) | 1.21 (0.94–1.56) |
| October–December vs. July–September | 1.39 (1.11–1.75) | 0.73 (0.58–0.93) |
| Time spent sitting (n = 4590) | Increased | Decreased |
| Women vs. Men | 1.01 (0.86–1.19) | 1.12 (0.84–1.48) |
| 18–59 y vs. 60–78 y | 1.36 (1.04–1.77) | 0.92 (0.62–1.38) |
| University vs. non-university | 1.61 (1.37–1.90) | 1.17 (0.88–1.55) |
| White collar vs. Blue collar | 1.75 (1.35–2.28) | 2.44 (1.47–4.04) |
| Low/moderate vs. high leisure time sitting * | 0.63 (0.49–0.80) | 1.14 (0.69–1.89) |
| April–June vs. July–September | 2.70 (2.20–3.32) | 2.19 (1.58–3.04) |
| October–December vs. July–September | 1.50 (1.24–1.82) | 0.79 (0.56–1.10) |
| Daily activity (n = 4576) | Decreased | Increased |
| Women vs. Men | 1.38 (1.17–1.61) | 1.06 (0.85–1.32) |
| 18–59 y vs. 60–78 y | 0.90 (0.71–1.12) | 1.48 (1.02–2.15) |
| University vs. non-university | 1.10 (0.93–1.29) | 1.05 (0.84–1.31) |
| White collar vs. Blue collar | 1.08 (0.86–1.36) | 2.03 (1.41–2.91) |
| Low/moderate vs. high leisure time sitting * | 0.65 (0.52–0.82) | 1.72 (1.11–2.68) |
| April–June vs. July–September | 2.19 (1.80–2.68) | 1.47 (1.13–1.91) |
| October–December vs. July–September | 1.45 (1.21–1.74) | 0.74 (0.58–0.95) |
| Exercise (n = 4591) | Decreased | Increased |
| Women vs. Men | 1.36 (1.16–1.60) | 1.03 (0.84–1.27) |
| 18–59 y vs. 60–78 y | 1.00 (0.79–1.25) | 1.29 (0.91–1.83) |
| University vs. non-university | 1.00 (0.85–1.18) | 1.12( 0.91–1.38) |
| White collar vs. Blue collar | 1.16 (0.93–1.46) | 1.93 (1.36–2.74) |
| ≥3 times/week of exercise vs. less | 0.65 (0.53–0.79) | 4.38 (3.07–6.23) |
| 1–2 times/week of exercise vs. less | 1.67 (1.38–2.02) | 2.46 (1.67–3.64) |
| April–June vs. July–September | 2.39 (1.95–2.92) | 1.38 (1.08–1.77) |
| October–December vs. July–September | 1.50 (1.25–1.80) | 0.67 (0.53–0.85) |
| Diet (n = 4579) | Impaired | Improved |
| Women vs. Men | 1.17 (0.89–1.54) | 1.16 (0.91–1.48) |
| 18–59 y vs. 60–78 y | 1.39 (0.88–2.21) | 1.78 (1.15–2.76) |
| University vs. non-university | 1.27 (0.97–1.67) | 1.04 (0.81–1.33) |
| White collar vs. Blue collar | 1.93 (1.22–3.06) | 1.91 (1.27–2.86) |
| Good vs. poor diet # | 0.19 (0.13–0.30) | 1.12 (0.54–2.32) |
| April–June vs. July–September | 2.02 (1.45–2.81) | 1.27 (0.95–1.69) |
| October–December vs. July–September | 1.08 (0.78–1.50) | 0.71 (0.54–0.94) |
| Alcohol intake (n = 5171) | Decreased | Increased |
| Women vs. Men | 0.60 (0.41–0.86) | 0.90 (0.72–1.13) |
| 18–59 y vs. 60–78 y | 1.99 (1.01–3.95) | 2.65 (1.68–4.20) |
| University vs. non-university | 1.07 (0.74–1.55) | 1.04 (0.83–1.30) |
| White collar vs. Blue collar | 1.24 (0.76–2.02) | 1.04 (0.77–1.41) |
| April–June vs. July–September | 1.93 (1.27–2.92) | 1.18 (0.89–1.58) |
| October–December vs. July–September | 0.85 (0.56–1.30) | 1.14 (0.89–1.44) |
| Smoking (n = 4505) | Decreased | Increased |
| Women vs. Men | 1.28 (0.47–3.48) | 1.42 (0.96–2.11) |
| 18–59 y vs. 60–78 y | - | 1.02 (0.58–1.81) |
| University vs. non-university | 3.14 (1.03–9.53) | 0.77 (0.50–1.19) |
| White collar vs. Blue collar | 0.74 (0.23–2.42) | 0.79 (0.48–1.28) |
| Never/occasionally vs. Daily smoker | 0.00 (0.00–0.01) | 0.23(0.12–0.44) |
| Occasionally smoker vs. Daily smoker | 0.19 (0.07–0.53) | 1.53 (0.76–3.10) |
| April–June vs. July–September | 2.47 (0.82–7.44) | 1.44 (0.91–2.29) |
| October–December vs. July–September | 1.32 (0.40–4.35) | 1.09 (0.71–1.67) |
| Total | Men | Women | 18–59 Years | 60–78 Years | White-Collar | Blue-Collar | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Health anxiety, own | ||||||||||
| I do not worry | 46% | 52% | 41% | 47% | 45% | 45% | 52% | |||
| I spend a lot/most of the time worrying | 5% | 4% | 6% | p < 0.001 | 5% | 3% | p = 0.010 | 5% | 5% | p < 0.001 |
| Health anxiety, relatives | ||||||||||
| I do not worry | 22% | 27% | 16% | 21% | 25% | 21% | 25% | |||
| I spend a lot/most of the time worrying | 12% | 8% | 15% | p < 0.001 | 12% | 8% | p = 0.002 | 12% | 10% | p = 0.006 |
| Generalized anxiety | ||||||||||
| Not at all | 80% | 85% | 75% | 80% | 81% | 80% | 82% | |||
| More than half of the days/Almost every day | 4% | 3% | 5% | p < 0.001 | 4% | 4% | p = 0.945 | 4% | 3% | p = 0.149 |
| Depression symptoms | ||||||||||
| Not at all | 73% | 80% | 67% | 73% | 78% | 73% | 77% | |||
| More than half of the days/Almost every day | 4% | 3% | 5% | p < 0.001 | 4% | 3% | p = 0.008 | 4% | 4% | p = 0.014 |
| Concerns employment | ||||||||||
| Not at all | 75% | 76% | 74% | 74% | 83% | 75% | 71% | |||
| Worry alot | 5% | 4% | 5% | p = 0.147 | 5% | 4% | p < 0.001 | 4% | 6% | p = 0.019 |
| Concerns economy | ||||||||||
| Not at all | 65% | 66% | 63% | 63% | 76% | 65% | 64% | |||
| Worry a lot | 6% | 5% | 7% | p = 0.003 | 7% | 4% | p < 0.001 | 6% | 6% | p = 0.856 |
| Clustered Risk ≥2 vs. Less * | Frequent Health Anxiety | Anxiety Symptoms | Depression Symptoms | High Concerns Employment | High Concerns Economy | ||
|---|---|---|---|---|---|---|---|
| Own | Relatives | ||||||
| Women vs. Men | 2.32 (1.70–3.17) | 2.15 (1.50–3.07) | 3.06 (2.44–3.84) | 2.60 (1.87–3.63) | 2.69 (1.94–3.72) | 1.48 (1.11–1.97) | 1.56 (1.21–2.00) |
| 18–59 yrs vs. 60–78 yrs | 1.94 (1.15–3.28) | 2.17 (1.13–4.19) | 1.90 (1.33–2.72) | 1.12 (0.71–1.75) | 1.83 (1.07–3.14) | 1.50 (0.97–2.34) | 1.88 (1.25–2.83) |
| University vs. non-university | 0.82 (0.61–1.11) | 1.30 (0.91–1.86) | 0.87 (0.69–1.09) | 0.73 (0.53–1.01) | 0.89 (0.65–1.21) | 0.68 (0.50–0.92) | 0.64 (0.49–0.83) |
| White collar vs. Blue collar | 0.94 (0.62–1.44) | 0.67 (0.42–1.08) | 0.93 (0.68–1.26) | 1.05 (0.66–1.67) | 0.74 (0.49–1.13) | 0.69 (0.48–0.98) | 0.93 (0.67–1.29) |
| April-June vs. July-Sept | 1.49 (1.03–2.16) | 2.17 (1.42–3.34) | 2.87 (2.16–3.81) | 1.18 (0.79–1.78) | 1.63 (1.11–2.40) | 0.93 (0.64–1.33) | 1.36 (0.99–1.86) |
| October-December vs. July–September | 1.39 (0.99–1.93) | 1.44 (0.97–2.13) | 1.32 (1.04–1.69) | 1.30 (0.93–1.81) | 1.34 (0.96–1.89) | 0.91 (0.67–1.22) | 1.17 (0.89–1.54) |
| Perceived good health vs. poor health | 0.11 (0.08–0.14) | 0.02 (0.01–0.03) | |||||
| Time in mentally passive sitting | |||||||
| T1; 0 to 90 min/day | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| T2; 90 to 120 min/day | 0.89 (0.62–1.27) | 1.36 (0.90–2.05) | 1.51 (1.14–1.99) | 1.05 (0.69–1.59) | 0.89 (0.57–1.38) | 1.24 (0.85–1.80) | 1.44 (1.04–1.99) |
| T3; >120 min day | 1.59 (1.12–2.25) | 1.82 (1.19–2.80) | 2.00 (1.48–2.71) | 1.62 (1.07–2.46) | 1.67 (1.10–2.52) | 1.77 (1.21–2.58) | 2.09 (1.50–2.92) |
| Time in mentally active sitting | |||||||
| Tertile 1; 0 to 30 min/day | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Tertile 2; 30 to 90 min/day | 0.98 (0.67–1.34) | 1.06 (0.69–1.61) | 1.09 (0.82–1.45) | 1.10 (0.73–1.66) | 0.88 (0.58–1.35) | 0.93 (0.65–1.32) | 0.83 (0.61–1.14) |
| Tertile 3; >90 min/day | 1.15 (0.82–1.60) | 1.36 (0.91–2.04) | 1.27 (0.96–1.67) | 1.27 (0.85–1.89) | 1.15 (0.78–1.71) | 1.08 (0.76–1.54) | 1.03 (0.76–1.40) |
| Time in sitting socializing | |||||||
| Tertile 1; 0 to 60 min/day | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Tertile 2; 60 to 90 min/day | 0.93 (0.45–1.90) | 1.13 (0.53–2.42) | 0.93 (0.54–1.61) | 0.72 (0.30–1.71) | 0.73 (0.30–1.78) | 0.70 (0.30–1.62) | 0.68 (0.33–1.42) |
| Tertile 3; >90 min/day | 1.01 (0.75–1.36) | 0.91 (0.64–1.29) | 1.13 (0.89–1.43) | 0.81 (0.56–1.17) | 0.74 (0.51–1.07) | 1.17 (0.86–1.59) | 0.85 (0.65–1.13) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blom, V.; Lönn, A.; Ekblom, B.; Kallings, L.V.; Väisänen, D.; Hemmingsson, E.; Andersson, G.; Wallin, P.; Stenling, A.; Ekblom, Ö.; et al. Lifestyle Habits and Mental Health in Light of the Two COVID-19 Pandemic Waves in Sweden, 2020. Int. J. Environ. Res. Public Health 2021, 18, 3313. https://doi.org/10.3390/ijerph18063313
Blom V, Lönn A, Ekblom B, Kallings LV, Väisänen D, Hemmingsson E, Andersson G, Wallin P, Stenling A, Ekblom Ö, et al. Lifestyle Habits and Mental Health in Light of the Two COVID-19 Pandemic Waves in Sweden, 2020. International Journal of Environmental Research and Public Health. 2021; 18(6):3313. https://doi.org/10.3390/ijerph18063313
Chicago/Turabian StyleBlom, Victoria, Amanda Lönn, Björn Ekblom, Lena V. Kallings, Daniel Väisänen, Erik Hemmingsson, Gunnar Andersson, Peter Wallin, Andreas Stenling, Örjan Ekblom, and et al. 2021. "Lifestyle Habits and Mental Health in Light of the Two COVID-19 Pandemic Waves in Sweden, 2020" International Journal of Environmental Research and Public Health 18, no. 6: 3313. https://doi.org/10.3390/ijerph18063313
APA StyleBlom, V., Lönn, A., Ekblom, B., Kallings, L. V., Väisänen, D., Hemmingsson, E., Andersson, G., Wallin, P., Stenling, A., Ekblom, Ö., Lindwall, M., Salier Eriksson, J., Holmlund, T., & Ekblom-Bak, E. (2021). Lifestyle Habits and Mental Health in Light of the Two COVID-19 Pandemic Waves in Sweden, 2020. International Journal of Environmental Research and Public Health, 18(6), 3313. https://doi.org/10.3390/ijerph18063313