1. Introduction
When severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first discovered in Wuhan (China) in December 2019, even the most qualified experts did not anticipate that it would rapidly spread to create the worst global public health crisis since the 1918 flu pandemic [
1]. The total number of COVID-19 cases in the world is counted in the tens of millions, with deaths in over two million cases. It is well known that emerging viral pandemics “can place extraordinary and sustained demands on public health and healthcare systems and on providers of essential community services” [
2]. A crisis such as the current COVID-19 pandemic is a dramatic event, which takes place in a difficult environment with enormous emotional tension, coupled with a serious disproportion between needs and available resources. In these circumstances, managing healthcare services is a constant and changing challenge [
3]. Therefore, flexibility in the usage of hospital beds is a crucial element for efficiently organizing critical capacity [
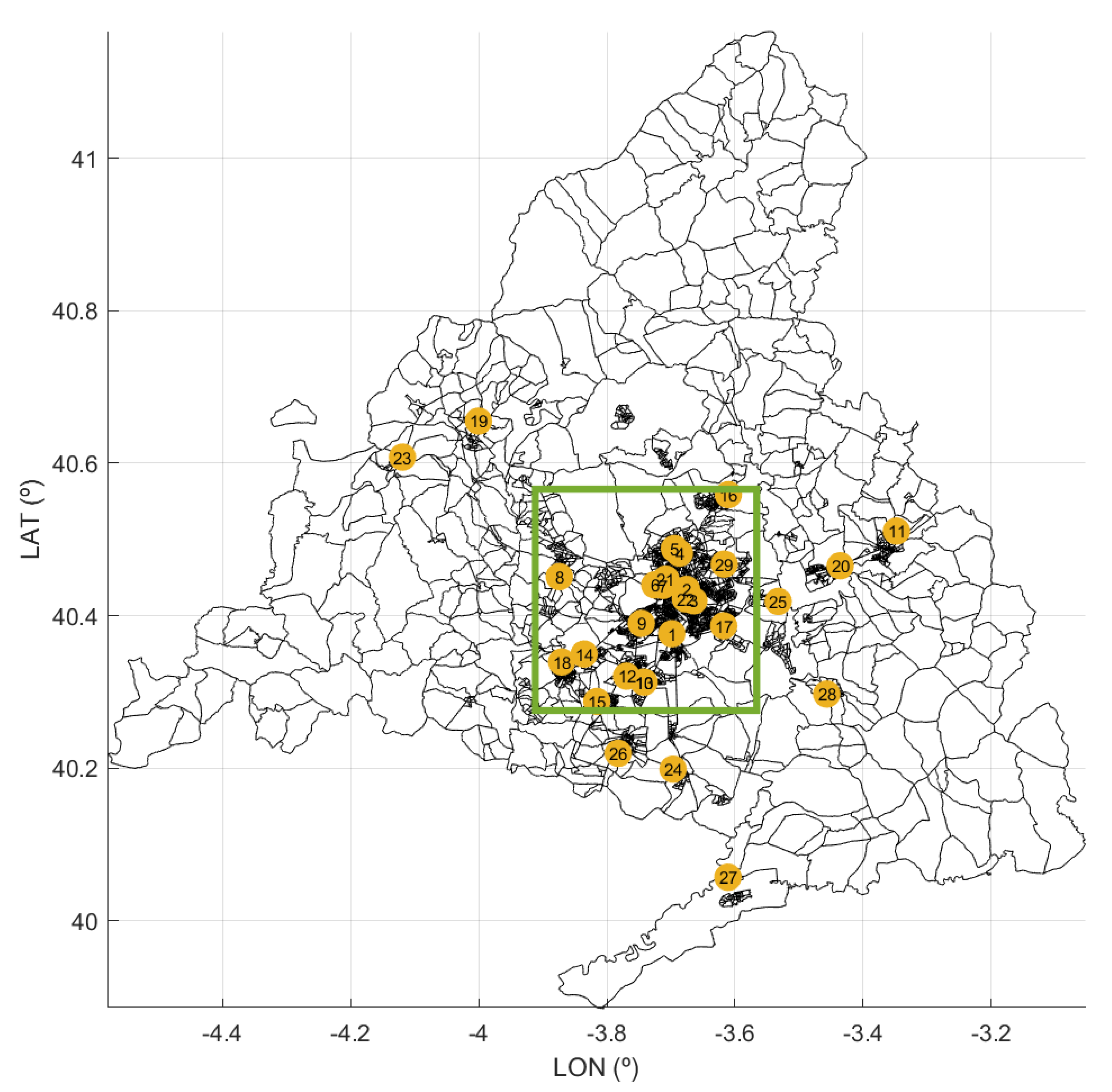
4]. In Spain, as in many other countries, in the spring of 2020, COVID-19 produced such a significant number of seriously ill patients that the healthcare system almost collapsed. In some of its Autonomous Communities (ACs), particularly in the Autonomous Community of Madrid (CoM), where the capital of Spain (Madrid city) is located, the situation was especially pronounced.
Thus, on 31 March, at least 450,611 cases had been reported in Europe. The CoM registered a cumulative incidence in the previous 14 days of 363.22 and Spain registered 192.3, followed by Italy (122.2), Belgium (103), France (56.6), and the UK (40). The accumulated cases in the CoM were 29,840, 29% those of all of Spain (102.136). The highest fatality rate in Europe was in Italy (11.7), followed by Spain with 8.9, while in the CoM, it reached 13 (46% higher). In the CoM, the deaths per 100,000 inhabitants amounted to 57.7, tripling that of Spain (17.3), which was followed by Belgium (14.8), Italy (13.4), France (6.24), and the UK (5.6). The accumulated deaths in the CoM (3865) represented 42.7% of those registered in Spain (9053) [
5,
6]. If we look at the situation of beds in the CoM’s hospitals to describe their evolution, which is the main objective of this paper, it can be seen that the number of patients hospitalized just for COVID-19 in the intensive care units (ICUs) was 1514, and 13,713 patients were in beds other than intensive care (non-ICU). However, the situation can be described even better by comparing the figures of the CoM beds with those of Spain: 5872 (ICU) and 45,546 (non-ICU) [
5]; Italy: 4023 (ICU) and 32,215 (non-ICU); France: 5496 (ICU) and 22,672 (non-ICU); and Belgium: 1088 (ICU) and 4989 (non-ICU) [
7].
Due to the need to hospitalize a huge number of COVID-19 patients, which increased relentlessly with different degrees of severity during this first wave, the CoM’s hospitals rapidly increased their capacity to levels never seen before. Not only the number of hospital beds, but also the intensive support and invasive ventilation were of concern, as COVID-19 is a disease with a potentially fatal evolution. These circumstances meant that the number of available beds had to be increased from 18,692 (18 March 2020) to 23,623 (2 April 2020) in just 15 days, i.e., an increment of 26.4%. Although the first admission for COVID-19 in a CoM hospital occurred on 25 February 2020, in this paper, we analyze the data for the period between 18 March 2020 and 31 May 2020. The first date corresponds to the first day on which we had the complete data of the hospitals that are analyzed in this article.
The COVID-19 pandemic, as mentioned above, forced the CoM’s hospitals to increase the number of available beds. Given the shortage of papers in the world on the capacities of hospitals to increase their numbers of beds with the speed required by a pandemic wave, the aim of this article is to set dynamic performance indicators in order to model the dynamic response in terms of the number of available beds instead of using more stationary approaches. For this purpose, not only are specific visualization graphs used to show the daily evolution of the variables under consideration, such as the bed margin of the CoM’s hospitals, but a new set of indexes for quantifying their flexibility and a robust estimation method are proposed. Thus, the proposed approach to analyzing and quantifying the dynamics related to flexibility could be used for further analysis and as a reference for decision making not only at the hospital level, but also from a centralized or global perspective.
The remainder of this paper is structured as follows.
Section 2 describes the materials and methods, and it is composed of three parts: (i) the healthcare system of the hospital network in the CoM; (ii) the data and the variables used in our study; and (iii) the methodology, where the proposed concepts of the bed margin and flexibility are defined. The results are presented in
Section 3, first as an aggregate view of the healthcare system, and second as disaggregated view by hospital. Finally,
Section 4 contains a discussion of the results, and conclusions and directions for future work are provided in
Section 5.
4. Discussion
Analyzing healthcare data through the first wave of SARS-CoV-2 has brought up an opportunity to better understand hospital performance under these severe circumstances. Specifically, by analyzing the flexibility and bed margin, it is possible to dynamically graph—as an alternative or complement to other, more static models—not only the day-to-day response of the system as a whole for all of the hospitals within the CoM region, but also the response of each hospital (
Figure 9 and
Figure 10). These graphs provide information for hospital managers and healthcare system supervisors, since they can check (in a dynamic way) certain situations that are referred to later on.
This paper focuses on modeling the hospital capacities in terms of ICU and non-ICU beds during the pandemic while distinguishing between patients with and without COVID-19, since most publications focus on bed management in other contexts [
28,
29,
30,
31,
32,
33] (except for Condes and Arribas [
34] and Fanelli et al. [
35]). We have not found a work in the literature that gives information on this topic with the details and large number of hospital and inpatients that this article uses, highlighting the fact that the hospitals involved in this study were in the epicenter of the first wave of the COVID-19 pandemic at the European level. Therefore, the data presented here could be beneficial in the future in order to compare what happened during the first wave in other healthcare systems and to better prepare in the event new epidemic waves caused by SARS-CoV-2 or other pathogens. Finally, this article shows a way to classify hospitalized patients in pandemic situations and to manage infected and uninfected inpatients. Among other things, this classification makes it possible, with the previously mentioned safeguards, to compare the first wave with the pre-pandemic situation in order to know how many patients could not be admitted to hospitals for diseases other than COVID-19. The previous situation, in our opinion, should be a clear invitation to other researchers to address such a critical scenario when that information is available.
The above-mentioned achievements were obtained by analyzing and extracting information from the available data from the CCC. The relevant figures of the first pandemic wave in the CoM were: From 18 March 2020 to 31 March 2020 (13 days), COVID-19 inpatients increased by 200% in non-ICU wards and by 155% in ICU wards. The maximum occupancy of available beds took place on 31 March 2020. On that day, in all of the hospitals that we analyzed, the total number of available beds was 23,463, of which 21,549 (92%) were occupied. The capacity in many hospitals was exhausted, but the fear that the demand would continue to increase caused the number of available beds to increase by 160 in 48 h, reaching the figure of 23,623 beds on 2 April 2020, with an occupancy of 90.3%.
The previous paragraph describes the first wave scenario in the CoM. Our analysis, which was focused on the proposed bed margin and flexibility indexes, shows that hospitals adapted to unexpected requirements with different responses. Notice the following fact: All but seven hospitals presented a non-ICU bed margin (
Figure 11, left) lower than 25% for at least 75% of the days, and one of them presented a median bed margin of 1.3% (five beds). Focusing on ICU beds, the lack of unoccupied beds in several hospitals over several days was notorious (
Table 5). For at least 75% of the days, in 14 of the 30 hospitals analyzed, the ICU bed margin was lower than or equal to 15%, and two hospitals lacked free ICU beds. Occupied non-ICU beds and ICU beds did not return to the values of 18 March 2020 until the third week of April and the first week of May, respectively.
Under normal conditions, hospitals sometimes operate with difficulties, especially in emergency departments. Contrary to popular belief, hospitals are complex but vulnerable institutions [
36]. This vulnerability is mainly due to three factors: First, as seen with personal protective equipment and laboratory reagents, they are highly dependent on external supplies. Second, the key staff is highly specialized and is not easy to increase or replace. Third, their infrastructure (beds, doctor offices, medical equipment, etc.) is dimensioned to care for a range of pathologies and a maximum number of patients. Therefore, a modest variation in the admission volume, as happens when the seasonal flu arrives, can lead the hospital beyond its functional reserves.
It is worth noting how unexpected demands cause situations like those shown in
Figure 4 and
Figure 5. These figures compare the beds occupied by patients with or without COVID-19 who were hospitalized inside and outside ICUs. Moreover, they show how the demand for hospitalizations due to COVID-19 severely reduced the hospitals’ capacities to admit new patients with other types of pathologies, especially in the ICUs. Flexibility in available beds is a significant driver for managing hospitals efficiently, and its importance acquires greater relevance in situations such as the COVID-19 pandemic.
Quantifying the flexibility with a regression technique such as the LHM is an attempt to model the dynamic performance from the observed data. More specifically, the LHM was used to obtain a robust estimation of the proposed flexibility indexes by means of the piecewise slope estimations that it provided for the time series of the number of available beds. In particular, the LHM obtained for available non-ICU and ICU beds in the CoM’s whole health system detected several different ramps before and after the peak (see
Figure 8). The reduction of the available beds after the peak is explained easily by the systematic decrease in bed demand. However, the slowdown in the ramp rate of available beds started before the bed demand decreased (see
Figure 5). The systematic reduction in the bed margin before the peak is noticeable for both non-ICU and ICU beds (see
Figure 6); thus, the ramps began to slow down as they approached the peak. The justification is supported by the reduction in bed demand and the system’s limitations for additional capacity when the bed demand was peaking. These limitations show up due to the lack of extra physical space, equipment, and qualified personnel.
The flexibility performance indicators and the LHM model were used in an attempt to provide insights that could help improve the hospitals’ management and decision making. However, it cannot be determined a priori what the optimal level of beds or human resources for facing a pandemic crisis should be. Unfortunately, it is not possible to respond to this question until after a new epidemic wave is addressed.
Figure 9 and
Figure 10 show the supply of and demand for beds. The observed variations can be explained, in a summarized way, by saying that hospitals of high complexity, which are those with more beds, generally fared better than hospitals of lower complexity (which are the ones with the fewest beds). This fact emphasizes the importance of having a real-time control panel that could avoid having hospitals under the pressure of a very narrow bed margin. Distributing inpatients throughout the hospital system can ease the pressure on some hospitals. In this way, two main objectives will be achieved in a very complex environment: avoiding the professionals’ exhaustion and providing the best care to patients. Let us remember that both objectives are intimately interweaved.
This paper focuses on the first wave of the COVID-19 pandemic in a specific geographic area (the CoM in Spain). The proposed model is dynamic (compared to existing static models) and could be used in other geographic regions, as well as in future waves of pandemics or other health crises. The introduction of new mathematical models for emulating the dynamics of a hospital network in terms of capacity, flexibility, and bed margin will pave the way to a better understanding of the impacts of health policies and resource management during health crises. An example of this type of research is the work by Wood [
37], where the ICU capacity of a large British public hospital in the context of COVID-19 was analyzed using public data from the Intensive Care National Audit and Research Centre [
38].
5. Conclusions
The main objective of our study was to analyze the dynamic response of the CoM’s hospitals during the first wave of the SARS-CoV-2 pandemic. In order to carry out this analysis, a set of very informative indicators was proposed. These indexes were able to summarize the observed dynamics of the curve of the available beds during the pandemic in a simple way. In particular, we proposed the bed margin as a useful index of the available resources, as well as three new indicators for capturing the flexibility with respect to the growing demand for beds. The main indicator of flexibility is the Average Ramp Rate Until the Peak (ARRUP), but it cannot be interpreted in isolation. The Ramp Duration Until the Peak (RDUP) and the Ramp Growth Until the Peak (RGUP) provide useful information that allows one to answering questions, such as: For how many days can the observed ramp rate be maintained? What is the maximum number of beds that can be available?
Our results, which are based on the proposed bed margin and flexibility indexes, show that the hospital network in the CoM can increase the number of available ICU beds with a rate of at least 61 beds/day for 10 days. Furthermore, the considered hospitals were able to adapt to unexpected requirements with different responses. This study offers valuable insights concerning not only the system’s response, but also about the individual responses of the CoM’s hospitals.
The proposed indicators are ready to use for monitoring of networks of hospitals. For example, the estimated indexes for a particular hospital during the first pandemic wave can be used as a reference for this hospital, which is useful for monitoring its behavior during a similar pandemic wave. Future research could apply the proposed methodology based on the bed margin and flexibility indexes in order to analyze a health system’s response during other pandemic waves or similar catastrophes. The comparison of our findings during this first wave with those of future responses may provide additional insights. Moreover, due to the existence of particular characteristics of the hospitals that could affect their dynamic responses under these critical circumstances, future research may be developed in order to identify machine learning models that are able to estimate a given hospital’s flexibility as a function of its characteristics.