Public Health Workforce Burnout in the COVID-19 Response in the U.S.
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Mental and Physical Health of Public Health Workers
3.2. Burnout of Public Health Workers
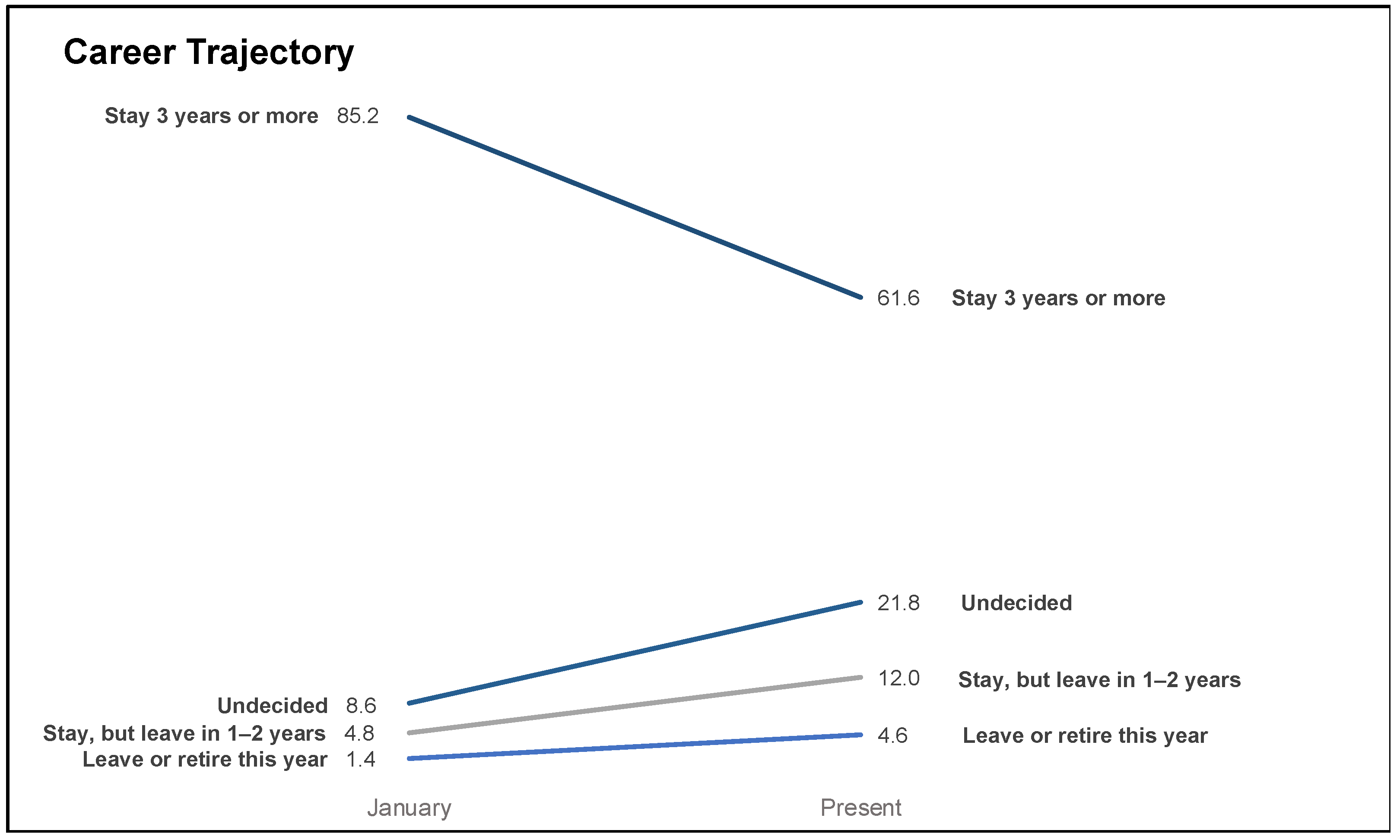
3.3. Impact of COVID on Career Trajectory
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19) Weekly Epidemiological Update; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Harcourt, J.; Tamin, A.; Lu, X.; Kamili, S.; Sakthivel, S.K.; Murray, J.; Queen, K.; Tao, Y.; Paden, C.R.; Zhang, J.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 from Patient with Coronavirus Disease, United States. Emerg. Infect. Dis. 2020, 26, 1266–1273. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins University of Medicine Coronavirus Resource Center. Mortality in the Most Affected Countries. 2020. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 24 September 2020).
- Cai, H.; Tu, B.; Ma, J.; Chen, L.; Fu, L.; Jiang, Y.; Zhuang, Q. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. 2020, 26, e924171. [Google Scholar] [PubMed] [Green Version]
- Felice, C.; Di Tanna, G.L.; Zanus, G.; Grossi, U. Impact of COVID-19 Outbreak on Healthcare Workers in Italy: Results from a National E-Survey. J. Community Health 2020, 45, 675–683. [Google Scholar] [CrossRef]
- García-Fernández, L.; Romero-Ferreiro, V.; López-Roldán, P.D.; Padilla, S.; Calero-Sierra, I.; Monzó-García, M.; Pérez-Martín, J.; Rodriguez-Jimenez, R. Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol. Med. 2020, 26, 1–3. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Naushad, V.A.; Bierens, J.J.; Nishan, K.P.; Firjeeth, C.P.; Mohammad, O.H.; Maliyakkal, A.M.; ChaliHadan, S.; Schreiber, M.D. A Systematic Review of the Impact of Disaster on the Mental Health of Medical Responders. Prehosp. Disaster Med. 2019, 34, 632–643. [Google Scholar] [CrossRef]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef] [PubMed]
- Stuijfzand, S.; Deforges, C.; Sandoz, V.; Sajin, C.-T.; Jaques, C.; Elmers, J.; Horsch, A. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health 2020, 20, 1230. [Google Scholar] [CrossRef]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef]
- Poon, E.; Liu, K.S.; Cheong, D.L.; Lee, C.K.; Yam, L.Y.; Tang, W.N. Impact of severe respiratory syndrome on anxiety levels of front-line health care workers. Hong Kong Med. J. 2004, 10, 325–330. [Google Scholar] [PubMed]
- Maunder, R.G.; Lancee, W.J.; Balderson, K.E.; Bennett, J.P.; Borgundvaag, B.; Evans, S.; Fernandes, C.M.B.; Goldbloom, D.S.; Gupta, M.; Hunter, J.J.; et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006, 12, 1924–1932. [Google Scholar] [CrossRef]
- Center for State and Local Government Excellence. How does The Public Health Workforce Compare with The Broader Public Sector; Center for State and Local Government Excellence: Washington, DC, USA, 2020. [Google Scholar]
- Tilson, H.; Gebbie, K.M. The public health workforce. Annu. Rev. Public Health 2004, 25, 341–356. [Google Scholar] [CrossRef] [Green Version]
- Gebbie, K.M.; Merrill, J.; Tilson, H.H. The public health workforce. Health Aff. 2002, 21, 57–67. [Google Scholar] [CrossRef]
- Beaglehole, R.; Dal Poz, M.R. Public health workfroce: Challenges and policy issues. Hum. Resour. Health 2003, 1, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Association of County and City Health Officials. Changes in Local Health Department Workforce and Finance Capacity since 2008; National Association of County and City Health Officials: Washington, DC, USA, 2019. [Google Scholar]
- Association of State and Territorial Health Officials. New Data on State Health Agencies Show Shrinking Workforce and Decreased Funding Leading Up to COVID-19 Pandemic; Association of State and Territorial Health Officials: Arlington, MA, USA, 2020. [Google Scholar]
- Leider, J.P.; Coronado, F.; Beck, A.J.; Harper, E. Reconciling Supply and Demand for State and Local Public Health Staff in an Era of Retiring Baby Boomers. Am. J. Prev. Med. 2018, 54, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arroll, B.; Goodyear-Smith, F.; Crengle, S.; Gunn, J.; Kerse, N.; Fishman, T.; Falloon, K.; Hatcher, S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Fam. Med. 2010, 8, 348–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dolan, E.D.; Mohr, D.; Lempa, M.; Joos, S.; Fihn, S.D.; Nelson, K.M.; Helfrich, C.D. Using a single item to measure burnout in primary care staff: A psychometric evaluation. J. Gen. Intern. Med. 2015, 30, 582–587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Center for Chronic Disease Prevention and Health Promotion. 2019 BRFSS Questionnaire; National Center for Chronic Disease Prevention and Health Promotion: Atlanta, GA, USA, 2019.
- U.S. Census Bureau. Census Bureau Regions and Divisions with State FIPS Codes; U.S. Census Bureau: Suitland, MD, USA, 1902.
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Halverson, P.K.; Yeager, V.A.; Menachemi, N.; Fraser, M.R.; Freeman, L.T. Public health officials and COVID-19: Leadership, politics, and the pandemic. J. Public Health Manag. Pract. 2021, 27, S11–S13. [Google Scholar] [CrossRef]
- Khaldun, J.S. Public health leadership during a pandemic: Michigan’s experience. J. Public Health Manag. Pract. 2021, 27, S14–S18. [Google Scholar] [CrossRef]
- Flaherty, C. Burning Out. Inside Higher Ed. 2020; Available online: https://www.insidehighered.com/news/2020/09/14/faculty-members-struggle-burnout (accessed on 26 September 2020).
- Makikangas, A.; Kinnunen, U. The person-oriented approach to burnout. Burn. Res. 2016, 3, 11–23. [Google Scholar] [CrossRef] [Green Version]
- Crowe, R.P.; Bower, J.K.; Cash, R.E.; Panchal, A.R.; Rodriguez, S.A. Association of burnout with workforce reducing factors among EMS professionals. Prehops. Emerg. Care 2018, 22, 229–236. [Google Scholar] [CrossRef]
- Coleman, E. Local Health Departments are Understaffed. Would Biden’s ‘Public Health Job Corps’ Help? Available online: https://www.route-fifty.com/health-human-services/2020/12/public-health-jobs-corps/170811/ (accessed on 15 February 2021).
- Bogaert, K.; Castrucci, B.C.; Gould, E.; Sellers, K.; Leider, J.P. Changes in the State Governmental Public Health Workforce: Demographics and Perceptions, 2014–2017. J. Public Health Manag. Pract. 2019, 25, S58–S66. [Google Scholar] [CrossRef]
- Li, J.; Xu, J.; Zhou, H.; You, H.; Wang, X.; Liang, Y.; Li, S.; Ma, L.; Zeng, J.; Cai, H. Working conditions and health status of 6,317 front line public health workers across five provinces in China during the COVID-19 epidemic: A cross sectional study. BMC Public Health 2021, 21, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Scudellari, M. How the pandemic might play out in 2021 and beyond. Nature 2020, 584, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, L.; Silver, G.B.; Helsing, K.; Evashwick, C.; Katz, R.; Klag, M.; Kominski, G.; Richter, D.; Sumaya, C. Confronting the public health workforce Crisis: ASPH Statement on the public health workforce. Public Health Rep. 2008, 123, 395–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Mental Health and Physical Health Outcomes (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Total n (%) | Anxiety Disorder | Depressive Disorder | Anxiety or Depressive Disorder | Burnout | Pool Physical Health Days (Mean) | Poor Mental Health Days (Mean) | Days Poor Mental or Physical Health Kept from Activity (Mean) |
| Total | 225 (100) | 41.0 | 29.1 | 45.6 | 66.2 | 5.0 | 12.4 | 6.7 |
| Gender | ||||||||
| Female | 185 (84.8) | 39.9 | 28.2 | 43.8 | 68.3 | 5.1 | 12.1 | 6.7 |
| Male | 30 (13.8) | 46.7 | 33.3 | 56.7 | 60.0 | 4.8 | 13.7 | 5.8 |
| Other a | <5 | |||||||
| Age (years) | ||||||||
| 18–29 | 46 (20.4) | 50.0 | 34.8 | 58.7 | 73.9 | 4.5 | 14.1 | 7.3 |
| 30–39 | 90 (40.0) | 39.5 | 29.2 | 41.4 | 66.7 | 5.1 | 11.6 | 8.1 |
| 40–49 | 45 (20.0) | 51.2 | 30.9 | 57.1 | 72.1 | 5.9 | 14.4 | 6.0 |
| 50–64 | 38 (16.9) | 27.8 | 24.3 | 33.3 | 56.8 | 4.6 | 11.2 | 3.7 |
| 65+ | 6 (2.7) | 0.0 | 0.0 | 0.0 | 16.7 | 2.7 | 2.8 | 2.2 |
| Race-Ethnicity | ||||||||
| Asian, non-Hispanic | 18 (8.2) | 41.2 | 23.5 | 41.2 | 55.5 | 4.6 | 13.2 | 8.3 |
| Black, non-Hispanic | 6 (2.7) | 0.0 | 0.0 | 0.0 | 33.3 | 8.2 | 3.7 | 3.8 |
| Hispanic, any race(s) | 21 (9.5) | 45.0 | 30.0 | 45.0 | 50.0 | 5.4 | 15.3 | 6.3 |
| White, non-Hispanic | 168 (76.4) | 42.1 | 31.9 | 48.2 | 70.1 | 4.6 | 12.3 | 6.7 |
| Other race or multiple races, non-Hispanic | 7 (3.2) | 42.9 | 14.3 | 42.9 | 71.4 | 7.7 | 11.4 | 3.9 |
| Marital Status | ||||||||
| Now Married/In Partnership | 123 (55.2) | 42.0 | 28.9 | 45.8 | 65.6 | 4.8 | 12.0 | 5.5 |
| Never Married | 77 (34.5) | 42.1 | 30.3 | 48.7 | 71.4 | 4.8 | 13.1 | 8.2 |
| Other b | 23 (10.3) | 25.0 | 23.8 | 28.6 | 47.6 | 5.9 | 9.8 | 8.3 |
| Household Size | ||||||||
| 1 | 52 (23.5) | 42.0 | 33.3 | 51.0 | 75.0 | 4.3 | 11.8 | 8.5 |
| 2 | 80 (36.2) | 45.5 | 31.6 | 48.1 | 68.4 | 4.9 | 13.2 | 7.0 |
| 3 | 40 (18.1) | 41.0 | 30.8 | 48.7 | 59.0 | 5.6 | 12.2 | 5.5 |
| 4+ | 49 (22.2) | 35.4 | 20.8 | 36.2 | 59.2 | 5.4 | 11.9 | 5.3 |
| Experience (years) | ||||||||
| <1 | 21 (9.4) | 42.7 | 28.6 | 47.6 | 38.1 | 4.1 | 12.1 | 9.2 |
| 1–4 | 58 (26.0) | 42.1 | 24.1 | 47.4 | 72.4 | 4.9 | 12.6 | 7.2 |
| 5–9 | 58 (26.0) | 40.0 | 37.5 | 45.5 | 71.9 | 4.8 | 12.1 | 6.7 |
| 10–14 | 34 (15.3) | 40.6 | 26.5 | 45.5 | 67.7 | 5.1 | 11.4 | 7.4 |
| 15+ | 52 (23.3) | 40.4 | 27.5 | 43.1 | 63.5 | 5.4 | 13.1 | 4.7 |
| Public Health Sector | ||||||||
| Public Health Practice | 176 (78.9) | 42.1 | 29.9 | 46.8 | 65.1 | 5.3 | 12.6 | 6.8 |
| Academic | 27 (12.1) | 42.3 | 23.1 | 46.2 | 85.2 | 3.5 | 12.0 | 5.7 |
| Other c | 20 (9.0) | 30.0 | 30.0 | 35.0 | 50.0 | 3.9 | 10.3 | 6.6 |
| Education | ||||||||
| ≤Bachelors | 33 (14.8) | 37.5 | 27.3 | 40.6 | 51.5 | 6.0 | 12.3 | 6.3 |
| Masters | 128 (57.4) | 42.9 | 31.5 | 47.6 | 67.2 | 4.2 | 11.9 | 7.3 |
| Doctoral | 62 (27.8) | 39.0 | 25.0 | 44.1 | 72.1 | 6.0 | 13.3 | 5.5 |
| Characteristic/Experience | Prevalence Ratio (95% CI) | |
|---|---|---|
| Some Level of Burnout | High Level of Burnout | |
| Gender | ||
| Female | Ref | Ref |
| Male | 0.9 (0.6–1.2) | 1.0 (0.5–1.9) |
| Age (years) | ||
| 18–29 | Ref | Ref |
| 30–39 | 0.9 (0.7–1.1) | 1.3 (0.7–2.6) |
| 40–49 | 1.0 (0.8–1.3) | 2.3 (1.2–4.4) |
| 50–64 | 0.8 (0.6–1.1) | 0.7 (0.3–1.9) |
| 65+ | 0.2 (0.0–1.4) | a |
| Race/Ethnicity | ||
| White, non-Hispanic | Ref | Ref |
| Asian, non-Hispanic | 0.8 (0.5–1.2) | 0.2 (0.0–1.3) |
| Black, non-Hispanic | 0.5 (0.2–1.5) | 0.6 (0.9–3.5) |
| Hispanic, any race(s) | 0.7 (0.5–1.1) | 0.7 (0.3–1.7) |
| Other race or multiple races, non-Hispanic | 1.0 (0.6–1.7) | 0.5 (0.1–3.1) |
| Marital Status | ||
| Now Married/In Partnership | Ref | Ref |
| Never Married | 1.1 (0.9–1.3) | 0.6 (0.3–1.1) |
| Other b | 0.7 (0.5–1.2) | 1.2 (0.6–2.3) |
| Household Size | ||
| 1 | Ref | Ref |
| 2 | 0.9 (0.7–1.1) | 1.0 (0.6–2.0) |
| 3 | 0.8 (0.6–1.1) | 1.1 (0.5–2.3) |
| 4+ | 0.8 (0.6–1.1) | 1.2 (0.6–2.4) |
| Experience (years) | ||
| <1 | Ref | Ref |
| 1–4 | 1.9 (1.1–3.4) | 2.7 (0.7–10.9) |
| 5–9 | 1.9 (1.1–3.3) | 2.0 (0.5–8.4) |
| 10–14 | 1.8 (1.0–3.2) | 4.3 (1.1–17.2) |
| 15+ | 1.7 (0.9–3.0) | 2.8 (0.7–11.4) |
| Public Health Sector | ||
| Public Health Practice | Ref | Ref |
| Academic | 1.3 (1.1–1.6) | 1.1 (0.5–2.1) |
| Other c | 0.8 (0.5–1.2) | 1.2 (0.6–2.5) |
| Education | ||
| ≤Bachelors | Ref | Ref |
| Masters | 1.3 (0.9–1.9) | 2.3 (0.9–5.9) |
| Doctoral | 1.4 (1.0–2.0) | 2.3 (0.8–6.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stone, K.W.; Kintziger, K.W.; Jagger, M.A.; Horney, J.A. Public Health Workforce Burnout in the COVID-19 Response in the U.S. Int. J. Environ. Res. Public Health 2021, 18, 4369. https://doi.org/10.3390/ijerph18084369
Stone KW, Kintziger KW, Jagger MA, Horney JA. Public Health Workforce Burnout in the COVID-19 Response in the U.S. International Journal of Environmental Research and Public Health. 2021; 18(8):4369. https://doi.org/10.3390/ijerph18084369
Chicago/Turabian StyleStone, Kahler W., Kristina W. Kintziger, Meredith A. Jagger, and Jennifer A. Horney. 2021. "Public Health Workforce Burnout in the COVID-19 Response in the U.S." International Journal of Environmental Research and Public Health 18, no. 8: 4369. https://doi.org/10.3390/ijerph18084369
APA StyleStone, K. W., Kintziger, K. W., Jagger, M. A., & Horney, J. A. (2021). Public Health Workforce Burnout in the COVID-19 Response in the U.S. International Journal of Environmental Research and Public Health, 18(8), 4369. https://doi.org/10.3390/ijerph18084369






