Climate Change and Mental Health: A Scoping Review
Abstract
:1. Introduction
2. Methods
2.1. Scoping Review
- Must relate to mental health and climate change across one or more of the domains defined by the Lancet Countdown for Health and Climate Change 2018 [11]: climate change impacts, exposures, and vulnerability; adaptation, planning, and resilience for health; mitigation actions and health co-benefits; finance and economics; and public and political engagement
- Must be original research (e.g., cross-sectional or cohort studies)
- Publication year must be from 2001 onwards
- English language
2.2. Quality Assessment
2.3. Research Framework
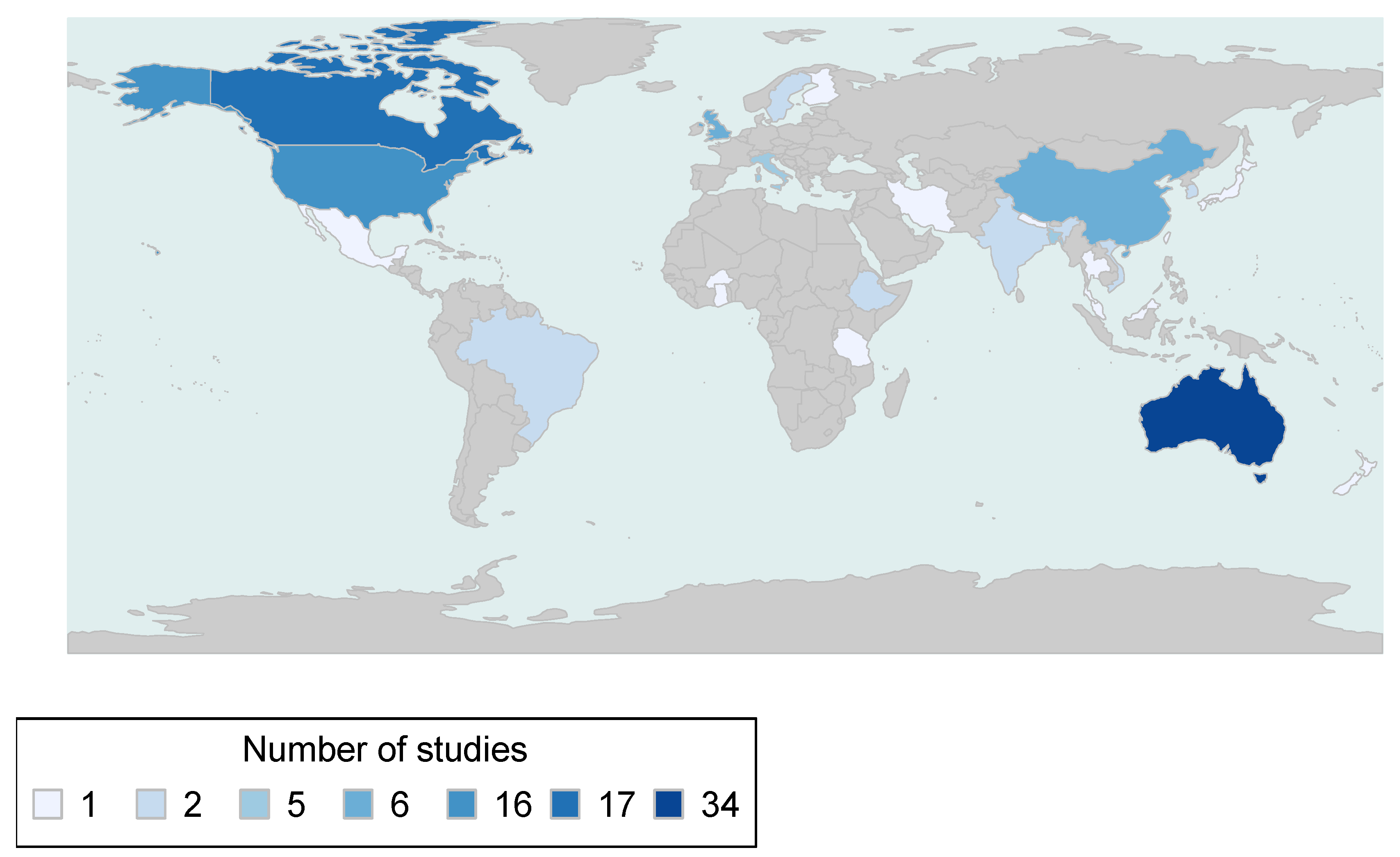
2.4. Figure Preparation
3. Results
3.1. Assessing the Risks
3.2. Environmental Exposures
3.2.1. Temperature and Humidity
3.2.2. Drought and Rainfall
3.2.3. Wildfire
3.2.4. Flood
3.3. Mental Health Outcomes
3.3.1. Symptom Scales and Screening Tools
3.3.2. Hospital Admissions
3.3.3. Mortality
3.3.4. Self-Harm
3.3.5. Burden of Disease
3.4. Vulnerable Populations and Life Stages
3.4.1. Pre-existing Mental Illness
3.4.2. Youth
3.4.3. Indigenous People
3.4.4. Low- and Middle-Income Countries
3.5. Identifying the Most Effective Interventions
3.6. Guiding Health-Promoting Mitigation and Adaptation Decisions in Other Sectors
3.7. Improving Decision-Support
3.8. Estimating the Costs of Protecting Health from Climate Change
3.9. Quality of Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
Appendix A.1. Protecting Health from Climate Change—Global Research Priorities from the World Health Organization (WHO 2009)
- (I)
- Assessing the risks
- Improved evaluation of current climate-related health risks, rather than a primary focus on risks over very long timeframes
- Identification of vulnerable populations and life stages
- Quantification of the fraction of morbidity and mortality attributable to climate hazards, and to climate change
- Better assessment of neglected climate-mental health linkages
- (II)
- Identifying the most effective interventions
- Systematic reviews of the evidence base for interventions
- Methodological research to improve analytical tools for cost-effectiveness analysis
- (III)
- Guiding health-promoting mitigation and adaption decisions in other sectors
- Improved methods for assessment of the health implications of decisions in other sectors
- Health implications of climate change mitigation: energy and transport sectors
- Health implications of climate change adaptation: water, food and agriculture sectors
- Improved integration of climate change mitigation, adaptation, and health through “settings-based” research
- (IV)
- Improving decision-support
- Research to improve vulnerability and adaptation assessments
- Improvement of operational predictions
- Improved understanding of decision-making processes
- (V)
- Estimating the costs of protecting health from climate change
- Definition of harmonized methods to estimate costs and benefits
- Assessment of the health costs of inaction and the costs of adaptation
- Improved economic assessment of the health co-benefits of climate change mitigation
Appendix A.2. Search Strings by Online Database
| Assessing the Risks (n = 101) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Exposure | Quality Rating | |
| Acharibasam and Anuga 2018 | Ghana | NR | Cross-sectional | Farmers from three districts in Northern Ghana | 180 | Emotional regulation practices (given psychological distance i.e., geographical, social) | Self-reported exposure to excessive heat, declined rainfall, prolonged drought, excessive floods, and strong wind using questionnaires | Fair | |
| Aguglia, Serafini et al., 2020 | Italy | 2013–2015 | Cross-sectional | Psychiatric patients in Turin | 730 | Involuntary admissions | Interpolated exposure using daily meteorological data on wind, temperature, humidity, barometric pressure, solar radiation, rain, and hours of sunshine from Italian Meteorology’s Climate Data Service of Physics Department of the University of Turin | Good | |
| Albrecht, Sartore et al., 2007 | Australia | 2003–2006 | Cross-sectional | Residents of the Upper Hunter region of NSW and rural NSW | 60 | Solastalgia and environmental distress | Self-reported exposure to drought and mining using interviews, focus groups, and surveys | Fair | |
| Allen 2020 | USA | NR | Cross-sectional | Social workers in Alaska | 159 | Social workers’ attitudes about climate change and perceptions of the effects of climate change on their clients | Self-reported exposure to climate change using surveys | Poor | |
| Anderson 2009 | Australia | 2004–2007 | Phenomenological | Women health workers from Mallee, Victoria | 2 | How drought and climate change impact rural mental health, and how discourse of endurance and uncertainty can exacerbate problems in rural social work. | Self-reported exposure to drought using oral histories | Good | |
| Asugeni, MacLaren et al., 2015 | Solomon Islands | NR | Cross-sectional | Residents of six remote villages in East Malaita | 57 | Mental health | Self-reported exposure to sea-level rise using questionnaires | Good | |
| Austin, Handley et al., 2018 | Australia | 2007–2013 | Cohort | Farmers in NSW | 664 | Concerns about climate change | Self-reported exposure to climate change using surveys | Good | |
| Austin, Rich et al., 2020 | Australia | 2007–2013 | Cohort | Rural residents in NSW | 823 | Personal drought-related stress (PDS), community drought-related stress (CDS), and general psychological distress (K10) | Interpolated exposure using monthly meteorological data on rainfall to assess drought conditions | Good | |
| Ayeb-Karlsson, Kniveton et al., 2020 | Bangladesh | 2014–2015 | Mixed-method: Q-methodology and discourse analysis | Residents of Bhola Slum, Dhaka | 62 | Wellbeing and immobility | Self-reported exposure to climate-induced noneconomic losses using storytelling methodology | N/A | |
| Ayeb-Karlsson 2020 | Bangladesh | 2014–2016 | Case study | Residents of Bhola Slum, Dhaka | 140 | Immobility decision-making and wellbeing | Self-reported exposure to climate-induced immobility using Q-based discourse analysis | Fair | |
| Ayeb-Karlsson 2020 | Bangladesh | 2014–2016 | Case study | Residents of three coastal cyclone affected study sites of Bangladesh (Dalbanga South, Mazer Char and Gabtola). | 280 | Emotional fear and mental trauma | Self-reported exposure to climate-induced immobility using Q-based discourse analysis | Fair | |
| Berry and Peel 2015 | Australia | 2013 | Cross-sectional | Residents of regional and rural Australia (all states except Tasmania) | 6674 | Psychological distress (K10), emotional well-being (life satisfaction, happiness, and optimism), CC attitudes (belief, worry, distrust) | Self-reported exposure to climate change using surveys | Good | |
| Billiot 2018 | USA | NR | Cross-sectional | Indigenous community in South Louisiana | 160 | Health (physical, emotional, mental) | Self-reported exposure to environmental changes (including foul smelling air, noise, heavy vehicle movement, pollution, heritage destruction, soil erosion, loss of native fisheries) using surveys | Good | |
| Bryan, Ward et al., 2020 | United Kingdom | NR | Case study | Community members of seven different river catchments | 41 | Health and well-being | Self-reported exposure to drought using semi-structured and narrative interviews | Good | |
| Bunce 2016 | Canada | 2015 | Case study | Inuit women in Iqaluit, Nunavut | 42 | Vulnerability and adaptive capacity | Self-reported exposure to climate change using interviews and focus groups | Good | |
| Burke, González et al., 2018 | USA and Mexico | USA 1968–2004 Mexico1990–2010 | Modelling | Populations of USA and Mexico | USA = 851,088; Mexico = 611,366 | Suicide rates and depressive language | Interpolated exposure using gridded (4 × 4 km) daily meteorological data, from <10,000 weather stations, on temperature and precipitation from PRISM for the US; gridded daily (Berkeley Earth Surface Temperature Dataset) and monthly (Temperature and Precipitation: 1900–2010 Gridded Monthly Time Series Version 3.02, University of Delaware) temperature and precipitation data for Mexico | N/A | |
| Carleton 2017 | India | 1967–2013 | Modelling | Population of India | 1472 deaths per 100,000 | Suicide rates | Interpolated exposure using gridded (1 × 1 degree) daily meteorological data on temperature from the National Center for Environmental Prediction and gridded (0.5 × 0.5 degree) monthly cumulative precipitation data from the University of Delaware | N/A | |
| Carlsen, Oudin et al., 2019 | Sweden | 2012–2017 | Case-crossover | Residents of Gothenburg | 84,230 | Daily psychiatric emergency visits | Interpolated exposure using daily meteorological data, from an urban background measuring station, on temperature from the Swedish Meteorological and Hydrological Institute data repository | N/A | |
| Carnie, Berry et al., 2011 | Australia | 2008–2009 | Case study | Young people, teachers, and service providers in rural drought-affected NSW | 96 | Mental health | Self-reported exposure to drought using consultative forums | Good | |
| Chan, Lam et al., 2018 | Hong Kong | 2002–2011 | Ecological | Public hospital admissions | N/A | Mental-disorder hospitalisation | Interpolated exposure using daily meteorological data, from a monitoring station near the centre of Hong Kong, on temperature and humidity from the Hong Kong Observatory and daily average level of air pollutants, from all general air quality monitoring stations except one rural location, from the Environmental Protection Department of Hong Kong | Good | |
| Chen, Lin et al., 2019 | Taiwan | 2003–2013 | Cohort | Taiwan health insurance beneficiaries | 945,171 | MDD diagnosis | Interpolated exposure using daily meteorological data, from the weather monitoring station nearest the residential township of subjects, on temperature, sunshine duration, and precipitation from the Taiwan Central Weather Bureau | Good | |
| Cooper, Hutchings et al., 2019 | Ethiopia | 2017–2018 | Cross-sectional | Members of three villages in Afar region: Eger, Tirtira, Adkonta | 36 | Emotional wellbeing | Self-reported exposure to water insecurity using focus groups and interviews | Good | |
| Cunsolo Willox, Harper et al., 2012 | Canada | 2009–2010 | Case study | Residents of the Inuit community of Rigolet, Nunatsiavut | 112 | Lived experiences of ecological grief and loss | Self-reported exposure to caribou decline using interviews | Good | |
| Cunsolo Willox, Harper et al., 2013 | Canada | 2010 | Case study | Residents of the Inuit community of Rigolet, Nunatsiavut, community-based health workers and Nunatsiavut Government health professionals | 67 | Sense of place, health, and well-being | Self-reported exposure to climate change using interviews | Good | |
| Cunsolo, Borish et al., 2020 | Canada | NR | Case study | Inuit from the Nunatsiavut and NunatuKavut regions | 105 | Mental health and well-being | Self-reported exposure to climate change using interviews | Good | |
| Dean and Stain 2010 | Australia | 2007 | Cross-sectional | Adolescents (aged 11–17) from five schools in rural NSW | 111 | Emotional well-being (Strengths and Difficulties Questionnaire) and perceived impacts of drought (Drought and Community Survey for Children) | Self-reported exposure to drought using focus groups and surveys | Fair | |
| Di Giorgi, Michielin et al., 2020 | Italy | NR | Cross-sectional | Migrants from African countries with extreme and high vulnerability to climate change in Northern Italy | 100 | Perception of climate change, loss of social capital, and mental health (depressive and anxiety symptoms) | Self-reported exposure to climate change using interviews | Fair | |
| Di Nicola, Mazza et al., 2020 | Italy | 2016–2019 | Cross-sectional | Euthymic bipolar patients in Rome | 704 (352 bipolar subjects, 352 healthy controls) | Weather sensitivity (assessed using METEO-Questionnaire) and its relationship to suicide attempts | Self-reported exposure to weather and climate variation using questionnaires | Good | |
| Ding, Berry et al., 2016 | Australia | 2006–2008 | Cross-sectional | Residents of NSW aged 45+ | 53,144 | Psychological distress (K10) and having been treated for depression or anxiety | Interpolated exposure using gridded (5 × 5 km) daily meteorological data, based on in situ observations and topography-resolving analysis, on temperature and vapour pressure (to approximate humidity) from the Australian Bureau of Meteorology | Good | |
| Dodd, Scott et al., 2018 | Canada | 2015 | Phenomenological | Residents of four Northwest Territories communities | 30 | Mental and emotional well-being, physical health, and livelihoods | Self-reported exposure to wildfires using interviews | Good | |
| du Bray 2018 | USA, Fiji, Cyprus, New Zealand, England | 2014 | Ethnography | Biophysically vulnerable communities in the US (Mobile, Alabama; Kodiak, Alaska; Phoenix, Arizona), Fiji (Viti Levu), Cyprus (Nicosia), New Zealand (Wellington), England (London | Total: 375 (USA: 103 Fiji: 68 Cyprus: 40 New Zealand: 86 London: 78) | Emotional impacts | Self-reported exposure to climate change using interviews and surveys | Good | |
| Durkalec, Furgal et al., 2015 | Canada | 2010–2011 | Case study | Residents of the Inuit community of Nain, Nunatsiavut | 22 | Health | Self-reported exposure to sea ice using focus groups and interviews | Good | |
| Eisenman, McCaffrey et al., 2015 | USA | 2012 | Cross-sectional | Residents of five communities affected by the Wallow Fire in Arizona | 416 | Psychological distress (K10) and solastalgia | Self-reported exposure to wildfires using surveys | Good | |
| Ellis and Albrecht 2017 | Australia | 2013–2014 | Case study | Family farmers in Newdegate, WA | 22 | Place-related mental health and wellbeing | Self-reported exposure to climate change using interviews | Good | |
| Farrokhi, Khankeh et al., 2020 | Iran | 2018–2019 | Case study | Not specified | 33 | Self-reported emotional and mood effects | Self-reported climate change risk perception using interviews | Fair | |
| Fearnley, Magalhaes et al., 2014 | Australia | 2006–2008 | Cross-sectional | Women in south-west WA | 879 | Mental health component scores | Interpolated exposure using environmental data, based on proportional mapping, on dryland salinity from the Western Australian Department of Agriculture’s soil and landscape mapping database, and gridded (5 × 5 km) land surface temperature and normalised difference vegetation index (proxy for rainfall) from the National Oceanographic and Atmospheric Administration’s (NOAA) Advanced Very High Radiometer | Good | |
| Fischer and Van de Vliert 2011 | Global | N/A | Modelling | Nonclinical adult populations | N/A | Indicators of general health complaints, burnout, state and trait anxiety, and depression | Interpolated exposure; monthly temperature deviations calculated at the country level but data source not provided. | N/A | |
| Flint, Robinson et al., 2011 | USA | 2008–2010 | Participatory research | Residents of three remote Alaska Native communities | Interviews: 65 Surveys: 116 | Perceived health status and impacts of berries, measured health benefits of berries, perceived environmental and community wellness | Self-reported exposure to environmental changes using interviews, focus groups, and surveys | Good | |
| Friel, Berry et al., 2014 | Australia | 2007–2008 | Cross-sectional | Nationally representative sample of Australian residents aged 15 years and over | 5012 | Psychological distress (K10) and three indicative measures of food insecurity | Interpolated exposure using gridded (0.25 degree) monthly meteorological data on rainfall (used to calculate Hutchinson Drought Indices) from the Australian Bureau of Meteorology | Good | |
| Fuentes, Asselin et al., 2020 | Canada | 2016 | Cross-sectional | Members of four Indigenous communities in the eastern Canadian boreal forest | 251 | Environmental distress (using questionnaire based on the Environmental Distress Scale (EDS) and the Connor–Davidson Resilience Scale (CD-RISC-10)) | Self-reported exposure to environmental changes using questionnaires | Good | |
| Gibson, Haslam et al., 2019 | Tuvalu | 2015 | Case study | Residents of Tuvalu and key informants | 39 | Psychological distress and associated impairment | Self-reported exposure to climate change using interviews | Good | |
| Gibson, Barnett et al., 2020 | Tuvalu | 2016 | Cross-sectional | Tuvaluan residents in Funafuti | 100 | Determinants and idioms of distress and culturally prescribed responses to coping with distress | Self-reported exposure to climate change using interviews | Fair | |
| Gu, Zhang et al., 2020 | China | 2009–2018 | Modelling | Residents in Ningo, China | 372,027 | Mortality | Interpolated exposure using daily meteorological data, from Yinzhou station (Lat. 29.79 N, Long. 121.55 E; the only national basic weather monitoring station in the central urban area of Ningbo) on temperature and humidity from the Ningbo Meteorological Bureau | N/A | |
| Hanigan, Schirmer et al., 2018 | Australia | 2015 | Cross-sectional | Adults living in rural areas in Victoria | 5312 | Psychological distress (K10) | Interpolated exposure using monthly meteorological data on rainfall (used to calculate Hutchinson Drought Indices) from the Australian Bureau of Meteorology | Good | |
| Hansen, Bi et al., 2008 | Australia | 1993–2006 | Ecological | Residents of Adelaide metropolitan area | 171,614 | Hospital admissions and mortality attributed to mental, behavioural, and cognitive disorders | Interpolated exposure using daily meteorological data, from a central city weather station, on temperature from the Australian Bureau of Meteorology | Good | |
| Helama, Holopainen et al., 2013 | Finland | 1751–2008 | Modelling | Finnish population | 94,356 | Suicide | Interpolated exposure using meteorological data on temperature from the Uppsala temperature record [Department of Meteorology, Uppsala University] | N/A | |
| Helm, Pollitt et al., 2018 | USA | NR | Cross-sectional | Adults who have at least one child | 342 | Depressive symptoms and pro-environmental behaviours | Self-reported exposure to environmental concern using surveys | Fair | |
| Hoffmann, Oliveira et al., 2016 | Brazil | 2014 | Case report | Individual patient with schizophrenia on clozapine treatment | 1 | Heat stroke | Not applicable | N/A | |
| Howard, Ahmed et al., 2020 | USA | 2017 | Cross-sectional | Farmers and ranchers in Montana | 125 | Climate risk perception and mental well-being, including climate-related anxiety | Self-reported exposure to climate change using surveys | Fair | |
| Jones, Wootton et al., 2012 | Australia | 2008–2009 | Cross-sectional | Patients with OCD checking subtype in Sydney | 50 | OCD symptoms | Self-reported exposure to climate change using clinical interviews | Fair | |
| Kabir 2018 | Bangladesh | 2015–2016 | Case study | Residents and health professionals in the Hill-Tracts region | 125 | Psychological health and well-being | Self-reported exposure to climate change using interviews | Fair | |
| Khalaj, Lloyd et al., 2010 | Australia | 1998–2006 | Case-only | Residents of Sydney East and West, Illawarra, Gosford-Wyong, and Newcastle | 1,497,655 | Emergency hospital admissions and underlying conditions | Interpolated exposure using daily meteorological data, from a monitoring station in each of the five regions of interest, on temperature (used to examine extreme heat) from the NSW Bureau of Meteorology | N/A | |
| Kim, Lim et al., 2015 | South Korea | 1992–2009 | Modelling | Residents of Seoul | 271,633 | Mortality (relative risks and attributable deaths) | Interpolated exposure using daily meteorological data, from the representative synoptic surface observation station in Seoul, on humidity, air pressure, and temperature from the Korea Meteorological Administration | N/A | |
| Li, Ferreira et al., 2020 | USA | 1993–2010 | Cross-sectional | USA adult population | 3,060,158 | Self-reported mental health | Interpolated exposure using gridded (4 × 4 km) daily meteorological data on temperature and precipitation from PRISM | Good | |
| Lindvall, Kinsman et al., 2020 | Somalia, Kenya and Ethiopia | 2018 | Case study | Stakeholders from different disciplines (climate, weather, environment, migration, and public health) and agencies (national, regional, and local; governmental, non-governmental, and UN) | 39 | Health and health care access | Self-reported exposure to drought-related migration using interviews | Good | |
| Liu, Liu et al., 2018 | China | 2010 | Case-crossover | Residents of Jinan | 19,569 | Daily hospital visits for mental illness | Interpolated exposure using daily meteorological data on temperature (used to define heatwave events), humidity, wind, and air pressure from the China Meteorological Data Sharing Service System | N/A | |
| Mason, Erwin et al., 2018 | USA | 2016 | Cross-sectional | Primarily low- and moderate-income residents of Knoxville, Tennessee | 424 | Self-reported mental health and potential mediating factors including feeling prepared for extreme weather, general health, income, social cohesion, and concern about climate change | Self-reported exposure to summer heat waves and extreme winter weather using surveys | Fair | |
| Mason, Sharma et al., 2020 | USA | 2016 | Cross-sectional | Low- to middle-income adults of different racial groups in Knoxville, Tennessee | 426 | Physical and mental health, associations with human, financial, physical, and social capital | Self-reported exposure to summer heat waves and extreme winter weather using surveys | Fair | |
| Mayner, Arbon et al., 2010 | Australia | 2009 | Cross-sectional | Emergency department patients in Adelaide | 9244 | ED patient presentations | Interpolated exposure using meteorological data in Adelaide was used to define two types of heat waves events (Australian Bureau of Meteorology criterion) | Good | |
| McNamara and Westoby 2011 | Australia | 2009–2010 | Case study | Aunties (respected older women) living on Erub Island, Torres Strait | 4 | Emotional, cultural, psycho-social impacts | Self-reported exposure to climate change using interviews | Good | |
| Middleton, Cunsolo et al., 2020 | Canada | 2012–2013 | Case study | Inuit community members and health professionals in Nunatsiavut | 116 | Mental health and wellness | Self-reported exposure to changing weather and seasonal patterns using interviews | Good | |
| Mulchandani, Armstrong et al., 2020 | England | 2015–2017 | Cohort | People living in neighbourhoods affected by flooding in the south of England between 1 December 2013, and 31 March 2014 | 819 | Depression, anxiety, and PTSD | Self-reported exposure to flooding using questionnaires | Good | |
| Ng, Wilson et al., 2015 | Australia | NR | Case study | Adults living in four rural communities in NSW | 46 | Wellbeing | Self-reported exposure to flood and drought using interviews and focus groups | Good | |
| Nitschke, Tucker et al., 2007 | Australia | 1993–2006 | Case-series | Residents of Adelaide metropolitan area | N/A | Ambulance transports, hospital admissions, and mortality | Interpolated exposure using daily meteorological data, from Kent Town station, on temperature (used to define heatwave events) from the Australian Bureau of Meteorology | Good | |
| Niu, Gao et al., 2020 | China | 2016–2018 | Time-series | Patients with mental disorders residing in Beijing | 16,606 | Daily emergency visits related to mental disorders | Interpolated exposure using daily meteorological data, from three fixed-site stations in Beijing, on temperature, humidity, duration of sunshine, barometric pressure, precipitation, and wind from the China Meteorological Data Service Center | N/A | |
| Noelke, McGovern et al., 2016 | USA | 2008–2013 | Cross-sectional | Population aged 18+ | 1,900,000 | Emotional well-being | Interpolated exposure using gridded (0.125 × 0.125 degree) daily meteorological data on temperature from the North American Land Data Assimilation System | Good | |
| Obradovich, Migliorini et al., 2018 | USA | 2002–2012 | Cross-sectional | USA residents | 1,961,743 | Mental health difficulties | Interpolated exposure using gridded (4 × 4 km) daily meteorological data on temperature and precipitation from PRISM, and average daily data on cloud cover, humidity, and wind from the National Centers for Environmental Prediction Reanalysis II project | Good | |
| OBrien, Berry et al., 2014 | Australia | 2007–2008 | Cross-sectional | Nationally representative sample of Australian residents aged 15 years and over | 5012 | Psychological distress (K10) | Interpolated exposure using daily meteorological data on rainfall (used to calculate Hutchinson Drought Indices) from the Australian Bureau of Meteorology | Good | |
| Ogunbode, Böhm et al., 2019 | United Kingdom | 2013–2014 | Cross-sectional | British sample (this study only used a sub-sample of a larger questionnaire. They only used individuals who indicated that they had been personally affected a little, a fair amount, or a great deal by the 2013/2014 UK winter flooding | 821 | Negative emotions and mitigation intention | Self-reported exposure to flooding using surveys | Good | |
| Oudin Astrom, Schifano et al., 2015 | Italy and Sweden | 2000–2008 | Cohort | Residents of Rome and Stockholm aged 50 years or older | 110,531 | Mortality | Interpolated exposure using daily meteorological data, from the airport station closest to the city in Rome and the station at Bromma City aiport in Stockholm, on temperature (used to define heatwave events) | Good | |
| Page, Hajat et al., 2012 | England | 1998–2007 | Cohort | Patients with primary diagnoses of psychosis, dementia, alcohol misuse, and other substance misuse | 22,562 | Mortality | Interpolated exposure using daily meteorological data, from all monitoring stations in England, on temperature from the British Atmospheric Data Centre | Good | |
| Pailler and Tsaneva 2018 | India | 2003 & 2007 | Cross-sectional | Sample of 8468 from World Health Survey (WHS) in 2003 and 7759 from 2007 Study on global AGEing and adult health (SAGE) | 16,227 | Depression; stress (cognitive and sleep difficulties, ability to cope); agency (control) | Interpolated exposure using gridded (0.5 × 0.5 degree) monthly meteorological data on temperature and precipitation (used to define weather extremes) from the Matsurra & Willmott ‘Terrestrial air temperature and precipitation: Monthly and annual time series (1950–1999)’ | Good | |
| Polain, Berry et al., 2011 | Australia | 2008 | Case study | Older farmers in NSW | 152 | Mental health | Self-reported exposure to drought using consultative forums | Good | |
| Powers, Dobson et al., 2015 | Australia | 1996–2008 | Cohort | Women living in rural Australia | 6664 | Mental Health Index scores (from the Medical Outcomes Study Short Form 36-SF36) | Interpolated exposure; the Hutchinson Drought Index was used but data source not provided. | Good | |
| Powers, Loxton et al., 2012 | Australia | 2004 | Cross-sectional | Women living outside major cities | 6584 | SF-36 General Health (GH) and Mental Health (MH) scores, and perceived stress | Interpolated exposure to Exceptional Circumstances declared area using the 2004 survey with latitude and longitude declared areas in the same year for each participant. | Good | |
| Preti, Lentini et al., 2007 | Italy | 1974–2003 | Modelling | Italians | 97,693 | Suicide | Interpolated exposure using monthly meteorological data on temperature anomalies from the Istituto di Scienze dell’Atmosfera e del Clima (Institute of Atmospheric Sciences and Climate) | N/A | |
| Proverbs, Lantz et al., 2020 | Canada | 2017 | Case study | Members of four Gwich’in First Nation communities in the Northwest Territories | 29 | Well-being | Self-reported exposure to access to fish using interviews | Good | |
| Qi, Hu et al., 2014 | Australia | 1986–2005 | Modelling | Population of Australia | 45,293 | Suicide rates | Interpolated exposure using monthly meteorological data, from monitoring stations in each Local Government Area, on rainfall, humidity, and temperature from the Australian Bureau of Meteorology | N/A | |
| Rahman, Mohamad et al., 2014 | Malaysia | 2012 | Cross-sectional | University students in Malaysia | 200 | Perceived awareness and perceived physical and psychological impact | Self-reported exposure to climate change using surveys | Good | |
| Rigby, Rosen et al., 2011 | Australia | 2008 | Case study | Aboriginal communities in NSW | 166 | Social and emotional well-being, and possible adaptive strategies | Self-reported exposure to drought using consultative forums | Good | |
| Rotge, Fossati et al., 2014 | Global | 2001–2005 | Ecological | Populations of 17 countries: Belgium, Colombia, France, Germany, Israel, Italy, Japan, Lebanon, Mexico, Netherlands, New Zealand, Nigeria, PR China, South Africa, Spain, Ukraine, United States | 85,052 | Lifetime prevalence of mood disorders | Interpolated exposure using monthly meteorological data on temperature and rainfall from the World Bank Group | Fair | |
| Sartore, Kelly et al., 2008 | Australia | NR | Case study | Two rural communities in NSW | 39 | Emotional and social wellbeing | Self-reported exposure to drought using focus groups | Good | |
| Searle and Gow 2010 | Australia | 2008 | Cross-sectional | University students and members of the general public in Queensland | 275 | Climate change distress; environmental beliefs (NEP); depression, anxiety, and stress (DASS-21); future anxiety (FAS3); intolerance of uncertainty (IUS-12); religiosity (SCSRFQ-SF) | Self-reported exposure to climate change using questionnaires | Good | |
| Sim, Kim et al., 2020 | Japan | 1972–2015 | Time-series | Population of Japan | 1,067,333 | Suicide | Interpolated exposure using daily meteorological data, from a weather station in the capital city of each prefecture, on temperature and humidity from the Japan Meteorology Agency | N/A | |
| Stain, Kelly et al., 2011 | Australia | 2006–2009 | Cross-sectional | Adults living in rural NSW | 302 | Psychological distress (K10) and an index of concern or worry about drought | Interpolated exposure using gridded (0.25 degree) monthly meteorological data on rainfall (used to calculate drought exposure) from the Australian Bureau of Meteorology | Good | |
| Sugg, Dixon et al., 2019 | USA | 2013–2017 | Time-series | Adolescents and young adults in Atlanta, Georgia; Chicago, Illinois; Los Angeles, California, and New York City; New York. | 59,000 | Crisis support-seeking behaviour | Interpolated exposure using daily meteorological data, from the following international airport weather stations: Atlanta Hartsfield, Chicago O’Hare, LaGuardia, and Los Angeles, on temperature from the Applied Climate Information System available from and maintained by the National Oceanic and Atmospheric Administration’s Regional Climate Centers | N/A | |
| Tasdik Hasan, Adhikary et al., 2020 | Bangladesh | 2015 | Case study | Key informants and cyclone-affected people in Koyra Sadar Upazila, Khulna district | 20 | Perceived need for mental health support and availability of such services | Self-reported exposure to cyclones using interviews | Good | |
| Tawatsupa, Lim et al., 2010 | Thailand | 2005 | Cross-sectional | Workers | 40,913 | Psychological distress (K10) and overall health (first question of SF8) | Self-reported exposure to heat stress using questionnaires | Fair | |
| Trang, Rocklov et al., 2016 | Vietnam | 2008–2012 | Time-series | Patients with mental disorders in the north of Vietnam | 21,443 | Hospital admissions for mental disorders | Interpolated exposure using daily meteorological data, from several monitoring stations in Hanoi, on temperature (used to define heatwave events) | N/A | |
| Trinh, Feeny et al., 2020 | Vietnam | 2002–2013 | Modelling | Children | 2000 | Stunting and underweight in children, and parental mental health as a mediating factor | Interpolated exposure using gridded (0.5 × 0.5 degree) monthly meteorological data on rainfall from the National Oceanic and Atmospheric Administration | N/A | |
| Verplanken and Roy 2013 | Europe and USA | 2012 | Participatory research | Participants who took survey in USA and Europe | 132 | Habitual ecological worrying | Self-reported exposure to climate change using surveys | Fair | |
| Vida, Durocher et al., 2012 | Canada | 1995–2007 | Modelling | Patients aged 15 years and older in Quebec | 347,552 | Emergency department visits for mental and psychosocial problems | Interpolated exposure using daily meteorological data, from available weather stations, on temperature and humidity from Environment Canada and the Ministry of Sustainable Development, Environment, and Parks | N/A | |
| Wang, Lavigne et al., 2014 | Canada | 2002–2010 | Ecological | Residents of Toronto | 271,746 | Emergency room (ER) visits related to mental and behavioural diseases (MBD) | Interpolated exposure using hourly meteorological data, from the monitoring station at Toronto Pearson International Airport, on temperature and humidity from Environment Canada | Good | |
| Wei, Zhang et al., 2020 | China | 2005–2014 | Ecological | Patients of Anhui Mental Health Center in Hefei | 36,607 | Admissions for schizophrenia | Interpolated exposure to precipitation data for the region Hefei and flood events were defined based on established criteria. | Poor | |
| Williams, Hill et al., 2016 | New Zealand | 1993–2009 | Modelling | Population of New Zealand | 47,265 | Self-harm hospitalisations | Interpolated exposure using gridded (5 km) daily meteorological data, from a virtual climate network, on temperature from the National Institute of Water and Atmospheric Research | N/A | |
| Williams, Nitschke et al., 2012 | Australia | 1993–2009 | Ecological | Population of Adelaide | N/A | Mortality, ambulance call-outs, emergency department (ED) presentations and hospital admissions | Interpolated exposure using daily meteorological data, from Kent Town station, on temperature from the Australian Bureau of Meteorology | Good | |
| Xu, Wheeler et al., 2018 | Australia | 2008–2014 | Cross-sectional | Australian children | 6857 | Mental health | Interpolated exposure using gridded daily meteorological data on temperature from the Australian Bureau of Meteorology | Good | |
| Xu, Zhao et al., 2020 | Brazil | 2000–2015 | Case-crossover | Brazilian population | 49,145,997 | All-cause and cause-specific hospitalisations | Interpolated exposure using gridded (0.25 degree) daily meteorological data on temperature, from a Brazilian meteorological dataset, with the analyses restricted to the hottest four consecutive months (hot season) for each city each year during the study period | N/A | |
| Yazd, Wheeler et al., 2020 | Australia | 2001–2015 | Panel | Farmers in the Murray-Darling Basin | 235 | Mental health, assessed using the mental health inventory (MHI-5), a sub-scale of the SF-36 | Interpolated exposure using gridded monthly meteorological data on rainfall (used to define drought) from the Australian Bureau of Meteorology | N/A | |
| Yoon, Oh et al., 2014 | South Korea | 2008, 2100 | Modelling (burden of disease) | Population of South Korea | N/A | Burden of disease (DALYs) attributable to climate factors | Interpolated exposure using daily meteorological data, from 77 regional meteorological offices and observatories, on temperature from the Korea Meteorological Administration; ozone concentration data from the 2008 Annual Report of Ambient Air Quality in Korea; and the number of natural disasters was based on the Annual Report of Disasters in Korea | N/A | |
| Zhao, Zhang et al., 2016 | China | 2005–2014 | Ecological | Population of Hubei | 36,607 | Emergency hospital admissions for schizophrenia | Interpolated exposure using daily meteorological data on temperature and humidity from the Hefei Bureau of Meteorology | Good | |
| Identifying the Most Effective Interventions (n = 8) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| Hart, Berry et al., 2011 | Australia | 2007–2010 | Program development | All rural communities facing prolonged drought in NSW | 3000 | A community development model effective in helping communities build capacity and resilience in the face of chronic drought-related hardship. | N/A | ||
| Hayes, Poland et al., 2020 | Canada | 2018 | Case study | Key informant health and social services leaders, front-line health and social services workers and community members who experienced the 2013 Southern Alberta flood | 46 | Health and social service responses to the long-term mental health impacts of the flood | Good | ||
| Heaney and Winter 2016 | Tanzania | 2013 | Case study | Two demographically matched adult Maasai populations in Arusha: rural-to-urban migrants and permanent rural residents (i.e., non-migrants) | 14 | Health perceptions and help-seeking behaviours | Good | ||
| Netuveli and Watts 2020 | United Kingdom | 2009–2010 | Panel | UK households | 22,427 people in 9344 households | Life satisfaction, self-rated health, mental health (assessed using 12-item version of the General Health Questionnaire (GHQ-12)), physical quality of life and mental quality of life | N/A | ||
| Patrick and Capetola 2011 | Australia | 2010–2011 | Case study | Victorian health care agencies that explicitly identified climate change as a priority | 10 | Health promotion practice | Good | ||
| Purcell and McGirr 2018 | Australia | NR | Cross-sectional | Health service managers working in rural remote metropolitan areas in NSW | 43 | Perceptions and recommendations of rural HSMs on climate change and its impact on health in their local communities | Fair | ||
| Valois, Blouin et al., 2016 | Canada | NR | Cross-sectional | Family physicians in Quebec | 24 | Family physicians’ educational needs regarding the health impacts of climate change | Good | ||
| Wang, Jiang et al., 2019 | China | 2018 | Cross-sectional | Chinese residents | 1273 | Environmental complaint behaviour | Fair | ||
| Guiding Health-Promoting Mitigation and Adaption Decisions in Other Sectors (n = 7) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| Harper, Edge et al., 2015 | Canada | 2010 | Participatory research | Inuit community members and government employees in the Nunatsiavut region | 209 | Climate-sensitive health issues | Good | ||
| MacFarlane, Shakya et al., 2015 | Nepal | 2014 | Participatory research | Female subsistence farmers aged 27–49 years in the Jumla district | 10 | Mental health | Good | ||
| Petrasek MacDonald, Cunsolo Willox et al., 2015 | Canada | 2012–2013 | Case study | Inuit youth in Nunatsiavut | 17 | Youth-specific protective factors that enhance mental health and well-being | Good | ||
| Raker, Arcaya et al., 2020 | USA | 2003–2018 | Cross-sectional | Low-income primarily Black parents in New Orleans and Houston | 113 | Lessons learned from the RISK project, including planning priorities to mitigate the health consequences of disasters | Good | ||
| Sawatzky, Cunsolo et al., 2020 | Canada | 2015–2016 | Case study | Inuit community members, government representatives and health professionals in Rigolet | 31 | Conceptual framework for an Inuit-led integrated environment and health monitoring system | Good | ||
| Sorgho, Mank et al., 2020 | Burkina Faso | 2018 | Case study | Subsistence farmers | 32 | Perceptions of climate change and health; agricultural adaptation strategies including barriers and possibilities; dietary adaptation practices; sources of support (social and governmental) | Good | ||
| Wong-Parodi 2020 | USA | 2019 | Cross-sectional | Individuals living in one of 41 California counties in PG&E’s and SCE’s (utility companies) public safety power shutoffs (PSPS) zone | 328 | Physical and mental health; views on the PSPS decisions; response to those decisions; views on wildfire risk | Fair | ||
| Improving Decision-Support (n = 3) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| McIver, Kim et al., 2016 | Cook Islands, Federated States of Micronesia, Fiji, Kiribati, Marshall Islands, Nauru, Niue, Palau, Samoa, Solomon Islands, Tonga, Tuvalu, and Vanuatu | 2010–2012 | Vulnerability assessment | Pacific island countries | 13 Pacific island countries | Health risks and adaptation strategies | N/A | ||
| Seidel and Bell 2014 | Australia, Belgium, Wales, Finland, Denmark, Germany, United Kingdom, Russia, USA, Spain, Scotland, Netherlands | 2012 | ‘Critical computational linguistics’ | High-income countries | Exhaustive sample of national adaptation policy documents from Annex 1 (‘developed’) countries of the UNFCC | Representation of climate-vulnerable groups in adaptation policy | N/A | ||
| Valois, Caron et al., 2019 | Canada | NR | Cross-sectional | Adults living in or near a designated flood-prone area in Quebec | 1951 | Behavioural indices of flood adaptation | Fair | ||
| Estimating the Costs of Protecting Health from Climate Change (n = 1) | |||||||||
| Authors and Date | Country | Study Period | Study Design | Study Population | Sample Size | Outcomes | Quality Rating | ||
| Maughan, Patel et al., 2016 | United Kingdom | 2011–2014 | Retrospective observational study | Patients with a common mental health condition attending the Connect service; control group of patients attending same primary care service not attending Connect | Connect group = 30, control group = 29 | Financial and environmental impacts of GP appointments, psychotropic medications and secondary-care referrals | Good | ||
References
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009, 373, 1693–1733. [Google Scholar] [CrossRef]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Beagley, J.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D. The 2020 report of The Lancet Countdown on health and climate change: Responding to converging crises. Lancet 2020, 397, 129–170. [Google Scholar] [CrossRef]
- Patel, V.; Chisholm, D.; Parikh, R.; Charlson, F.J.; Degenhardt, L.; Dua, T.; Ferrari, A.J.; Hyman, S.; Laxminarayan, R.; Levin, C.; et al. Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition. Lancet 2015, 387, 1672–1685. [Google Scholar] [CrossRef] [Green Version]
- Berry, H.L.; Bowen, K.; Kjellstrom, T. Climate change and mental health: A causal pathways framework. Int. J. Public Health 2010, 55, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Middleton, J.; Cunsolo, A.; Jones-Bitton, A.; Wright, C.J.; Harper, S.L. Indigenous mental health in a changing climate: A systematic scoping review of the global literature. Environ. Res. Lett. 2020, 15, 53001. [Google Scholar] [CrossRef]
- Hayes, K.; Poland, B. Addressing Mental Health in a Changing Climate: Incorporating Mental Health Indicators into Climate Change and Health Vulnerability and Adaptation Assessments. Int. J. Environ. Res. Public Health 2018, 15, 1806. [Google Scholar] [CrossRef] [Green Version]
- Cianconi, P.; Betrò, S.; Janiri, L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Front. Psychiatry 2020, 11, 1–15. [Google Scholar] [CrossRef]
- WHO. Protecting Health from Climate Change: Global Research Priorities; World Health Organisation: Geneva, Switzerland, 2009. [Google Scholar]
- Page, M.J.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.; Shamseer, L. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. MetaArXiv 2020. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Berry, H.; Bouley, T.; Boykoff, M.; Byass, P.; Cai, W.; et al. The 2018 report of the Lancet Countdown on health and climate change: Shaping the health of nations for centuries to come. Lancet 2018, 392, 2479–2514. [Google Scholar] [CrossRef]
- National Institute for Health. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 8 February 2021).
- CASP. CASP Checklists. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 8 February 2021).
- Cortes-Ramirez, J.; Naish, S.; Sly, P.D.; Jagals, P. Mortality and morbidity in populations in the vicinity of coal mining: A systematic review. BMC Public Health 2018, 18, 721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haddaway, N.R.; McGuinness, L.A. PRISMA2020: R package and ShinyApp for producing PRISMA 2020 compliant flow diagrams (Version 0.0.1). Zenodo 2020. [Google Scholar] [CrossRef]
- South, A. rworldmap: A new R package for mapping global data. R J. 2011, 3, 43. [Google Scholar] [CrossRef] [Green Version]
- Team, R. RStudio: Integrated Development for R. RStudio. Available online: http://www.rstudio.com/ (accessed on 23 April 2021).
- Team, R.C. R: A language and environment for statistical computing. Available online: https://www.R-project.org/ (accessed on 23 April 2021).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis. Available online: https://ggplot2.tidyverse.org (accessed on 23 April 2021).
- Ding, N.; Berry, H.L.; Bennett, C.M. The Importance of Humidity in the Relationship between Heat and Population Mental Health: Evidence from Australia. PLoS ONE 2016, 11, e0164190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, S.; Nitschke, M.; Sullivan, T.; Tucker, G.R.; Weinstein, P.; Pisaniello, D.L.; Parton, K.A.; Bi, P. Heat and health in Adelaide, South Australia: Assessment of heat thresholds and temperature relationships. Sci. Total Environ. 2012, 414, 126–133. [Google Scholar] [CrossRef]
- Xu, Y.; Wheeler, S.A.; Zuo, A. Will boys’ mental health fare worse under a hotter climate in Australia? Popul. Environ. 2018, 40, 158–181. [Google Scholar] [CrossRef]
- Kabir, S.M.S. Psychological health challenges of the hill-tracts region for climate change in Bangladesh. Asian J. Psychiatry 2018, 34, 74–77. [Google Scholar] [CrossRef]
- Pailler, S.; Tsaneva, M. The effects of climate variability on psychological well-being in India. World Dev. 2018, 106, 15–26. [Google Scholar] [CrossRef]
- Tawatsupa, B.; Lim, L.L.; Kjellstrom, T.; Seubsman, S.A.; Sleigh, A.; The Thai Cohort Study, T. The association between overall health, psychological distress, and occupational heat stress among a large national cohort of 40,913 Thai workers. Glob. Health Action 2010, 3, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.T.; Lin, P.H.; Guo, Y.L. Long-term exposure to high temperature associated with the incidence of major depressive disorder. Sci. Total Environ. 2019, 659, 1016–1020. [Google Scholar] [CrossRef] [PubMed]
- Noelke, C.; McGovern, M.; Corsi, D.J.; Jimenez, M.P.; Stern, A.; Wing, I.S.; Berkman, L. Increasing ambient temperature reduces emotional well-being. Environ. Res. 2016, 151, 124–129. [Google Scholar] [CrossRef] [Green Version]
- Obradovich, N.; Migliorini, R.; Paulus, M.P.; Rahwan, I. Empirical evidence of mental health risks posed by climate change. Proc. Natl. Acad. Sci. USA 2018, 115, 10953–10958. [Google Scholar] [CrossRef] [Green Version]
- Sugg, M.M.; Dixon, P.G.; Runkle, J.D. Crisis support-seeking behavior and temperature in the United States: Is there an association in young adults and adolescents? Sci. Total Environ. 2019, 669, 400–411. [Google Scholar] [CrossRef] [PubMed]
- Mason, L.R.; Erwin, J.; Brown, A.; Ellis, K.N.; Hathaway, J.M. Health Impacts of Extreme Weather Events: Exploring Protective Factors with a Capitals Framework. J. Evid. Inf. Soc. Work 2018, 15, 579–593. [Google Scholar] [CrossRef]
- OBrien, L.; Berry, H.L.; Coleman, C.; Hanigan, I.C. Drought as a mental health exposure. Environ. Res. 2014, 131, 181–187. [Google Scholar] [CrossRef] [Green Version]
- Austin, E.K.; Handley, T.; Kiem, A.S.; Rich, J.L.; Lewin, T.J.; Askland, H.H.; Askarimarnani, S.S.; Perkins, D.A.; Kelly, B.J. Drought-related stress among farmers: Findings from the Australian Rural Mental Health Study. Med. J. Aust. 2018, 209, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Polain, J.D.; Berry, H.L.; Hoskin, J.O. Rapid change, climate adversity and the next ‘big dry’: Older farmers’ mental health. Aust. J. Rural Health 2011, 19, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Stain, H.J.; Kelly, B.; Carr, V.J.; Lewin, T.J.; Fitzgerald, M.; Fragar, L. The psychological impact of chronic environmental adversity: Responding to prolonged drought. Soc. Sci. Med. 2011, 73, 1593–1599. [Google Scholar] [CrossRef]
- Hanigan, I.C.; Schirmer, J.; Niyonsenga, T. Drought and Distress in Southeastern Australia. EcoHealth 2018, 15, 642–655. [Google Scholar] [CrossRef]
- Powers, J.R.; Dobson, A.J.; Berry, H.L.; Graves, A.M.; Hanigan, I.C.; Loxton, D. Lack of association between drought and mental health in a cohort of 45-61 year old rural Australian women. Aust. N. Z. J. Public Health 2015, 39, 518–523. [Google Scholar] [CrossRef]
- Powers, J.R.; Loxton, D.; Baker, J.; Rich, J.L.; Dobson, A.J. Empirical evidence suggests adverse climate events have not affected Australian women’s health and well-being. Aust. N. Z. J. Public Health 2012, 36, 452–457. [Google Scholar] [CrossRef] [Green Version]
- Rotge, J.Y.; Fossati, P.; Lemogne, C. Climate and prevalence of mood disorders: A cross-national correlation study. J. Clin. Psychiatry 2014, 75, 408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dodd, W.; Scott, P.; Howard, C.; Scott, C.; Rose, C.; Cunsolo, A.; Orbinski, J. Lived experience of a record wildfire season in the Northwest Territories, Canada. Can. J. Public Health Rev. Can. De Sante Publique 2018, 109, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Higginbotham, N.; Connor, L.; Albrecht, G.; Freeman, S.; Agho, K. Validation of an Environmental Distress Scale. EcoHealth 2006, 3, 245–254. [Google Scholar] [CrossRef]
- Eisenman, D.; McCaffrey, S.; Donatello, I.; Marshal, G. An Ecosystems and Vulnerable Populations Perspective on Solastalgia and Psychological Distress After a Wildfire. EcoHealth 2015, 12, 602–610. [Google Scholar] [CrossRef] [Green Version]
- Ng, F.Y.; Wilson, L.A.; Veitch, C. Climate adversity and resilience: The voice of rural Australia. Rural Remote Health 2015, 15, 3071. [Google Scholar] [PubMed]
- Mulchandani, R.; Armstrong, B.; Beck, C.R.; Waite, T.D.; Amlôt, R.; Kovats, S.; Leonardi, G.; Rubin, G.J.; Oliver, I. The English National Cohort Study of Flooding & Health: Psychological morbidity at three years of follow up. BMC Public Health 2020, 20, 321. [Google Scholar] [CrossRef] [Green Version]
- Farrokhi, M.; Khankeh, H.R.; Amanat, N.; Kamali, M.; Fathi, M. Psychological aspects of climate change risk perception: A content analysis in Iranian context. J. Educ. Health Promot. 2020, 9, 346. [Google Scholar] [CrossRef]
- Howard, M.; Ahmed, S.; Lachapelle, P.; Schure, M.B. Farmer and rancher perceptions of climate change and their relationships with mental health. J. Rural Ment. Health 2020, 44, 87–95. [Google Scholar] [CrossRef]
- Albrecht, G.; Sartore, G.M.; Connor, L.; Higginbotham, N.; Freeman, S.; Kelly, B.; Stain, H.; Tonna, A.; Pollard, G. Solastalgia: The distress caused by environmental change. Australas. Psychiatry Bull. R. Aust. N. Z. Coll. Psychiatr. 2007, 15 (Suppl. 1), S95–S98. [Google Scholar] [CrossRef]
- Fuentes, L.; Asselin, H.; Bélisle, A.C.; Labra, O. Impacts of Environmental Changes on Well-Being in Indigenous Communities in Eastern Canada. Int. J. Environ. Res. Public Health 2020, 17, 637. [Google Scholar] [CrossRef] [Green Version]
- Searle, K.; Gow, K. Do concerns about climate change lead to distress? Int. J. Clim. Chang. Strat. Manag. 2010, 2, 362–379. [Google Scholar] [CrossRef]
- Billiot, S.M. How Do Environmental Changes and Shared Cultural Experiences Impact the Health of Indigenous Peoples in South Louisiana? Ph.D. Thesis, Washington University, St Louis, MO, USA, 2018. [Google Scholar]
- Chan, E.Y.Y.; Lam, H.C.Y.; So, S.H.W.; Goggins, W.B.; Ho, J.Y.; Liu, S.; Chung, P.P.W. Association between Ambient Temperatures and Mental Disorder Hospitalizations in a Subtropical City: A Time-Series Study of Hong Kong Special Administrative Region. Int. J. Environ. Res. Public Health 2018, 15, 754. [Google Scholar] [CrossRef] [Green Version]
- Xu, R.; Zhao, Q.; Coelho, M.S.; Saldiva, P.H.; Abramson, M.J.; Li, S.; Guo, Y.J.P.M. Socioeconomic level and associations between heat exposure and all-cause and cause-specific hospitalization in 1,814 Brazilian cities: A nationwide case-crossover study. PLoS Med. 2020, 17, e1003369. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, P.; Nitschke, M.; Ryan, P.; Pisaniello, D.; Tucker, G. The effect of heat waves on mental health in a temperate Australian city. Environ. Health Perspect. 2008, 116, 1369–1375. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Lavigne, E.; Ouellette-kuntz, H.; Chen, B.E. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J. Affect. Disord. 2014, 155, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Trang, P.M.; Rocklov, J.; Giang, K.B.; Kullgren, G.; Nilsson, M. Heatwaves and Hospital Admissions for Mental Disorders in Northern Vietnam. PLoS ONE 2016, 11, e0155609. [Google Scholar] [CrossRef]
- Liu, X.; Liu, H.; Fan, H.; Liu, Y.; Ding, G. Influence of Heat Waves on Daily Hospital Visits for Mental Illness in Jinan, China—A Case-Crossover Study. Int. J. Environ. Res. Public Health 2018, 16, 87. [Google Scholar] [CrossRef] [Green Version]
- Page, L.A.; Hajat, S.; Kovats, R.S.; Howard, L.M. Temperature-related deaths in people with psychosis, dementia and substance misuse. Br. J. Psychiatry J. Ment. Sci. 2012, 200, 485–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oudin Astrom, D.; Schifano, P.; Asta, F.; Lallo, A.; Michelozzi, P.; Rocklov, J.; Forsberg, B. The effect of heat waves on mortality in susceptible groups: A cohort study of a mediterranean and a northern European City. Environ. Health A Glob. Access Sci. Source 2015, 14, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nitschke, M.; Tucker, G.R.; Bi, P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med. J. Aust. 2007, 187, 662–665. [Google Scholar] [CrossRef] [Green Version]
- Gu, S.; Zhang, L.; Sun, S.; Wang, X.; Lu, B.; Han, H.; Yang, J.; Wang, A.J.E.I. Projections of temperature-related cause-specific mortality under climate change scenarios in a coastal city of China. Environ. Int. 2020, 143, 105889. [Google Scholar] [CrossRef]
- Williams, M.N.; Hill, S.R.; Spicer, J. Do hotter temperatures increase the incidence of self-harm hospitalisations? Psychol. Health Med. 2016, 21, 226–235. [Google Scholar] [CrossRef]
- Carleton, T.A. Crop-damaging temperatures increase suicide rates in India. Proc. Natl. Acad. Sci. USA 2017, 114, 8746–8751. [Google Scholar] [CrossRef] [Green Version]
- Helama, S.; Holopainen, J.; Partonen, T. Temperature-associated suicide mortality: Contrasting roles of climatic warming and the suicide prevention program in Finland. Environ. Health Prev. Med. 2013, 18, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Preti, A.; Lentini, G.; Maugeri, M. Global warming possibly linked to an enhanced risk of suicide: Data from Italy, 1974–2003. J. Affect. Disord. 2007, 102, 19–25. [Google Scholar] [CrossRef]
- Burke, M.; González, F.; Baylis, P.; Heft-Neal, S.; Baysan, C.; Basu, S.; Hsiang, S. Higher temperatures increase suicide rates in the United States and Mexico. Nat. Clim. Chang. 2018, 8, 723–729. [Google Scholar] [CrossRef]
- Yoon, S.J.; Oh, I.H.; Seo, H.Y.; Kim, E.J. Measuring the burden of disease due to climate change and developing a forecast model in South Korea. Public Health 2014, 128, 725–733. [Google Scholar] [CrossRef]
- Hoffmann, M.S.; Oliveira, L.M.; Lobato, M.I.; Belmonte-de-Abreu, P. Heat stroke during long-term clozapine treatment: Should we be concerned about hot weather? Trends Psychiatry Psychother. 2016, 38, 56–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, M.K.; Wootton, B.M.; Vaccaro, L.D.; Menzies, R.G. The impact of climate change on obsessive compulsive checking concerns. Aust. N. Z. J. Psychiatry 2012, 46, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Dean, J.G.; Stain, H.J. Mental health impact for adolescents living with prolonged drought. Aust. J. Rural Health 2010, 18, 32–37. [Google Scholar] [CrossRef]
- Cunsolo Willox, A.; Harper, S.L.; Ford, J.D.; Landman, K.; Houle, K.; Edge, V.L. “From this place and of this place:” climate change, sense of place, and health in Nunatsiavut, Canada. Soc. Sci. Med. 2012, 75, 538–547. [Google Scholar] [CrossRef]
- Carnie, T.L.; Berry, H.L.; Blinkhorn, S.A.; Hart, C.R. In their own words: Young people’s mental health in drought-affected rural and remote NSW. AJRH 2011, 19, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Durkalec, A.; Furgal, C.; Skinner, M.W.; Sheldon, T. Climate change influences on environment as a determinant of Indigenous health: Relationships to place, sea ice, and health in an Inuit community. Soc. Sci. Med. 2015, 136–137, 17–26. [Google Scholar] [CrossRef]
- Cunsolo Willox, A.; Harper, S.L.; Ford, J.D.; Edge, V.L.; Landman, K.; Houle, K.; Blake, S.; Wolfrey, C. Climate change and mental health: An exploratory case study from Rigolet, Nunatsiavut, Canada. Clim. Chang. 2013, 121, 255–270. [Google Scholar] [CrossRef]
- Flint, C.G.; Robinson, E.S.; Kellogg, J.; Ferguson, G.; Boufajreldin, L.; Dolan, M.; Raskin, I.; Lila, M.A. Promoting wellness in Alaskan villages: Integrating traditional knowledge and science of wild berries. EcoHealth 2011, 8, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Bunce, A.; Ford, J.; Harper, S.; Edge, V. Ihacc Research Team. Vulnerability and adaptive capacity of Inuit women to climate change: A case study from Iqaluit, Nunavut. Nat. Hazards 2016, 83, 1419–1441. [Google Scholar] [CrossRef]
- McNamara, K.E.; Westoby, R. Solastalgia and the gendered nature of climate change: An example from Erub Island, Torres Strait. EcoHealth 2011, 8, 233–236. [Google Scholar] [CrossRef]
- Rigby, C.W.; Rosen, A.; Berry, H.L.; Hart, C.R. If the land’s sick, we’re sick:* the impact of prolonged drought on the social and emotional well-being of Aboriginal communities in rural New South Wales. Aust J. Rural Health 2011, 19, 249–254. [Google Scholar] [CrossRef]
- Qi, X.; Hu, W.; Mengersen, K.; Tong, S. Socio-environmental drivers and suicide in Australia: Bayesian spatial analysis. BMC Public Health 2014, 14, 681. [Google Scholar] [CrossRef] [Green Version]
- Cooper, S.; Hutchings, P.; Butterworth, J.; Joseph, S.; Kebede, A.; Parker, A.; Terefe, B.; Van Koppen, B. Environmental associated emotional distress and the dangers of climate change for pastoralist mental health. Glob. Environ. Chang. 2019, 59, 1–15. [Google Scholar] [CrossRef]
- Asugeni, J.; MacLaren, D.; Massey, P.D.; Speare, R. Mental health issues from rising sea level in a remote coastal region of the Solomon Islands: Current and future. Australas. Psychiatry Bull. R. Aust. N. Z. Coll. Psychiatr. 2015, 23, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Gibson, K.E.; Barnett, J.; Haslam, N.; Kaplan, I. The mental health impacts of climate change: Findings from a Pacific Island atoll nation. J. Anxiety Disord. 2020, 73, 102237. [Google Scholar] [CrossRef] [PubMed]
- Ayeb-Karlsson, S. ‘When we were children we had dreams, then we came to Dhaka to survive’: Urban stories connecting loss of wellbeing, displacement and (im)mobility. Clim. Dev. 2020, 1–12. [Google Scholar] [CrossRef]
- Ayeb-Karlsson, S. ‘I do not like her going to the shelter’: Stories on gendered disaster (im) mobility and wellbeing loss in coastal Bangladesh. J. Int. J. Disaster Risk Reduct. 2020, 50, 101904. [Google Scholar] [CrossRef]
- Ayeb-Karlsson, S.; Kniveton, D.; Cannon, T. Trapped in the prison of the mind: Notions of climate-induced (im)mobility decision-making and wellbeing from an urban informal settlement in Bangladesh. Palgrave Commun. 2020, 6. [Google Scholar] [CrossRef] [Green Version]
- Hayes, K.; Poland, B.; Cole, D.C.; Agic, B. Psychosocial adaptation to climate change in High River, Alberta: Implications for policy and practice. Can. J. Public Health Rev. Can. De Sante Publique 2020, 111, 880–889. [Google Scholar] [CrossRef]
- Hart, C.R.; Berry, H.L.; Tonna, A.M. Improving the mental health of rural New South Wales communities facing drought and other adversities. Aust. J. Rural Health 2011, 19, 231–238. [Google Scholar] [CrossRef]
- Purcell, R.; McGirr, J. Rural health service managers’ perspectives on preparing rural health services for climate change. Aust. J. Rural Health 2018, 26, 20–25. [Google Scholar] [CrossRef]
- Patrick, R.; Capetola, T. It’s here! Are we ready? Five case studies of health promotion practices that address climate change from within Victorian health care settings. Health Promot. J. Aust. 2011, 22, S61–S67. [Google Scholar] [CrossRef]
- Valois, P.; Blouin, P.; Ouellet, C.; Renaud, J.S.; Belanger, D.; Gosselin, P. The Health Impacts of Climate Change: A Continuing Medical Education Needs Assessment Framework. J. Contin. Educ. Health Prof. 2016, 36, 218–225. [Google Scholar] [CrossRef]
- Wang, S.; Jiang, J.; Zhou, Y.; Li, J.; Zhao, D.; Lin, S. Climate-change information, health-risk perception and residents’ environmental complaint behavior: An empirical study in China. Environ. Geochem. Health 2019, 42, 719–732. [Google Scholar] [CrossRef]
- Netuveli, G.; Watts, P. Pro-environmental behaviours and attitudes are associated with health, wellbeing and life satisfaction in multiple occupancy households in the UK Household Longitudinal Study. Popul. Environ. 2020, 41, 347–371. [Google Scholar] [CrossRef]
- Heaney, A.K.; Winter, S.J. Climate-driven migration: An exploratory case study of Maasai health perceptions and help-seeking behaviors. Int. J. Public Health 2016, 61, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Petrasek MacDonald, J.; Cunsolo Willox, A.; Ford, J.D.; Shiwak, I.; Wood, M. Protective factors for mental health and well-being in a changing climate: Perspectives from Inuit youth in Nunatsiavut, Labrador. Soc. Sci. Med. 2015, 141, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Sawatzky, A.; Cunsolo, A.; Jones-Bitton, A.; Gillis, D.; Wood, M.; Flowers, C.; Shiwak, I.; Harper, S.L.; Rigolet Inuit Community, G. “The best scientists are the people that’s out there”: Inuit-led integrated environment and health monitoring to respond to climate change in the Circumpolar North. Clim. Chang. 2020, 160, 45–66. [Google Scholar] [CrossRef]
- Harper, S.L.; Edge, V.L.; Ford, J.; Willox, A.C.; Wood, M.; McEwen, S.A. Climate-sensitive health priorities in Nunatsiavut, Canada. BMC Public Health 2015, 15, 605. [Google Scholar] [CrossRef] [Green Version]
- MacFarlane, E.K.; Shakya, R.; Berry, H.L.; Kohrt, B.A. Implications of participatory methods to address mental health needs associated with climate change: ‘Photovoice’ in Nepal. BJPsych. Int. 2015, 12, 33–35. [Google Scholar] [CrossRef] [Green Version]
- Raker, E.J.; Arcaya, M.C.; Lowe, S.R.; Zacher, M.; Rhodes, J.; Waters, M.C. Mitigating Health Disparities After Natural Disasters: Lessons From The RISK Project: Study examines mitigating health disparities after natural disasters. Health Aff. 2020, 39, 2128–2135. [Google Scholar] [CrossRef]
- Sorgho, R.; Mank, I.; Kagoné, M.; Souares, A.; Danquah, I.; Sauerborn, R.J.I.J.o.E.R.; Health, P. “We Will Always Ask Ourselves the Question of How to Feed the Family”: Subsistence Farmers’ Perceptions on Adaptation to Climate Change in Burkina Faso. Int. J. Environ. Res. Public Health 2020, 17, 7200. [Google Scholar] [CrossRef]
- Wong-Parodi, G. When climate change adaptation becomes a “looming threat” to society: Exploring views and responses to California wildfires and public safety power shutoffs. Energy Res. Soc. Sci. 2020, 70. [Google Scholar] [CrossRef]
- McIver, L.; Kim, R.; Woodward, A.; Hales, S.; Spickett, J.; Katscherian, D.; Hashizume, M.; Honda, Y.; Kim, H.; Iddings, S.; et al. Health Impacts of Climate Change in Pacific Island Countries: A Regional Assessment of Vulnerabilities and Adaptation Priorities. Environ. Health Perspect. 2016, 124, 1707–1714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seidel, B.M.; Bell, E. Health adaptation policy for climate vulnerable groups: A ‘critical computational linguistics’ analysis. BMC Public Health 2014, 14, 1235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valois, P.; Caron, M.; Gousse-Lessard, A.S.; Talbot, D.; Renaud, J.S. Development and validation of five behavioral indices of flood adaptation. BMC Public Health 2019, 19, 245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maughan, D.L.; Patel, A.; Parveen, T.; Braithwaite, I.; Cook, J.; Lillywhite, R.; Cooke, M. Primary-care-based social prescribing for mental health: An analysis of financial and environmental sustainability. Prim. Health Care Res. Dev. 2016, 17, 114–121. [Google Scholar] [CrossRef] [PubMed]
- PRISM Climate Group. PRISM Climate Data. Available online: https://prism.oregonstate.edu/ (accessed on 8 February 2021).
- Berkeley Earth. Data Overview. Available online: http://berkeleyearth.org/data/ (accessed on 8 February 2021).
- Schinasi, L.H.; Benmarhnia, T.; De Roos, A.J. Modification of the association between high ambient temperature and health by urban microclimate indicators: A systematic review and meta-analysis. Environ. Res. 2018, 161, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Tsoka, S.; Tsikaloudaki, K.; Theodosiou, T.; Bikas, D. Urban Warming and Cities’ Microclimates: Investigation Methods and Mitigation Strategies—A Review. Energies 2020, 13, 1414. [Google Scholar] [CrossRef] [Green Version]
- Weissbecker, I. Climate Change and Human Well-Being Global Challenges and Opportunities; Springer: New York, NY, USA, 2011. [Google Scholar]
- Kameg, B.N. Climate Change and Mental Health: Implications for Nurses. J. Psychosoc. Nurs. Ment. Health Serv. 2020, 58, 25–30. [Google Scholar] [CrossRef]
- Nicholas, P.K.; Breakey, S.; White, B.P.; Brown, M.J.; Fanuele, J.; Starodub, R.; Ros, A.V. Mental Health Impacts of Climate Change: Perspectives for the ED Clinician. J. Emerg. Nurs. 2020, 46, 590–599. [Google Scholar] [CrossRef]
- Liu, J.; Potter, T.; Zahner, S. Policy brief on climate change and mental health/well-being. Nurs. Outlook 2020, 68, 517–522. [Google Scholar] [CrossRef]
- Pinsky, E.; Guerrero, A.P.S.; Livingston, R. Our House Is on Fire: Child and Adolescent Psychiatrists in the Era of the Climate Crisis. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 580–582. [Google Scholar] [CrossRef]
- Seritan, A.L.; Seritan, I. The Time Is Now: Climate Change and Mental Health. Acad. Psychiatry 2020, 44, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Arabena, K.; Armstrong, F.; Berry, H.; Brooks, P.; Capon, T.; Crabb, B.; Demaio, A.; Doherty, P.; Lewin, S.; Lo, S.; et al. Australian health professionals’ statement on climate change and health. Lancet 2018, 392, 2169–2170. [Google Scholar] [CrossRef] [Green Version]
- Berry, H.L.; Waite, T.D.; Dear, K.B.; Capon, A.G.; Murray, V. The case for systems thinking about climate change and mental health. Nat. Clim. Chang. 2018, 8, 282–290. [Google Scholar] [CrossRef]
- Clayton, S.; Karazsia, B.T. Development and validation of a measure of climate change anxiety. J. Environ. Psychol. 2020, 69. [Google Scholar] [CrossRef]
- Hope, E.C.; Velez, G.; Offidani-Bertrand, C.; Keels, M.; Durkee, M.I. Political activism and mental health among Black and Latinx college students. Cult. Divers. Ethn. Minor. Psychol. 2018, 24, 26–39. [Google Scholar] [CrossRef]
- World Health Organization. Health and Climate Change Country Profiles. Available online: https://www.who.int/activities/monitoring-health-impacts-of-climate-change-and-national-progress (accessed on 10 March 2021).
- World Health Organization. Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization. mhGAP Humanitarian Intervention Guide (mhGAP-HIG): Clinical Management of Mental, Neurological and Substance Use Conditions in Humanitarian Emergencies. Available online: http://www.who.int/mental_health/publications/mhgap_hig/en/ (accessed on 10 March 2021).
- World Health Organization. Building Back Better: Sustainable Mental Health Care after Emergencies. Available online: https://www.who.int/mental_health/emergencies/building_back_better/en/ (accessed on 10 March 2021).
- World Health Organization. Scalable Psychological Interventions for People in Communities Affected by Adversity: A New Area of Mental Health and Psychosocial Work at WHO. Available online: https://apps.who.int/iris/handle/10665/254581 (accessed on 10 March 2021).
- Palinkas, L.A.; O’Donnell, M.L.; Lau, W.; Wong, M.J.I.J.O.E.R.; Health, P. Strategies for Delivering Mental Health Services in Response to Global Climate Change: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 8562. [Google Scholar] [CrossRef]
- Climate and Health Alliance. Climate and Health Alliance. Available online: https://www.caha.org.au/ (accessed on 2 November 2020).
- Fearnley, E.J.; Magalhaes, R.J.; Speldewinde, P.; Weinstein, P.; Dobson, A. Environmental correlates of mental health measures for women in Western Australia. EcoHealth 2014, 11, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Woodward, A.; Campbell-Lendrum, D.D.; Chadee, D.; Honda, Y.; Liu, Q.; Olwoch, J.M.; Revich, B.; Sauerborn, R. Human health: Impacts, adaptation, and co-benefits. In Climate Change 2014: Impacts, Adaptation, and Vulnerability; Cambridge University Press: Cambridge, UK, 2014; pp. 709–754. [Google Scholar]
- Hayes, K.; Blashki, G.; Wiseman, J.; Burke, S.; Reifels, L. Climate change and mental health: Risks, impacts and priority actions. Int. J. Ment. Health Syst. 2018, 12, 28. [Google Scholar] [CrossRef]
- Maplecroft, V. Climate Change Vulnerabillity Index 2017. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/verisk%20index.pdf (accessed on 10 March 2021).
- Ingle, H.E.; Mikulewicz, M. Mental health and climate change: Tackling invisible injustice. Lancet Planet. Health 2020, 4, e128–e130. [Google Scholar] [CrossRef]
- Goldmann, E.; Galea, S. Mental health consequences of disasters. Annu. Rev. Public Health 2014, 35, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Watts, N.; Amann, M.; Ayeb-Karlsson, S.; Belesova, K.; Bouley, T.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; Chambers, J.; et al. The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. Lancet 2018, 391, 581–630. [Google Scholar] [CrossRef]
- Patel, V.; Saxena, S.; Lund, C.; Thornicroft, G.; Baingana, F.; Bolton, P.; Chisholm, D.; Collins, P.Y.; Cooper, J.L.; Eaton, J.; et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018, 392, 1553–1598. [Google Scholar] [CrossRef] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charlson, F.; Ali, S.; Benmarhnia, T.; Pearl, M.; Massazza, A.; Augustinavicius, J.; Scott, J.G. Climate Change and Mental Health: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 4486. https://doi.org/10.3390/ijerph18094486
Charlson F, Ali S, Benmarhnia T, Pearl M, Massazza A, Augustinavicius J, Scott JG. Climate Change and Mental Health: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(9):4486. https://doi.org/10.3390/ijerph18094486
Chicago/Turabian StyleCharlson, Fiona, Suhailah Ali, Tarik Benmarhnia, Madeleine Pearl, Alessandro Massazza, Jura Augustinavicius, and James G. Scott. 2021. "Climate Change and Mental Health: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 9: 4486. https://doi.org/10.3390/ijerph18094486
APA StyleCharlson, F., Ali, S., Benmarhnia, T., Pearl, M., Massazza, A., Augustinavicius, J., & Scott, J. G. (2021). Climate Change and Mental Health: A Scoping Review. International Journal of Environmental Research and Public Health, 18(9), 4486. https://doi.org/10.3390/ijerph18094486







