What Happened Pre- and during COVID-19 in South Korea? Comparing Physical Activity, Sleep Time, and Body Weight Status
Abstract
:1. Introduction
2. Methods
2.1. Study Participants
2.2. Levels of Social Distancing
2.3. Measures
2.3.1. Device-Based Physical Activity
2.3.2. Self-Reported Sleep Time
2.3.3. Self-Reported Body Weight Changes
2.3.4. Other Study Covariates
2.4. Statistical Analysis
3. Results
3.1. Average Daily Step Counts per Month and Level of Social Distancing in COVID-19
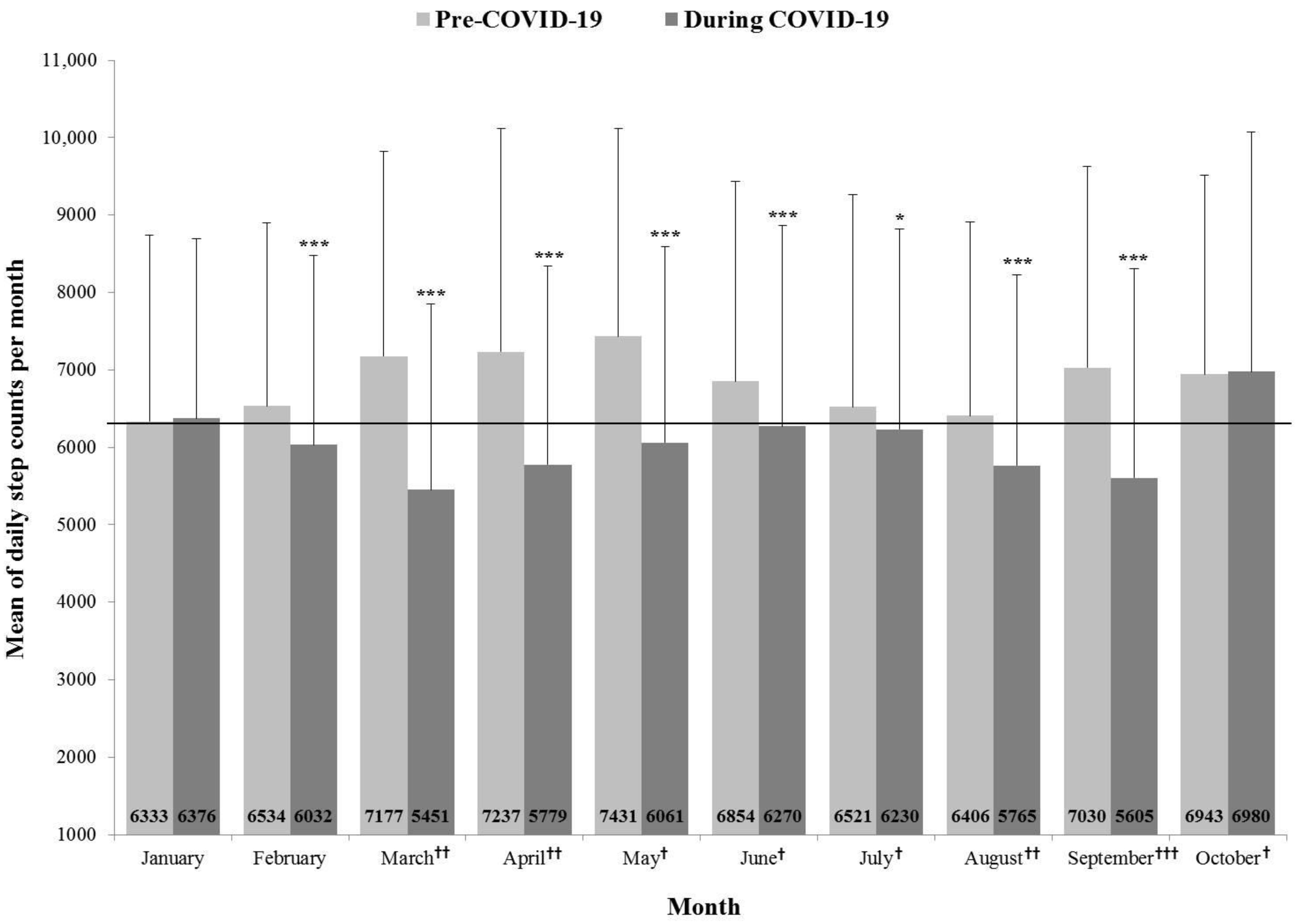
3.2. Average Daily Step Counts per Month and Pre- and during COVID-19
3.3. Average Sleep Time and Pre- and during COVID-19
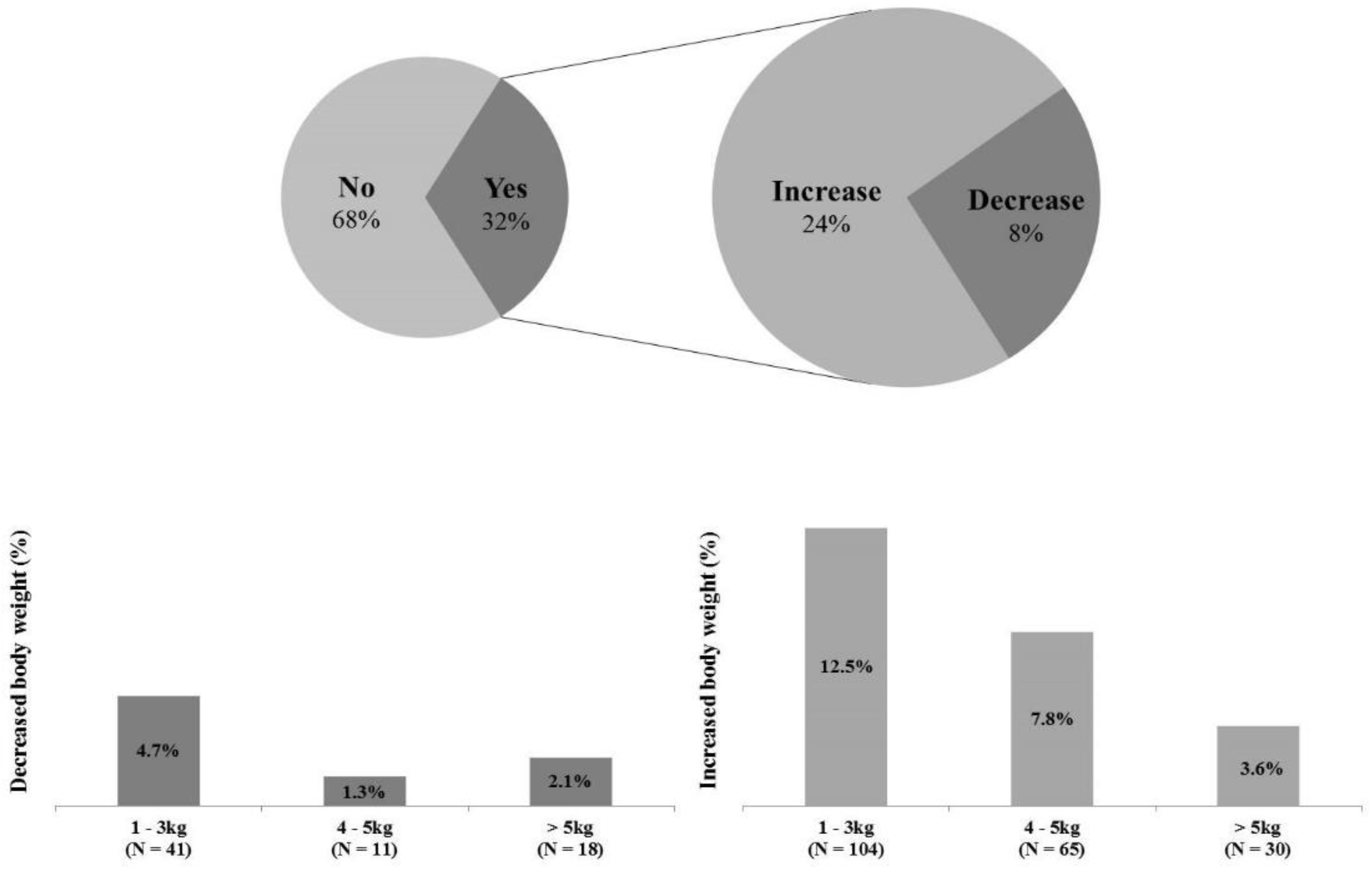
3.4. Body Weight and Pre- and during COVID-19
4. Discussion
4.1. Average Daily Step Counts per Month and Level of Social Distancing in COVID-19
4.2. Average Daily Step Counts per Month and Pre- and during COVID-19
4.3. Average Sleep Time and Pre- and during COVID-19
4.4. Body Weight and Pre- and during COVID-19
4.5. Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Carlson, S.A.; Adams, E.K.; Yang, Z.; Fulton, J.E. Percentage of Deaths Associated With Inadequate Physical Activity in the United States. Prev. Chronic Dis. 2018, 15, E38. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Gale, J.; Bauman, A.; Ekelund, U.; Hamer, M.; Ding, D. Sitting Time, Physical Activity, and Risk of Mortality in Adults. J. Am. Coll. Cardiol. 2019, 73, 2062–2072. [Google Scholar] [CrossRef]
- Reidy, P.T.; Yonemura, N.M.; Madsen, J.H.; McKenzie, A.I.; Mahmassani, Z.S.; Rondina, M.T.; Lin, Y.K.; Kaput, K.; Drummond, M.J. An accumulation of muscle macrophages is accompanied by altered insulin sensitivity after reduced activity and recovery. Acta Physiol. 2019, 226, e13251. [Google Scholar] [CrossRef]
- Zheng, Q.; Cui, G.; Chen, J.; Gao, H.; Wei, Y.; Uede, T.; Chen, Z.; Diao, H. Regular Exercise Enhances the Immune Response Against Microbial Antigens Through Up-Regulation of Toll-like Receptor Signaling Pathways. Cell. Physiol. Biochem. 2015, 37, 735–746. [Google Scholar] [CrossRef] [PubMed]
- Laddu, D.R.; Lavie, C.J.; Phillips, S.A.; Arena, R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic. Prog. Cardiovasc. Dis. 2020, 64, S0033–S0620. [Google Scholar] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Colley, R.C.; Garriguet, D.; Janssen, I.; Wong, S.L.; Saunders, T.J.; Carson, V.; Tremblay, M.S. The association between accelerometer-measured patterns of sedentary time and health risk in children and youth: Results from the Canadian Health Measures Survey. BMC Public Health 2013, 13, 200. [Google Scholar] [CrossRef]
- Carson, V.; Stone, M.; Faulkner, G. Patterns of sedentary behavior and weight status among children. Pediatric Exerc. Sci. 2014, 26, 95–102. [Google Scholar] [CrossRef]
- Flausino, N.H.; Da Silva Prado, J.M.; de Queiroz, S.S.; Tufik, S.; de Mello, M.T. Physical exercise performed before bedtime improves the sleep pattern of healthy young good sleepers. Psychophysiology 2012, 49, 186–192. [Google Scholar] [CrossRef]
- Gilbert, S.S.; van den Heuvel, C.J.; Ferguson, S.A.; Dawson, D. Thermoregulation as a sleep signalling system. Sleep Med. Rev. 2004, 8, 81–93. [Google Scholar] [CrossRef]
- Besedovsky, L.; Lange, T.; Born, J. Sleep and immune function. Pflügers Arch. Eur. J. Physiol. 2012, 463, 121–137. [Google Scholar] [CrossRef]
- Hong, H.; Schotland, H.; Perez, I.A. Sleep and Performance. Am. J. Respir. Crit. Care Med. 2018, 197, 13–14. [Google Scholar] [CrossRef]
- Ferrie, J.E.; Shipley, M.J.; Akbaraly, T.N.; Marmot, M.G.; Kivimäki, M.; Singh-Manoux, A. Change in sleep duration and cognitive function: Findings from the Whitehall II Study. Sleep 2011, 34, 565–573. [Google Scholar] [CrossRef]
- Surani, S.R. Diabetes, sleep apnea, obesity and cardiovascular disease: Why not address them together? World J. Diabetes 2014, 5, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Knutson, K.L. Does inadequate sleep play a role in vulnerability to obesity? Am. J. Hum. Biol. 2012, 24, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Sparling, P.B.; Healy, G.N.; Dunstan, D.W.; Matthews, C.E. Sedentary behavior: Emerging evidence for a new health risk. Mayo Clin. Proc. 2010, 85, 1138–1141. [Google Scholar] [CrossRef]
- Matricciani, L.; Bin, Y.S.; Lallukka, T.; Kronholm, E.; Dumuid, D.; Paquet, C.; Olds, T. Past, present, and future: Trends in sleep duration and implications for public health. Sleep Health 2017, 3, 317–323. [Google Scholar] [CrossRef]
- Ding, D.; Nguyen, B.; Learnihan, V.; Bauman, A.E.; Davey, R.; Jalaludin, B.; Gebel, K. Moving to an active lifestyle? A systematic review of the effects of residential relocation on walking, physical activity and travel behaviour. Br. J. Sports Med. 2018, 52, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Samson, D.R.; Crittenden, A.N.; Mabulla, I.A.; Mabulla, A.Z.; Nunn, C.L. Hadza sleep biology: Evidence for flexible sleep-wake patterns in hunter-gatherers. Am. J. Phys. Anthropol. 2017, 162, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.; Yang, X.; Tsui, H.Y.; Kim, J.H. Impacts of SARS on health-seeking behaviors in general population in Hong Kong. Prev. Med. 2005, 41, 454–462. [Google Scholar] [CrossRef]
- Morganstein, J.C.; Fullerton, C.S.; Ursano, R.J.; Donato, D.; Holloway, H.C. Pandemics: Health care emergencies. In Textbook of Disaster Psychiatry, 2nd ed.; Cambridge Univ Pr: Cambridge, UK, 2017; pp. 270–283. [Google Scholar]
- Gastañaduy, P.A.; Funk, S.; Paul, P.; Tatham, L.; Fisher, N.; Budd, J.; Fowler, B.; de Fijter, S.; DiOrio, M.; Wallace, G.S.; et al. Impact of Public Health Responses During a Measles Outbreak in an Amish Community in Ohio: Modeling the Dynamics of Transmission. Am. J. Epidemiol. 2018, 187, 2002–2010. [Google Scholar] [CrossRef] [PubMed]
- Liao, Q.; Cowling, B.J.; Lam, W.W.; Ng, D.M.; Fielding, R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infect. Dis. 2014, 14, 169. [Google Scholar] [CrossRef]
- Serino, L.; Meleleo, C.; Maurici, M.; Bagnato, B.; Sorbara, D.; Zaratti, L.; Franco, E. Knowledge and worry as basis for different behaviors among university students: The case of pandemic flu H1N1v. J. Prev. Med. Hyg. 2011, 52, 144–147. [Google Scholar]
- Bourdas, D.; Zacharakis, E. Impact of lockdown on physical activity in the early COVID-19 presence: Greece national cross-sectional study. Lancet 2020, 31. [Google Scholar] [CrossRef]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide effect of COVID-19 on physical activity: A descriptive study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef]
- Kim, M.-H.; Cho, W.; Choi, H.; Hur, J.-Y. Assessing the South Korean Model of Emergency Management during the COVID-19 Pandemic. Asian Stud. Rev. 2020, 22, 1–12. [Google Scholar] [CrossRef]
- Park, S.; Kim, B.; Lee, J. Social Distancing and Outdoor Physical Activity during the COVID-19 Outbreak in South Korea: Implications for Physical Distancing Strategies. Asia Pac. J. Public Health 2020, 32, 360–362. [Google Scholar] [CrossRef]
- Höchsmann, C.; Knaier, R. Validity of activity trackers, smartphones, and phone applications to measure steps in various walking conditions. Scand. J. Med. Sci. Sports 2018, 28, 1818–1827. [Google Scholar] [CrossRef]
- Hekler, E.B.; Buman, M.P. Validation of Physical Activity Tracking via Android Smartphones Compared to ActiGraph Accelerometer: Laboratory-Based and Free-Living Validation Studies. J. Med. Internet Res. 2015, 3, e36. [Google Scholar] [CrossRef]
- Dunton, G.F.; Wang, S.D.; Do, B.; Courtney, J. Early effects of the COVID-19 pandemic on physical activity locations and behaviors in adults living in the United States. Prev. Med. Rep. 2020, 20, 101241. [Google Scholar] [CrossRef]
- González, M.C.; Hidalgo, C.A.; Barabási, A.L. Understanding individual human mobility patterns. Nature 2008, 453, 779–782. [Google Scholar] [CrossRef]
- Althoff, T.; Sosič, R.; Hicks, J.L.; King, A.C.; Delp, S.L.; Leskovec, J. Large-scale physical activity data reveal worldwide activity inequality. Nature 2017, 547, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Case, M.A.; Burwick, H.A.; Volpp, K.G.; Patel, M.S. Accuracy of smartphone applications and wearable devices for tracking physical activity data. Jama 2015, 313, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Casadevall, A. Climate change brings the specter of new infectious diseases. J. Clin. Investig. 2020, 130, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Stimson, G.V. The future of global health is urban health. Lancet (Lond. Engl.) 2013, 382, 1475. [Google Scholar] [CrossRef]
- Wu, T.; Perrings, C.; Kinzig, A.; Collins, J.P.; Minteer, B.A.; Daszak, P. Economic growth, urbanization, globalization, and the risks of emerging infectious diseases in China: A review. Ambio 2017, 46, 18–29. [Google Scholar] [CrossRef]
- Choi, J.; Cho, Y.; Shim, E.; Woo, H. Web-based infectious disease surveillance systems and public health perspectives: A systematic review. BMC Public Health 2016, 16, 1238. [Google Scholar] [CrossRef]
- Zumla, A.; Dar, O.; Kock, R.; Muturi, M.; Ntoumi, F.; Kaleebu, P.; Eusebio, M.; Mfinanga, S.; Bates, M.; Mwaba, P.; et al. Taking forward a ‘One Health’ approach for turning the tide against the Middle East respiratory syndrome coronavirus and other zoonotic pathogens with epidemic potential. Int. J. Infect. Dis. 2016, 47, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Staiano, M.F.; Marcelli, F. Italy’s response to COVID-19 and the need for International Cooperation. Relac. Int. 2020, 58, 117–137. [Google Scholar]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B. Physical Activity Change during COVID-19 Confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef] [PubMed]
- Plasqui, G.; Westerterp, K.R. Seasonal variation in total energy expenditure and physical activity in Dutch young adults. Obes. Res. 2004, 12, 688–694. [Google Scholar] [CrossRef]
- Clemes, S.A.; Hamilton, S.L.; Griffiths, P.L. Summer to winter variability in the step counts of normal weight and overweight adults living in the UK. J. Phys. Act. Health 2011, 8, 36–44. [Google Scholar] [CrossRef]
- Hamilton, S.L.; Clemes, S.A.; Griffiths, P.L. UK adults exhibit higher step counts in summer compared to winter months. Ann. Hum. Biol. 2008, 35, 154–169. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, S.E.; Griffiths, P.L.; Clemes, S.A. Seasonal variation in physical activity, sedentary behaviour and sleep in a sample of UK adults. Ann. Hum. Biol. 2014, 41, 1–8. [Google Scholar] [CrossRef]
- McCormack, G.R.; Friedenreich, C.; Shiell, A.; Giles-Corti, B.; Doyle-Baker, P.K. Sex- and age-specific seasonal variations in physical activity among adults. J. Epidemiol. Community Health 2010, 64, 1010–1016. [Google Scholar] [CrossRef]
- Chouchou, F.; Augustini, M.; Caderby, T.; Caron, N.; Turpin, N.A.; Dalleau, G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: Reunion island as a case study. Sleep Med. 2020, S1389, 30417. [Google Scholar]
- Mulgrew, A.T.; Ryan, C.F.; Fleetham, J.A.; Cheema, R.; Fox, N.; Koehoorn, M.; Fitzgerald, J.M.; Marra, C.; Ayas, N.T. The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med. 2007, 9, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Uehli, K.; Mehta, A.J.; Miedinger, D.; Hug, K.; Schindler, C.; Holsboer-Trachsler, E.; Leuppi, J.D.; Künzli, N. Sleep problems and work injuries: A systematic review and meta-analysis. Sleep Med. Rev. 2014, 18, 61–73. [Google Scholar] [CrossRef]
- Ingram, J.; Maciejewski, G.; Hand, C.J. Changes in Diet, Sleep, and Physical Activity Are Associated With Differences in Negative Mood during COVID-19 Lockdown. Front. Psychol. 2020, 11, 588–604. [Google Scholar]
- Sánchez-Sánchez, E.; Ramírez-Vargas, G.; Avellaneda-López, Y.; Orellana-Pecino, J.I. Eating Habits and Physical Activity of the Spanish Population during the COVID-19 Pandemic Period. Nutrients 2020, 12, 2826. [Google Scholar] [CrossRef] [PubMed]
- López-Bueno, R.; Calatayud, J.; Casaña, J.; Casajús, J.A.; Smith, L.; Tully, M.A.; Andersen, L.L.; López-Sánchez, G.F. COVID-19 Confinement and Health Risk Behaviors in Spain. Front. Psychol. 2020, 11, 1426. [Google Scholar] [CrossRef] [PubMed]
- Alford, C.; Martinkova, Z.; Tiplady, B.; Reece, R.; Verster, J.C. The Effects of Alcohol Hangover on Mood and Performance Assessed at Home. J. Clin. Med. 2020, 9, 1068. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Kraus, W.E.; Janz, K.F.; Powell, K.E.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Daily Step Counts for Measuring Physical Activity Exposure and Its Relation to Health. Med. Sci. Sports Exerc. 2019, 51, 1206–1212. [Google Scholar] [CrossRef]
- Hall, K.S.; Hyde, E.T.; Bassett, D.R.; Carlson, S.A.; Carnethon, M.R.; Ekelund, U.; Evenson, K.R.; Galuska, D.A.; Kraus, W.E.; Lee, I.M.; et al. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 78. [Google Scholar] [CrossRef]

| Variable | All Participants | ||
|---|---|---|---|
| No. (%) | Mean ± SD | ||
| Age (year) | 23.7 ± 6.0 | ||
| Gender | Male | 454 (54.4) | |
| Female | 380 (45.6) | ||
| Anthropometrics | Height (cm) | 170.0 ± 8.9 | |
| Weight (kg) | 64.8 ± 13.5 | ||
| BMI (kg·m-2) | 22.3 ± 3.7 | ||
| Location | Urban | 212 (25.4) | |
| Suburban | 427 (51.2) | ||
| Rural | 177 (21.2) | ||
| Education | Less than high school | 0 (0.0) | |
| High school diploma | 0 (0.0) | ||
| Some college | 712 (85.4) | ||
| College graduate | 79 (9.5) | ||
| Graduate degree | 43 (5.2) | ||
| Annual Household Income | <1000 thousand KRW (USD < 915) | 394 (47.2) | |
| 1000–2000 thousand KRW (USD 915–1830) | 43 (5.2) | ||
| 2000–3000 thousand KRW (USD 1830–2745) | 34 (4.1) | ||
| ≥3000 thousand KRW (USD ≥ 2745) | 48 (5.8) | ||
| Occupation | Office workers | 23 (2.8) | |
| Administrators, managers, and professionals | 19 (2.3) | ||
| Skilled agricultural and fishery workers | 44 (5.3) | ||
| Students | 742 (89.0) | ||
| Jobless (e.g., housewife) | 5 (0.6) | ||
| Married | Married or living as married | 58 (7.0) | |
| Single | 774 (92.8) | ||
| Infection of COVID-19 | Yes | 0 (0.0) | |
| No | 834 (100.0) | ||
| Variable | Pre-COVID-19 (n = 576) | during COVID-19 | ||||
|---|---|---|---|---|---|---|
| Level 1 (n = 597) | Level 2 (n = 587) | Level 2.5 (n = 587) | ||||
| Overall | 6747.09 ± 1987.55 | 6208.77 ± 2320.85 *** | 5616.35 ± 2181.45 *** | 5611.19 ± 2702.18 *** | ||
| Gender | Male | 7002.45 ± 1992.47 | 6545.95 ± 2379.93 | 5892.16 ± 2199.26 | 5659.44 ± 2553.51 | |
| Female | 6500.44 ± 1944.64 | 5877.19 ± 2215.57 | 5347.04 ± 2133.38 | 5564.39 ± 2842.47 | ||
| Location | Urban | 6986.71 ± 1926.39 | 6236.50 ± 2269.87 | 5462.51 ± 1973.94 | 5474.28 ± 2706.81 | |
| Suburban | 6778.90 ± 1933.82 | 6241.32 ± 2120.55 | 5786.31 ± 2121.34 | 5497.52 ± 2552.63 | ||
| Rural | 6380.80 ± 2162.28 | 6037.84 ± 2740.61 | 5358.23 ± 2471.12 | 5966.95 ± 2858.90 | ||
| Gender × Location | Urban | Male | 7280.85 ± 1659.71 | 6639.77 ± 2099.91 | 5790.21 ± 1936.97 | 5701.71 ± 2442.82 |
| Female | 6791.79 ± 2071.11 | 5963.01 ± 2350.71 | 5251.58 ± 1979.71 | 5325.27 ± 2870.63 | ||
| Suburban | Male | 7000.71 ± 2000.49 | 6395.19 ± 2162.82 | 5875.33 ± 2134.69 | 5488.27 ± 2361.61 | |
| Female | 6495.83 ± 1813.43 | 6043.16 ± 2055.61 | 5671.76 ± 2106.34 | 5509.27 ± 2785.26 | ||
| Rural | Male | 6738.55 ± 2300.28 | 6921.85 ± 3215.30 | 6063.09 ± 2681.75 | 6167.73 ± 3186.09 | |
| Female | 6100.82 ± 2020.65 | 5309.84 ± 2027.60 | 4769.10 ± 2126.18 | 5799.15 ± 2566.35 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-H.; Yoo, E.; Kim, Y.; Lee, J.-M. What Happened Pre- and during COVID-19 in South Korea? Comparing Physical Activity, Sleep Time, and Body Weight Status. Int. J. Environ. Res. Public Health 2021, 18, 5863. https://doi.org/10.3390/ijerph18115863
Park J-H, Yoo E, Kim Y, Lee J-M. What Happened Pre- and during COVID-19 in South Korea? Comparing Physical Activity, Sleep Time, and Body Weight Status. International Journal of Environmental Research and Public Health. 2021; 18(11):5863. https://doi.org/10.3390/ijerph18115863
Chicago/Turabian StylePark, Jeong-Hui, Eunhye Yoo, Youngdeok Kim, and Jung-Min Lee. 2021. "What Happened Pre- and during COVID-19 in South Korea? Comparing Physical Activity, Sleep Time, and Body Weight Status" International Journal of Environmental Research and Public Health 18, no. 11: 5863. https://doi.org/10.3390/ijerph18115863
APA StylePark, J.-H., Yoo, E., Kim, Y., & Lee, J.-M. (2021). What Happened Pre- and during COVID-19 in South Korea? Comparing Physical Activity, Sleep Time, and Body Weight Status. International Journal of Environmental Research and Public Health, 18(11), 5863. https://doi.org/10.3390/ijerph18115863








