Pain Neuroscience Education Combined with Therapeutic Exercises Provides Added Benefit in the Treatment of Chronic Neck Pain
Abstract
:1. Introduction
2. Materials and Methods
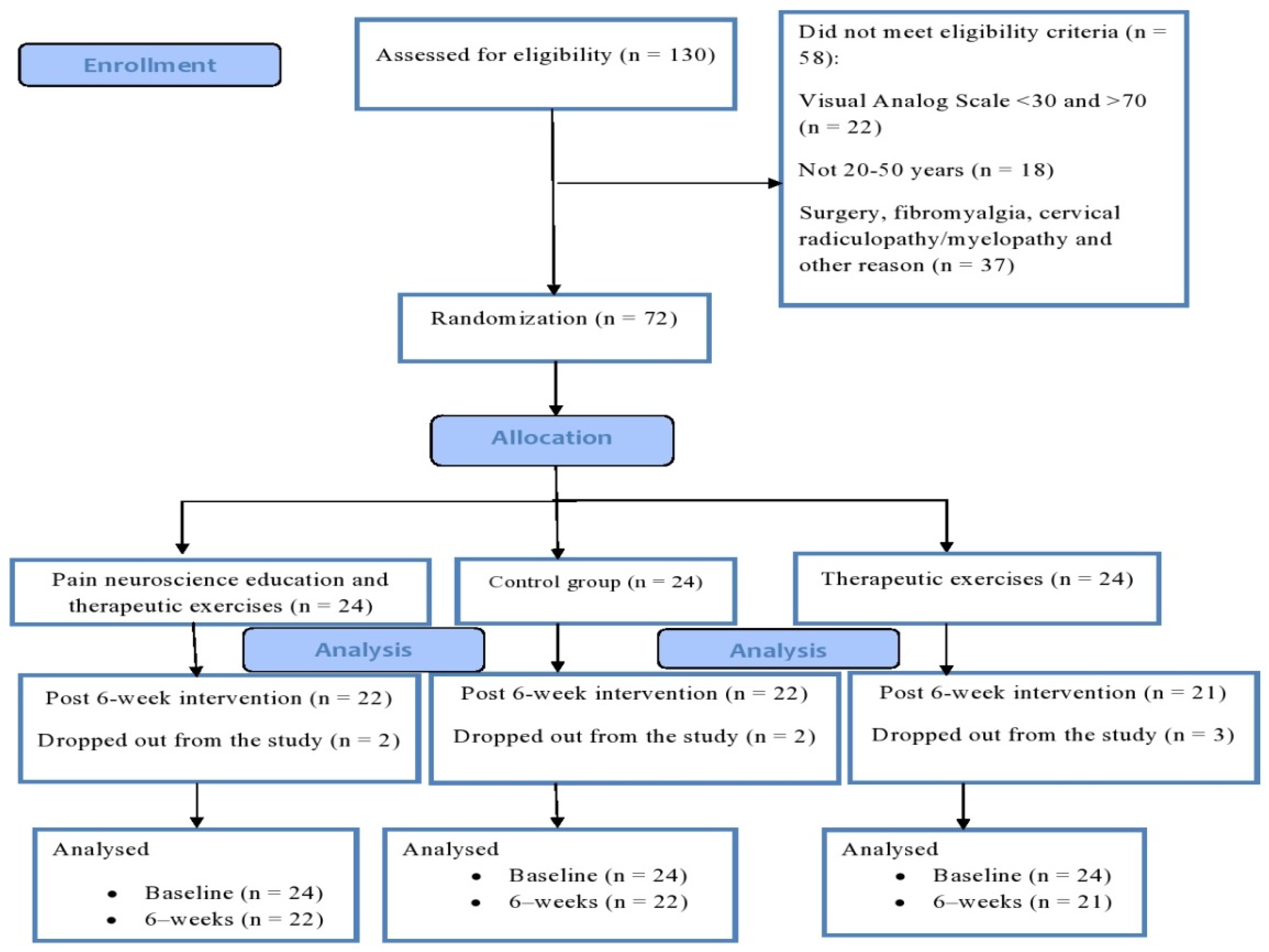
2.1. Study Design
2.2. Outcome Measures
2.2.1. Neck Pain and Disability Scale (NPAD)
2.2.2. Fear–Avoidance Beliefs
2.2.3. Pain Catastrophizing
2.2.4. Pain Self-Efficacy
2.3. Interventions
2.3.1. Therapeutic Exercises
2.3.2. Pain Neuroscience Education
2.3.3. Control Group
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hanvold, T.N.; Wærsted, M.; Mengshoel, A.M.; Bjertness, E.; Twisk, J.; Veiersted, K.B. A longitudinal study on risk factors for neck and shoulder pain among young adults in the transition from technical school to working life. Scand. J. Work. Environ. Health 2014, 40, 597–609. [Google Scholar] [CrossRef] [Green Version]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity amonhg dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef] [Green Version]
- Hogg-Johnson, S.; van der Velde, G.; Carroll, L.J.; Holm, L.W.; Cassidy, J.D.; Guzman, J.; Côté, P.; Haldeman, S.; Ammendolia, C.; Carragee, E.; et al. The Burden and Determinants of Neck Pain in the General Population: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. J. Manip. Physiol. Ther. 2009, 32, S46–S60. [Google Scholar] [CrossRef]
- Miranda, I.F.; Neto, E.S.W.; Dhein, W.; Brodt, G.A.; Loss, J.F. Individuals With Chronic Neck Pain Have Lower Neck Strength Than Healthy Controls: A Systematic Review With Meta-Analysis. J. Manip. Physiol. Ther. 2019, 42, 608–622. [Google Scholar] [CrossRef] [PubMed]
- Barton, P.M.; Hayes, K.C. Neck flexor muscle strength, efficiency, and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch. Phys. Med. Rehabil. 1996, 77, 680–687. [Google Scholar] [CrossRef]
- Gross, A.; Kay, T.M.; Paquin, J.P.; Blanchette, S.; Lalonde, P.; Christie, T.; Dupont, G.; Graham, N.; Burnie, S.J.; Gelley, G.; et al. Exercises for mechanical neck disorders. Cochrane Database Syst. Rev. 2015, 1, CD004250. [Google Scholar] [CrossRef]
- Thompson, D.P.; Urmston, M.; Oldham, J.A.; Woby, S.R. The association between cognitive factors, pain and disability in patients with idiopathic chronic neck pain. Disabil. Rehabil. 2010, 32, 1758–1767. [Google Scholar] [CrossRef]
- Dimitriadis, Z.; Kapreli, E.; Strimpakos, N.; Oldham, J. Do psychological states associate with pain and disability in chronic neck pain patients? J. Back Musculoskelet. Rehabil. 2015, 28, 797–802. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M. Social context and acceptance of chronic pain: The role of solicitous and punishing responses. Pain 2005, 113, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.; Thorn, B.; Haythornthwaite, J.A.; Keefe, F.; Martin, M.; Bradley, L.A.; Lefebvre, J.C. Theoretical Perspectives on the Relation Between Catastrophizing and Pain. Clin. J. Pain 2001, 17, 52–64. [Google Scholar] [CrossRef]
- Pool, J.J.; Ostelo, R.; Knol, D.; Bouter, L.; De Vet, H.C. Are psychological factors prognostic indicators of outcome in patients with sub-acute neck pain? Man. Ther. 2010, 15, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.-C.; Chiu, T.T.; Lam, T.H. The role of fear-avoidance beliefs in patients with neck pain: Relationships with current and future disability and work capacity. Clin. Rehabil. 2007, 21, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Rocca, B.; Cazzaniga, D.; Liquori, V.; Pedrocchi, A.; Vernon, H. Group-based multimodal exercises integrated with cognitive-behavioural therapy improve disability, pain and quality of life of subjects with chronic neck pain: A randomized controlled trial with one-year follow-up. Clin. Rehabil. 2017, 31, 742–752. [Google Scholar] [CrossRef]
- Meeus, M.; Nijs, J.; Van Oosterwijck, J.; Van Alsenoy, V.; Truijen, S. Pain Physiology Education Improves Pain Beliefs in Patients With Chronic Fatigue Syndrome Compared With Pacing and Self-Management Education: A Double-Blind Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2010, 91, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The Effect of Neuroscience Education on Pain, Disability, Anxiety, and Stress in Chronic Musculoskeletal Pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef]
- Pires, D.; Cruz, E.; Caeiro, C. Aquatic exercise and pain neurophysiology education versus aquatic exercise alone for patients with chronic low back pain: A randomized controlled trial. Clin. Rehabil. 2014, 29, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Andias, R.; Neto, M.; Silva, A.G. The effects of pain neuroscience education and exercise on pain, muscle endurance, catastrophizing and anxiety in adolescents with chronic idiopathic neck pain: A school-based pilot, randomized and controlled study. Physiother. Theory Pract. 2018, 34, 682–691. [Google Scholar] [CrossRef]
- Clarke, C.L.; Ryan, C.G.; Martin, D.J. Pain neurophysiology education for the management of individuals with chronic low back pain: A systematic review and meta-analysis. Man. Ther. 2011, 16, 544–549. [Google Scholar] [CrossRef]
- Louw, A.; Butler, D.S.; Diener, I.; Puentedura, E.J. Development of a Preoperative Neuroscience Educational Program for Patients with Lumbar Radiculopathy. Am. J. Phys. Med. Rehabil. 2013, 92, 446–452. [Google Scholar] [CrossRef] [Green Version]
- Malfliet, A.; Kregel, J.; Meeus, M.; Roussel, N.; Danneels, L.; Cagnie, B.; Dolphens, M.; Nijs, J. Blended-Learning Pain Neuroscience Education for People With Chronic Spinal Pain: Randomized Controlled Multicenter Trial. Phys. Ther. 2017, 98, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef]
- Louw, A.; Puentedura, E.J.; Zimney, K.; Schmidt, S. Know Pain, Know Gain? A Perspective on Pain Neuroscience Education in Physical Therapy. J. Orthop. Sports Phys. Ther. 2016, 46, 131–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bovim, G.; Schrader, H.; Sand, T. Neck Pain in the General Population. Spine 1994, 19, 1307–1309. [Google Scholar] [CrossRef]
- Galán-Martín, M.A.; Montero-Cuadrado, F.; Lluch-Girbes, E.; Coca-López, M.C.; Mayo-Iscar, A.; Cuesta-Vargas, A. Pain neuroscience education and physical exercise for patients with chronic spinal pain in primary healthcare: A randomised trial protocol. BMC Musculoskelet. Disord. 2019, 20, 505. [Google Scholar] [CrossRef]
- Goolkasian, P.; Wheeler, A.H.; Gretz, S.S. The Neck Pain and Disability Scale: Test–Retest Reliability and Construct Validity. Clin. J. Pain 2002, 18, 245–250. [Google Scholar] [CrossRef]
- Mousavi, S.J.; Parnianpour, M.; Montazeri, A.; Mehdian, H.; Karimi, A.; Abedi, M.; Ashtiani, A.A.; Mobini, B.; Hadian, M.R. Translation and Validation Study of the Iranian Versions of the Neck Disability Index and the Neck Pain and Disability Scale. Spine 2007, 32, E825–E831. [Google Scholar] [CrossRef] [PubMed]
- Young, B.A.; Walker, M.J.; Strunce, J.B.; Boyles, R.E.; Whitman, J.M.; Childs, J.D. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J. 2009, 9, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Jorritsma, W.; Dijkstra, P.U.; De Vries, G.E.; Geertzen, J.H.B.; Reneman, M.F. Detecting relevant changes and responsiveness of Neck Pain and Disability Scale and Neck Disability Index. Eur. Spine J. 2012, 21, 2550–2557. [Google Scholar] [CrossRef] [Green Version]
- Waddell, G.; Newton, M.; Henderson, I.; Somerville, D.; Main, C.J. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993, 52, 157–168. [Google Scholar] [CrossRef]
- Askary-Ashtiani, A.; Ebrahimi-Takamjani, I.; Torkaman, G.; Amiri, M.; Mousavi, S.J. Reliability and Validity of the Persian Versions of the Fear Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in Patients With Neck Pain. Spine 2014, 39, E1095–E1102. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Rahmati, N.; Moghadam, M.A.A.; Shairi, M.; Paknejad, M.; Rahmati, Z.; Ghassami, M.; Marofi, N.; Aghaei, H.N. A Study of the Psychometric Properties of the Pain Catastrophizing Scale Amongst Iranian Patients with Chronic Persistent Pain. J. Ilam Univ. Med Sci. 2017, 25, 63–79. [Google Scholar] [CrossRef] [Green Version]
- Jackson, T.; Wang, Y.; Wang, Y.; Fan, H. Self-Efficacy and Chronic Pain Outcomes: A Meta-Analytic Review. J. Pain 2014, 15, 800–814. [Google Scholar] [CrossRef] [PubMed]
- Asghari, A.; Nicholas, M.K. An Investigation of Pain Self-Efficacy Beliefs in Iranian Chronic Pain Patients: A Preliminary Validation of a Translated English-Language Scale. Pain Med. 2009, 10, 619–632. [Google Scholar] [CrossRef] [Green Version]
- Javdaneh, N.; Letafatkar, A.; Shojaedin, S.S.; Hadadnezhad, M. Scapular exercise combined with cognitive functional therapy is more effective at reducing chronic neck pain and kinesiophobia than scapular exercise alone: A randomized controlled trial. Clin. Rehabil. 2020, 34, 1485–1496. [Google Scholar] [CrossRef]
- Javdaneh, N.; Molayei, F.; Kamranifraz, N. Effect of adding motor imagery training to neck stabilization exercises on pain, disability and kinesiophobia in patients with chronic neck pain. Complement. Ther. Clin. Pract. 2021, 42, 101263. [Google Scholar] [CrossRef] [PubMed]
- Medicine ACoS. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013.
- Nijs, J.; Meeus, M.; Cagnie, B.; Roussel, N.; Dolphens, M.; Van Oosterwijck, J.; Danneels, L. A Modern Neuroscience Approach to Chronic Spinal Pain: Combining Pain Neuroscience Education With Cognition-Targeted Motor Control Training. Phys. Ther. 2014, 94, 730–738. [Google Scholar] [CrossRef] [Green Version]
- Larsen, J.B.; Skou, S.T.; Arendt-Nielsen, L.; Simonsen, O.; Madeleine, P. Neuromuscular exercise and pain neuroscience education compared with pain neuroscience education alone in patients with chronic pain after primary total knee arthroplasty: Study protocol for the NEPNEP randomized controlled trial. Trials 2020, 21, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Malfliet, A.; Kregel, J.; Meeus, M.; Danneels, L.; Cagnie, B.; Roussel, N.; Nijs, J. Patients With Chronic Spinal Pain Benefit From Pain Neuroscience Education Regardless the Self-Reported Signs of Central Sensitization: Secondary Analysis of a Randomized Controlled Multicenter Trial. PM&R 2018, 10, 1330–1343. [Google Scholar] [CrossRef]
- Saracoglu, I.; Arik, M.I.; Afşar, E.; Gokpinar, H.H. The effectiveness of pain neuroscience education combined with manual therapy and home exercise for chronic low back pain: A single-blind randomized controlled trial. Physiother. Theory Pract. 2020, 2020, 1–11. [Google Scholar] [CrossRef]
- Marris, D.; Theophanous, K.; Cabezon, P.; Dunlap, Z.; Donaldson, M. The impact of combining pain education strategies with physical therapy interventions for patients with chronic pain: A systematic review and meta-analysis of randomized controlled trials. Physiother. Theory Pract. 2019, 2019, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Kan, S.; Fujino, Y.; Shibata, M. Verbal Instruction Can Induce Extinction of Fear of Movement-Related Pain. J. Pain 2018, 19, 1063–1073. [Google Scholar] [CrossRef] [PubMed]
- Pardo, G.B.; Girbés, E.L.; Roussel, N.; Izquierdo, T.G.; Penick, V.J.; Pecos-Martin, D. Pain Neurophysiology Education and Therapeutic Exercise for Patients With Chronic Low Back Pain: A Single-Blind Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2018, 99, 338–347. [Google Scholar] [CrossRef]
- Galan-Martin, M.A.; Montero-Cuadrado, F.; Lluch-Girbes, E.; Coca-López, M.C.; Mayo-Iscar, A.; Cuesta-Vargas, A. Pain Neuroscience Education and Physical Exercise therapy for Patients with Chronic Spinal Pain in Spanish Physiotherapy Primary Care: A Pragmatic Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1201. [Google Scholar] [CrossRef]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1140.e1–1140.e22. [Google Scholar] [CrossRef] [PubMed]
- Doménech, J.; Sanchis-Alfonso, V.; Espejo, B. Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surgery, Sports Traumatol. Arthroscopy 2014, 22, 2295–2300. [Google Scholar] [CrossRef] [Green Version]
- Thompson, D.; Oldham, J.; Woby, S. Does adding cognitive-behavioural physiotherapy to exercise improve outcome in patients with chronic neck pain? A randomised controlled trial. Physiotherapy 2016, 102, 170–177. [Google Scholar] [CrossRef]
- Butler, D.S.; Moseley, G.L. Explain Pain, 2nd ed.; Noigroup Publications: Adelaide, SA, Australia, 2013. [Google Scholar]
- Moseley, G.L.; Nicholas, M.K.; Hodges, P.W. A Randomized Controlled Trial of Intensive Neurophysiology Education in Chronic Low Back Pain. Clin. J. Pain 2004, 20, 324–330. [Google Scholar] [CrossRef]
| Exercise | Dosage | Description |
|---|---|---|
| Craniocervical flexion exercise | 5–10 reps × 5–10 s | The patients were requested to do a slow and controlled craniocervical flexion task in the supine status. The patient concentrated on feeling the back of the head slide in the cephalad and caudal directions of the supporting surface. The exercises started with five repetitions in each set. Then, in the following sessions, two repeats were added to the repetitions of the previous session. |
| cervical isometric exercises | 5–10 reps × 5–15 s | Isometric neck exercises were performed straight back and forth, to the right and left, with elastic resistance bands. The patients exert force in the opposite direction of the applied resistance. Initially, the exercise started with five repetitions and a maintaining time of five seconds each, and then the number of repetitions and the time gradually increased. |
| Scapular upward rotation | 10–15 reps × 3 sets | The subjects stood with their back against a wall (wall contact from head to buttock) and with the feet shoulder-width apart. In the starting position, the shoulders were abducted 90 °, with the elbows flexed 90 °. The patients were instructed to slide their arms up the wall. The sliding movement ended when the shoulders reached 180 ° of abduction. The subjects were then instructed to maintain the arm position for three seconds. For the first two weeks, they performed only un-resisted exercises. After the first two weeks, exercise was performed with elastic rubber bands. The resistive elastic band was selected from four color-coded resistance levels (yellow, red, green, and blue; The Hygienic Corp, Akron, Ohio), and a gradual overload was applied based on the band’s color. |
| Backward rocking arm lift | 10–15 reps × 3 sets | Initially, the subjects were placed in the quadruped position and instructed to rock backward slowly, until the buttocks touched both heels. The subject was then instructed to lift the arms. For the first two weeks, only un-resisted exercises were performed. After the first two weeks, exercise was performed with dumbbells. Exercises using dumbbells gradually progressed with increasing loads during the intervention period from an initial load of 20% of a 1-repetition maximum and then increased 10% each week. |
| L to Y | 10–15 reps × 3 sets | This exercise was performed on a Swiss ball. The arms were abducted to 90 ° and externally rotated. The elbows were flexed to 90 °, with retracted scapula. The arms were elevated above the head, and the elbows were fully extended so that the arms formed the letter Y. The gradual overload program was performed like the above exercise (backward rocking arm lift). |
| Variables | Groups (No.) | ||||
|---|---|---|---|---|---|
| Ther Ex (n = 24) | Combined (n = 24) | Control (n = 24) | p-Value | ||
| Age (year), mean ± SD | 31.18 ± 6.37 | 33.45 ± 7.08 | 33.70 ± 8.13 | 0.76 | |
| Weight (kg), mean ± SD | 80.15 ± 5.10 | 80.50 ± 4.00 | 78.23 ± 6.05 | 0.72 | |
| Height (cm), mean ± SD | 175 ± 6.15 | 174 ± 6.50 | 177 ± 7.68 | 0.81 | |
| BMI (kg/m2), mean ± SD | 25.05 ± 1.22 | 25.93 ± 1.45 | 24.16 ± 1.05 | 0.79 | |
| Duration of pain (year), mean ± SD | 3.45 ± 0.84 | 3.12 ± 0.85 | 3.76 ± 1.17 | 0.64 | |
| Gender, n (%) | Female | 10 (41.66%) | 13(54.16%) | 12 (50%) | 0.47 |
| Male | 14 (58.33%) | 11(45.83%) | 12(50%) | ||
| Variables | Group | Pre-Training a | Post-Training a | Between-Groups Difference (BONFERRONI Post Hoc Test) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Ther Ex vs. Combined | Ther Ex vs. Control | Combined vs. Control | |||||||
| Mean Difference (95% CI) | ES (p-Value) | Mean difference (95% CI) | ES (p-Value) | Mean Difference (95% CI) | ES (p-Value) | ||||
| NPAD (0–100) | Ther Ex | 52.55 ± 3.60 | 35.50 ± 3.80 | 5.84 (3.09,8.67) | 2.30 (0.001 *) | −10.24 (−13.15,−7.34) | 3.28 (0.001 *) | −16.09 (−18.98,−13.24) | 5.91 (0.001 *) |
| Combined | 52.86 ± 4.40 | 23.50 ± 4.83 | |||||||
| Control | 54.63 ± 4.88 | 53.90 ± 4.09 | |||||||
| PCS (0–52) | Ther Ex | 21.50 ± 2.76 | 15.25 ± 2.55 | 2.07 (0.06,4.09) | 1.85 (0.041 *) | −3.28 (−5.25,−1.22) | 2.20 (0.001 *) | −5.31 (−7.38,−3.35) | 4.17 (0.001) * |
| Combined | 21.81 ± 2.90 | 10.77 ± 2.89 | |||||||
| Control | 22.63 ± 2.61 | 20.59 ± 3.76 | |||||||
| FAB (0–96) | Ther Ex | 48.15 ± 3.80 | 37.20 ± 4.86 | 2.92 (0.06,5.78) | 2.94 (0.044 *) | −5.89 (−8.75,−3.02) | 2.73 (0.001 *) | −8.81 (−11.61,−6.06) | 5.83 (0.001 *) |
| Combined | 50.40 ± 3.45 | 29.09 ± 3.17 | |||||||
| Control | 49.00 ± 4.15 | 48.13 ± 3.89 | |||||||
| PSE (0–60) | Ther Ex | 25.33 ± 5.84 | 40.66 ± 5.83 | −0.68 (−4.77,3.41) | 0.41 (0.99) | 8.08 (4.07,12.04) | 2.50 (0.001 *) | 8.76 (4.80,12.72) | 3.52 (0.001 *) |
| Combined | 23.22 ± 3.84 | 44.13 ± 5.60 | |||||||
| Control | 24.62 ± 6.25 | 25.20 ± 5.65 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Javdaneh, N.; Saeterbakken, A.H.; Shams, A.; Barati, A.H. Pain Neuroscience Education Combined with Therapeutic Exercises Provides Added Benefit in the Treatment of Chronic Neck Pain. Int. J. Environ. Res. Public Health 2021, 18, 8848. https://doi.org/10.3390/ijerph18168848
Javdaneh N, Saeterbakken AH, Shams A, Barati AH. Pain Neuroscience Education Combined with Therapeutic Exercises Provides Added Benefit in the Treatment of Chronic Neck Pain. International Journal of Environmental Research and Public Health. 2021; 18(16):8848. https://doi.org/10.3390/ijerph18168848
Chicago/Turabian StyleJavdaneh, Norollah, Atle Hole Saeterbakken, Arash Shams, and Amir Hossein Barati. 2021. "Pain Neuroscience Education Combined with Therapeutic Exercises Provides Added Benefit in the Treatment of Chronic Neck Pain" International Journal of Environmental Research and Public Health 18, no. 16: 8848. https://doi.org/10.3390/ijerph18168848
APA StyleJavdaneh, N., Saeterbakken, A. H., Shams, A., & Barati, A. H. (2021). Pain Neuroscience Education Combined with Therapeutic Exercises Provides Added Benefit in the Treatment of Chronic Neck Pain. International Journal of Environmental Research and Public Health, 18(16), 8848. https://doi.org/10.3390/ijerph18168848








