The Comparative Efficacy of Treatments for Children and Young Adults with Internet Addiction/Internet Gaming Disorder: An Updated Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search and Study Selection
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.3.1. Types of Treatment
2.3.2. Types of Symptom Measurement Scales
2.3.3. Type of Comorbid Diagnosis
2.3.4. Types of Study Design
3. Statistical Analysis
4. Additional Analysis
5. Results
5.1. Univariate Meta-Regression Analysis
5.2. Multiple Meta-Regression Analysis
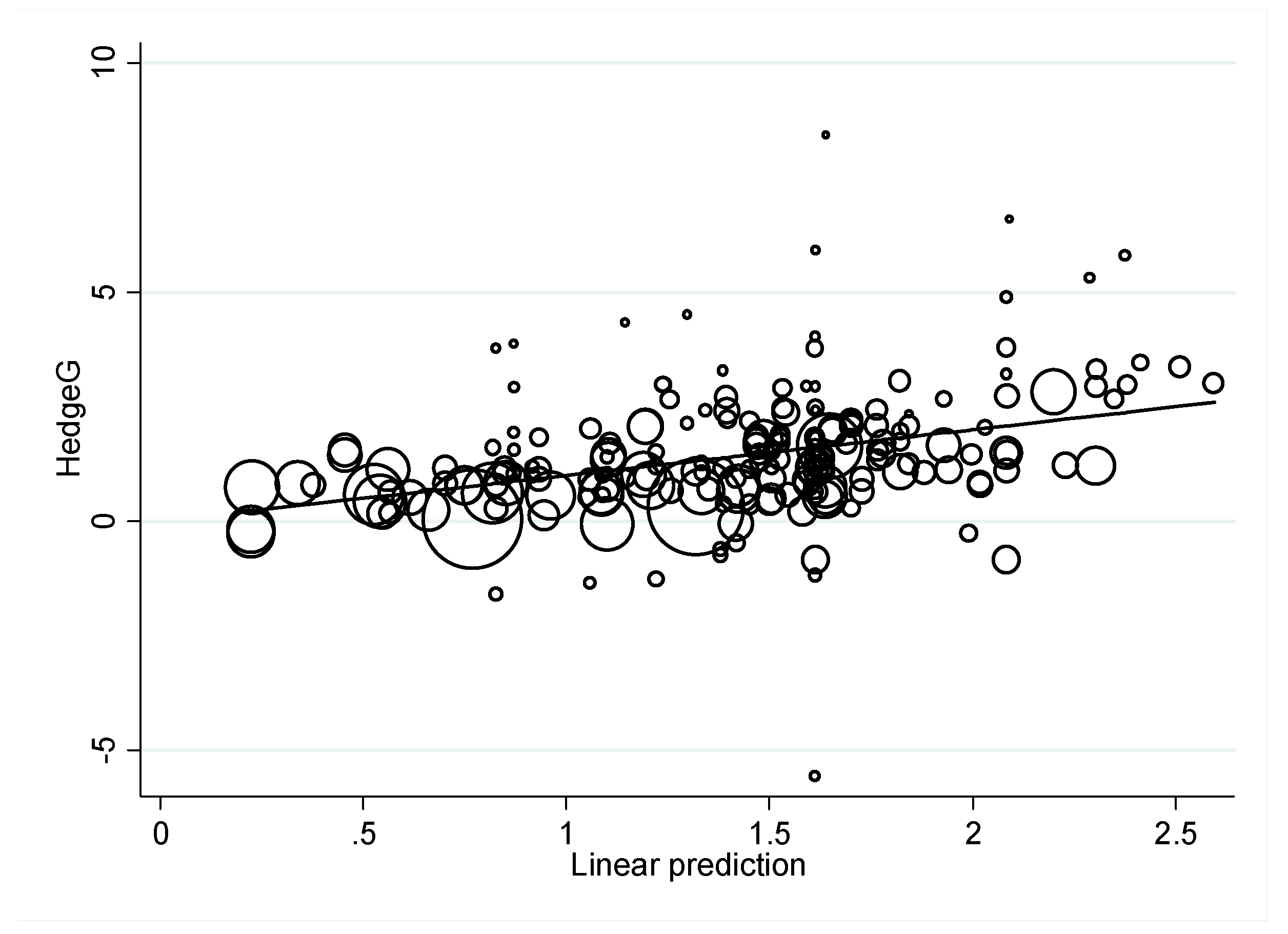
5.3. Checking for Publication Bias
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, S.; Zhuang, Y.; Lee, P.; Li, J.C.; Wong, P.W.C. Leisure and Problem Gaming Behaviors Among Children and Adolescents During School Closures Caused by COVID-19 in Hong Kong: Quantitative Cross-sectional Survey Study. JMIR Serious Games 2021, 9, e26808. [Google Scholar] [CrossRef] [PubMed]
- Shahid, R.; Kumari, S.; Doumas, S. COVID-19’s impact on internet gaming disorder among children and adolescents. Curr. Psychiatry 2021, 20, 41–42. [Google Scholar] [CrossRef]
- Higuchi, S.; Mihara, S.; Kitayuguchi, T.; Miyakoshi, H.; Ooi, M.; Maezono, M.; Nishimura, K.; Matsuzaki, T. Prolonged use of Internet and gaming among treatment seekers arising out of social restrictions related to COVID-19 pandemic. Psychiatry Clin. Neurosci. 2020, 74, 607–608. [Google Scholar] [CrossRef] [PubMed]
- Hawes, M.T.; Szenczy, A.K.; Klein, D.N.; Hajcak, G.; Nelson, B.D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2021, in press. [CrossRef]
- Gjoneska, B.; Potenza, M.N.; Jones, J.; Corazza, O.; Hall, N.; Sales, C.M.D.; Grunblatt, E.; Martinotti, G.; Burkauskas, J.; Werling, A.M.; et al. Problematic use of the internet during the COVID-19 pandemic: Good practices and mental health recommendations. Compr. Psychiatry 2021, 112, 152279. [Google Scholar] [CrossRef]
- Chamberlain, S.R.; Lochner, C.; Stein, D.J.; Goudriaan, A.E.; van Holst, R.J.; Zohar, J.; Grant, J.E. Behavioural addiction-A rising tide? Eur. Neuropsychopharmacol. 2016, 26, 841–855. [Google Scholar] [CrossRef] [Green Version]
- Weinstein, A.; Lejoyeux, M. Internet addiction or excessive internet use. Am. J. Drug Alcohol Abus. 2010, 36, 277–283. [Google Scholar] [CrossRef] [Green Version]
- Kilic, M.; Avci, D.; Uzuncakmak, T. Internet Addiction in High School Students in Turkey and Multivariate Analyses of the Underlying Factors. J. Addict. Nurs. 2016, 27, 39–46. [Google Scholar] [CrossRef]
- Floros, G.; Paradisioti, A.; Hadjimarcou, M.; Mappouras, D.G.; Karkanioti, O.; Siomos, K. Adolescent online gambling in Cyprus: Associated school performance and psychopathology. J. Gambl. Stud. 2015, 31, 367–384. [Google Scholar] [CrossRef]
- Gentile, D. Pathological video-game use among youth ages 8 to 18: A national study. Psychol. Sci. 2009, 20, 594–602. [Google Scholar] [CrossRef]
- Calado, F.; Alexandre, J.; Griffiths, M.D. Prevalence of Adolescent Problem Gambling: A Systematic Review of Recent Research. J. Gambl. Stud. 2017, 33, 397–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Kim, M.S.; Park, B.; Kim, J.H.; Choi, H.G. Lack of sleep is associated with internet use for leisure. PLoS ONE 2018, 13, e0191713. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.A.; King, D.L.; Delfabbro, P.H. Family factors in adolescent problematic Internet gaming: A systematic review. J. Behav. Addict. 2017, 6, 321–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.Y.; Park, E.C.; Han, K.T.; Kim, S.J.; Chun, S.Y.; Park, S. The Association of Level of Internet Use with Suicidal Ideation and Suicide Attempts in South Korean Adolescents: A Focus on Family Structure and Household Economic Status. Can. J. Psychiatry 2016, 61, 243–251. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, J.; Amiri, A.; Ghanizadeh, A.; Khademalhosseini, M.; Khademalhosseini, Z.; Gholami, Z.; Sharifian, M. Prevalence of Addiction to the Internet, Computer Games, DVD, and Video and Its Relationship to Anxiety and Depression in a Sample of Iranian High School Students. Iran. J. Psychiatry Behav. Sci. 2014, 8, 75–80. [Google Scholar]
- De Pasquale, C.; Dinaro, C.; Sciacca, F. Relationship of Internet gaming disorder with dissociative experience in Italian university students. Ann. Gen. Psychiatry 2018, 17, 28. [Google Scholar] [CrossRef]
- Ma, H.K. Internet addiction and antisocial internet behavior of adolescents. Sci. World J. 2011, 11, 2187–2196. [Google Scholar] [CrossRef] [Green Version]
- Yamada, T.; Moshier, S.J.; Otto, M.W. No site unseen: Predicting the failure to control problematic Internet use among young adults. Cogn. Behav. Ther. 2016, 45, 496–500. [Google Scholar] [CrossRef]
- Winkler, A.; Dorsing, B.; Rief, W.; Shen, Y.; Glombiewski, J.A. Treatment of internet addiction: A meta-analysis. Clin. Psychol. Rev. 2013, 33, 317–329. [Google Scholar] [CrossRef]
- Wang, B.Q.; Yao, N.Q.; Zhou, X.; Liu, J.; Lv, Z.T. The association between attention deficit/hyperactivity disorder and internet addiction: A systematic review and meta-analysis. BMC Psychiatry 2017, 17, 260. [Google Scholar] [CrossRef] [Green Version]
- Nam, B.; Bae, S.; Kim, S.M.; Hong, J.S.; Han, D.H. Comparing the Effects of Bupropion and Escitalopram on Excessive Internet Game Play in Patients with Major Depressive Disorder. Clin. Psychopharmacol. Neurosci. 2017, 15, 361–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.H.; Lee, Y.S.; Sohn, J.H.; Han, D.H. Effectiveness of atomoxetine and methylphenidate for problematic online gaming in adolescents with attention deficit hyperactivity disorder. Hum. Psychopharmacol. 2016, 31, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Seo, Y.; Hwang, H.; Kim, S.M.; Han, D.H. Efficacy of cognitive behavioural therapy for internet gaming disorder. Clin. Psychol. Psychother. 2020, 27, 203–213. [Google Scholar] [CrossRef]
- King, D.L.; Delfabbro, P.H.; Wu, A.M.S.; Doh, Y.Y.; Kuss, D.J.; Pallesen, S.; Mentzoni, R.; Carragher, N.; Sakuma, H. Treatment of Internet gaming disorder: An international systematic review and CONSORT evaluation. Clin. Psychol. Rev. 2017, 54, 123–133. [Google Scholar] [CrossRef] [Green Version]
- Zajac, K.; Ginley, M.K.; Chang, R.; Petry, N.M. Treatments for Internet gaming disorder and Internet addiction: A systematic review. Psychol. Addict. Behav. 2017, 31, 979–994. [Google Scholar] [CrossRef] [PubMed]
- Chambless, D.L.; Hollon, S.D. Defining empirically supported therapies. J. Consult. Clin. Psychol. 1998, 66, 7–18. [Google Scholar] [CrossRef]
- Furukawa, T.A.; Cipriani, A.; Barbui, C.; Brambilla, P.; Watanabe, N. Imputing response rates from means and standard deviations in meta-analyses. Int. Clin. Psychopharmacol. 2005, 20, 49–52. [Google Scholar] [CrossRef] [Green Version]
- Young, K.S. Caught in the Net: How to Recognize the Signs of Internet Addiction and a Winning Strategy for Recovery; John Wiley & Sons: Hoboken, NJ, USA, 1998. [Google Scholar]
- Meerkerk, G.J.; Van Den Eijnden, R.J.; Vermulst, A.A.; Garretsen, H.F. The Compulsive Internet Use Scale (CIUS): Some psychometric properties. Cyberpsychol. Behav. 2009, 12, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Demetrovics, Z.; Szeredi, B.; Rozsa, S. The three-factor model of Internet addiction: The development of the Problematic Internet Use Questionnaire. Behav. Res. Methods 2008, 40, 563–574. [Google Scholar] [CrossRef] [Green Version]
- Laconi, S.; Rodgers, R.F.; Chabrol, H. The measurement of Internet addiction: A critical review of existing scales and their psychometric properties. Comput. Hum. Behav. 2014, 41, 190–202. [Google Scholar] [CrossRef]
- Bangdiwala, S.I.; Bhargava, A.; O’Connor, D.P.; Robinson, T.N.; Michie, S.; Murray, D.M.; Stevens, J.; Belle, S.H.; Templin, T.N.; Pratt, C.A. Statistical methodologies to pool across multiple intervention studies. Transl. Behav. Med. 2016, 6, 228–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, R.; Ware, J.H. Detecting moderator effects using subgroup analyses. Prev. Sci. Off. J. Soc. Prev. Res. 2013, 14, 111–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baker, W.L.; White, C.M.; Cappelleri, J.C.; Kluger, J.; Coleman, C.I.; Health Outcomes, Policy, and Economics (HOPE) Collaborative Group. Understanding heterogeneity in meta-analysis: The role of meta-regression. Int. J. Clin. Pract. 2009, 63, 1426–1434. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Lopez-Fernandez, O. Internet addiction and problematic Internet use: A systematic review of clinical research. World J. Psychiatry 2016, 6, 143–176. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef]
- Kuss, D.J.; Griffiths, M.D. Internet and gaming addiction: A systematic literature review of neuroimaging studies. Brain Sci. 2012, 2, 347–374. [Google Scholar] [CrossRef]
- Sepede, G.; Tavino, M.; Santacroce, R.; Fiori, F.; Salerno, R.M.; Di Giannantonio, M. Functional magnetic resonance imaging of internet addiction in young adults. World J. Radiol. 2016, 8, 210–225. [Google Scholar] [CrossRef] [Green Version]
- Rumpf, H.J.; Achab, S.; Billieux, J.; Bowden-Jones, H.; Carragher, N.; Demetrovics, Z.; Higuchi, S.; King, D.L.; Mann, K.; Potenza, M.; et al. Including gaming disorder in the ICD-11: The need to do so from a clinical and public health perspective. J. Behav. Addict. 2018, 7, 556–561. [Google Scholar] [CrossRef]
- Koo, C.; Wati, Y.; Lee, C.C.; Oh, H.Y. Internet-addicted kids and South Korean government efforts: Boot-camp case. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 391–394. [Google Scholar] [CrossRef]
- Throuvala, M.A.; Griffiths, M.D.; Rennoldson, M.; Kuss, D.J. School-based Prevention for Adolescent Internet Addiction: Prevention is the Key. A Systematic Literature Review. Curr. Neuropharmacol. 2019, 17, 507–525. [Google Scholar] [CrossRef]
- Thair, H.; Holloway, A.L.; Newport, R.; Smith, A.D. Transcranial Direct Current Stimulation (tDCS): A Beginner’s Guide for Design and Implementation. Front. Neurosci. 2017, 11, 641. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Paper | Year | Country | No. of Studies | Age | Measurements | No. of Patients | Treatment Sections | Type of Subjects | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Cao FL et al. | 2007 | China | 1 | 14.8 | YDQ, CIAS | 57 | 8 | IA | CBT vs. Control |
| Li G & Dai XY | 2009 | China | 1 | 16.5 | CIAS | 76 | 12 | IA | CBT vs. Control |
| Shao Z et al. | 2015 | China | 1 | 16 | SDS, SCL-90 | 66 | 8 | IA + Depression | CBT + Drug vs. CBT |
| Wei QX | 2008 | China | 1 | 17 | SAS, SDS | 60 | 12 | IA | Others (Psychology Nursing) vs. Control |
| Yang FR et al. | 2005 | China | 1 | 15.2 | IAD-DQ, SCL-90, Time | 52 | 12 | IA | SFBT (No control) |
| Liao XC | 2010 | China | 1 | 15 | IAD-DQ, SCL-90 | 284 | 32 | IA + Depression | CBT + Drug vs. CBT |
| Wu LZ et al. | 2007 | China | 1 | 19.5 | Time | 27 | 6 | IA | Others (HANS) vs. Control |
| Pan SJ et al. | 2010 | China | 1 | 17 | CIAS, SCL-90, SDS | 11 | 16 | IA | Others (EEG Biofeedback) (No control) |
| Liao YR et al. | 2012 | Taiwan | 1 | 14 | CIAS-R, Time | 18 | 8 | IA | Others (Adlerian Group Counseling) vs. Control |
| Li & Dai | 2009 | China | 1 | 16.5 | CIAS | 76 | 9 | IA | CBT vs. Control |
| Bai & Fan | 2007 | China | 1 | 19 | CIAS | 48 | 8 | IA | MLC vs. Control |
| Du YS et al. | 2010 | China | 1 | 15.9 | IOSRS | 56 | 8 | IA | CBT vs. Control |
| Han DH et al. | 2009 | Korea | 1 | 9.3 | YIAS-K, Time | 62 | 8 | IA + ADHD | Drug (Methylphenidate) (No control) |
| Yang R et al. | 2005 | China | 1 | 16 | CIUS, SDS, SCL-90 | 18 | 8 | IA | MLC + Drug (Fluoxetine) + Others (No control) |
| Zhu TM et al. | 2009 | China | 1 | 22.2 | ISS, SAS, SDS, HAMA, HAMD | 45 | 20, 10 | IA | CBT+ acupuncture vs. CBT |
| Yeun YR et al. | 2016 | Korea | 33 | 8~12 | K-scale, YIAS, IGAS | 1330 | 6~22 | IA | CBT, MLC, CBT/MLC + Others, Others |
| Liu J et al. | 2017 | China, Korea | 49 | 15.5~20 | IA | 2304 | IA | CBT, MLC, Others | |
| Winkler et al. | 2013 | China, Korea, US | 16 | 14.8~23 | Anx., Dep., IA, Time | 454 | IA | Drug, CBT, MLC, Others | |
| Liu QX et al. | 2015 | China | 1 | 15.7 | APIUS, Time | 46 | 6 | IA | MLC vs. Control |
| Yang Y et al. | 2017 | China | 1 | 21.1, 21.7 | YIAS | 32 | 10, 20 | IA | CBT vs. Electro-acupuncture |
| Han DH et al. | 2012 | Korea | 1 | 20.2 | YIAS, BDI, Time | 50 | 8 | IA + Depression | Drug (Bupropion) |
| Park JH et al. | 2016 | Korea | 1 | 17 | YIAS, CDI | 86 | 12 | IA + ADHD | Drug (Methylphenidate) vs. Drug (Atomoxetine) |
| Mun SY et al. | 2015 | Korea | 1 | 10.5 | IA, Time | 56 | 8 | IA | CBT vs. Control |
| Lien T.-C. | 2007 | Taiwan | 1 | 16.8 | YDQ | 20 | 8 | IA | MLC vs. Control |
| Huang Z et al. | 2010 | China | 1 | 21 | CGAI | 27 | 6 | IA | MLC vs. Control |
| Khazaei et al. | 2017 | Iran | 1 | 20 | YIAS | 48 | 10 | IA | CBT (Positive psychology Interventions) vs. Control |
| Hui Li et al. | 2017 | China | 1 | 22 | ISS, SCL-90 | 112 | 10 | IA | CBT + Others (EA) vs. CBT vs. Others (EA) |
| Kim SM et al. | 2012 | Korea | 1 | 16 | YIAS, BAI, BDI, Time | 65 | 8 | IA + Depression | CBT + Drug (Bupropion) vs. Drug (Bupropion) |
| Han DH et al. | 2012 | Korea | 1 | 14.2 | YIAS, Time | 15 | 12 | IA | MLC (No control) |
| SMD | Coefficients | SE | t | p | τ2 | I2-Residual | Adjusted-R2 | No. |
|---|---|---|---|---|---|---|---|---|
| Year | 0.025 | 0.027 | 0.93 | 0.354 | 1.415 | 93.00% | 0.05% | 207 |
| Mean Age | 0.062 | 0.025 | 2.51 | 0.013 | 1.36 | 92.52% | 3.99% | 207 |
| Treatments | 1.39 | 93.00% | 1.83% | 207 | ||||
| Treat 2 vs. Treat 1 | 0.613 | 0.320 | 1.92 | 0.056 | ||||
| Treat 3 vs. Treat 1 | 0.263 | 0.311 | 0.85 | 0.398 | ||||
| Treat 4 vs. Treat 1 | 0.834 | 0.427 | 1.96 | 0.052 | ||||
| Treat 5 vs. Treat 1 | 0.665 | 0.408 | 1.63 | 0.104 | ||||
| Treat 6 vs. Treat 1 | 0.269 | 0.377 | 0.71 | 0.477 | ||||
| Measurements | 1.39 | 91.89% | 1.80% | 207 | ||||
| Type 2 vs. Type 1 | 0.137 | 0.384 | 0.36 | 0.722 | ||||
| Type 3 vs. Type 1 | 0.533 | 0.309 | 1.73 | 0.086 | ||||
| Type 4 vs. Type 1 | 0.744 | 0.406 | 1.83 | 0.068 | ||||
| Type 5 vs. Type 1 | −0.107 | 0.531 | −0.20 | 0.841 | ||||
| Study Types | 1.432 | 92.87% | −1.13% | 207 | ||||
| StudType 2 vs StudType 1 | −0.077 | 0.265 | −0.29 | 0.772 | ||||
| StudType 3 vs StudType 1 | −0.298 | 0.310 | −0.96 | 0.338 | ||||
| StudType 4 vs StudType 1 | −0.211 | 0.267 | −0.79 | 0.429 | ||||
| Types of Subjects | 1.402 | 92.66% | 1.01% | 207 | ||||
| PType 2 vs. PType 1 | −0.487 | 0.356 | −1.37 | 0.172 | ||||
| PType 3 vs. PType 1 | −0.726 | 0.526 | −1.38 | 0.169 | ||||
| Group Therapy | 1.420 | 93.01% | −0.29% | 207 | ||||
| Yes vs. No | −0.126 | 0.188 | −0.67 | 0.503 | ||||
| Parents Involved in the Therapy program | 1.441 | 93.07% | −0.02% | 203 | ||||
| Yes vs. No | 0.188 | 0.221 | 0.85 | 0.396 | ||||
| SMD | Coefficients | SE | t | p | τ2 | I2-Residual | Adjusted-R2 | No. |
|---|---|---|---|---|---|---|---|---|
| 1.209 | 90.32% | 14.65% | 207 | |||||
| Mean Age | 0.087 | 0.025 | 3.53 | 0.001 | ||||
| Treatments | ||||||||
| Treat 2 vs. Treat 1 | 0.623 | 0.315 | 1.98 | 0.049 | ||||
| Treat 3 vs. Treat 1 | 0.152 | 0.309 | 0.49 | 0.624 | ||||
| Treat 4 vs. Treat 1 | 1.175 | 0.409 | 2.87 | 0.005 | ||||
| Treat 5 vs. Treat 1 | 0.829 | 0.399 | 2.08 | 0.039 | ||||
| Treat 6 vs. Treat 1 | 0.382 | 0.370 | 1.03 | 0.302 | ||||
| Measurements | ||||||||
| Type 2 vs. Type 1 | 0.232 | 0.369 | 0.63 | 0.531 | ||||
| Type 3 vs. Type 1 | 0.880 | 0.304 | 2.89 | 0.004 | ||||
| Type 4 vs. Type 1 | 1.171 | 0.398 | 2.94 | 0.004 | ||||
| Type 5 vs. Type 1 | −0.089 | 0.504 | −0.18 | 0.860 |
| SMD | Coefficients | SE | t | p | τ2 | I2-Residual | Adjusted-R2 | No. |
|---|---|---|---|---|---|---|---|---|
| 1.188 | 89.74% | 16.10% | 207 | |||||
| Mean Age | 0.125 | 0.037 | 3.33 | 0.001 | ||||
| Treatments | ||||||||
| Treat 2 vs. Treat 1 | 0.528 | 0.365 | 1.45 | 0.150 | ||||
| Treat 3 vs. Treat 1 | 0.092 | 0.374 | 0.25 | 0.805 | ||||
| Treat 4 vs. Treat 1 | 1.044 | 0.458 | 2.28 | 0.024 | ||||
| Treat 5 vs. Treat 1 | 0.505 | 0.462 | 1.09 | 0.276 | ||||
| Treat 6 vs. Treat 1 | 0.171 | 0.422 | 0.41 | 0.685 | ||||
| Measurements | ||||||||
| Type 2 vs. Type 1 | 0.283 | 0.370 | 0.76 | 0.446 | ||||
| Type 3 vs. Type 1 | 1.027 | 0.321 | 3.20 | 0.002 | ||||
| Type 4 vs. Type 1 | 1.125 | 0.409 | 2.75 | 0.006 | ||||
| Type 5 vs. Type 1 | −0.318 | 0.514 | −0.62 | 0.536 | ||||
| Year | −0.007 | 0.030 | −0.22 | 0.823 | ||||
| PType 2 vs. PType 1 | −0.681 | 0.383 | −1.78 | 0.077 | ||||
| PType 3 vs. PType 1 | −0.323 | 0.624 | −0.52 | 0.605 | ||||
| StudType 2 vs. StudType 1 | 0.115 | 0.301 | 0.38 | 0.702 | ||||
| StudType 3 vs. StudType 1 | 0.131 | 0.420 | 0.31 | 0.757 | ||||
| StudType 4 vs. StudType 1 | −0.553 | 0.280 | −1.97 | 0.050 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-H.; Chang, Y.-C.; Yang, L.; Tzang, R.-F. The Comparative Efficacy of Treatments for Children and Young Adults with Internet Addiction/Internet Gaming Disorder: An Updated Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2612. https://doi.org/10.3390/ijerph19052612
Chang C-H, Chang Y-C, Yang L, Tzang R-F. The Comparative Efficacy of Treatments for Children and Young Adults with Internet Addiction/Internet Gaming Disorder: An Updated Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(5):2612. https://doi.org/10.3390/ijerph19052612
Chicago/Turabian StyleChang, Chuan-Hsin, Yue-Cune Chang, Luke Yang, and Ruu-Fen Tzang. 2022. "The Comparative Efficacy of Treatments for Children and Young Adults with Internet Addiction/Internet Gaming Disorder: An Updated Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 5: 2612. https://doi.org/10.3390/ijerph19052612
APA StyleChang, C.-H., Chang, Y.-C., Yang, L., & Tzang, R.-F. (2022). The Comparative Efficacy of Treatments for Children and Young Adults with Internet Addiction/Internet Gaming Disorder: An Updated Meta-Analysis. International Journal of Environmental Research and Public Health, 19(5), 2612. https://doi.org/10.3390/ijerph19052612






