Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis
Abstract
:1. Introduction
2. Method
2.1. Design
2.2. Search Strategy and Database
2.3. Study Criteria
2.4. Study Selection, Data Extraction and Quality Assessment
2.5. Outcome Measure
2.6. Data Synthesis and Statistical Assessment
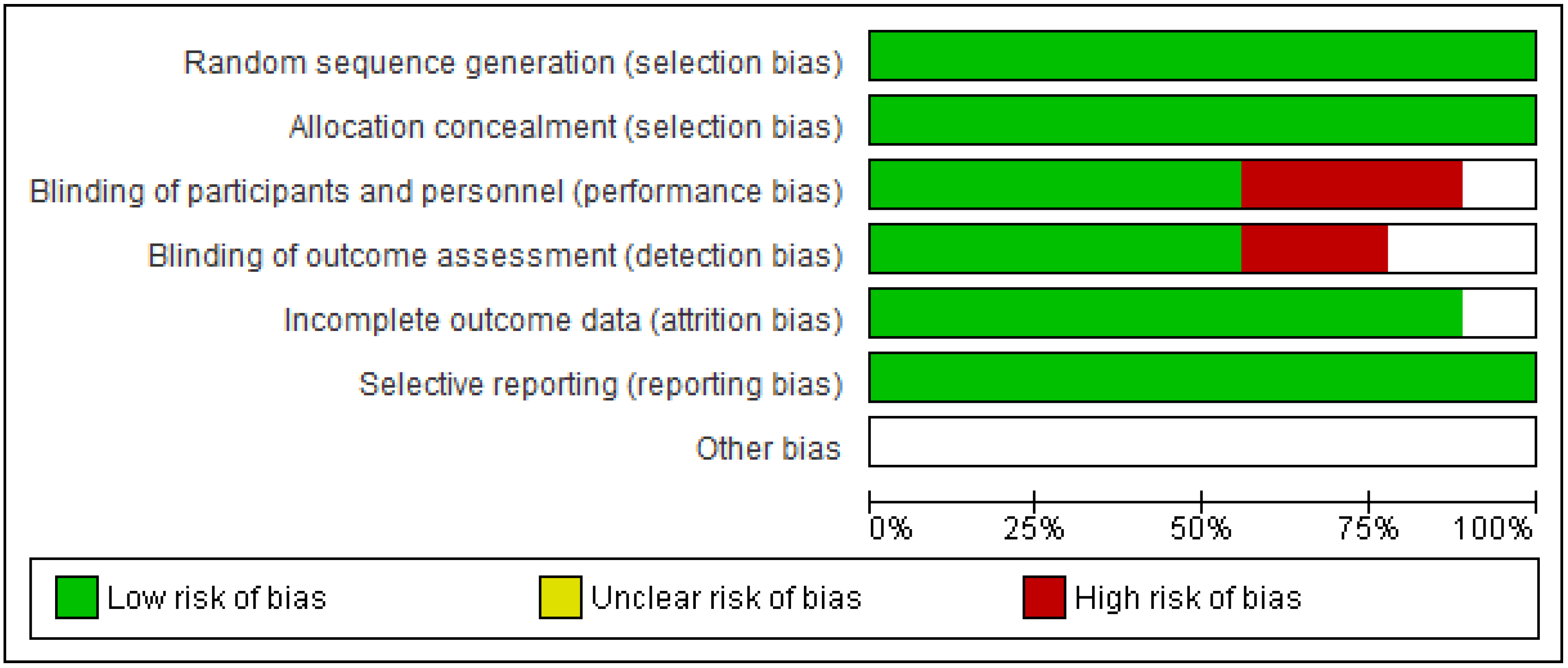
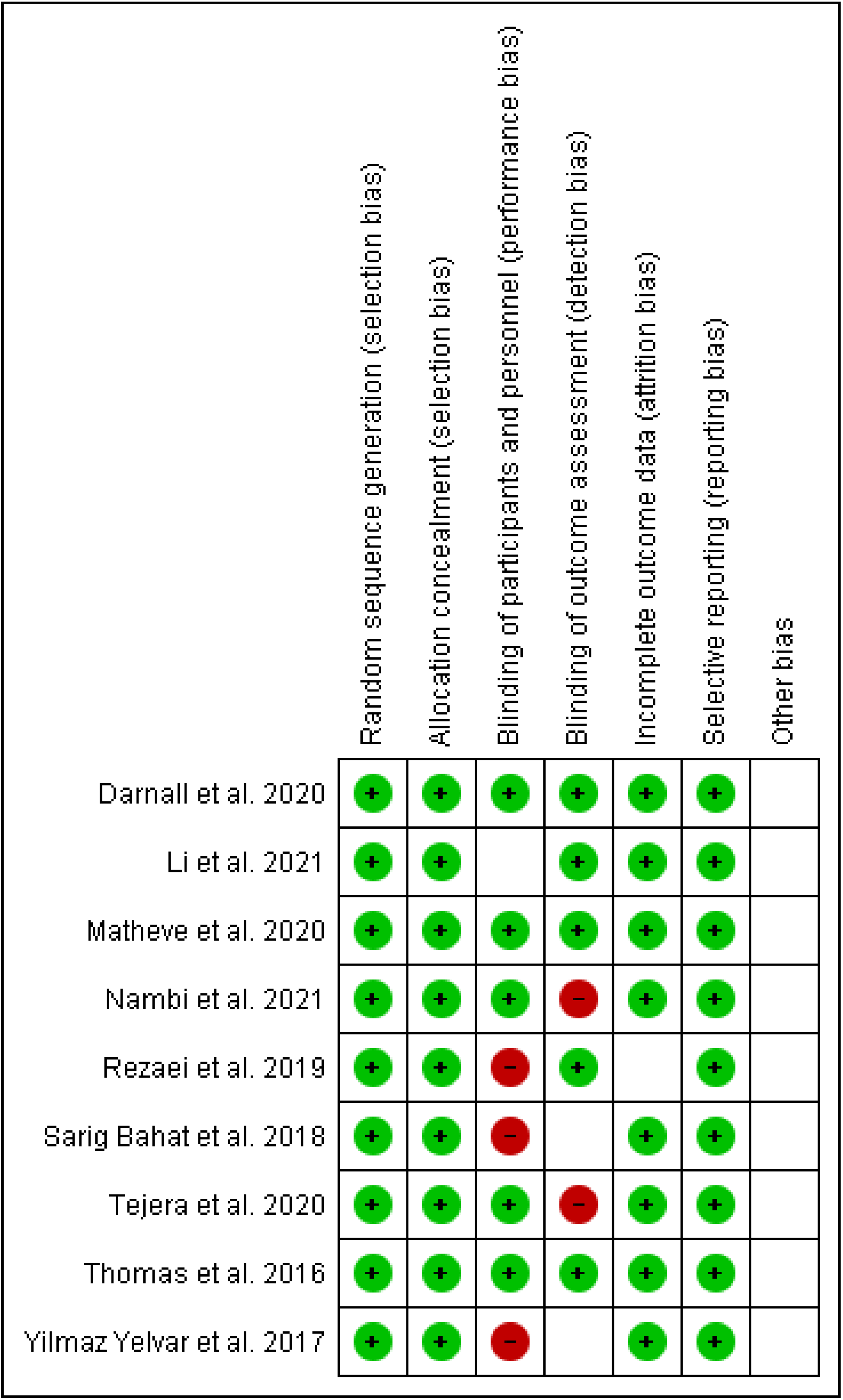
2.7. Risk of Bias (ROB) Assessment of Eligible Studies
3. Results
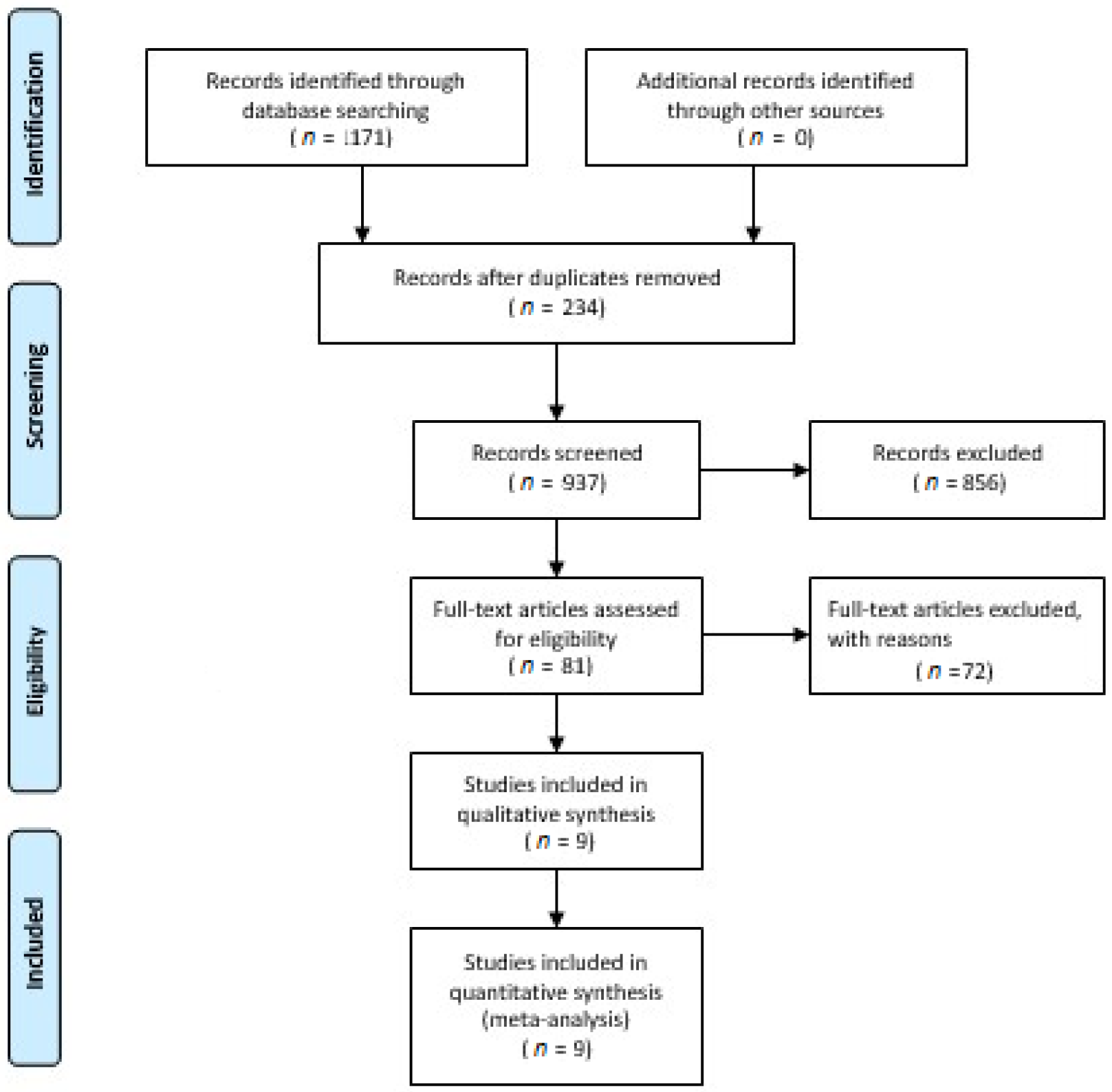
3.1. Literature Search and Characteristic of Study
3.2. Measure of Primary Outcomes
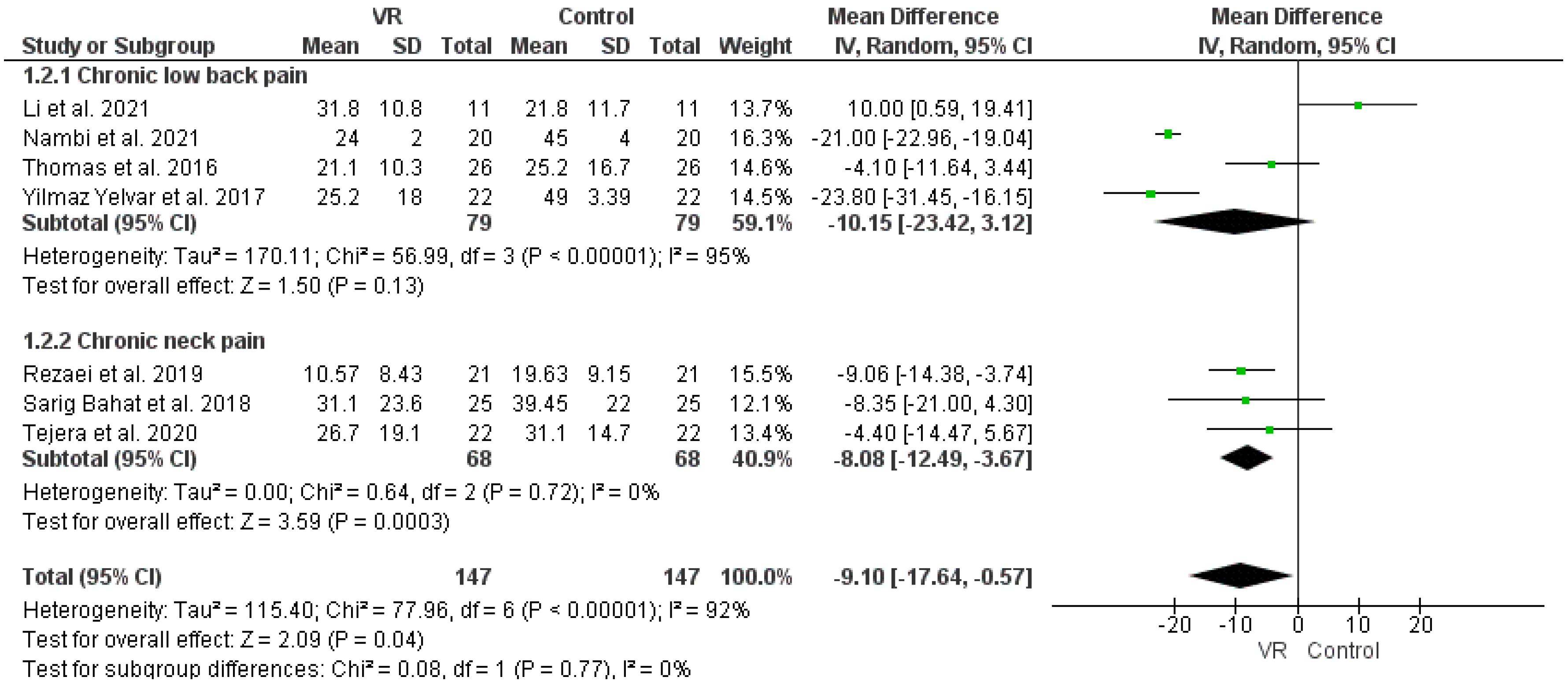
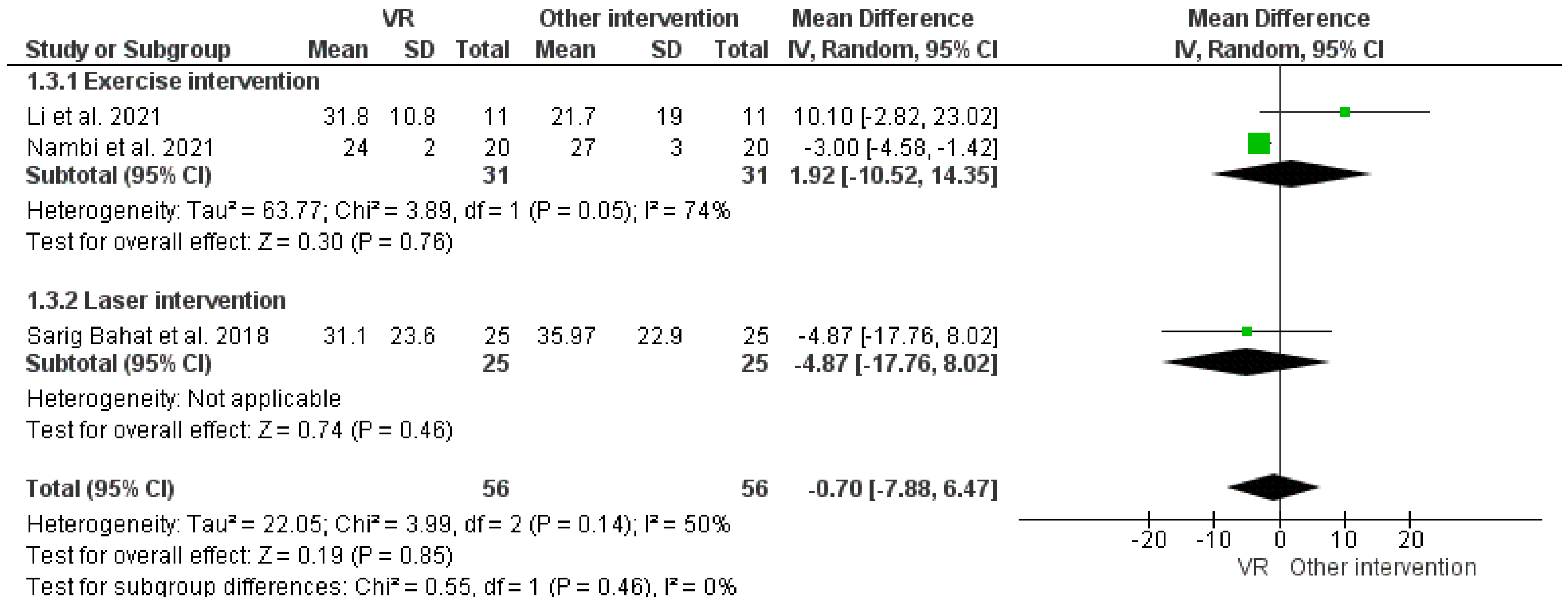
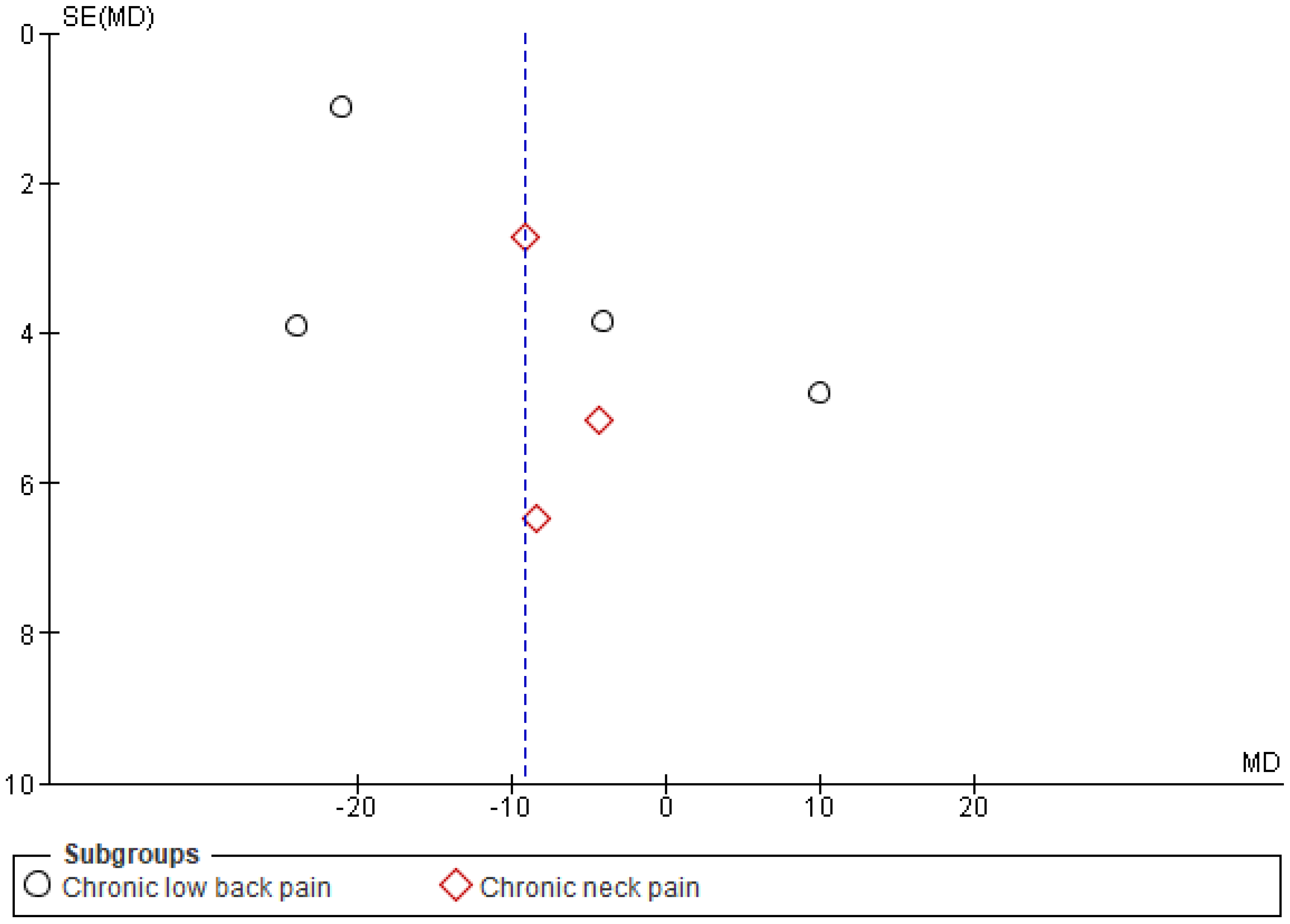
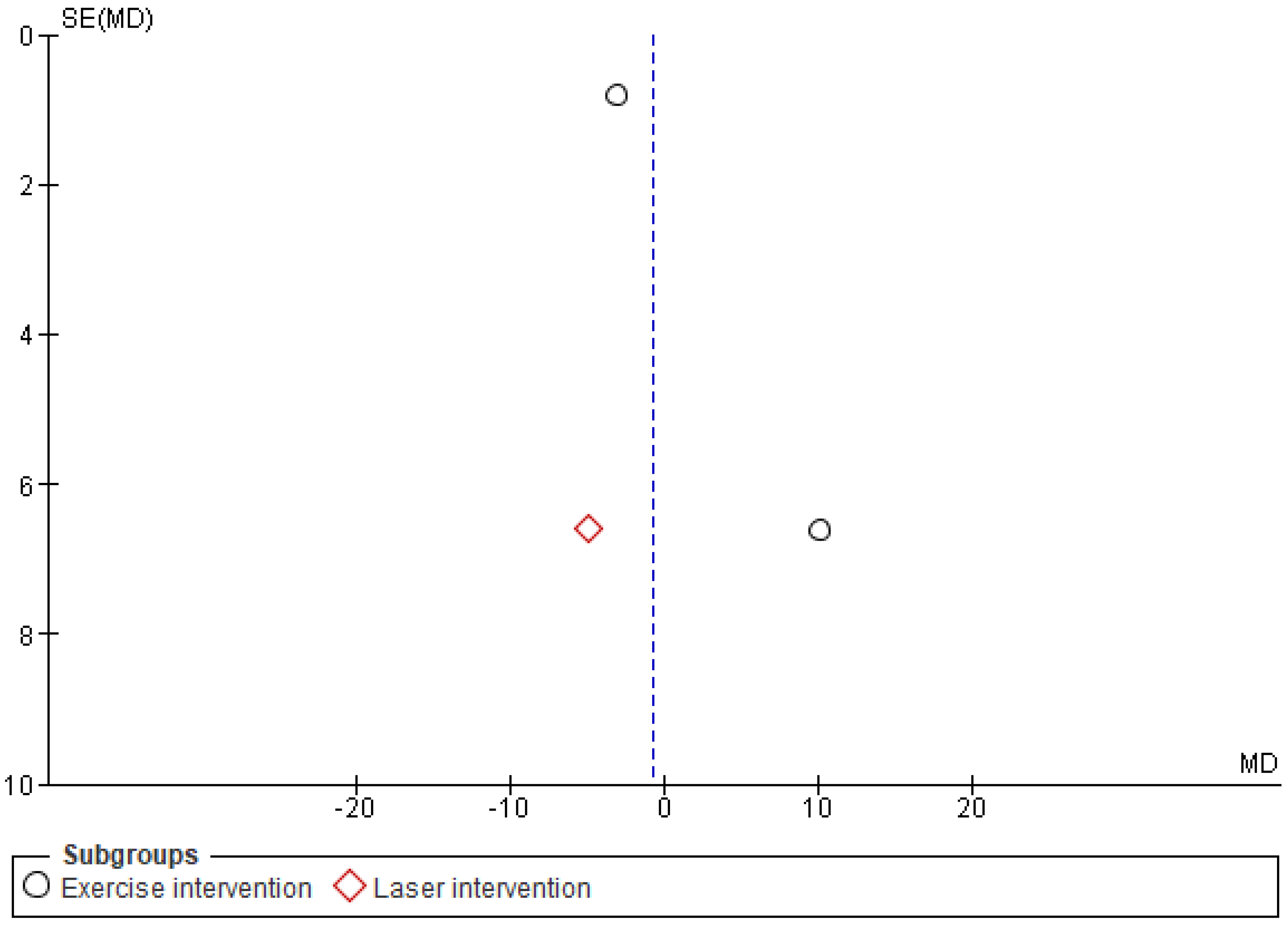
3.2.1. Measure of VAS before and after Therapy
3.2.2. Measure of Secondary Outcome
Analysis of TSK
Analysis of ODI
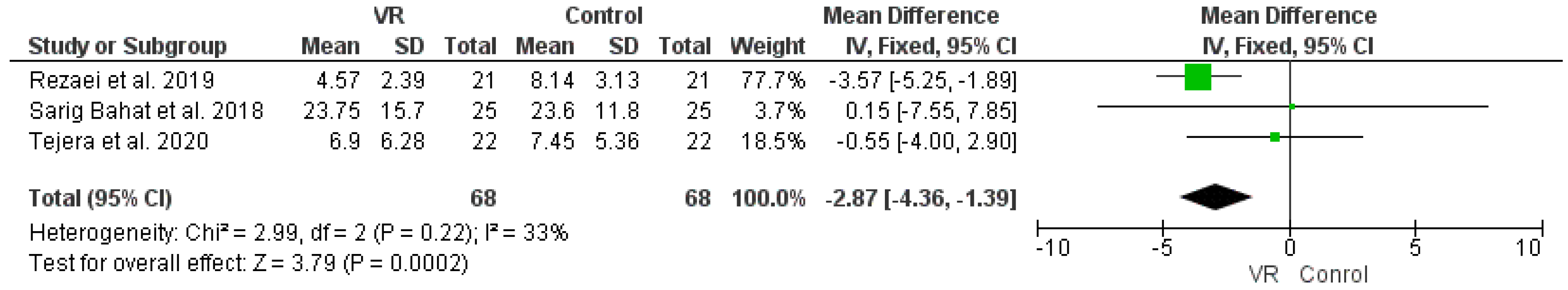
Analysis of NDI
3.3. ROB of Eligible Studies
4. Discussion
4.1. Future Implication
4.2. Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonica, J.J. The need of a taxonomy. Pain 1979, 6, 247–248. [Google Scholar]
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.; Mogil, J.S.; Ringkamp, R.M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef] [PubMed]
- Noble, M.; Treadwell, J.R.; Tregear, S.J.; Coates, V.H.; Wiffen, P.J.; Akafomo, C.; Schoelles, K.M.; Chou, R. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst. Rev. 2010, 1, CD006605. [Google Scholar] [CrossRef]
- Wardhan, R.; Chelly, J. Recent advances in acute pain management: Understanding the mechanisms of acute pain, the prescription of opioids, and the role of multimodal pain therapy. F1000Research 2017, 6, 2065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [Green Version]
- McMahon, S.B.; Dargan, P.; Lanas, A.; Wiffen, P. The burden of musculoskeletal pain and the role of topical non-steroidal anti-inflammatory drugs (NSAIDs) in its treatment. Ten underpinning statements from a global pain faculty. Curr. Med. Res. Opin. 2021, 37, 287–292. [Google Scholar] [CrossRef]
- Nadeau, S.E.; Wu, J.K.; Lawhern, R.A. Opioids and chronic pain: An analytic review of the clinical evidence. Front. Pain Res. 2021, 2, 44. [Google Scholar] [CrossRef]
- Højsted, J.; Sjøgren, P. Addiction to opioids in chronic pain patients: A literature review. Eur. J. Pain 2007, 11, 490–518. [Google Scholar] [CrossRef]
- Gerner, P. Postthoracotomy pain management problems. Anesthesiol. Clin. 2008, 26, 355–367. [Google Scholar]
- Chou, R.; Qaseem, A.; Snow, V.; Casey, D.; Cross, J.T.; Shekelle, P., Jr.; Owens, D.K. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann. Intern. Med. 2007, 147, 478–491. [Google Scholar] [CrossRef] [PubMed]
- Blondell, R.D.; Azadfard, M.; Wisniewski, A.M. Pharmacologic therapy for acute pain. Am. Fam. Physician 2013, 87, 766–772. [Google Scholar] [PubMed]
- Wiederhold, B.K.; Soomro, A.; Riva, G.; Wiederhold, M.D. Future directions: Advances and implications of virtual environments designed for pain management. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 414–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zadro, J.R.; Shirley, D.; Simic, M.; Mousavi, S.J.; Ceprnja, D.; Maka, K.; Sung, J.; Ferreira, P. Video-Game–Based Exercises for Older People with Chronic Low Back Pain: A Randomized Controlledtable Trial (GAMEBACK). Phys. Ther. 2019, 99, 14–27. [Google Scholar] [CrossRef]
- Grassini, S.; Laumann, K. Immersive visual technologies and human health. In Proceedings of the European Conference on Cognitive Ergonomics, Siena, Italy, 26 April 2021; pp. 1–6. [Google Scholar]
- Pereira, M.F.; Prahm, C.; Kolbenschlag, J.; Oliveira, E.; Rodrigues, N.F. Application of AR and VR in hand rehabilitation: A systematic review. J. Biomed. Inform. 2020, 111, 103584. [Google Scholar] [CrossRef] [PubMed]
- Piskorz, J.; Czub, M. Distraction of attention with the use of virtual reality. Influence of the level of game complexity on the level of experienced pain. Pol. Psychol. Bull. 2014, 45, 480–487. [Google Scholar] [CrossRef]
- Wiederhold, M.D.; Wiederhold, B.K. Virtual reality and interactive simulation for pain distraction. Pain Med. 2007, 8, S182–S188. [Google Scholar] [CrossRef]
- Sween, J.; Wallington, S.F.; Sheppard, V.; Taylor, T.; Llanos, A.A.; Adams-Campbell, L.L. The role of exergaming in improving physical activity: A review. J. Phys. Act. Health 2014, 11, 864. [Google Scholar] [CrossRef] [Green Version]
- Goyal, C.; Vardhan, V.; Naqvi, W. Virtual Reality-Based Intervention for Enhancing Upper Extremity Function in Children With Hemiplegic Cerebral Palsy: A Literature Review. Cureus 2022, 14, e21693. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, H.; Chen, Z.; Fu, R.; Yang, H.; Zeng, H.; Ren, Z. Benefits of Virtual Reality Balance Training for Patients With Parkinson Disease: Systematic Review, Meta-analysis, and Meta-Regression of a Randomized Controlled Trial. JMIR Serious Games 2022, 10, e30882. [Google Scholar] [CrossRef]
- Sevcenko, K.; Lindgren, I. The effects of virtual reality training in stroke and Parkinson’s disease rehabilitation: A systematic review and a perspective on usability. Eur. Rev. Aging Phys. Act. 2022, 19, 4. [Google Scholar] [CrossRef] [PubMed]
- Chou, P.H.; Tseng, P.T.; Wu, Y.C.; Chang, J.P.C.; Tu, Y.K.; Stubbs, B.; Carvalho, A.F.; Lin, P.-Y.; Chen, Y.-W.; Su, K.-P. Efficacy and acceptability of different interventions for acrophobia: A network meta-analysis of randomised controlled trials. J. Affect. Disord. 2021, 282, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Grassini, S.; Laumann, K. Questionnaire measures and physiological correlates of presence: A systematic review. Front. Psychol. 2020, 11, 349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grassini, S.; Laumann, K.; Topranin, V.D.M.; Thorp, S. Evaluating the effect of multi-sensory stimulations on simulator sickness and sense of presence during HMD-mediated VR experience. Ergonomics 2021, 64, 1532–1542. [Google Scholar] [CrossRef] [PubMed]
- Grassini, S.; Laumann, K.; Luzi, A. Association of individual factors with simulator sickness and sense of presence in virtual reality mediated by Head-Mounted Displays (HMDs). Multimodal Technol. Interact. 2021, 5, 7. [Google Scholar] [CrossRef]
- Slater, M.; Lotto, R.; Arnold, M.; Sanchez-Vives, M. How we experience immersive virtual environments: The concept of presence and its measurement. Anu. Psicol. 2009, 40, 193–210. [Google Scholar]
- Baus, O.; Bouchard, S. Moving from Virtual Reality Exposure-Based Therapy to Augmented Reality Exposure-Based Therapy: A Review. Front. Hum. Neurosci. 2014, 8, 112. [Google Scholar] [CrossRef] [Green Version]
- Li, A.; Montaño, Z.; Chen, V.J.; Gold, J.I. Virtual reality and pain management: Current trends and future directions. Pain Manag. 2011, 1, 147–157. [Google Scholar] [CrossRef] [Green Version]
- Garrett, B.; Taverner, T.; Masinde, W.; Gromala, D.; Shaw, C.; Negraeff, M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin. J. Pain 2014, 30, 1089–1098. [Google Scholar] [CrossRef]
- Triberti, S.; Repetto, C.; Riva, G. Psychological factors influencing the effectiveness of virtual reality-based analgesia: A systematic review. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 335–345. [Google Scholar] [CrossRef]
- Pourmand, A.; Davis, S.; Marchak, A.; Whiteside, T.; Sikka, N. Virtual reality as a clinical tool for pain management. Curr. Pain Headache Rep. 2018, 22, 53. [Google Scholar] [CrossRef] [PubMed]
- Ahmadpour, N.; Randall, H.; Choksi, H.; Gao, A.; Vaughan, C.; Poronnik, P. Virtual Reality interventions for acute and chronic pain management. Int. J. Biochem. Cell Biol. 2019, 114, 105568. [Google Scholar] [CrossRef] [PubMed]
- Trost, Z.; France, C.; Anam, M.; Shum, C. Virtual reality approaches to pain: Toward a state of the science. Pain 2021, 162, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.; Foster, S.; Sambell, R.; Leong, P. Clinical efficacy of virtual reality for acute procedural pain management: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0200987. [Google Scholar] [CrossRef] [Green Version]
- Mallari, B.; Spaeth, E.K.; Goh, H.; Boyd, B.S. Virtual reality as an analgesic for acute and chronic pain in adults: A systematic review and meta-analysis. J. Pain Res. 2019, 12, 2053. [Google Scholar] [CrossRef] [Green Version]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [Green Version]
- Chou, L.; Ranger, T.A.; Peiris, W.; Cicuttini, F.; Urquhart, D.M.; Sullivan, K.; Seneviwickrama, M.; Briggs, A.M.; Wluka, A.E. Patients’ perceived needs for medical services for non-specific low back pain: A systematic scoping review. PLoS ONE 2018, 13, e0204885. [Google Scholar] [CrossRef]
- Noori, S.A.; Rasheed, A.; Aiyer, R.; Jung, B.; Bansal, N.; Chang, K.V.; Ottestad, E.; Gulati, A. Therapeutic ultrasound for pain management in chronic low back pain and chronic neck pain: A systematic review. Pain Med. 2020, 21, 1482–1493. [Google Scholar] [CrossRef]
- Cherkin, D.C.; Herman, P.M. Cognitive and mind-body therapies for chronic low back pain and neck pain: Effectiveness and value. JAMA Intern. Med. 2018, 178, 556–557. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Oxford, 2000. [Google Scholar]
- Zwetsloot, P.P.; Van Der Naald, M.; Sena, E.S.; Howells, D.W.; IntHout, J.; De Groot, J.A.H.; Chamuleau, S.J.A.; MacLeod, M.R.; Wever, K.E. Standardized mean differences cause funnel plot distortion in publication bias assessments. Elife 2017, 6, e24260. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef] [Green Version]
- Chapman, J.R.; Norvell, D.C.; Hermsmeyer, J.T.; Bransford, R.J.; DeVine, J.; McGirt, M.J.; Lee, M.J. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine 2011, 36 (Suppl. 21), S54–S68. [Google Scholar] [CrossRef]
- Fairbank, J.; Couper, J.; Davies, J.; O’brien, J. The Oswestry low back pain disability questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar] [PubMed]
- Dennison, B.S.; Leal, M.H. Chapter 7—Mechanical neck pain. In Neck and Arm Pain Syndromes; Fernández de las Peñas, C., Cleland, J.A., Huijbregts, P.A., Eds.; Churchill Livingstone: Edinburgh, UK, 2011; pp. 94–111. [Google Scholar] [CrossRef]
- Review Manager (RevMan), version 5.4.1; The Cochrane Collaboration: Copenhagen, Denmark, 2020.
- Sterne, J.; Higgins, J.; Reeves, B. A Cochrane risk of bias assessment tool: For non-randomized studies of interventions (ACROBAT-NRSI). Version 2014, 1, 24. [Google Scholar]
- The EndNote Team. Endnote, version Endnote V20 [64 bit]; Clarivate: Philadelphia, PA, USA, 2013.
- Thomas, J.S.; France, C.R.; Applegate, M.E.; Leitkam, S.T.; Walkowski, S. Feasibility and Safety of a Virtual Reality Dodgeball Intervention for Chronic Low Back Pain: A Randomized Clinical Trial. J. Pain 2016, 17, 1302–1317. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Yu, Q.; Luo, H.; Liang, W.; Li, X.; Ge, L.; Zhang, S.; Li, L.; Wang, C. The Effect of Virtual Reality Training on Anticipatory Postural Adjustments in Patients with Chronic Nonspecific Low Back Pain: A Preliminary Study. Neural Plast. 2021, 2021, 9975862. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz Yelvar, G.D.; Cirak, Y.; Dalkilinc, M.; Parlak Demir, Y.; Guner, Z.; Boydak, A. Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial. Eur. Spine J. 2017, 26, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Darnall, B.D.; Krishnamurthy, P.; Tsuei, J.; Minor, J.D. Self-Administered Skills-Based Virtual Reality Intervention for Chronic Pain: Randomized Controlled Pilot Study. JMIR Res. 2020, 4, e17293. [Google Scholar] [CrossRef]
- Rezaei, I.; Razeghi, M.; Ebrahimi, S.; Kayedi, S.; Rezaeian Zadeh, A. A novel virtual reality technique (Cervigame®) compared to conventional proprioceptive training to treat neck pain: A randomized controlled trial. J. Biomed. Phys. Eng. 2019, 9, 355. [Google Scholar] [CrossRef]
- Sarig Bahat, H.; Croft, K.; Carter, C.; Hoddinott, A.; Sprecher, E.; Treleaven, J. Remote kinematic training for patients with chronic neck pain: A randomised controlled trial. Eur. Spine J. 2018, 27, 1309–1323. [Google Scholar] [CrossRef]
- Tejera, D.M.; Beltran-Alacreu, H.; Cano-de-la-Cuerda, R.; Leon Hernandez, J.V.; Martin-Pintado-Zugasti, A.; Calvo-Lobo, C.; Gil-Martinez, A.; Fernandez-Carnero, J. Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 5950. [Google Scholar] [CrossRef] [PubMed]
- Matheve, T.; Bogaerts, K.; Timmermans, A. Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: A randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 55. [Google Scholar] [CrossRef] [PubMed]
- Nambi, G.; Abdelbasset, W.K.; Alrawaili, S.M.; Alsubaie, S.F.; Abodonya, A.M.; Saleh, A.K. Virtual reality or isokinetic training; its effect on pain, kinesiophobia and serum stress hormones in chronic low back pain: A randomized controlled trial. Technol. Health Care 2021, 29, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Sarig Bahat, H.; Takasaki, H.; Chen, X.; Bet-Or, Y.; Treleaven, J. Cervical kinematic training with and without interactive VR training for chronic neck pain—A randomized clinical trial. Man. Ther. 2015, 20, 68–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.J.; Heo, M. Effects of virtual reality programs on balance in functional ankle instability. J. Phys. Sci. 2015, 27, 3097–3101. [Google Scholar] [CrossRef]
- Murray, C.D.; Patchick, E.L.; Caillette, F.; Howard, T.; Pettifer, S. Can immersive virtual reality reduce phantom limb pain? Stud. Health Technol. Inf. 2006, 119, 407–412. [Google Scholar]
- Bordeleau, M.; Stamenkovic, A.; Tardif, P.A.; Thomas, J. The Use of Virtual Reality in Back Pain Rehabilitation: A Systematic Review and Meta-Analysis. J. Pain. 2021, 23, 175–195. [Google Scholar] [CrossRef]
- Cipresso, P.; Giglioli, I.A.C.; Raya, M.A.; Riva, G. The Past, Present, and Future of Virtual and Augmented Reality Research: A Network and Cluster Analysis of the Literature. Front. Psychol. 2018, 9, 2086. [Google Scholar] [CrossRef] [Green Version]
- Kober, S.E.; Neuper, C. Using auditory event-related EEG potentials to assess presence in virtual reality. Int. J. Hum.-Comput. Stud. 2012, 70, 577–587. [Google Scholar] [CrossRef]
- Grassini, S.; Laumann, K.; Thorp, S.; Topranin, V.D.M. Using electrophysiological measures to evaluate the sense of presence in immersive virtual environments: An event-related potential study. Brain Behav. 2021, 11, e2269. [Google Scholar] [CrossRef]





| Authors & Years | Study Design | Participants (I/C) | Age (I/C) | Pain Type | VR Environments | Treatment Conditions | Pain Assessment | Summary | NOS |
|---|---|---|---|---|---|---|---|---|---|
| Thomas et al. [50] | RCT | 52 (26/26) | I: 23.9 ± 6.8 C: 26.7 ± 8.5 | chronic low back pain | VR Dodgeball | IG: VR entertainment and distraction; CG: CAU | VAS, PPI, PRI, TKS | Decrease in VAS score & Pain intensity in VR group. | 7 |
| Li et al. [51] | RCT | 34 (I: 11; EG: 12; C:11) | I: 21.91 ± 2.43 EG: 23.75 ± 4.09 CG: 25.36 ± 3.72 | chronic low back pain | Kinect Xbox 360 system: Fruit Ninja game | IG: VR gaming + MT EG: Four-point kneeling exercise + MT CG:MT | VAS, ODI | VAS scores were reduced in each group after intervention. | 6 |
| Rezaei et al. [54] | RCT | 42 (21/21) | I: 36.19 ± 9.80 C: 31.23 ± 9.49 | chronic neck pain | Gaming: Cervi game | IG: VR gaming CG: CAU | VAS, NDI | VR improved neck pain and disability | 7 |
| Yilmaz Yelvar et al. [52] | RCT | 44 (22/22) | I: 46.3 ± 3.4 C: 52.8 ± 11.5 | chronic low-back pain | Video of walking down the Ireland forest | IG: virtual walking task CG: CAU | VAS, TSK, ODI | VR reduced VAS and TKS | 8 |
| Sarig Bahat et al. [55] | RCT | 90 IG: 30 LG: 30 CG: 30 | IG: 48 ± 5.49 LG: 47.6 ± 6.78 CG: 47.5 ± 6.9 | chronic neck pain | VR: kinematic training | IG: kinematic training | VAS, NDI, TSK, | VR demonstrate improved pain relief | 6 |
| Matheve et al. [57] | RCT | 84 (42/42) | I: 42.1 ± 11.5 C: 44.2 ± 11.9 | chronic low back pain | VR gaming | IG: Exercise + VR CG: CAU | PPI | VR reduced PPI. | 8 |
| Darnall et al. [53] | RCT | 74 (35/39) | 18–74 | chronic low back pain | VR multimedia with audio | IG: VR CG: audio effect | PPI | both groups demonstrated reduced pain effects | 7 |
| Tejera et al. [56] | RCT | 44 (22/22) | I: 32.72 ± 11.63 C: 26.68 ± 9.21 | chronic neck pain | VR Vox Play glass with HMD clamping system and smartphone + Full dive VR + VR Ocean Aquarium 3D | IG: VR Vox Play glass with HMD clamping system and smartphone CG: CAU | VAS, NDI, TSK, | VR did not demonstrate significant difference | 8 |
| Nambi et al. [58] | RCT | 60 IG: 20 EG: 20 CG: 20 | IG: 23.2 ± 1.5 EG: 22.8 ± 1.6 CG: 23.3 ± 1.5 | chronic low back pain | VR shooting game | IG: VR + Shooting game EG: isokinetic exercise CG: conventional training | VAS, TSK | VAS and TSK reduced after VR therapy | 6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grassini, S. Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4071. https://doi.org/10.3390/ijerph19074071
Grassini S. Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(7):4071. https://doi.org/10.3390/ijerph19074071
Chicago/Turabian StyleGrassini, Simone. 2022. "Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 7: 4071. https://doi.org/10.3390/ijerph19074071






