Is the SARS CoV-2 Omicron Variant Deadlier and More Transmissible Than Delta Variant?
Abstract
:1. Introduction
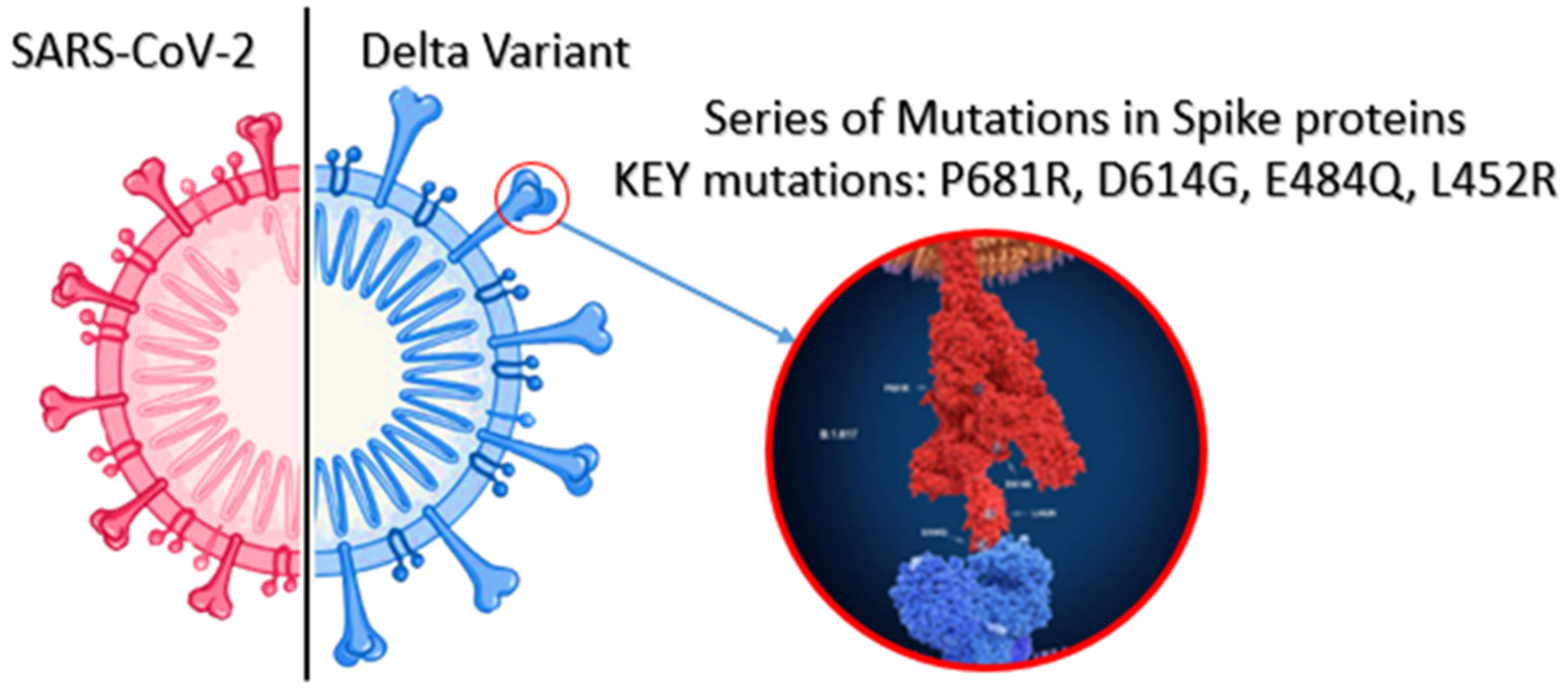
2. SARS-CoV-2, Delta Variant and Omicron Variant
2.1. Chemical Composition
2.2. Delta Variant and Omicron Variant Outbreaks
2.3. Transmission
2.3.1. Respiratory Droplet Transmission
2.3.2. Transmission by Exposure to Contaminants
2.3.3. Airborne or Aerosol Transmission
2.3.4. Animal to Human
2.3.5. Human Behaviours—Sneezing without Wearing a Mask
2.4. The Difference in Transmissibility between the Delta Variant and Omicron Variant
2.5. Severity and Mortality
3. Preventions
Vaccination Programs
4. Conclusions
- The Delta variant is highly infectious, estimated to be more than double that of the previous variants.
- Fully vaccinated people can significantly become infected by the Delta variant versus other variants, known as breakthrough infections.
- The Omicron variant is currently the most divergent variant, with a high number of 26 unique mutations in the spike protein.
- There are limited data on the severity and mortality profile of the Omicron variant. However, based on the available meta-data from the validated resources, the Omicron variant significantly affected the increase in daily hospitalization compared to the daily cases during the peak of the Delta outbreak. However, the Omicron variant had less effect on the daily ICU case. A higher fully vaccinated rate is one of the main factors for the reduction of daily ICU cases recently.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hasnain, M.; Pasha, M.F.; Ghani, I. Combined measures to control the COVID-19 pandemic in Wuhan, Hubei, China: A narrative review. J. Biosaf. Biosecur. 2020, 2, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Gui, X.; Gao, S.; Ke, H.; Xiong, Y. Clinical progression and changes of chest CT findings among asymptomatic and pre-symptomatic patients with SARS-CoV-2 infection in Wuhan, China. Expert Rev. Respir. Med. 2021, 15, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Duan, S.; Zhou, M.; Zhang, W.; Shen, J.; Qi, R.; Qin, X.; Yu, H.; Zhou, C.; Hu, Q.; Yu, X.-J. Seroprevalence and asymptomatic carrier status of SARS-CoV-2 in Wuhan City and other places of China. PLoS Negl. Trop. Dis. 2021, 15, e0008975. [Google Scholar] [CrossRef] [PubMed]
- Dash, D.P.; Sethi, N.; Dash, A.K. Infectious disease, human capital, and the BRICS economy in the time of COVID-19. MethodsX 2021, 8, 101202. [Google Scholar] [CrossRef]
- Khurshid, A.; Khan, K. How COVID-19 shock will drive the economy and climate? A data-driven approach to model and forecast. Environ. Sci. Pollut. Res. 2021, 28, 2948–2958. [Google Scholar] [CrossRef]
- Lim, W.M.; To, W.-M. The economic impact of a global pandemic on the tourism economy: The case of COVID-19 and Macao’s destination- and gambling-dependent economy. Curr. Issues Tour. 2021, 25, 1258–1269. [Google Scholar] [CrossRef]
- Pham, T.D.; Dwyer, L.; Su, J.-J.; Ngo, T. COVID-19 impacts of inbound tourism on Australian economy. Ann. Tour. Res. 2021, 88, 103179. [Google Scholar] [CrossRef]
- Sandmann, F.G.; Davies, N.G.; Vassall, A.; Edmunds, W.J.; Jit, P.M. The potential health and economic value of SARS-CoV-2 vaccination alongside physical distancing in the UK: A transmission model-based future scenario analysis and economic evaluation. Lancet Infect. Dis. 2021, 21, 962–974. [Google Scholar] [CrossRef]
- Gu, Q.; Qi, S.; Yue, Y.; Shen, J.; Zhang, B.; Sun, W.; Qian, W.; Islam, M.S.; Saha, S.; Wu, J. Structural and functional alterations of the tracheobronchial tree after left upper pulmonary lobectomy for lung cancer. Biomed. Eng. Online 2019, 18, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Islam, M.S.; Saha, S.C.; Sauret, E.; Gu, Y.; Ristovski, Z. Numerical investigation of aerosol particle transport and deposition in realistic lung airway. In Proceedings of the International Conference on Computational Methods, Auckland, New Zealand, 14–17 July 2015. [Google Scholar]
- Islam, M.S.; Saha, S.C.; Sauret, E.; Ong, H.; Young, P.; Gu, Y. Euler–Lagrange approach to investigate respiratory anatomical shape effects on aerosol particle transport and deposition. Toxicol. Res. Appl. 2019, 3, 2397847319894675. [Google Scholar] [CrossRef] [Green Version]
- Islam, M.; Larpruenrudee, P.; Hossain, S.; Rahimi-Gorji, M.; Gu, Y.; Saha, S.; Paul, G. Polydisperse Aerosol Transport and Deposition in Upper Airways of Age-Specific Lung. Int. J. Environ. Res. Public Health 2021, 18, 6239. [Google Scholar] [CrossRef] [PubMed]
- Hendryx, M.; Islam, M.S.; Dong, G.-H.; Paul, G. Air Pollution Emissions 2008–2018 from Australian Coal Mining: Implications for Public and Occupational Health. Int. J. Environ. Res. Public Health 2020, 17, 1570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Islam, M.S.; Gu, Y.; Farkas, A.; Paul, G.; Saha, S.C. Helium–Oxygen Mixture Model for Particle Transport in CT-Based Upper Airways. Int. J. Environ. Res. Public Health 2020, 17, 3574. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Raghav, V.; Padhmashali, V.; Paul, G.; Islam, M.S.; Saha, S.C. Airflow and Particle Transport Prediction through Stenosis Airways. Int. J. Environ. Res. Public Health 2020, 17, 1119. [Google Scholar] [CrossRef] [Green Version]
- Larpruenrudee, P.; Islam, M.S.; Paul, G.; Paul, A.R.; Gu, Y.T.; Saha, S.C. Model for Pharmaceutical Aerosol Transport through Stenosis Airway. In Handbook of Lung Targeted Drug Delivery Systems; Pathak, Y., Islam, N., Eds.; Taylor & Francis Group: Boca Raton, FL, USA, 2021; p. 38. Available online: https://www.taylorfrancis.com/chapters/edit/10.1201/9781003046547-8/model-pharmaceutical-aerosol-transport-stenosis-airway-puchanee-larpruenrudee-mohammad-islam-gunther-paul-akshoy-paul-gu-suvash-saha (accessed on 23 March 2022).
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef]
- Islam, M.S.; Larpruenrudee, P.; Saha, S.C.; Pourmehran, O.; Paul, A.R.; Gemci, T.; Collins, R.; Paul, G.; Gu, Y. How severe acute respiratory syndrome coronavirus-2 aerosol propagates through the age-specific upper airways. Phys. Fluids 2021, 33, 081911. [Google Scholar] [CrossRef]
- Islam, M.S.; Larpruenrudee, P.; Paul, A.R.; Paul, G.; Gemci, T.; Gu, Y.; Saha, S.C. SARS CoV-2 aerosol: How far it can travel to the lower airways? Phys. Fluids 2021, 33, 061903. [Google Scholar] [CrossRef]
- Ghosh, A.; Islam, M.S.; Saha, S.C. Targeted Drug Delivery of Magnetic Nano-Particle in the Specific Lung Region. Computation 2020, 8, 10. [Google Scholar] [CrossRef] [Green Version]
- Frampton, M.W. Systemic and Cardiovascular Effects of Airway Injury and Inflammation: Ultrafine Particle Exposure in Humans. Environ. Health Perspect. 2001, 109, 529. [Google Scholar] [CrossRef]
- Hsiao, I.-L.; Huang, Y.-J. Effects of serum on cytotoxicity of nano- and micro-sized ZnO particles. J. Nanopart. Res. 2013, 15, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Oberdörster, G. Pulmonary effects of inhaled ultrafine particles. Int. Arch. Occup. Environ. Health 2000, 74, 1–8. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 29 March 2022).
- Van Oosterhout, C.; Hall, N.; Ly, H.; Tyler, K.M. COVID-19 evolution during the pandemic—Implications of new SARS-CoV-2 variants on disease control and public health policies. Virulence 2021, 12, 507–508. [Google Scholar] [CrossRef] [PubMed]
- Sixt, T.; Moretto, F.; Devilliers, H.; Abdallahoui, M.; Eberl, I.; Rogier, T.; Duong, M.; Salmon-Rousseau, A.; Mahy, S.; Buisson, M.; et al. The Usefullness of NEWS2 at Day 7 of Hospitalisation in Predicting COVID-19 Evolution and As an Early Endpoint in Therapeutic Trials. J. Infect. 2021, 82, 282–327. [Google Scholar] [CrossRef]
- Ben Hassen, H.; Elaoud, A.; Ben Salah, N.; Masmoudi, A. A SIR-Poisson Model for COVID-19: Evolution and Transmission Inference in the Maghreb Central Regions. Arab. J. Sci. Eng. 2021, 46, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Veronese, S.; Sbarbati, A. Chemosensory Systems in COVID-19: Evolution of Scientific Research. ACS Chem. Neurosci. 2021, 12, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Communicable Diseases Genomics Network. Available online: https://www.cdgn.org.au/variants-of-concern (accessed on 23 August 2021).
- European Centre for Disease Prevention and Control. SARS-CoV-2 Variants of Concern as of 26 August 2021. Available online: https://www.ecdc.europa.eu/en/covid-19/variants-concern (accessed on 26 August 2021).
- Centers for Disease Control and Prevention. SARS-CoV-2 Variant Classifications and Definitions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcases-updates%2Fvariant-surveillance%2Fvariant-info.html (accessed on 24 August 2021).
- World Health Organization. Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed on 23 March 2022).
- Kadri, S.S.; Simpson, S.Q. Potential Implications of SARS-CoV-2 Delta Variant Surges for Rural Areas and Hospitals. JAMA 2021, 326, 1003–1004. [Google Scholar] [CrossRef]
- Del Rio, C.; Malani, P.N.; Omer, S.B. Confronting the Delta Variant of SARS-CoV-2, Summer 2021. JAMA 2021, 326, 1001–1002. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, M.; Bhattacharyya, R.; Purkayastha, S.; Zimmermann, L.; Ray, D.; Hazra, A.; Kleinsasser, M.; Mellan, T.; Whittaker, C.; Flaxman, S.; et al. Resurgence of SARS-CoV-2 in India: Potential role of the B.1.617.2 (Delta) variant and delayed interventions. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.06.23.21259405v1 (accessed on 23 March 2022).
- Yang, W.; Shaman, J. COVID-19 Pandemic Dynamics in India and Impact of the SARS-CoV-2 Delta (B.1.617.2) Variant. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.06.21.21259268v1 (accessed on 23 March 2022).
- Novelli, G.; Colona, V.L.; Pandolfi, P.P. A focus on the spread of the delta variant of SARS-CoV-2 in India. Indian J. Med. Res. 2021, 153, 537. [Google Scholar] [CrossRef]
- Kupferschmidt, K.; Wadman, M. Delta variant triggers new phase in the pandemic. Science 2021, 372, 1375–1376. [Google Scholar] [CrossRef]
- Alexandar, S.; Ravisankar, M.; Kumar, R.S.; Jakkan, K. A Comprehensive Review on COVID-19 Delta Variant. International Journal of Parmacology and Clinical Research (IJPCR). Available online: https://www.researchgate.net/profile/Ravisankar-Mathesan/publication/353179027_A_Comprehensive_Review_on_Covid-19_Delta_variant/links/60ec151630e8e50c01fbf87c/A-Comprehensive-Review-on-Covid-19-Delta-variant.pdf (accessed on 23 March 2022).
- Twohig, K.A.; Nyberg, T.; Zaidi, A.; Thelwall, S.; Sinnathamby, M.A.; Aliabadi, S.; Seaman, S.R.; Harris, R.J.; Hope, R.; Lopez-Bernal, J.; et al. Hospital Admission and Emergency Care Attendance Risk for SARS-CoV-2 Delta (B.1.617.2) Compared with Alpha (B.1.1.7) Variants of Concern: A Cohort Study. Lancet Infect. Dis. 2021, 22, 35–42. [Google Scholar] [CrossRef]
- Liu, Y.; Rocklöv, J. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J. Travel Med. 2021, 28, taab124. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.; McMenamin, J.; Taylor, B.; Robertson, C. SARS-CoV-2 Delta VOC in Scotland: Demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021, 397, 2461–2462. [Google Scholar] [CrossRef]
- Fisman, D.N.; Tuite, A.R. Progressive Increase in Virulence of Novel SARS-CoV-2 Variants in Ontario, Canada. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.07.05.21260050v2 (accessed on 23 March 2022).
- Riemersma, K.A.; Grogan, B.E.; Kirta-Yarbo, A.; Halfmann, P.J.; Segaloff, H.E.; Kocharian, A.; Florek, K.R.; Westergaard, R.; Bateman, A.; Jeppson, G.E.; et al. Vaccinated and Unvaccinated Individuals Have Similar Viral Loads in Communities with a High Prevalence of the SARS-CoV-2 Delta Variant. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.07.31.21261387v1 (accessed on 23 March 2022).
- Nasreen, S.; Chung, H.; He, S.; Brown, K.A.; Gubbay, J.B.; Buchan, S.A.; Fell, D.B.; Austin, P.C.; Schwartz, K.L.; Sundaram, M.E.; et al. Effectiveness of COVID-19 Vaccines against Variants of Concern in Ontario, Canada. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.06.28.21259420v2 (accessed on 23 March 2022).
- Chang, S.L.; Cliff, O.M.; Zachreson, C.; Prokopenko, M. Nowcasting Transmission and Suppression of the Delta Variant of SARS-CoV-2 in Australia. Available online: https://assets.researchsquare.com/files/rs-757351/v1_covered.pdf?c=1631875806 (accessed on 23 March 2022).
- Blakely, T.; Thompson, J.; Carvalho, N.; Bablani, L.; Wilson, N.; Stevenson, M. The Probability of the 6-Week Lockdown in Victoria (Commencing 9 July 2020) Achieving Elimination of Community Transmission of SARS-CoV-2. Med. J. Aust. 2020, 213, 349–351.e341. [Google Scholar] [CrossRef] [PubMed]
- Zachreson, C.; Mitchell, L.; Lydeamore, M.J.; Rebuli, N.; Tomko, M.; Geard, N. Risk mapping for COVID-19 Outbreaks in Australia using mobility data. J. R. Soc. Interface 2021, 18, 20200657. [Google Scholar] [CrossRef]
- Nguyen, K. Sweeping New Lockdown Restrictions Announced as NSW Records 111 New COVID Cases. ABC News. 2021. Available online: https://www.abc.net.au/news/2021-07-17/nsw-records-111-covid-19-cases/100300492 (accessed on 17 July 2021).
- World Health Organization. Classification of Omicron (B.1.1529): SARS-CoV-2 Variant of Concern. Available online: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed on 26 November 2021).
- Rao, S.; Singh, M. The Newly Detected B.1.1.529 (Omicron) Variant of SARS-CoV-2 with Multiple Mutations. DHR Proc. 2021, 1, 7–10. [Google Scholar] [CrossRef]
- Venkatakrishnan, A.; Anand, P.; Lenehan, P.; Suratekar, R.; Raghunathan, B.; Niesen, M.J.; Soundararajan, V. Omicron Variant of SARS-CoV-2 Harbors a Unique Insertion Mutation of Putative Viral or Human Genomic Origin. Available online: https://osf.io/f7txy/ (accessed on 23 March 2022).
- Karim SS, A.; Karim, Q.A. Omicron SARS-CoV-2 variant: A new chapter in the COVID-19 pandemic. Lancet 2021, 398, 2126–2128. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). COVID-19 Situation Updates. Available online: https://www.ecdc.europa.eu/en/covid-19/situation-updates (accessed on 23 March 2022).
- Meo, S.A.; Meo, A.S.; Al-Jassir, F.F.; Klonoff, D.C. Omicron SARS-CoV-2 new variant: Global prevalence and biological and clinical characteristics. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 8012–8018. [Google Scholar] [PubMed]
- Mohapatra, R.K.; Sarangi, A.K.; Kandi, V.; Azam, M.; Tiwari, R.; Dhama, K. Omicron (B.1.1.529 variant of SARS-CoV-2); an emerging threat: Current global scenario. J. Med. Virol. 2021, 94, 1780–1783. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Understanding Variants. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/understanding-variants.html (accessed on 23 March 2022).
- Alizong, S.; Haim-Boukobza, S.; Foulongne, V.; Verdurme, L.; Trombert-Paolantoni, S.; Lecorche, E.; Roquebert, B.; Sofonea, M.T. Rapid Spread of the SARS-CoV-2 Delta Variant in Some French Regions, June 2021. Eurosurveillance 2021, 26, 2100573. [Google Scholar]
- Stern, A.; Fleishon, S.; Kustin, T.; Dotan, E.; Mandelboim, M.; Erster, O.; Israel Consortium of SARS-CoV-2 Sequencing; Mendelson, E.; Mor, O.; Zuckerman, N.S. The Unique Evolutionary Dynamics of the SARS-CoV-2 Delta Variant. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.08.05.21261642v2.full.pdf+html (accessed on 23 March 2022).
- Patane, J.; Viala, V.; Lima, L.; Martins, A.; Barros, C.; Marqueze, E.; Bernardino, J.; Moretti, D.; Slavov, S.; Bezerra, R.; et al. SARS-CoV-2 Delta Variant of Concern in Brazil—Multiple Introdutions, Communitary Transmission, and Early Signs of Local Evolution. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.09.15.21262846v1 (accessed on 23 March 2022).
- Kannan, S.R.; Spratt, A.N.; Cohen, A.R.; Naqvi, S.H.; Chand, H.S.; Quinn, T.P.; Lorson, C.L.; Byrareddy, S.N.; Singh, K. Evolutionary analysis of the Delta and Delta Plus variants of the SARS-CoV-2 viruses. J. Autoimmun. 2021, 124, 102715. [Google Scholar] [CrossRef]
- Mishra, S.; Mindermann, S.; Sharma, M.; Whittaker, C.; A Mellan, T.; Wilton, T.; Klapsa, D.; Mate, R.; Fritzsche, M.; Zambon, M.; et al. Changing composition of SARS-CoV-2 lineages and rise of Delta variant in England. EClinicalMedicine 2021, 39, 101064. [Google Scholar] [CrossRef]
- Mohammadi, M.; Shayestehpour, M.; Mirzaei, H. The impact of spike mutated variants of SARS-CoV2 [Alpha, Beta, Gamma, Delta, and Lambda] on the efficacy of subunit recombinant vaccines. Braz. J. Infect. Dis. 2021, 25, 101606. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed on 23 March 2022).
- Ashly Hagen, M.S. How Dangerous Is the Delta Variant (B.1.617.2). Available online: https://asm.org/Articles/2021/July/How-Dangerous-is-the-Delta-Variant-B-1-617-2 (accessed on 30 July 2021).
- NSW Health, COVID-19 (Coronavirus). Available online: https://www.health.nsw.gov.au/Infectious/covid-19/Pages/stats-nsw.aspx (accessed on 23 March 2022).
- Our World in Data, SARS-CoV-2 Sequences by Variant, 21 March 2022. Available online: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=latest&facet=none&pickerSort=asc&pickerMetric=location&Interval=7-day+rolling+average&Relative+to+Population=true&Color+by+test+positivity=false&country=USA~GBR~IND~AUS~BRA~FRA&Metric=Variants (accessed on 23 March 2022).
- Tommaso, C.B.; Mohsen, M.; George, W.R.; Nooshin, R. Outdoor Transmission of SARS-CoV-2 and Other Respiratory Viruses: A Systematic Review. J. Infect. Dis. 2021, 223, 550–561. [Google Scholar] [CrossRef]
- Athalia, C.; John, T.; Lauri, A.; Sauber-Schatz, E.K.; Yoder, J.S.; Honein, M.A. Guidance for Implementing COVID-9 Prevention Strategies in the Context of Varying Community Transmission Levels and Vaccination Coverage. Available online: https://www.cdc.gov/mmwr/volumes/70/wr/mm7030e2.htm (accessed on 27 July 2021).
- Jonathan, R.; Kendall, D.; Russell, E.; Christensen, J.H.; Halvorsen, T.G.; Hogan, C.G., Jr.; O’horo, J.C.; Breeher, L.E.; Callstrom, M.R.; Wehde, M.B. Combined Effects of Masking and Distance on Aerosol Exposure Potential. Mayo Clin. Proc. 2021, 96, 1792–1800. [Google Scholar] [CrossRef]
- Morawska, L.; Johnson, G.R.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Corbett, S.; Chao, C.Y.H.; Li, Y.; Katoshevski, D. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J. Aerosol. Sci. 2009, 40, 256–269. [Google Scholar] [CrossRef] [Green Version]
- Lea, H.; Polly, D.; Ian, C.; Ross, A.; Jordan, A.; Lee, J.; Lynn, J.; Ball, A.; Narwal, S.; Russell, S.; et al. High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice—Skagit County, Washington, March 2020. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e6.htm (accessed on 15 May 2020).
- Jamous, F.; Meyer, N.; Buus, D.; Ateeli, H.; Taggart, K.; Hanson, T.; Alzoubaidi, M.; Nazir, J.; Devasahayam, J. Critical Illness Due to Covid-19: A Description of the Surge in a Single Center in Sioux Falls. SD Med. 2020, 73, 312–317. [Google Scholar]
- De Man, P.; Paltansing, S.; Ong, D.S.Y.; Vaessen, N.; van Nielen, G.; Koeleman, J.G.M. Outbreak of Coronavirus Disease 2019 (COVID-19) in a Nursing Home Associated with Aerosol Transmission as a Result of Inadequate Ventilation. Clin. Infect. Dis. 2020, 73, 170–171. [Google Scholar] [CrossRef] [PubMed]
- Bilinski, A.; Mostashari, F.; Salomon, J.A. Modeling Contact Tracing Strategies for COVID-19 in the Context of Relaxed Physical Distancing Measures. JAMA Netw. Open 2020, 3, e2019217. [Google Scholar] [CrossRef]
- Public Health England. SARS-CoV-2 Variants of Concern and Variants under Investigation in England. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1018547/Technical_Briefing_23_21_09_16.pdf (accessed on 23 March 2022).
- Khedar, R.S.; Mittal, K.; Ambaliya, H.C.; Mathur, A.; Gupta, J.B.; Sharma, K.K.; Singh, Y.; Sharma, G.; Gupta, A.; Bhargava, V. Greater Covid-19 Severity and Mortality in Hospitalized Patients in Second (Delta Variant) Wave Compared to the First: Single Centre Prospective Study in India. medRxiv 2021. [Google Scholar] [CrossRef]
- Chia, P.Y.; Xiang Ong, S.W.; Chiew, C.J.; Ang, L.W.; Chavatte, J.-M.; Mak, T.-M.; Cui, L.; Kalimuddin, S.; Chia, W.N.; Tan, C.W.; et al. Virological and serological kinetics of SARS-CoV-2 Delta variant vaccine-breakthrough infections: A multi-center cohort study. medRxiv 2021, 28, 612.e1–612.e7. [Google Scholar] [CrossRef]
- Riemersma, K.K.; Grogan, B.E.; Kita-Yarbro, A.; Halfmann, P.J.; Segaloff, H.E.; Kocharian, A.; Florek, K.R.; Westergaard, R.; Bateman, A.; Jeppson, G.E.; et al. Shedding of Infectious SARS-CoV-2 Despite Vaccination. medRxiv 2021. [Google Scholar] [CrossRef]
- Chakraborty, C.; Bhattacharya, M.; Sharma, A.R. Present variants of concern and variants of interest of severe acute respiratory syndrome coronavirus 2: Their significant mutations in S-glycoprotein, infectivity, re-infectivity, immune escape and vaccines activity. Rev. Med. Virol. 2021, 32, e2270. [Google Scholar] [CrossRef]
- Lechien, J.R.; Saussez, S. Importance of epidemiological factors in the evaluation of transmissibility and clinical severity of SARS-CoV-2 variants. Lancet Infect. Dis. 2021, 22, 2–3. [Google Scholar] [CrossRef]
- Honein, M.A.; Christie, A.; Rose, D.A.; Brooks, J.T.; Meaney-Delman, D.; Cohn, A.; Sauber-Schatz, E.K.; Walker, A.; McDonald, L.C.; Liburd, L.C.; et al. Summary of Guidance for Public Health Strategies to Address High Levels of Community Transmission of SARS-CoV-2 and Related Deaths, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1860–1867. [Google Scholar] [CrossRef] [PubMed]
- Heath Data. Gov, COVID-19 Report Patient Impact and Hospital Capacity by State Timeseries. Available online: https://healthdata.gov/Hospital/COVID-19-Reported-Patient-Impact-and-Hospital-Capa/g62h-syeh (accessed on 23 March 2022).
- GOV.UK Coronavirus (COVID-19) in the UK, Healthcare in United Kingdom. Available online: https://coronavirus.data.gov.uk/details/healthcare (accessed on 23 March 2022).
- Données Hospitalières Relatives à l’épidémie de COVID-19 SIVIC. Available online: https://www.data.gouv.fr/fr/datasets/donnees-hospitalieres-relatives-a-lepidemie-de-covid-19/ (accessed on 23 March 2022).
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; COVID-19 Systematic Urgent Review Group Effort (SURGE) Study Authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Harris, R.J.; Hall, J.A.; Zaidi, A.; Andrews, N.J.; Dunbar, J.K.; Dabrera, G. Effect of Vaccination on Household Transmission of SARS-CoV-2 in England. N. Engl. J. Med. 2021, 385, 759–760. [Google Scholar] [CrossRef] [PubMed]
- Bose, P. Researchers Examnie the Effectiveness of the Pfizer-BioNTech COVID-19 Vaccine in Reducing Household Transmission. News Medical Life Sciences. Available online: https://www.news-medical.net/news/20210720/Researchers-examine-the-effectiveness-of-the-Pfizer-BioNTech-COVID-19-vaccine-in-reducing-household-transmission.aspx (accessed on 20 July 2021).
- Vitiello, A.; Ferrara, F.; Troiano, V.; La Porta, R. COVID-19 vaccines and decreased transmission of SARS-CoV-2. Inflammopharmacology 2021, 29, 1357–1360. [Google Scholar] [CrossRef]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef]
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Gallagher, E.; Simmons, R.; Thelwall, S.; Stowe, J.; Tessier, E.; Groves, N.; Dabrera, G.; et al. Effectiveness of COVID-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. 2021, 385, 585–594. [Google Scholar] [CrossRef]
- Catherine, M.; Johanna, V.; Hillary, J.; Burns, M.; Gharpure, R.; Sami, S.; Sabo, R.T.; Hall, N.; Foreman, A.; Schubert, P.L.; et al. Outbreak of SARS-CoV-2 Infections, Including COVID-19 Vaccine Breakthrough Infections, Associated with Large Public Gatherings—Barnstable County, Massachusetts. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/mmwr/volumes/70/wr/mm7031e2.htm (accessed on 6 August 2021).
- UK Health Security Agency. Technical Briefing: Update on Hospitalisation and Vaccine Effectiveness for Omicron VOC-21NOV-01 (B.1.1529). SARS-CoV-2 Variants of Concern and Variants Under Investigation in England. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1044481/Technical-Briefing-31-Dec-2021-Omicron_severity_update.pdf (accessed on 31 December 2021).


















| WHO Label | Pango Lineages | GISAID Clade | Next Strain Clade | Additional Amino Acid Changes Monitored | Earliest Documented Samples | Date of Designation |
|---|---|---|---|---|---|---|
| Alpha | B.1.1.7 | GRY | 201 (V1) | +S:484K +S:452R | United Kingdom, September 2020 | 18 December 2020 |
| Beta | B.1.351 B.1.351.2 B.1.351.3 | GH/501Y.V2 | 20H (V2) | +S:L18F | South Africa, May 2020 | 18 December 2020 |
| Gamma | P.1 P.1.1 P.1.2 P.1.4 P.1.6 P.1.7 | GR/501Y.V3 | 20J (V3) | +S:681H | Brazil, November 2020 | 11 January 2021 |
| Delta | B.1.617.2 AY.1 AY.2 AY.3 AY.3.1 | G/478K.V1 | 21A | +S 417N | India, October 2020 | VOI: 4 April 2021 VOC: 11 May 2021 |
| Omicron | B.1.1.529 | GR/484A | 21K | +G339D +S371L +S373L | Botswana, 11 November 2021 | VOC: 26 November 2021 |
| Variants | Total Spike Mutations | Unique Spike Mutations |
|---|---|---|
| Alpha | 11 | (4): A570D, D1118H, S982A, T716I |
| Beta | 10 | (6): A701V, D215G, D80A, ΔL242, ΔA243 |
| Gamma | 12 | (8): D138Y, K417T, L18F, P26S, R190S, T1027I, T20N, V1176F |
| Delta | 10 | (7): D960N, E156G, L452R, P681R, T19R, ΔF157, ΔR158 |
| Omicron | 37 | (26): A67V, D796Y, E484A, G339D, G446S, G496S, L212I, L981F, N440K, N679K, N764K, N856K, ins214EPE, N969K, Q493R, Q498R, Q954H, S371L, S373P, S375F, S477N, T547K, T95I, Y505H, ΔV143, ΔN211 |
| Measure | Discussion |
|---|---|
 Getting Vaccinated | Current vaccines are partially remaining effective in protecting people from becoming infected or severely ill. According to analyses, the widely administered vaccines, Pfizer BioNTech and Oxford-AstraZeneca, have 96% and 92% effectiveness in preventing hospitalization after taking two doses, respectively [42,45,91]. Thus, the improvement of the vaccination rate is the most reliable solution to stop the current Delta variant pandemic. |
 Wearing a mask |
|
 Practicing Social Distancing (1.5 m) |
|
 Avoiding overcrowded areas |
|
 Thoroughly washing hands often |
|
 Covering sneezes and coughs |
|
 Regularly Cleaning and Disinfecting |
|
 Monitoring health daily |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duong, B.V.; Larpruenrudee, P.; Fang, T.; Hossain, S.I.; Saha, S.C.; Gu, Y.; Islam, M.S. Is the SARS CoV-2 Omicron Variant Deadlier and More Transmissible Than Delta Variant? Int. J. Environ. Res. Public Health 2022, 19, 4586. https://doi.org/10.3390/ijerph19084586
Duong BV, Larpruenrudee P, Fang T, Hossain SI, Saha SC, Gu Y, Islam MS. Is the SARS CoV-2 Omicron Variant Deadlier and More Transmissible Than Delta Variant? International Journal of Environmental Research and Public Health. 2022; 19(8):4586. https://doi.org/10.3390/ijerph19084586
Chicago/Turabian StyleDuong, Bao V., Puchanee Larpruenrudee, Tianxin Fang, Sheikh I. Hossain, Suvash C. Saha, Yuantong Gu, and Mohammad S. Islam. 2022. "Is the SARS CoV-2 Omicron Variant Deadlier and More Transmissible Than Delta Variant?" International Journal of Environmental Research and Public Health 19, no. 8: 4586. https://doi.org/10.3390/ijerph19084586
APA StyleDuong, B. V., Larpruenrudee, P., Fang, T., Hossain, S. I., Saha, S. C., Gu, Y., & Islam, M. S. (2022). Is the SARS CoV-2 Omicron Variant Deadlier and More Transmissible Than Delta Variant? International Journal of Environmental Research and Public Health, 19(8), 4586. https://doi.org/10.3390/ijerph19084586










