The Prevalence of Adolescent Social Fears and Social Anxiety Disorder in School Contexts
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.2.1. Screening for Intense Social Fears
2.2.2. Diagnostic Assessment
2.2.3. Self-Reported Core Social Fears
2.3. Procedures
3. Results
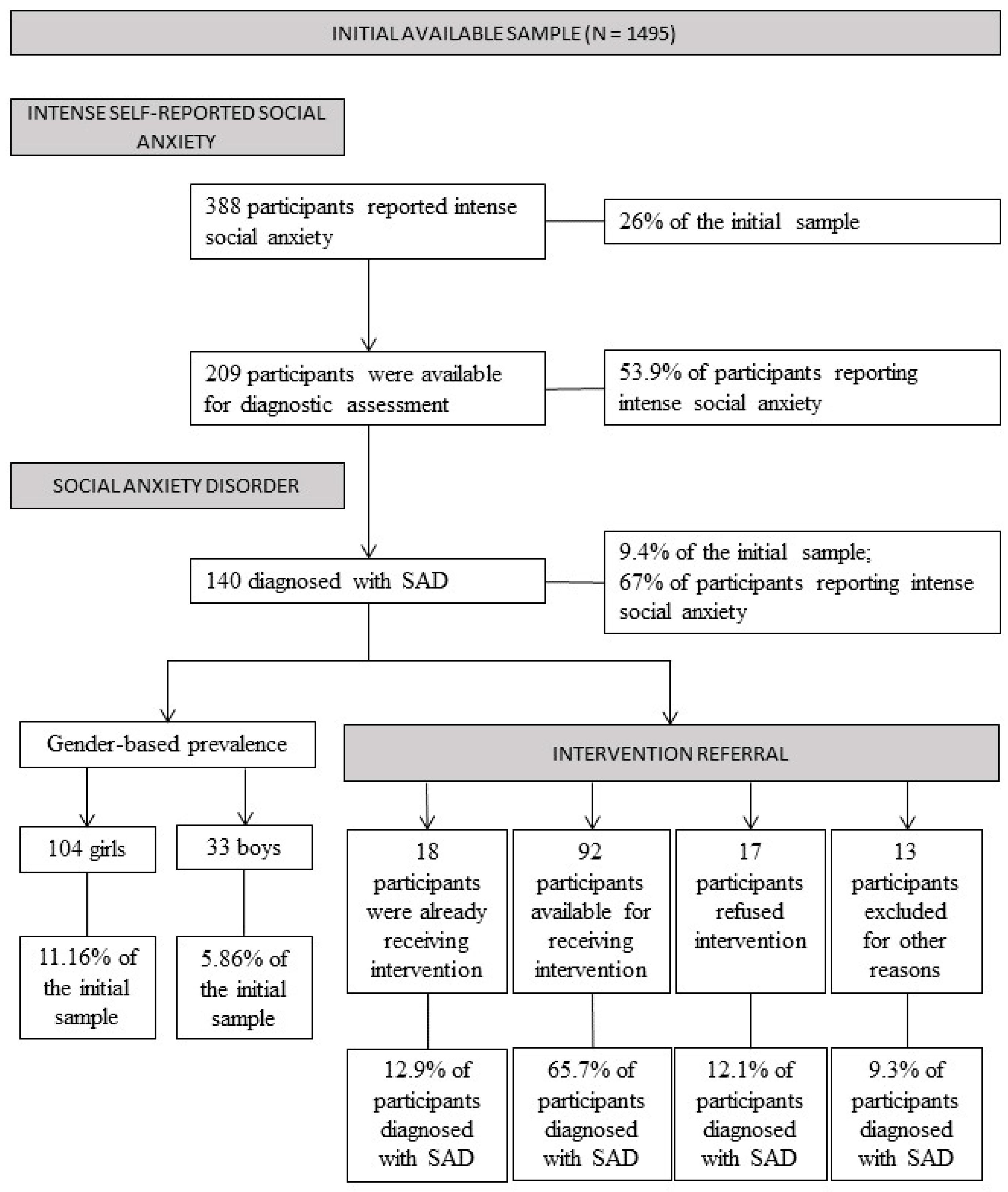
3.1. Prevalence of Intense Self-Reported Social Fears
3.2. Prevalence of Social Anxiety Disorder
3.3. Intervention Referral
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gilbert, P. Evolution and social anxiety: The Role of Attraction, Social Competition, and Social Hierarchies. Psychiatr. Clin. N. Am. 2001, 24, 723–751. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Jefferies, P.; Ungar, M. Social anxiety in young people: A prevalence study in seven countries. PLoS ONE 2020, 15, e0239133. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Lim, C.C.W.; Roest, A.M.; De Jonge, P.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Benjet, C.; Bromet, E.J.; Bruffaerts, R.; et al. The cross-national epidemiology of social anxiety disorder: Data from the World Mental Health Survey Initiative. BMC Med. 2017, 15, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Knappe, S.; Sasagawa, S.; Creswell, C. Developmental Epidemiology of Social Anxiety and Social Phobia in Adolescents. In Social Anxiety and Phobia in Adolescents; Springer: Cham, Switzerland, 2015; pp. 39–70. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Chavira, D.A.; Stein, M.B. Childhood Social Anxiety Disorder: From Understanding to Treatment. Child Adolesc. Psychiatr. Clin. N. Am. 2005, 14, 797–818. [Google Scholar] [CrossRef]
- Stein, M.B.; Kean, Y.M. Disability and Quality of Life in Social Phobia: Epidemiologic Findings. Am. J. Psychiatry 2000, 157, 1606–1613. [Google Scholar] [CrossRef]
- Bruce, S.E.; Yonkers, K.A.; Otto, M.; Eisen, J.L.; Weisberg, R.; Pagano, M.; Shea, M.T.; Keller, M.B. Influence of Psychiatric Comorbidity on Recovery and Recurrence in Generalized Anxiety Disorder, Social Phobia, and Panic Disorder: A 12-Year Prospective Study. Am. J. Psychiatry 2005, 162, 1179–1187. [Google Scholar] [CrossRef]
- Steinert, C.; Hofmann, M.; Leichsenring, F.; Kruse, J. What do we know today about the prospective long-term course of social anxiety disorder? A systematic literature review. J. Anxiety Disord. 2013, 27, 692–702. [Google Scholar] [CrossRef]
- Acquah, E.O.; Topalli, P.-Z.; Wilson, M.L.; Junttila, N.; Niemi, P.M. Adolescent loneliness and social anxiety as predictors of bullying victimisation. Int. J. Adolesc. Youth 2014, 21, 320–331. [Google Scholar] [CrossRef]
- Hebert, K.R.; Fales, J.; Nangle, D.W.; Papadakis, A.A.; Grover, R.L. Linking Social Anxiety and Adolescent Romantic Relationship Functioning: Indirect Effects and the Importance of Peers. J. Youth Adolesc. 2012, 42, 1708–1720. [Google Scholar] [CrossRef]
- Jystad, I.; Bjerkeset, O.; Haugan, T.; Sund, E.R.; Vaag, J. Sociodemographic Correlates and Mental Health Comorbidities in Adolescents with Social Anxiety: The Young-HUNT3 Study, Norway. Front. Psychol. 2021, 12, 663161. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, M.R.; Salehi, M.; Khaleghi, A.; Hooshyari, Z.; Mostafavi, S.A.; Ahmadi, N.; Hojjat, S.K.; Safavi, P.; Amanat, M. Social anxiety disorder among children and adolescents: A nationwide survey of prevalence, socio-demographic characteristics, risk factors and co-morbidities. J. Affect. Disord. 2019, 263, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Burstein, M.; He, J.-P.; Kattan, G.; Albano, A.M.; Avenevoli, S.; Merikangas, K.R. Social Phobia and Subtypes in the National Comorbidity Survey–Adolescent Supplement: Prevalence, Correlates, and Comorbidity. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 870–880. [Google Scholar] [CrossRef]
- Cunha, M. Ansiedade Social Na Adolescência: Avaliação e Trajectórias de Desenvolvimento; Universidade de Coimbra: Coimbra, Portugal, 2005. [Google Scholar]
- Kashdan, T.B.; Herbert, J.D. Social anxiety disorder in childhood and adolescence: Current status and future directions. Clin. Child Fam. Psychol. Rev. 2001, 4, 37–61. [Google Scholar] [CrossRef]
- Coles, M.E.; Ravid, A.; Gibb, B.; George-Denn, D.; Bronstein, L.R.; McLeod, S. Adolescent Mental Health Literacy: Young People’s Knowledge of Depression and Social Anxiety Disorder. J. Adolesc. Health 2016, 58, 57–62. [Google Scholar] [CrossRef]
- Anderson, K.N.; Jeon, A.B.; Blenner, J.A.; Wiener, R.L.; Hope, D.A. How people evaluate others with social anxiety disorder: A comparison to depression and general mental illness stigma. Am. J. Orthopsychiatry 2015, 85, 131–138. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, C.; Lynch, H.; Hennessy, E. Do stigma and level of social anxiety predict adolescents’ help-seeking intentions for social anxiety disorder? Early Interv. Psychiatry 2021, 16, 456–460. [Google Scholar] [CrossRef]
- Al-Modayfer, O.; Alatiq, Y. A pilot study on the prevalence of psychiatric disorders among Saudi children and adolescents: A sample from a selected community in Riyadh city. Arab. J. Psychiatry 2015, 26, 184–192. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Sheehan, K.H.; Shytle, R.D.; Janavs, J.; Bannon, Y.; Rogers, J.E.; Milo, K.M.; Stock, S.L.; Wilkinson, B. Reliability and Validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J. Clin. Psychiatry 2010, 71, 313–326. [Google Scholar] [CrossRef]
- Bener, A.; Ghuloum, S.; Dafeeah, E. Prevalence of common phobias and their socio-demographic correlates in children and adolescents in a traditional developing society. Afr. J. Psychiatry 2011, 14, 140–145. [Google Scholar] [CrossRef]
- Kessler, R.C.; Üstün, T.B. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int. J. Methods Psychiatr. Res. 2004, 13, 93–121. [Google Scholar] [CrossRef] [PubMed]
- Canals, J.; Voltas, N.; Hernández-Martínez, C.; Cosi, S.; Arija, V. Prevalence of DSM-5 anxiety disorders, comorbidity, and persistence of symptoms in Spanish early adolescents. Eur. Child Adolesc. Psychiatry 2018, 28, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Khetarpal, S.; Brent, D.; Cully, M.; Balach, L.; Kaufman, J.; Neer, S.M. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale Construction and Psychometric Characteristics. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 545–553. [Google Scholar] [CrossRef]
- Cunha, M.; Pinto-Gouveia, J.; Soares, I. Natureza, Frequência e Consequências Dos Medos Sociais Na Adolescência: Dados Na População Portuguesa. Psychologica 2007, 44, 207–236. [Google Scholar]
- La Greca, A.M.; Lopez, N. Social Anxiety among Adolescents: Linkages with Peer Relations and Friendships. J. Abnorm. Child Psychol. 1998, 26, 83–94. [Google Scholar] [CrossRef]
- Cunha, M.; Gouveia, J.P.; Salvador, M.D.C. Social Fears in Adolescence—The social anxiety and avoidance scale for adolescents. Eur. Psychol. 2008, 13, 197–213. [Google Scholar] [CrossRef]
- Farshidfar, Z.; Dastjerdi, R.; Mohammadi, M.R.; Alavi, S.; Ahmadi, A. Prevalence of Psychiatric Disorders in Children and Adolescents of South Khorasan Province in 2017. Mod. Care J. 2019, 16, e90937. [Google Scholar] [CrossRef]
- Ghanizadeh, A.; Mohammadi, M.R.; Yazdanshenas, A. Psychometric properties of the Farsi translation of the kiddie schedule for affective disorders and schizophrenia-present and lifetime version. BMC Psychiatry 2006, 6, 10. [Google Scholar] [CrossRef]
- Gren-Landell, M.; Tillfors, M.; Furmark, T.; Bohlin, G.; Andersson, G.; Svedin, C.G. Social phobia in Swedish adolescents. Soc. Psychiatry 2008, 44, 1. [Google Scholar] [CrossRef]
- Furmark, T.; Tillfors, M.; Everz, P.-O.; Marteinsdottir, I.; Gefvert, O.; Fredrikson, M. Social phobia in the general population: Prevalence and sociodemographic profile. Soc. Psychiatry 1999, 34, 416–424. [Google Scholar] [CrossRef]
- Iancu, I.; Levin, J.; Hermesh, H.; Dannon, P.; Poreh, A.; Ben-Yehuda, Y.; Kaplan, Z.; Marom, S.; Kotler, M. Social phobia symptoms: Prevalence, sociodemographic correlates, and overlap with specific phobia symptoms. Compr. Psychiatry 2006, 47, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Liebowitz, M.R. Social Phobia. Mod. Probl. Pharm. 1987, 22, 141–173. [Google Scholar] [CrossRef]
- Mattick, R.P.; Clarke, J.C. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav. Res. Ther. 1998, 36, 455–470. [Google Scholar] [CrossRef]
- Knappe, S.; Beesdo-Baum, K.; Fehm, L.; Stein, M.B.; Lieb, R.; Wittchen, H.-U. Social fear and social phobia types among community youth: Differential clinical features and vulnerability factors. J. Psychiatr. Res. 2011, 45, 111–120. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.-P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef]
- Millon, T. Millon Multiaxial Clinical Inventory Manual; National Computer Systems: Minneapolis, MN, USA, 1977. [Google Scholar]
- Ohayon, M.M.; Schatzberg, A.F. Social phobia and depression: Prevalence and comorbidity. J. Psychosom. Res. 2010, 68, 235–243. [Google Scholar] [CrossRef]
- Ohayon, M.M. Prevalence of DSM-IV diagnostic criteria of insomnia: Distinguishing insomnia related to mental disorders from sleep disorders. J. Psychiatr. Res. 1997, 31, 333–346. [Google Scholar] [CrossRef]
- Spence, S.H.; Zubrick, S.R.; Lawrence, D. A profile of social, separation and generalized anxiety disorders in an Australian nationally representative sample of children and adolescents: Prevalence, comorbidity and correlates. Aust. N. Z. J. Psychiatry 2017, 52, 446–460. [Google Scholar] [CrossRef]
- Shaffer, D.; Fisher, P.; Lucas, C.P.; Dulcan, M.K.; Schwab-Stone, M.E. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, Differences From Previous Versions, and Reliability of Some Common Diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 28–38. [Google Scholar] [CrossRef]
- Vicente, B.; Saldivia, S.; de la Barra, F.; Kohn, R.; Pihan, R.; Valdivia, M.; Rioseco, P.; Melipillan, R. Prevalence of child and adolescent mental disorders in Chile: A community epidemiological study. J. Child Psychol. Psychiatry 2012, 53, 1026–1035. [Google Scholar] [CrossRef]
- Yuvaraj, K.; Kumar, G.D.; Priyan, S.; Yamini, M.; Kumar, S.G.; Subitha, L. Prevalence and associated factors for social phobia among school-going adolescents in a rural area of Puducherry, South India. Int. J. Adolesc. Med. Health 2018, 33. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R.T.; Churchill, L.E.; Sherwood, A.; Weisler, R.H.; Foa, E.B. Psychometric properties of the Social Phobia Inventory (SPIN). Br. J. Psychiatry 2000, 176, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Wong, Q.J.; Chen, J.; Gregory, B.; Baillie, A.J.; Nagata, T.; Furukawa, T.; Kaiya, H.; Peters, L.; Rapee, R.M. Measurement equivalence of the Social Interaction Anxiety Scale (SIAS) and Social Phobia Scale (SPS) across individuals with social anxiety disorder from Japanese and Australian sociocultural contexts. J. Affect. Disord. 2018, 243, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Ng, K.L.; Kwok, K.P.; Tsang, A. Prevalence and correlates of social fears in Hong Kong. J. Anxiety Disord. 2009, 23, 327–332. [Google Scholar] [CrossRef]
- Asher, M.; Asnaani, A.; Aderka, I.M. Gender differences in social anxiety disorder: A review. Clin. Psychol. Rev. 2017, 56, 1–12. [Google Scholar] [CrossRef]
- Holbrook, J.R.; Bitsko, R.H.; Danielson, M.L.; Visser, S.N. Interpreting the Prevalence of Mental Disorders in Children: Tribulation and Triangulatio. Health Promot. Pract. 2016, 18, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Cunha, M.; Pinto-Gouveia, J.; Alegre, S.; Salvador, M.C. Avaliação Da Ansiedade Na Adolescência: A Versão Portuguesa Da SAS-A. Psychologica 2004, 35, 245–263. [Google Scholar]
- Rijo, D.; Brazão, N.; Barroso, R.; da Silva, D.R.; Vagos, P.; Vieira, A.; Lavado, A.; Macedo, A.M. Mental health problems in male young offenders in custodial versus community based-programs: Implications for juvenile justice interventions. Child Adolesc. Psychiatry Ment. Health 2016, 10, 1–12. [Google Scholar] [CrossRef]
- Vagos, P.; Pereira, A.; Cunha, M. Evaluating social fears in late adolescence: Study with a Portuguese sample. Eur. J. Dev. Psychol. 2013, 11, 373–385. [Google Scholar] [CrossRef]
- Vagos, P.; Figueiredo, D.V.; Cunha, M. Assessing Core Social Fears in Adolescence: The Core Social Fears Version of the Social Anxiety and Avoidance Scale for Adolescents. 2022; Manuscript in preparation. [Google Scholar]
- Filho, A.S.; Hetem, L.A.B.; Ferrari, M.C.F.; Trzesniak, C.; Martín-Santos, R.; Borduqui, T.; Osório, F.D.L.; Loureiro, S.R.; Filho, G.B.; Zuardi, A.W.; et al. Social anxiety disorder: What are we losing with the current diagnostic criteria? Acta Psychiatr. Scand. 2010, 121, 216–226. [Google Scholar] [CrossRef]
- Marinucci, A.; Grové, C.; Allen, K.-A.; Riebschleger, J. Evaluation of a youth mental health literacy and action program: Protocol for a cluster controlled trial. Ment. Health Prev. 2021, 24, 200216. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Ojio, Y.; Foo, J.C.; Michigami, E.; Usami, S.; Fuyama, T.; Onuma, K.; Oshima, N.; Ando, S.; Togo, F.; et al. A quasi-cluster randomized controlled trial of a classroom-based mental health literacy educational intervention to promote knowledge and help-seeking/helping behavior in adolescents. J. Adolesc. 2020, 82, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Poole, K.L.; Degnan, K.A.; Harrewijn, A.; Almas, A.; Fox, N.A.; Henderson, H.A. Trajectories of socially anxious behavior from age 5 to 13: Temperamental and sociocognitive pathways. Child Dev. 2022, 93, 1334–1346. [Google Scholar] [CrossRef]
- Miers, A.C.; Blöte, A.; De Rooij, M.; Bokhorst, C.L.; Westenberg, P.M. Trajectories of Social Anxiety during Adolescence and Relations with Cognition, Social Competence, and Temperament. J. Abnorm. Child Psychol. 2012, 41, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Morrissette, M. School Closures and Social Anxiety during the COVID-19 Pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2020, 60, 6–7. [Google Scholar] [CrossRef]
- Teo, A.R.; Lerrigo, R.; Rogers, M. The role of social isolation in social anxiety disorder: A systematic review and meta-analysis. J. Anxiety Disord. 2013, 27, 353–364. [Google Scholar] [CrossRef]
- Coyle, S.; Vagos, P.; Masia-Warner, C.; Silva, J.; Xavier, A.; Martin, G.; Wimmer, J.; Kalver, A.; Jeyanayagam, B.; Lekas, H.; et al. A Qualitative Study of Social Anxiety and Impairment amid the COVID-19 Pandemic for Adolescents and Young Adults in Portugal and the US. Eur. J. Educ. Psychol. 2022, in press. [Google Scholar]
- Fredrick, J.W.; Luebbe, A.M. Prospective Associations between Fears of Negative Evaluation, Fears of Positive Evaluation, and Social Anxiety Symptoms in Adolescence. Child Psychiatry Hum. Dev. 2022, 1–11. [Google Scholar] [CrossRef]
- Vilaplana-Pérez, A.; Pérez-Vigil, A.; Sidorchuk, A.; Brander, G.; Isomura, K.; Hesselmark, E.; Kuja-Halkola, R.; Larsson, H.; Mataix-Cols, D.; de la Cruz, L.F. Much more than just shyness: The impact of social anxiety disorder on educational performance across the lifespan. Psychol. Med. 2020, 51, 861–869. [Google Scholar] [CrossRef]
- Masia-Warner, C.; Klein, R.G.; Dent, H.C.; Fisher, P.H.; Alvir, J.; Albano, A.M.; Guardino, M. School-Based Intervention for Adolescents with Social Anxiety Disorder: Results of a Controlled Study. J. Abnorm. Child Psychol. 2005, 33, 707–722. [Google Scholar] [CrossRef]
- Olfson, M.; Guardino, M.; Struening, E.; Schneier, F.R.; Hellman, F.; Klein, D.F. Barriers to the Treatment of Social Anxiety. Am. J. Psychiatry 2000, 157, 521–527. [Google Scholar] [CrossRef]
- Kessler, R.C. The impairments caused by social phobia in the general population: Implications for intervention. Acta Psychiatr. Scand. 2003, 108, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Warner, C.M.; Fisher, P.H.; Shrout, P.E.; Rathor, S.; Klein, R.G. Treating adolescents with social anxiety disorder in school: An attention control trial. J. Child Psychol. Psychiatry 2007, 48, 676–686. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.L.; Warner, C.M. Treating Adolescents with Social Anxiety Disorder in Schools. Child Adolesc. Psychiatr. Clin. N. Am. 2012, 21, 105–118. [Google Scholar] [CrossRef]
- Mayo-Wilson, E.; Dias, S.; Mavranezouli, I.; Kew, K.; Clark, D.M.; Ades, A.E.; Pilling, S. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry 2014, 1, 368–376. [Google Scholar] [CrossRef]
- Leigh, E.; Clark, D.M. Cognitive Therapy for Social Anxiety Disorder in Adolescents: A Development Case Series. Behav. Cogn. Psychother. 2015, 44, 1–17. [Google Scholar] [CrossRef]
- Leigh, E.; Creswell, C.; Stallard, P.; Waite, P.; Violato, M.; Pearcey, S.; Brooks, E.; Taylor, L.; Warnock-Parkes, E.; Clark, D.M. Delivering cognitive therapy for adolescent social anxiety disorder in NHS CAMHS: A clinical and cost analysis. Behav. Cogn. Psychother. 2021, 49, 385–397. [Google Scholar] [CrossRef]
- Ganho-Ávila, A.; Figueiredo, D.V.; Vagos, P. Online Cognitive Therapy for Social Anxiety Disorder in Adolescence: A Clinical Case Study Using the CT@TeenSAD. Clin. Case Stud. 2022, 15346501221091519. [Google Scholar] [CrossRef]
- Alves, F.; Figueiredo, D.V.; Vagos, P. ACT for Social Anxiety Disorder in Adolescence: Preliminary Appraisal Based on a Case Study Approach. 2022; Manuscript submitted for publication. [Google Scholar]

| Study | Country | Age | Diagnosis Method | Prevalence | Prevalence by Gender |
|---|---|---|---|---|---|
| [21] | Saudi Arabia | 11–17 | MINI-KID [22] (structured interview of DSM-IV diagnoses) | 4.6% (time-point) | NR |
| [23] | Qatar | 6–18 | Systematic review of the symptoms performed by psychiatrists | 12.7% (time-point) | Females (21.9%) had higher rates of all phobic disorders than males (16.8%) |
| [15] | United States | 13–18 | CIDI [24] (structured interview of DSM-IV diagnoses) | 8.6% (lifetime) | Female (9.2%) Male (7.9%) |
| [25] | Spain | 8–12 | SCARED [26] (cut-off point for detecting anxiety disorders symptoms was 25); MINI-KID [22] (structured interview of DSM-IV diagnoses) | 3.4% (time-point) | Female (5.5%) Male (2.4%) |
| [27] | Portugal | 12–18 | SAS-A [28] (the higher the score, the higher the level of measured anxiety); SAASA [29] (the higher the score, the higher the level of measured anxiety) | 3.6% (time-point) | Significant differences were found between girls and boys in all SA indices, with girls reporting higher values. Regarding the number of social fears, 59.4% females reported one or more, while 43.9% of boys reported one or more. |
| [30] | Iran | 6–18 | K-SADS-PL [31] (semi-structured diagnostic interview of DSM-IV diagnoses) | 0.8% (time-point) | NR |
| [32] | Sweden | 12–14 | SPSQ-C [33] (rate at least one potentially phobic situation as marked fear on the social fear scale and it had to be consistently endorsed in the diagnostic questions covering SAD criteria) | 4.4% (time-point) | Females (6.6%) Males (1.8%) |
| [34] | Israel | 18–25 | LSAS [35] (fear was defined if at least one of the three questions was endorsed) | 4.5% (time-point) | NR |
| [3] | Brazil China Indonesia Russia Thailand United States Vietnam | 16–29 | SIAS [36] (cut-off point for detecting SAD was 29) | 36% (time-point) | Male (35.6%) Female (36.5%) NS |
| [37] | United States | 14–24 | CIDI [24] (structured interview of DSM-IV diagnoses) | 6.6% (time-period) | NR |
| [38] | United States | 13–18 | CIDI [24] (structured interview of DSM-IV diagnoses) | 9.1% (lifetime) | Females (12.2%) Males (7%) |
| [14] | Iran | 6–18 | K-SADS-PL [31] (semi-structure psychiatric interview based on DSM-IV); MCMI-III [39] (self-administrated psychological instrument) | 1.8% (lifetime) | NR |
| [40] | United Kingdom Germany Italy Portugal Spain | 15–101 (exception of Portugal, where the minimum age was set at 18) | Sleep-EVAL Expert System [41] (software with standard questionnaire and diagnostic pathways covering the DSM-IV) | 4.4% (time-point) | Female (5.4%) Male (3.4%) |
| [42] | Australia | 4–17 | DISC-IV [43] (criteria for impairment required either severe impairment in one or more functional domains or at least moderate impairment in two or more domains) | 2.3% (time-period) | Male (2.4%) Female (2.2%) NS |
| [44] | Chile | 4–18 | DISC-IV [43] (criteria for impairment required at least two intermediate or one severe criteria) for 4–11 years old; 12–18 years old were directly interviewed | Total = 3.7% 4–11 = 3.5% 12–18 = 3.9% (time-point) | Male (1.8%) Female (5.7%) |
| [45] | South India | 10–16 | SPIN [46] (a score less than 20 was considered normal, scores 21–30 as mild, 31–40 as moderate, 41–50 as severe, and more than 51 as a very severe social phobia) | 22.9% (time-point) | Male (15.2%) Female (30.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alves, F.; Figueiredo, D.V.; Vagos, P. The Prevalence of Adolescent Social Fears and Social Anxiety Disorder in School Contexts. Int. J. Environ. Res. Public Health 2022, 19, 12458. https://doi.org/10.3390/ijerph191912458
Alves F, Figueiredo DV, Vagos P. The Prevalence of Adolescent Social Fears and Social Anxiety Disorder in School Contexts. International Journal of Environmental Research and Public Health. 2022; 19(19):12458. https://doi.org/10.3390/ijerph191912458
Chicago/Turabian StyleAlves, Francisca, Diana Vieira Figueiredo, and Paula Vagos. 2022. "The Prevalence of Adolescent Social Fears and Social Anxiety Disorder in School Contexts" International Journal of Environmental Research and Public Health 19, no. 19: 12458. https://doi.org/10.3390/ijerph191912458
APA StyleAlves, F., Figueiredo, D. V., & Vagos, P. (2022). The Prevalence of Adolescent Social Fears and Social Anxiety Disorder in School Contexts. International Journal of Environmental Research and Public Health, 19(19), 12458. https://doi.org/10.3390/ijerph191912458







