The Effect of Daily Practice of Puzzle-Game Apps on Cognition in Two Groups of Older Adults: A Pre-Post Experimental Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population
2.3. Tools
2.3.1. Tools to Describe the Population
2.3.2. Outcome Measures
2.3.3. The TECH Intervention
2.4. Procedure
2.5. Data Analysis
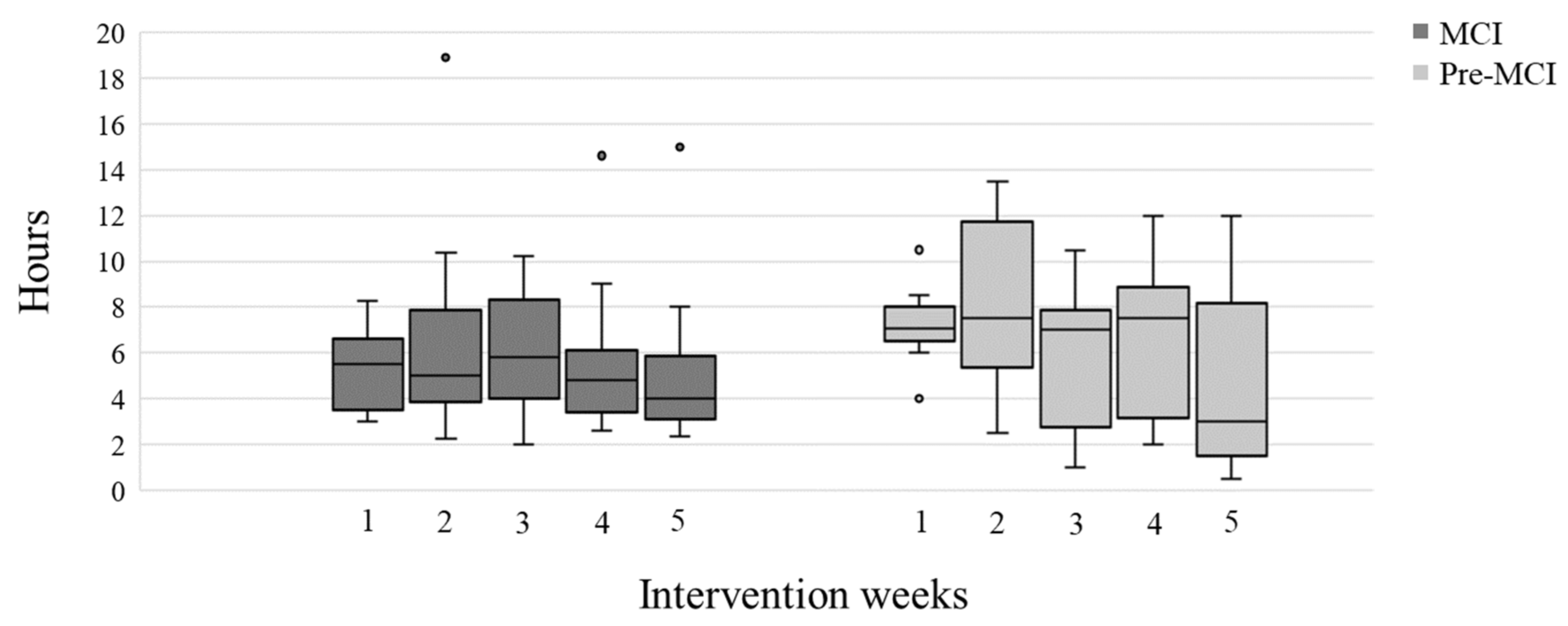
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Decade of Healthy Ageing: Baseline Report 2020. Available online: https://apps.who.int/iris/handle/10665/338677 (accessed on 14 September 2022).
- Park, D.C.; Reuter-Lorenz, P. The adaptive brain: Aging and neurocognitive scaffolding. Annu. Rev. Psychol. 2009, 60, 173–196. [Google Scholar] [CrossRef] [Green Version]
- Gatz, M. Genetics, dementia, and the elderly. Curr. Dir. Psychol. Sci. 2007, 16, 123–127. [Google Scholar] [CrossRef]
- Rotenberg, S.; Dawson, D.R. Characterizing Cognition in Everyday Life of Older Adults With Subjective Cognitive Decline. OTJR 2022, 42, 269–276. [Google Scholar] [CrossRef]
- Anderson, N.D. State of the science on mild cognitive impairment (MCI). CNS Spectr. 2019, 24, 78–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reisberg, B.; Ferris, S.; De Leon, M.J.; Torossian, C.; Kadiyala, S.; Zhu, W. Subjective Cognitive Impairment: The pre-Mild Cognitive Impairment stage of brain degeneration-Longitudinal outcome after a mean of 7 years follow-up. Neuropsychopharmacology 2005, 30, S81. [Google Scholar]
- Reisberg, B.; Gauthier, S. Current evidence for subjective cognitive impairment (SCI) as the pre-mild cognitive impairment (MCI) stage of subsequently manifest Alzheimer’s disease. Int. Psychogeriatr. 2008, 20, 1–16. [Google Scholar] [CrossRef]
- Reid, L.M.; Maclullich, A.M. Subjective memory complaints and cognitive impairment in older people. Dement. Geriatr. Cogn. Disord. 2006, 22, 471–485. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.W.; Plassman, B.L.; Burke, J.; Benjamin, S. Preventing Alzheimer’s disease and cognitive decline. Evid. Rep. Technol. Assess. 2010, 193, 1–727. [Google Scholar]
- Kueider, A.M.; Parisi, J.M.; Gross, A.L.; Rebok, G.W. Computerized cognitive training with older adults: A systematic review. PLoS ONE 2012, 7, e40588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tetlow, A.M.; Edwards, J.D. Systematic literature review and meta-analysis of commercially available computerized cognitive training among older adults. J. Cogn. Enhanc. 2017, 1, 559–575. [Google Scholar] [CrossRef]
- Ge, S.; Zhu, Z.; Wu, B.; McConnell, E.S. Technology-based cognitive training and rehabilitation interventions for individuals with mild cognitive impairment: A systematic review. BMC Geriatr. 2018, 18, 213. [Google Scholar] [CrossRef] [Green Version]
- Hill, N.T.; Mowszowski, L.; Naismith, S.L.; Chadwick, V.L.; Valenzuela, M.; Lampit, A. Computerized Cognitive Training in Older Adults With Mild Cognitive Impairment or Dementia: A Systematic Review and Meta-Analysis. Am. J. Psychiatry 2017, 174, 329–340. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Huntley, J.; Bhome, R.; Holmes, B.; Cahill, J.; Gould, R.L.; Wang, H.; Yu, X.; Howard, R. Effect of computerised cognitive training on cognitive outcomes in mild cognitive impairment: A systematic review and meta-analysis. BMJ Open 2019, 9, e027062. [Google Scholar] [CrossRef] [Green Version]
- Lampit, A.; Gavelin, H.M.; Sabates, J.; Launder, N.H.; Hallock, H.; Finke, C.; Krohn, S.; Peeters, G. Computerized cognitive training in cognitively healthy older adults: A systematic review and network meta-analysis. MedRxiv 2020. [Google Scholar] [CrossRef]
- Verghese, J.; Lipton, R.B.; Katz, M.J.; Hall, C.B.; Derby, C.A.; Kuslansky, G.; Ambrose, A.F.; Sliwinski, M.; Buschke, H. Leisure activities and the risk of dementia in the elderly. N. Engl. J. Med. 2003, 19, 2508–2516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yates, L.A.; Ziser, S.; Spector, A.; Orrell, M. Cognitive leisure activities and future risk of cognitive impairment and dementia: Systematic review and meta-analysis. Int. Psychogeriatr. 2016, 28, 1791–1806. [Google Scholar] [CrossRef]
- Schaham, N.G.; Vitek, H.; Donda, N.; Golan, I.E.; Buckman, Z.; Rand, D. The Development and Feasibility of TECH: Tablet Enhancement of Cognition and Health, a Novel Cognitive Intervention for People with Mild Cognitive Impairment. Games Health J. 2020, 9, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1983, 17, 37–49. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Silverstein, S.M.; Berten, S.; Olson, P.; Paul, R.; Williams, L.M.; Cooper, N.; Gordon, E. Development and validation of a World-Wide-Web-based neurocognitive assessment battery: WebNeuro. Behav. Res. Methods 2007, 39, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Lenhard, W.; Lenhard, A. Computation of Effect Sizes 2016. Available online: https://www.psychometrica.de/effect_size.html (accessed on 14 September 2022).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of health status: Ascertaining the minimal clinically important difference. Control. Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Hung, S.-J.; Lin, K.-C.; Chen, K.-H.; Chen, P.; Tsay, P.-K. Responsiveness, minimal clinically important difference, and validity of the MoCA in stroke rehabilitation. Occup. Ther. Int. 2019, 2019, 2517658. [Google Scholar] [CrossRef] [PubMed]
- Djabelkhir, L.; Wu, Y.-H.; Vidal, J.-S.; Cristancho-Lacroix, V.; Marlats, F.; Lenoir, H.; Carno, A.; Rigaud, A.-S. Computerized cognitive stimulation and engagement programs in older adults with mild cognitive impairment: Comparing feasibility, acceptability, and cognitive and psychosocial effects. Clin. Interv. Aging 2017, 12, 1967–1975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitbourne, S.K.; Ellenberg, S.; Akimoto, K. Reasons for playing casual video games and perceived benefits among adults 18 to 80 years old. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 892–897. [Google Scholar] [CrossRef]
- Kizony, R.; Zeilig, G.; Dudkiewicz, I.; Schejter-Margalit, T.; Rand, D. Tablet Apps and Dexterity: Comparison between 3 Age Groups and Proof of Concept for Stroke Rehabilitation. J. Neurol. Phys. Ther. 2016, 40, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Ramprasad, C.; Tamariz, L.; Garcia-Barcena, J.; Nemeth, Z.; Palacio, A. The Use of Tablet Technology by Older Adults in Health Care Settings-Is It Effective and Satisfying? A Systematic Review and Meta Analysis. Clin. Gerontol. 2019, 42, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Vaportzis, E.; Giatsi Clausen, M.; Gow, A.J. Older Adults Experiences of Learning to Use Tablet Computers: A Mixed Methods Study. Front. Psychol. 2018, 9, 1631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Button, K.S.; Ioannidis, J.P.A.; Mokrysz, C.; Nosek, B.A.; Flint, J.; Robinson, E.S.J.; Munafò, M.R. Power failure: Why small sample size undermines the reliability of neuroscience. Nat. Rev. Neurosci. 2013, 14, 365–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, D.C.; Lodi-Smith, J.; Drew, L.; Haber, S.; Hebrank, A.; Bischof, G.N.; Aamodt, W. The impact of sustained engagement on cognitive function in older adults: The Synapse Project. Psychol. Sci. 2014, 25, 103–112. [Google Scholar] [CrossRef] [Green Version]
- Chan, M.Y.; Haber, S.; Drew, L.M.; Park, D.C. Training older adults to use tablet computers: Does it enhance cognitive function? Gerontologist 2016, 56, 475–484. [Google Scholar] [CrossRef]
| MCI (N = 30) | Pre-MCI (N = 10) | Independent Samples t-Test | ||
|---|---|---|---|---|
| Mean ± SD Min-Max | Mean (SD) Min-Max | t (p) | ||
| Age (years) | 76.3 WQ± 5.3 65–87 | 72.4 ± 6.9 65–86 | 1.8 (0.07) | |
| Education (years) | 13.6 ± 4.1 8–30 | 16.3 ± 2.5 12–20 | −1.9 (0.06) | |
| MoCA (0–30) | 22.7 ± 1.9 19–25 | 27.3 ± 0.9 26–29 | −7.4 (<0.001) | |
| GSES (10–40) | 33.6 ± 4.5 19–39 | 31.2 ± 6.5 19–38 | 1.2 (0.2) | |
| IADL Questionnaire (0–23) | 21.8 ± 2.9 8–23 | 23.1 ± 0.3 23–24 | −1.3 (0.2) | |
| N (%) | N (%) | χ2 (p) | ||
| Sex | Female | 13 (46.4) | 5 (50) | 0.04 (0.85) |
| Male | 15 (53.6) | 5 (50) | ||
| Residence | Alone | 5 (17.9) | 4 (40) | 5.3 (0.07) |
| With family | 23 (82.1) | 6 (60) | ||
| Main occupation | Working | 6 (21.4) | 3 (30) | 0.3 (0.6) |
| Retired | 22 (78.6) | 7 (70) | ||
| Drive | Yes | 23 (82.1) | 10 (100) | 2.0 (0.1) |
| Computer use | Yes | 23 (82.1) | 10 (100) | 5.1 (0.2) |
| Smartphone use | Yes | 24 (85.7) | 10 (100) | 1.6 (0.2) |
| Tablet use | Yes | 6 (21.4) | 7 (70) | 7.7 (0.005) |
| MCI (N = 23) | Pre-MCI (N = 10) | |
|---|---|---|
| % | % | |
| General satisfaction from TECH | ||
| Very Satisfied | 47.8 | 60.0 |
| Satisfied | 30.4 | 30.0 |
| Neutral | 21.7 | 10.0 |
| Satisfaction from the group sessions | ||
| Very Satisfied | 28.6 | 70.0 |
| Satisfied | 50.0 | 30.0 |
| Neutral | 13.6 | |
| Enjoyment from the group sessions | ||
| Enjoyed very much | 50 | 50.0 |
| Enjoyed | 31.8 | 30.0 |
| So-so | 18.2 | 20.0 |
| Satisfaction from self-training at home | ||
| Very Satisfied | 52.2 | 60.0 |
| Satisfied | 34.8 | 30.0 |
| Neutral | 13.0 | 10.0 |
| Satisfaction from persisting to self-train over-time | ||
| Very Satisfied | 17.4 | 30.0 |
| Satisfied | 47.8 | 40.0 |
| Neutral | 30.4 | 20.0 |
| Slightly Satisfied | 4.3 | 10.0 |
| Motivation from the self-training | ||
| Very motivated | 39.1 | 30.0 |
| Motivated | 47.8 | 40.0 |
| Neutral | 13.0 | 30.0 |
| Satisfaction from the cognitive demands | ||
| Very Satisfied | 39.1 | 50.0 |
| Satisfied | 43.5 | 50.0 |
| Neutral | 13.0 | |
| Slightly Satisfied | 4.3 | |
| Perceived improvement following TECH | ||
| Substantial improvement | 13.0 | 11.1 |
| Some improvement | 30.4 | 33.3 |
| Neutral | 39.1 | 22.2 |
| Very little improvement | 8.7 | 22.2 |
| Not at all | 8.7 | 11.1 |
| The demand for daily training | ||
| Too short | 26.1 | 22.2 |
| Just right | 47.8 | 55.6 |
| Too long | 26.1 | 22.2 |
| Duration of the program | ||
| Too short | 69.6 | 50.0 |
| Just Right | 26.1 | 50.0 |
| Too long | 4.3 | |
| Will you continue to practice following TECH? | ||
| Yes | 86.4 | 85.7 |
| No | 13.6 | 14.3 |
| (a) | |||||
|---|---|---|---|---|---|
| MCI (N = 25) | |||||
| Pre | Post | % Change Pre-Post | Differences Between Pre-Post | ||
| Median IQR | Median IQR | Median IQR | Z(p) | ||
| MoCA (0–30) | 23.0 21.0–24.0 | 23.0 21.5–25.0 | 4.2 −4.2–11.3 | −1.2 (0.2) | |
| WebNeuro Computerized Cognitive Battery | Sustained Attention | −0.6 −1.0–(−0.1) | −0.5 −0.9–0.2 | −35.2 −109.1–61.4 | −0.2 (0.8) |
| Controlled Attention | −1.2 −1.7–(−0.6) | −1.1 −1.5–(−0.9) | 9.0 −21.6–66.1 | −1.1 (0.3) | |
| Flexibility | −1.2 −1.9–(−0.5) | −1.2 −1.9–(−0.7) | −0.1 −42.6–20.5 | −0.4 (0.7) | |
| Inhibition | −0.3 −0.8−0.2 | 0.0 −0.6–0.4 | −53.1 −157.3–85.3 | −0.7 (0.4) | |
| Working Memory | −1.4 −1.9–(−0.8) | −1.1 −1.8–(−0.8) | −14.9 −51.6–21.9 | −1.3 (0.2) | |
| Memory Recall | −0.9 −1.8–0.1 | −1.2 −2.2–(−0.3) | 1.9 −84.1–126.6 | −2.7 (0.006) | |
| Problem solving | 0.2 −0.3–0.6 | 0.5 −0.2–0.8 | −12.9 −148.1–66.0 | −0.5 (0.6) | |
| Total Thinking Score | −0.6 −1.1–(−0.3) | −0.7 −0.9–(−0.3) | 0.5 −38.8–41.3 | −0.3 (0.8) | |
| (b) | |||||
| Pre-MCI (N = 10) | |||||
| Pre | Post | % Change Pre-Post | Differences Between Pre-Post | ||
| Median IQR | Median IQR | Median IQR | Z(p) | ||
| MoCA (0–30) | 27.0 26.75–28.0 | 28.0 26.0–29.0 | 1.7 −5.5–4.6 | −0.3 (0.8) | |
| WebNeuro Computerized Cognitive Battery | Sustained Attention | −0.04 −0.5–0.6 | 0.1 −0.3–0.4 | −19.0 −88.3–143.3 | −0.8 (0.4) |
| Controlled Attention | −0.5 −1.1–(−0.3) | -0.05 −0.9–(−0.1) | −23.6 −59.8–77.5 | −1.1 (0.2) | |
| Flexibility | −0.2 −0.9–0.7 | −0.3 −1.9–0.8 | 10.5 −16.3–113.5 | −0.2 (0.8) | |
| Inhibition | 0.2 −0.3–0.5 | 0.2 −0.7–0.6 | 0.0 −16.7–159.0 | −0.3 (0.7) | |
| Working Memory | −1.1 −1.9–0.2 | −1.2 −1.8–(−0.6) | 6.0 −26.3–22.0 | −0.9 (0.4) | |
| Memory Recall | 0.1 −0.5–0.6 | −0.0 −0.8–0.6 | −6.4 −124.3–161.7 | −1.0 (0.3) | |
| Problem solving | 0.1 −0.2–0.6 | 0.6 −0.1–0.8 | −0.8 −261.1–335.7 | −1.8 (0.06) | |
| Total Thinking Score | −3 −0.4–0.1 | −0.2 −0.5–0.3 | 23.2 −25.6–106.8 | −0.6 (0.5) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Givon Schaham, N.; Buckman, Z.; Rand, D. The Effect of Daily Practice of Puzzle-Game Apps on Cognition in Two Groups of Older Adults: A Pre-Post Experimental Study. Int. J. Environ. Res. Public Health 2022, 19, 15454. https://doi.org/10.3390/ijerph192315454
Givon Schaham N, Buckman Z, Rand D. The Effect of Daily Practice of Puzzle-Game Apps on Cognition in Two Groups of Older Adults: A Pre-Post Experimental Study. International Journal of Environmental Research and Public Health. 2022; 19(23):15454. https://doi.org/10.3390/ijerph192315454
Chicago/Turabian StyleGivon Schaham, Noa, Zvi Buckman, and Debbie Rand. 2022. "The Effect of Daily Practice of Puzzle-Game Apps on Cognition in Two Groups of Older Adults: A Pre-Post Experimental Study" International Journal of Environmental Research and Public Health 19, no. 23: 15454. https://doi.org/10.3390/ijerph192315454
APA StyleGivon Schaham, N., Buckman, Z., & Rand, D. (2022). The Effect of Daily Practice of Puzzle-Game Apps on Cognition in Two Groups of Older Adults: A Pre-Post Experimental Study. International Journal of Environmental Research and Public Health, 19(23), 15454. https://doi.org/10.3390/ijerph192315454






