Contextual Factors Associated with Abuse of Home-Dwelling Persons with Dementia: A Cross-Sectional Exploratory Study of Informal Caregivers
Abstract
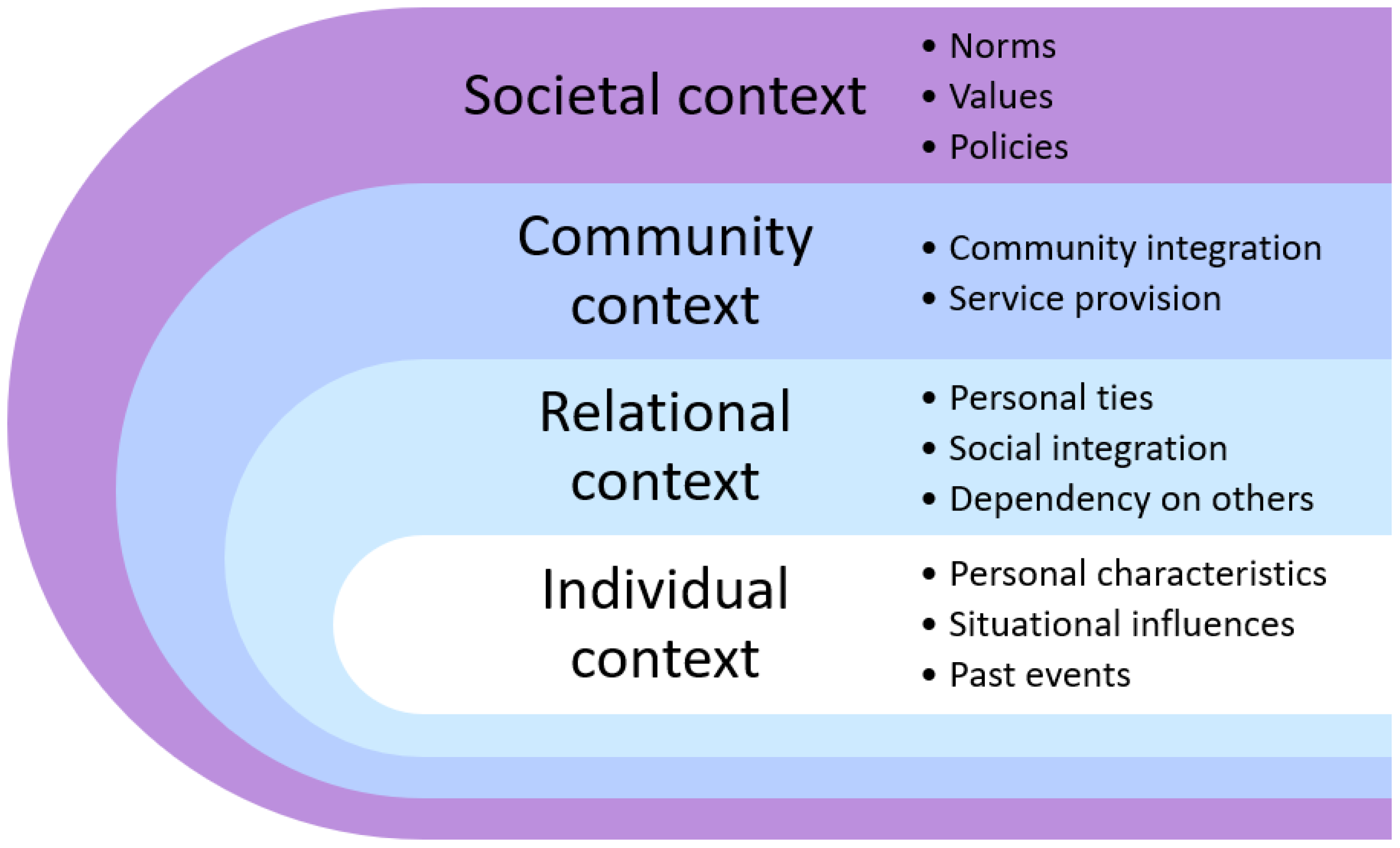
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Participants and Data Collection
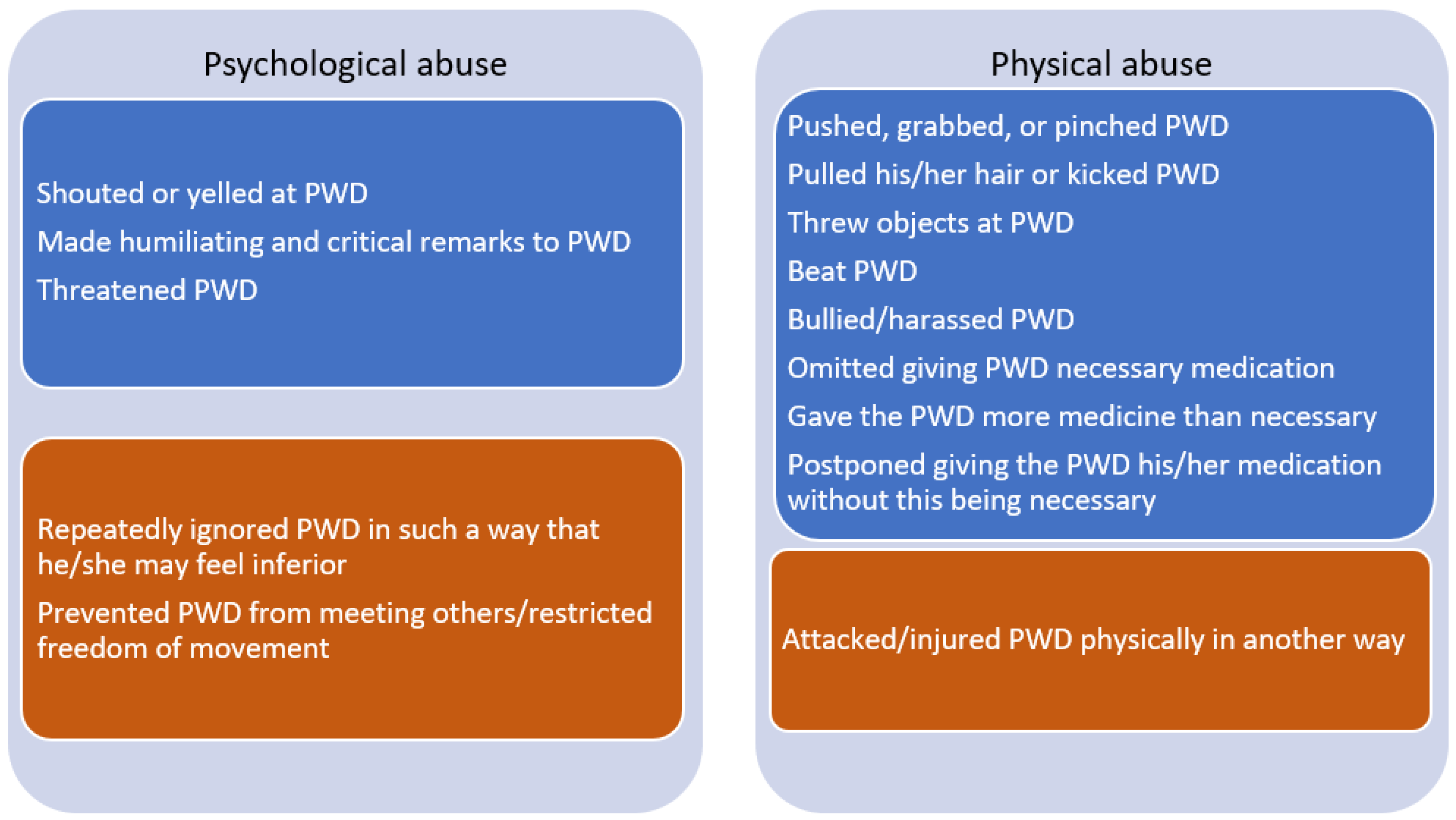
2.3. Measurements
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Individual Context
4.2. Relational Context
4.3. Community Context
4.4. Societal Context
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. The Toronto Declaration on the Global Prevention of Elder Abuse; World Health Organization: Geneve, Switzerland, 2002.
- Yunus, R.M.; Hairi, N.N.; Choo, W.Y. Consequences of Elder Abuse and Neglect: A Systematic Review of Observational Studies. Trauma Violence Abus. 2019, 20, 197–213. [Google Scholar] [CrossRef]
- Yon, Y.; Mikton, C.R.; Gassoumis, Z.D.; Wilber, K.H. Elder abuse prevalence in community settings: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e147–e156. [Google Scholar] [CrossRef] [PubMed]
- WHO. Infographic on Elder Abuse; World Health Organization: Geneve, Switzerland, 2016.
- Gjøra, L.; Strand, B.H.; Bergh, S.; Borza, T.; Brækhus, A.; Engedal, K.; Johannessen, A.; Kvello-Alme, M.; Krokstad, S.; Livingston, G.; et al. Current and future prevalence estimates of mild cognitive impairment, dementia, and its subtypes in a population-based sample of people 70 years and older in Norway: The HUNT Study. J. Alzheimers Dis. 2021, 79, 1213–1226. [Google Scholar] [CrossRef] [PubMed]
- Marshall, K.; Herbst, J.; Girod, C.; Annor, F. Do interventions to prevent or stop abuse and neglect among older adults work? A systematic review of reviews. J. Elder Abus. Negl. 2020, 32, 409–433. [Google Scholar] [CrossRef]
- Roberto, K.; Teaster, P. Theorizing Elder Abuse. In Elder Abuse: Research, Practice ans Policy; Dong, X., Ed.; Springer: Cham, Switzerland, 2017; pp. 21–41. [Google Scholar]
- Kim, T.; Jeong, H.; Won Han, J.; Kwak, K.P.; Kim, B.J.; Kim, S.K.; Kim, J.L.; Kim, T.H.; Ryu, S.H.; Moon, S.W.; et al. Prevalence and risk factors of abusive behaviors in the caregivers of people with dementia in Korea. Psychiatry Investig. 2018, 15, 677–686. [Google Scholar] [CrossRef]
- Kishimoto, Y.; Terada, S.; Takeda, N.; Oshima, E.; Honda, H.; Yoshida, H.; Yokota, O.; Uchitomi, Y. Abuse of people with cognitive impairment by family caregivers in Japan (a cross-sectional study). Psychiatry Res. 2013, 209, 699–704. [Google Scholar] [CrossRef]
- Wiglesworth, A.; Mosqueda, L.; Mulnard, R.; Liao, S.; Gibbs, L.; Fitzgerald, W. Screening for abuse and neglect of people with dementia. J. Am. Geriatr. Soc. 2010, 58, 493–500. [Google Scholar] [CrossRef]
- Yan, E. Abuse of older persons with dementia by family caregivers: Results of a 6-month prospective study in Hong Kong. Int. J. Geriatr. Psychiatry 2014, 29, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- VandeWeerd, C.; Paveza, G.J. Verbal mistreatment in older adults: A look at persons with Alzheimer’s disease and their caregivers in the State of Florida. J. Elder Abus. Negl. 2005, 17, 11–30. [Google Scholar] [CrossRef]
- VandeWeerd, C.; Paveza, G.J.; Walsh, M.; Corvin, J. Physical mistreatment in persons with Alzheimer’s disease. J. Aging Res. 2013, 2013, 920324. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Sun, H.; Zhang, J.; Ruan, J. Prevalence and associated factors of elder abuse in family caregivers of older people with dementia in central China cross-sectional study. Int. J. Geriatr. Psychiatry 2019, 34, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Blanchard, M.; Selwood, A.; Walker, Z.; Livingston, G. Family carers’ distress and abusive behaviour: Longitudinal study. Br. J. Psychiatry 2010, 196, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Yan, E.; Kwok, T. Abuse of older Chinese with dementia by family caregivers: An inquiry into the role of caregiver burden. Int. J. Geriatr. Psychiatry 2011, 26, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Krug, E.G.; Dahlberg, L.L.; Mercy, J.A.; Zwi, A.B.; Lozano, R. World Report on Violence and Health; World Health Organization: Geneva, Switzerland, 2002.
- WHO. Tackling Abuse of Older People: Five Priorities for the United Nations Decade of Healthy Ageing (2021–2030); World Health Organization: Geneva, Switzerland, 2022.
- Johannesen, M.; LoGiudice, D. Elder abuse: A systematic review of risk factors in community-dwelling elders. Age Ageing 2013, 42, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Steinsheim, G. Stretched to the Limit?—The Role Caregiver Burden has on the Extent of Elder Abuse among Home-Dwelling Persons with Dementia (OSF Preregistration). Available online: https://osf.io/9f6sm (accessed on 21 December 2022).
- Steinsheim, G.; Saga, S.; Olsen, B.; Broen, H.K.; Malmedal, W. Abusive episodes among home-dwelling persons with dementia and their informal caregivers: A cross-sectional Norwegian study. BMC Geriatr. 2022, 22, 852. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Prev. Med. 2007, 45, 247–251. [Google Scholar] [CrossRef]
- OECD/European Observatory on Health Systems and Policies. Norway: Country Health Profile 2021, State of Health in the EU; OECD Publishing, European Observatory on Health Systems and Policies: Paris, France; Brussels, Belgium, 2021. [Google Scholar]
- Vislapuu, M.; Angeles, R.C.; Berge, L.I.; Kjerstad, E.; Gedde, M.H.; Husebo, B.S. The consequences of COVID-19 lockdown for formal and informal resource utilization among home-dwelling people with dementia: Results from the prospective PAN. DEM study. BMC Health Serv. Res. 2021, 21, 1–12. [Google Scholar] [CrossRef]
- Gedde, M.H.; Husebo, B.S.; Vahia, I.V.; Mannseth, J.; Vislapuu, M.; Naik, M.; Berge, L.I. Impact of COVID-19 restrictions on behavioural and psychological symptoms in home-dwelling people with dementia: A prospective cohort study (PAN.DEM). BMJ Open 2022, 12, e050628. [Google Scholar] [CrossRef]
- Vossius, C.; Selbæk, G.; Ydstebø, A.; Benth, J.; Godager, G.; Lurås, H.; Bergh, S. Ressursbruk og Sykdomsforløp ved Demens (REDIC) [Resource use and Disease Course in Dementia]; Alderspsykiatrisk forskningssenter Sykehuset Innlandet: Ottestad, Norway, 2015. [Google Scholar]
- Ringard, Å.; Sagan, A.; Sperre Saunes, I.; Lindahl, A.K. Norway: Health System Review; World Health Organization. Regional Office for Europe: Copenhagen, Denmark, 2013.
- Skinner, M.S.; Sogstad, M.K.R.; Tingvold, L. Voluntary work in the Norwegian long-term care sector: Complementing or substituting formal services? Eur. J. Soc. Work. 2019, 22, 999–1011. [Google Scholar] [CrossRef]
- Botngård, A.; Eide, A.H.; Mosqueda, L.; Malmedal, W. Elder abuse in Norwegian nursing homes: A cross-sectional exploratory study. BMC Health Serv. Res. 2020, 20, 9. [Google Scholar] [CrossRef]
- Sandmoe, A.; Wentzel-Larsen, T.; Hjemdal, O.K. Violence and Abuse against Elderly People in Norway: A National Prevalence Study; Norwegian Centre for Violence and Traumatic Stress: Oslo, Norway, 2017. [Google Scholar]
- Pillemer, K.; Finkelhor, D. The prevalence of elder abuse: A random sample survey. Gerontologist 1988, 28, 51–57. [Google Scholar] [CrossRef]
- Straus, M.A.; Hamby, S.L.; Boney-McCoy, S.U.E.; Sugarman, D.B. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. J. Fam. Issues 1996, 17, 283–316. [Google Scholar] [CrossRef]
- Botngård, A.; Eide, A.H.; Mosqueda, L.; Malmedal, W. Resident-to-resident aggression in Norwegian nursing homes: A cross-sectional exploratory study. BMC Geriatr. 2020, 20, 222. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics 2009, 50, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Linn, M.W.; Linn, B.S. The Rapid Disability Rating Scale—2. J. Am. Geriatr. Soc. 1982, 30, 378–382. [Google Scholar] [CrossRef]
- Kaufer, D.I.; Cummings, J.L.; Ketchel, P.; Smith, V.; MacMillan, A.; Shelley, T.; Lopez, O.L.; DeKosky, S.T. Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J. Neuropsychiatry Clin. Neurosci. 2000, 12, 233–239. [Google Scholar] [CrossRef]
- Hansen, T.; Slagsvold, B.; Ingebretsen, R. The Strains and Gains of Caregiving: An Examination of the Effects of Providing Personal Care to a Parent on a Range of Indicators of Psychological Well-Being. Soc. Indic. Res. 2013, 114, 323–343. [Google Scholar] [CrossRef]
- Greene, J.G.; Smith, R.; Gardiner, M.; Timbury, G.C. Measuring behavioural disturbance of elderly demented patients in the community and its effects on relatives: A factor analytic study. Age Ageing 1982, 11, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Ulstein, I.; Bruun Wyller, T.; Engedal, K. The relative stress scale, a useful instrument to identify various aspects of carer burden in dementia? Int. J. Geriatr. Psychiatry 2007, 22, 61–67. [Google Scholar] [CrossRef]
- Moholt, J.-M.; Friborg, O.; Skaalvik, M.W.; Henriksen, N. Psychometric validation of the Carers of Older People in Europe Index among family caregivers of older persons with dementia. SAGE Open Med. 2018, 6, 205031211879281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- StataCorp. Stata: Release 17. Statistical Software; StataCorp LLC.: College Station, TX, USA, 2021. [Google Scholar]
- Tibshirani, R. Regression Shrinkage and Selection Via the Lasso. J. R. Stat. Soc. Ser. B (Methodol.) 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Cooper, C.; Manela, M.; Katona, C.; Livingston, G. Screening for elder abuse in dementia in the LASER-AD study: Prevalence, correlates and validation of instruments. Int. J. Geriatr. Psychiatry 2008, 23, 283–288. [Google Scholar] [CrossRef]
- Lee, M.; Kolomer, S. Caregiver burden, dementia, and elder abuse in South Korea. J. Elder Abus. Negl. 2005, 17, 61–74. [Google Scholar] [CrossRef]
- Storey, J.E. Risk factors for elder abuse and neglect: A review of the literature. Aggress. Violent Behav. 2020, 50, 101339. [Google Scholar] [CrossRef]
- Pillemer, K.; Burnes, D.; Riffin, C.; Lachs, M.S. Elder Abuse: Global situation, risk factors, and prevention strategies. Gerontologist 2016, 56, S194–S205. [Google Scholar] [CrossRef]
- Wharton, T.C.; Ford, B.K. What is known about dementia care recipient violence and aggression against caregivers? J. Gerontol. Soc. Work. 2014, 57, 460–477. [Google Scholar] [CrossRef] [PubMed]
- Nordtug, B.; Malmedal, W.K.; Alnes, R.E.; Blindheim, K.; Steinsheim, G.; Moe, A. Informal caregivers and persons with dementia’s everyday life coping. Health Psychol. Open 2021, 8, 20551029211000954. [Google Scholar] [CrossRef]
- Lethin, C.; Hallberg, I.R.; Karlsson, S.; Janlöv, A.-C. Family caregivers experiences of formal care when caring for persons with dementia through the process of the disease. Scand. J. Caring Sci. 2016, 30, 526–534. [Google Scholar] [CrossRef]
- Backhouse, A.; Ukoumunne, O.C.; Richards, D.A.; Mccabe, R.; Watkins, R.; Dickens, C. The effectiveness of community-based coordinating interventions in dementia care: A meta-analysis and subgroup analysis of intervention components. BMC Health Serv. Res. 2017, 17, 1–10. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Li, K.-K.; Losada, A.; Zhang, F.; Au, A.; Thompson, L.W.; Gallagher-Thompson, D. The effectiveness of nonpharmacological interventions for informal dementia caregivers: An updated systematic review and meta-analysis. Psychol. Aging 2020, 35, 55–77. [Google Scholar] [CrossRef]
- Cooper, C.; Barber, J.; Griffin, M.; Rapaport, P.; Livingston, G. Effectiveness of START psychological intervention in reducing abuse by dementia family carers: Randomized controlled trial. Int. Psychogeriatr. 2016, 28, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Kruger, J.; Dunning, D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J. Pers. Soc. Psychol. 1999, 77, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Roberto, K.A.; Deater-Deckard, K. Risk for elder abuse among persons with dementia. In APA Handbook of Dementia; Smith, G.E., Farias, S.T., Eds.; APA handbooks in psychology®; American Psychological Association: Washington, DC, USA, 2018; pp. 599–614. [Google Scholar]
- Pillemer, K.; Burnes, D.; MacNeil, A. Investigating the connection between ageism and elder mistreatment. Nat. Aging 2021, 1, 159–164. [Google Scholar] [CrossRef]
- Botngård, A.; Eide, A.H.; Mosqueda, L.; Blekken, L.; Malmedal, W. Factors associated with staff-to-resident abuse in Norwegian nursing homes: A cross-sectional exploratory study. BMC Health Serv. Res. 2021, 21, 244. [Google Scholar] [CrossRef] [PubMed]



| Variable | Questions/Measure | Categorizations/Score | |
|---|---|---|---|
| Individual context, ICG | ICG gender | Your gender? | 1. Female; 2. Male |
| ICG age | Your birth year? | 2021—birth year | |
| ICG employment | What is your current main activity? (Employment includes studies, not working includes unemployed, retired, disabled or similar) | 1. Full-time employment; 2. Working part-time; 3. Not working | |
| ICG health | All in all, how do you assess your health? Would you say it is: 1. Excellent; 2. Good; 3. Average; 4. Poor; 5. Very poor. Recoded 4–5 = 1, 3 = 2, 1–2 = 3. | 1. Poor; 2. Average; 3. Good | |
| ICG mental health | Measured by the Patient Health Questionnaire for Depression and Anxiety (the PHQ–4) [34]. Four questions. Question scoring from 0 “Not at all” (bothered) to 3 (bothered) “Nearly every day”. | Sum score: 0–12. A higher score indicates a higher risk of anxiety and/or depression. | |
| ICG education | What is your highest completed level of education? | 1. High/vocational school level or lower; 2. University/college level or higher | |
| ICG economy | How easy or difficult is it for your household to manage financially on a daily basis, given your income? | 1. Hard; 2. Easy | |
| Individual context, PWD | PWD gender | What gender is the PWD? | 1. Female; 2. Male |
| PWD age | What year were they born? | 2021—birth year | |
| Dementia duration | Approximately how long has he/she had symptoms of dementia? | 0. ≤2 years; 1. >2–4 years 2. >4 years | |
| PWD disability | Measured by Rapid Disability Rating Scale 2 (RDRS2) [35] with 18 questions (without “degree of special problems subscale”—q18–20). Questions scored from 1 “None” (completely independent or normal behavior) to 4 “Total” (the person cannot, will not, or may not perform a behavior or has the most severe form of disability/problem). | Sum score 18–72. Higher score indicates more disability. | |
| BPSD | Neuropsychiatric Inventory–Questionnaire (NPI-Q) [36]. 12 questions measuring whether a symptom has been present in the past month (Yes/No) and the severity of the present symptom (1—mild, 2—moderate, 3—severe). | Sum score 0–36. Higher score indicates a more severe symptom burden. | |
| PWD alcohol consumption * | Approximately how often has the PWD consumed alcohol during the past 12 months? | 1. Never; 2. Monthly or less often; 3. Weekly | |
| Relational context | Relationship | What is your relationship with the PWD? | 1. Spouse/cohabitant/partner; 2. Child, sibling, or other |
| Caregiving duration | How long have you been helping them because of their illness? | 1. 0–2 years; 2. 3–5 years; 3. 6 years or longer | |
| Extent of care | How often do you help him/her? | 1. ≤Once a week; 2. 2–3 times a week; 3. 4–6 times a week; 4. Every day | |
| Previous relationship satisfaction | Measured by adapting a partnership satisfaction index [37]. Instructions: Think about the relationship you had with him/her before the illness. How much do you agree with the statement (a) We agreed on what is important in life; (b) We often had conflicts (inverted); (c) She/he often criticized me (inverted); (d) She/he understood me when I had problems. Rated on a scale from 0 “strongly disagree” to 5 “strongly agree.” | Sum score 0–20. Higher score indicates higher satisfaction. | |
| ICG burden | Caregiver subjective burden measured by the Relative Stress Scale (RSS) [38], 15 questions. The Norwegian version of the RSS is tested among ICGs of persons with dementia [39]. Rated from 0 “Never/not at all” to 4 “Always/considerably.” | Sum score 0–60. Higher score indicates a higher burden. | |
| PWD psychological aggression | Has the PWD done anything similar towards you? (Following questions regarding psychological abuse towards the PWD) | 0. No 1. Yes | |
| PWD physical aggression | Has the PWD done anything similar towards you? (Following questions regarding physical abuse towards the PWD) | 0. No 1. Yes | |
| Community context | ICG friends * | How often are you together with good friends? Do not include members of your own family. | 1. Weekly; 2. Monthly; 3. Less often |
| ICG leisure activity * | Approximately how often do you do the following in your spare time? (a) Exercises or are physically active so that you breathe heavily and/or sweat; (b) Go to the cinema, theater, concerts, and/or art exhibitions; (c) Participate in social activities in a club, association, or organization; (d) Attend worship services or other religious meetings. Score: 0 “Never,” 1 “ Less often,” 2 “Few times a year,” 3 “Monthly, but not weekly,” 4 “Weekly, but not daily,” 5 “Daily.” | Sum score 0–20. Higher score indicates more leisure activity. | |
| PWD leisure activity * | How is the PWD’s participation in social and cultural activities (think a weekly average for the year)? Do not include services and activities provided by the municipality. (a) Social activities; (b) Cultural activities | 0. No activity; 1. Activity | |
| Social restriction | Measured by The Modified Social Restriction Scale [40]. This scale consists of two questions regarding whether you have anyone else who can take care of the PWD if you get sick or need a break. Score: 1. “Yes, it will be easy to find someone,” 2. “Yes, I can find some, but it will not be that easy,” 3. “No, there is no one else.” | Score categorization: 2–3 = 1 “Low” (quite easy); 4 = 2 “Medium” (possible, but not easy); 5–6 = 3 “Hard” (no one else) | |
| Coop. w/municipal svcs. | Thinking of the municipality the PWD receives services from, how much do you agree with the statements: (a) The cooperation between me as a caregiver and the municipality works well; (b) I am consulted on questions regarding services and offers for the person with dementia; (c) I get sufficient information from the municipality about the services the person with dementia receives. Scale: 1 (strongly disagree)—5 (strongly agree) or 100 (Not applicable). | Sum score categorization: 1–7, 102–105, 201, 202 = 1 “Disagree”; 8–10, 106, 203 = 2 “Neither nor”; 11–15, 107–110, 204, 205 = 3 “Agree”; 300 = 4 “Not applicable” | |
| ICG training program | Have you participated/are you participating in a caregiver training program? (This is a course that consists of lectures and theme-based group discussions where the participants exchange experiences and gain knowledge about dementia, communication, coping, legislation, and services). | 1. Yes; 2. No | |
| ICG other training | Have you received/are you receiving other training about dementia? | 1. Yes; 2. No | |
| ICG support group | Do you participate in a peer support group with other caregivers of PWDs? | 1. Yes; 2. No | |
| PWD education prog. | Has the PWD attended, or do they attend a dementia education program? (This is a course for PWDs that provides knowledge about dementia, stimulates self-management, and is a meeting place for exchanging experiences and mutual support); Does the PWD participate in a peer support group? If “Yes” on one or both questions: Yes; if “No” on both: No | 1. Yes; 2. No | |
| Municipal svcs. contact | Have you been assigned a contact person/coordinator from the municipal health services for you and the PWD to contact? | 1. Yes; 2. No | |
| Do you, due to your caregiver role, or the PWD receive any of the following services or offers? | |||
| Dementia care team | Follow-up from dementia care team/dementia contact | 1. Yes; 2. No | |
| Adult daycare center | Activity offer, adult day care center, or similar | 1. Yes; 2. No | |
| Institutional respite care | Respite care in an institution (nursing home/care home/assisted living facility) | 1. Yes; 2. No | |
| Home care nursing | Home care nursing | 1. Yes; 2. No | |
| PWD support person | Support contact (a person who helps another person to have an active and meaningful leisure time. These services are publicly funded); Friendly visitor volunteer (a volunteer that meets and does different activities with a PWD). If “Yes” on one or both questions: Yes; if “No” on both: No. | 1. Yes; 2. No | |
| General practitioner | General practitioner (consultation/follow-up) | 1. Yes; 2. No | |
| Hospital follow-up | Follow-up in hospital/outpatient clinic | 1. Yes; 2. No | |
| Psychological Abuse | Physical Abuse | ||||
|---|---|---|---|---|---|
| No Abuse n = 429 | Abuse n = 108 | No Abuse n = 486 | Abuse n = 53 | ||
| Individual context, ICG | ICG gender: Female (vs. male) | 283 (66.6) | 78 (75.0) | 330 (68.8) | 32 (62.8) |
| ICG age | 66.53 ± 12.24 | 70.81 ± 8.88 | 66.68 ± 11.99 | 74.25 ± 6.13 | |
| ICG employment: Full-time | 126 (29.7) | 18 (17.6) | 141 (29.6) | 3 (5.9) | |
| Part-time | 43 (10.1) | 7 (6.9) | 47 (9.9) | 3 (5.9) | |
| Not working | 255 (60.1) | 77 (75.5) | 289 (60.6) | 45 (88.2) | |
| ICG health: Poor | 44 (10.4) | 14 (13.1) | 52 (10.9) | 6 (11.3) | |
| Average | 111 (26.2) | 36 (33.6) | 129 (26.9) | 18 (34.0) | |
| Good | 268 (63.4) | 57 (53.3) | 298 (62.2) | 29 (54.7) | |
| ICG mental health | 2.46 ± 2.24 | 3.98 ± 3.08 | 2.65 ± 2.44 | 3.77 ± 2.83 | |
| ICG education: ≤High school (vs. college/univ.) | 252 (59.2) | 53 (51.0) | 279 (58.0) | 27 (52.9) | |
| ICG economy: Hard (vs. easy) | 39 (9.3) | 8 (7.7) | 41 (8.6) | 6 (11.8) | |
| Individual context, PWD | PWD gender: Female (vs. male) | 224 (52.5) | 32 (30.2) | 238 (49.2) | 19 (37.3) |
| PWD age | 79.20 ± 7.81 | 77.72 ± 7.58 | 79.14 ± 7.92 | 76.94 ± 5.92 | |
| Dementia duration: ≤2 years | 96 (22.4) | 19 (17.8) | 105 (21.7) | 10 (19.2) | |
| >2–4 years | 159 (37.2) | 39 (36.5) | 183 (37.7) | 16 (30.8) | |
| >4 years | 173 (40.4) | 49 (45.8) | 197 (40.6) | 26 (50.0) | |
| PWD disability | 39.18 ± 9.72 | 42.01 ± 9.93 | 39.13 ± 9.64 | 44.32 ± 10.46 | |
| BPSD | 8.51 ± 6.34 | 9.89 ± 5.53 | 8.49 ± 6.03 | 10.67 ± 7.17 | |
| PWD alcohol consumption: Never | 147 (34.4) | 28 (26.7) | 159 (32.9) | 16 (31.4) | |
| ≤Monthly | 156 (36.5) | 40 (38.1) | 180 (37.3) | 18 (35.3) | |
| Weekly | 124 (29.0) | 37 (35.2) | 144 29.8 | 17 (33.3) | |
| Relational context | Relationship: Spouse (vs. child or other) | 242 (56.5) | 94 (89.5) | 288 (59.5) | 50 (98.0) |
| Caregiving duration: 0–2 years | 152 (35.6) | 29 (27.6) | 166 (34.3) | 15 (30.0) | |
| 3–5 years | 201 (47.1) | 58 (55.2) | 233 (48.1) | 27 (54.0) | |
| ≥6 year | 74 (17.3) | 18 (17.1) | 85 (17.6) | 8 (16.0) | |
| Extent of care: ≤Once a week | 37 (8.7) | 3 (2.9) | 40 (8.3) | 0 (0.0) | |
| 2–3 times/week | 76 (17.9) | 4 (3.8) | 80 (16.6) | 0 (0.0) | |
| 4–6 times/week | 67 (15.8) | 3 (2.9) | 68 (14.1) | 2 (4.0) | |
| Every day | 245 (57.7) | 95 (90.5) | 294 (61.0) | 48 (96.0) | |
| Previous relationship satisfaction | 3.78 ± 0.96 | 3.56 ± 0.90 | 3.75 ± 0.96 | 3.58 ± 0.90 | |
| ICG burden | 23.35 ± 11.37 | 31.72 ± 9.91 | 24.36 ± 11.49 | 30.69 ± 11.39 | |
| PWD psychological aggression: Yes | 125 (29.8) | 54 (50.5) | 158 (33.1) | 21 (41.2) | |
| PWD physical aggression: Yes | 29 (6.9) | 12 (11.5) | 29 (6.2) | 12 (22.6) | |
| Community context | ICG w/friends: Weekly | 163 (38.4) | 28 (26.2) | 177 (36.8) | 15 (28.9) |
| Monthly | 139 (32.7) | 41 (38.3) | 160 (33.3) | 20 (38.5) | |
| Less often | 123 (28.9) | 38 (35.5) | 144 (29.9) | 17 (32.7) | |
| ICG leisure activity | 6.99 ± 3.11 | 6.22 ± 3.46 | 6.84 ± 3.13 | 6.80 ± 3.76 | |
| PWD leisure activity: Activity (vs. no activity) | 337 (79.3) | 80 (76.9) | 380 (79.5) | 38 (73.1) | |
| Social restriction: Low | 186 (44.1) | 26 (24.3) | 201 (42.1) | 11 (20.8) | |
| Medium | 133 (31.5) | 39 (36.5) | 152 (31.9) | 21 (39.6) | |
| High | 103 (24.4) | 42 (39.3) | 124 (26.0) | 21 (39.6) | |
| Coop. w/municipal svcs.: Disagree | 69 (16.2) | 14 (13.2) | 78 (16.2) | 5 (9.4) | |
| Neither nor | 87 (20.4) | 29 (27.4) | 102 (21.2) | 14 (26.4) | |
| Agree | 239 (56.0) | 61 (57.6) | 272 (56.6) | 29 (54.7) | |
| Not applicable | 32 (7.5) | 2 (1.9) | 29 (6.0) | 5 (9.4) | |
| ICG training program: Yes | 175 (40.8) | 52 (48.6) | 193 (39.8) | 34 (64.2) | |
| ICG other training: Yes | 90 (21.0) | 22 (20.6) | 103 (21.2) | 9 (17.7) | |
| ICG support group: Yes | 75 (17.5) | 30 (27.8) | 90 (18.6) | 15 (28.3) | |
| PWD education prog.: Yes | 61 (14.2) | 14 (13.0) | 66 (13.6) | 9 (17.0) | |
| Municipal svcs. contact: Yes | 281 (65.7) | 73 (67.6) | 325 (67.0) | 30 (56.6) | |
| Dementia care team: Yes | 191 (45.1) | 50 (47.2) | 222 (46.4) | 19 (37.3) | |
| Daycare center etc.: Yes | 224 (52.6) | 69 63.9) | 260 (53.8) | 34 (65.4) | |
| Institutional respite care: Yes | 102 (23.8) | 39 (36.5) | 116 (24.0) | 25 (48.1) | |
| Home care nursing: Yes | 238 (56.5) | 45 (41.7) | 259 (54.3) | 24 (46.2) | |
| Support person: Yes | 52 (12.2) | 15 (13.9) | 58 (12.0) | 9 (17.0) | |
| General practitioner: Yes | 336 (78.9) | 95 (88.0) | 386 (80.1) | 45 (86.5) | |
| Hospital follow-up: Yes | 138 (32.2) | 35 (33.0) | 157 (32.6) | 16 (30.2) | |
| Psychological Abuse | Physical Abuse | ||||
|---|---|---|---|---|---|
| Variable | OR | Perc. Not 0 | OR | Perc. Not 0 | |
| Individual context, ICG | ICG gender: Female (vs. male) | 1 | 49.5 | 0.63 | 83.5 |
| ICG age | 1 | 17.5 | 1 | 20.9 | |
| ICG employment: Full-time | 1 | 19.9 | 0.87 | 47.8 | |
| Part-time | 1 | 32.8 | 1 | 16.2 | |
| Not working | 1 | 12.8 | 1 | 38.3 | |
| ICG health: Poor | 1 | 27.7 | 1 | 37.5 | |
| Average | 1 | 26.6 | 1 | 30.3 | |
| Good | 1 | 19.5 | 1 | 27.7 | |
| ICG mental health | 1 | 38.3 | 1 | 33.0 | |
| ICG education: Lower (vs. higher) | 1 | 72.7 | 1 | 61.0 | |
| ICG economy: Hard (vs. easy) | 1 | 43.0 | 1 | 43.4 | |
| Individual context, PWD | PWD gender: Female (vs. male) | 1 | 30.7 | 1 | 14.2 |
| PWD age | 1 | 32.0 | 1 | 50.9 | |
| Dementia duration: ≤2 years | 1 | 21.9 | 1 | 47.3 | |
| >2–4 years | 1 | 24.4 | 1 | 24.0 | |
| >4 years | 1 | 22.0 | 1 | 30.7 | |
| PWD disability | 1 | 37.7 | 1.03 | 85.4 | |
| BPSD | 1 | 24.7 | 1.02 | 67.1 | |
| PWD alcohol consumption: Never | 1 | 41.1 | 1 | 34.1 | |
| ≤Monthly | 1 | 24.9 | 1 | 35.7 | |
| Weekly | 1 | 28.1 | 1 | 26.4 | |
| Relational context | Relationship: Spouse (vs. child or other) | 2.82 | 100.0 | 6.45 | 99.7 |
| Caregiving duration: 0–2 years | 1 | 38.0 | 1 | 20.8 | |
| 3–5 years | 1 | 31.8 | 1 | 36.7 | |
| ≥6 year | 1 | 24.0 | 1 | 36.7 | |
| Extent of care: ≤Once a week | 1 | 19.9 | 1 | 17.9 | |
| 2–3 times/week | 1 | 16.2 | 1 | 18.7 | |
| 4–6 times/week | 1 | 52.4 | 1 | 3.1 | |
| Every day | 1.18 | 59.6 | 1.46 | 76.5 | |
| Previous relationship satisfaction | 1 | 46.8 | 0.96 | 59.9 | |
| ICG burden | 1.04 | 99.5 | 1 | 27.8 | |
| PWD psychological aggression: No | 0.92 | 80.5 | 1.22 | 74.0 | |
| PWD physical aggression: No | 1 | 39.5 | 0.33 | 95.0 | |
| Community context | ICG w/friends: Weekly | 1 | 44.7 | 1 | 39.4 |
| Monthly | 1 | 42.8 | 1.03 | 50.8 | |
| Less often | 1 | 17.4 | 1 | 24.1 | |
| ICG leisure activity | 1 | 29.4 | 1 | 60.3 | |
| PWD leisure activity: No activity (vs. activity) | 1 | 48.8 | 1 | 45.6 | |
| Social restriction: Low | 1 | 41.1 | 0.72 | 71.0 | |
| Medium | 1 | 47.1 | 1 | 51.4 | |
| High | 1 | 19.6 | 1 | 19.2 | |
| Coop. w/municipal svcs.: Disagree | 1 | 23.3 | 1 | 50.6 | |
| Neither nor | 1 | 50.1 | 1.02 | 55.2 | |
| Agree | 1 | 13.6 | 1 | 18.6 | |
| Not applicable | 1 | 72.3 | 1.56 | 74.2 | |
| ICG training program: Yes | 1 | 46.3 | 1.91 | 95.0 | |
| ICG other training: Yes | 1 | 35.3 | 1 | 40.8 | |
| ICG support group: Yes | 1 | 37.4 | 1 | 43.3 | |
| PWD education prog.: Yes | 1 | 45.1 | 1 | 43.3 | |
| Municipal svcs. contact: Yes | 1 | 38.3 | 0.47 | 95.8 | |
| Dementia care team: Yes | 1 | 37.2 | 0.97 | 59.8 | |
| Adult daycare center: Yes | 1 | 61.7 | 1 | 42.8 | |
| Institutional respite care: Yes | 1 | 38.6 | 1.26 | 74.0 | |
| Home care nursing: Yes | 1 | 61.3 | 1 | 40.5 | |
| Support person: Yes | 1 | 35.4 | 1 | 38.3 | |
| General practitioner: Yes | 1.15 | 88.1 | 1 | 42.8 | |
| Hospital follow-up: Yes | 1 | 34.9 | 1 | 38.7 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinsheim, G.; Malmedal, W.; Follestad, T.; Olsen, B.; Saga, S. Contextual Factors Associated with Abuse of Home-Dwelling Persons with Dementia: A Cross-Sectional Exploratory Study of Informal Caregivers. Int. J. Environ. Res. Public Health 2023, 20, 2823. https://doi.org/10.3390/ijerph20042823
Steinsheim G, Malmedal W, Follestad T, Olsen B, Saga S. Contextual Factors Associated with Abuse of Home-Dwelling Persons with Dementia: A Cross-Sectional Exploratory Study of Informal Caregivers. International Journal of Environmental Research and Public Health. 2023; 20(4):2823. https://doi.org/10.3390/ijerph20042823
Chicago/Turabian StyleSteinsheim, Gunn, Wenche Malmedal, Turid Follestad, Bonnie Olsen, and Susan Saga. 2023. "Contextual Factors Associated with Abuse of Home-Dwelling Persons with Dementia: A Cross-Sectional Exploratory Study of Informal Caregivers" International Journal of Environmental Research and Public Health 20, no. 4: 2823. https://doi.org/10.3390/ijerph20042823
APA StyleSteinsheim, G., Malmedal, W., Follestad, T., Olsen, B., & Saga, S. (2023). Contextual Factors Associated with Abuse of Home-Dwelling Persons with Dementia: A Cross-Sectional Exploratory Study of Informal Caregivers. International Journal of Environmental Research and Public Health, 20(4), 2823. https://doi.org/10.3390/ijerph20042823








