Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis
Abstract
:1. Introduction
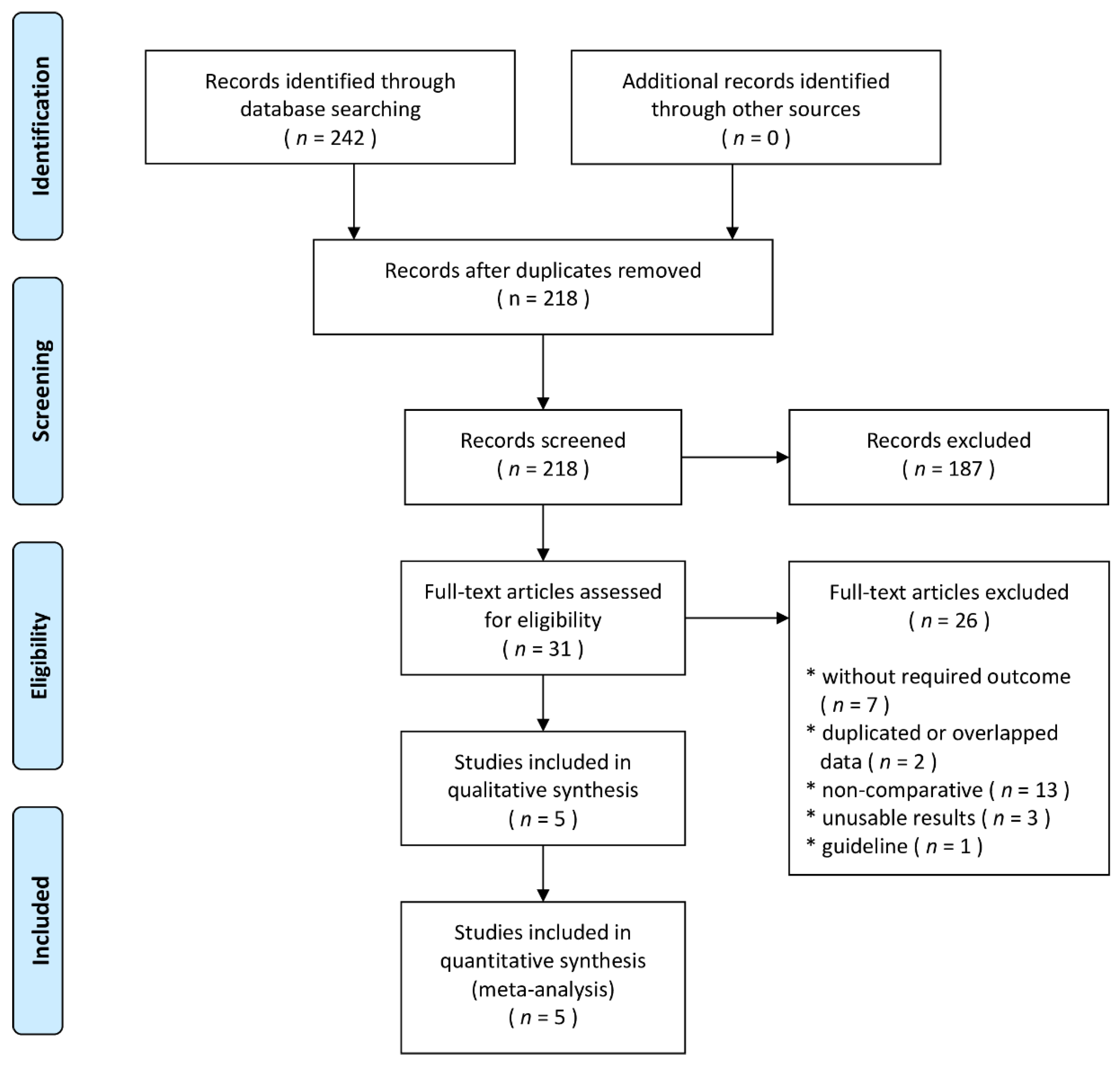
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
2.6. Role of the Funding Source
3. Results
3.1. Study Characteristics
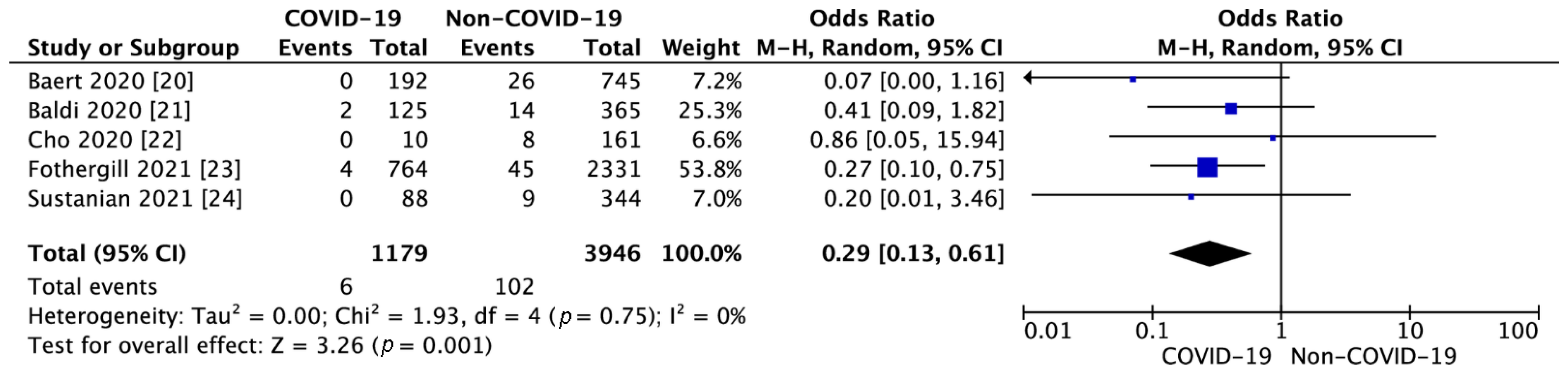
3.2. OHCA Outcomes
3.3. Cardiopulmonary Resuscitation Parameters
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Vreede-Swagemakers, J.J.; Gorgels, A.P.; Dubois-Arbouw, W.I.; van Ree, J.W.; Daemen, M.J.; Houben, L.G.; Wellens, H.J. Out-of-hospital cardiac arrest in the 1990’s: A population-based study in the Maastricht area on incidence, characteristics and survival. J. Am. Coll. Cardiol. 1997, 30, 1500–1505. [Google Scholar] [CrossRef] [Green Version]
- Gräsner, J.T.; Herlitz, J.; Koster, R.W.; Rosell-Ortiz, F.; Stamakis, L.; Bossaert, L. Quality management in resuscitation–towards a European cardiac arrest registry (EuReCa). Resuscitation 2011, 82, 989–994. [Google Scholar] [CrossRef]
- Malysz, M.; Dabrowski, M.; Böttiger, B.W.; Smereka, J.; Kulak, K.; Szarpak, A.; Jaguszewski, M.; Filipiak, K.J.; Ladny, J.R.; Ruetzler, K.; et al. Resuscitation of the patient with suspected/confirmed COVID-19 when wearing personal protective equipment: A randomized multicenter crossover simulation trial. Cardiol. J. 2020, 27, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Wren, C. Sudden death in children and adolescents. Heart 2002, 88, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: A systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef]
- Tunstall-Pedoe, H.; Bailey, L.; Chamberlain, D.A.; Marsden, A.K.; Ward, M.E.; Zideman, D.A. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): Methods and overall results. BMJ 1992, 304, 1347–1351. [Google Scholar] [CrossRef] [Green Version]
- Dzieciatkowski, T.; Szarpak, L.; Filipiak, K.J.; Jaguszewski, M.; Ladny, J.R.; Smereka, J. COVID-19 challenge for modern medicine. Cardiol. J. 2020, 27, 175–183. [Google Scholar] [CrossRef] [Green Version]
- Szarpak, L.; Ruetzler, K.; Dabrowski, M.; Nadolny, K.; Ladny, J.R.; Smereka, J.; Jaguszewski, M.; Filipiak, K.J. Dilemmas in resuscitation of COVID-19 patients based on current evidence. Cardiol. J. 2020, 27, 327–328. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available online: https://coronavirus.jhu.edu/map.html (accessed on 19 February 2021).
- Jaguszewski, M.J.; Szarpak, L.; Filipiak, K.J. Impact of COVID-19 pandemic on out-of-hospital cardiac arrest survival rate. Resuscitation 2020, 159, 40–41. [Google Scholar] [CrossRef] [PubMed]
- Gąsecka, A.; Borovac, J.A.; Guerreiro, R.A.; Giustozzi, M.; Parker, W.; Caldeira, D.; Chiva-Blanch, G. Thrombotic Complications in Patients with COVID-19: Pathophysiological Mechanisms, Diagnosis, and Treatment. Cardiovasc. Drugs Ther. 2020, 1–15. [Google Scholar] [CrossRef]
- Gąsecka, A.; Filipiak, K.J.; Jaguszewski, M.J. Impaired microcirculation function in COVID-19 and implications for potential therapies. Cardiol. J. 2020, 27, 485–488. [Google Scholar] [CrossRef] [PubMed]
- Lai, P.H.; Lancet, E.A.; Weiden, M.D.; Webber, M.P.; Zeig-Owens, R.; Hall, C.B.; Prezant, D.J. Characteristics Associated With Out-of-Hospital Cardiac Arrests and Resuscitations During the Novel Coronavirus Disease 2019 Pandemic in New York City. JAMA Cardiol. 2020, 5, 1154–1163. [Google Scholar] [CrossRef] [PubMed]
- Marijon, E.; Karam, N.; Jost, D.; Perrot, D.; Frattini, B.; Derkenne, C.; Waldmann, V.; Beganton, F.; Narayanan, K. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: A population-based, observational study. Lancet Public Health 2020, 5, e437–e443. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schünemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ. Int. 2018, 121, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [Green Version]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [Green Version]
- Baert, V.; Jaeger, D.; Hubert, H.; Lascarrou, J.B.; Debaty, G.; Chouihed, T.; Javaudin, F.; on Behalf of the GR-RéAC. Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: A registry-based study. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 119. [Google Scholar] [CrossRef]
- Baldi, E.; Sechi, G.M.; Mare, C.; Canevari, F.; Brancaglione, A.; Primi, R.; Klersy, C.; Palo, A.; Contri, E.; Ronchi, V.; et al. COVID-19 kills at home: The close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur. Heart J. 2020, 41, 3045–3054. [Google Scholar] [CrossRef]
- Cho, J.W.; Jung, H.; Lie, M.J.; Lee, S.H.; Lee, S.H.; Mun, Y.H.; Chung, H.; Kim, Y.H.; Kim, G.M.; Park, S.; et al. Preparedness of personal protective equipment and implementation of new CPR strategies for patients with out-of-hospital cardiac arrest in the COVID-19 era. Resusc. Plus 2020, 3, 100015. [Google Scholar] [CrossRef]
- Fothergill, R.T.; Smith, A.L.; Wrigley, F.; Perkins, G.D. Out-of-Hospital Cardiac Arrest in London during the COVID-19 pandemic. Resusc. Plus 2021, 5, 100066. [Google Scholar] [CrossRef] [PubMed]
- Sultanian, P.; Lundgren, P.; Strömsöe, A.; Aune, S.; Bergström, G.; Hagberg, E.; Hollenberg, J.; Lindqvist, J.; Djärv, T.; Castelheim, A.; et al. Cardiac arrest in COVID-19: Characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur. Heart J. 2021, ehaa1067. [Google Scholar] [CrossRef]
- Brown, E.; Chan, L.M. Should chest compressions be considered an aerosol-generating procedure? A literature review in response to recent guidelines on personal protective equipment for patients with suspected COVID-19. Clin. Med. 2020, 20, e154–e159. [Google Scholar] [CrossRef] [PubMed]
- Kulak, K.; Wieczorek, K.; Krupski, A.; Fajfer, Z. SARS-CoV-2 as a real threat for healthcare workers. Disaster Emerg. Med. J. 2020, 5, 110–111. [Google Scholar] [CrossRef]
- Nolan, J.P.; Monsieurs, K.G.; Bossaert, L.; Böttiger, B.W.; Greif, R.; Lott, C.; Madar, J.; Olasveengen, T.M.; Roehr, C.C.; Semeraro, F.; et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation 2020, 153, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Edelson, D.P.; Sasson, C.; Chan, P.S.; Atkins, D.L.; Aziz, K.; Becker, L.B.; Berg, R.A.; Bradley, S.M.; Brooks, S.C.; Cheng, A.; et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates with Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get with the Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation 2020, 141, e933–e943. [Google Scholar] [CrossRef] [Green Version]
- Smereka, J.; Szarpak, L. COVID 19 a challenge for emergency medicine and every health care professional. Am. J. Emerg. Med. 2020, 38, 2232–2233. [Google Scholar] [CrossRef]
- Ruetzler, K.; Smereka, J.; Ludwin, K.; Drozd, A.; Szarpak, L. Respiratory protection among healthcare workers during cardiopulmonary resuscitation in COVID-19 patients. Am. J. Emerg. Med. 2021, 39, 233–234. [Google Scholar] [CrossRef] [PubMed]
- Ludwin, K.; Bialka, S.; Czyzewski, L.; Smereka, J.; Dabrowski, M.; Dabrowska, A.; Ladny, J.R.; Ruetzler, K.; Szarpak, L. Video laryngoscopy for endotracheal intubation of adult patients with suspected/confirmed COVID-19. A systematic review and meta-analysis of randomized controlled trials. Disaster Emerg. Med. J. 2020, 5, 85–97. [Google Scholar] [CrossRef]
- Renzi, S.; Landoni, G.; Zangrillo, A.; Ciceri, F. MicroCLOTS pathophysiology in COVID 19. Korean J. Intern. Med. 2020. [Google Scholar] [CrossRef]
- Zhang, L.; Yan, Y.; Fan, Q.; Liu, H.; Liu, X.; Liu, Z.; Zhang, Z. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J. Thromb. Haemost. 2020, 18, 1324–1329. [Google Scholar] [CrossRef]
- Lindner, D.; Fitzek, A.; Bräuninger, H.; Aleshcheva, G.; Edler, C.; Meissner, K.; Scherschel, K.; Kirchhof, P.; Escher, F.; Schultheiss, H.P.; et al. Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020, 5, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J. COVID-19 can affect the heart. Science 2020, 370, 408–409. [Google Scholar] [CrossRef] [PubMed]
- Lorente-Ros, A.; Monteagudo Ruiz, J.M.; Rincón, L.M.; Ortega Pérez, R.; Rivas, S.; Martínez-Moya, R.; Sanromán, M.A.; Manzano, L.; Alonso, G.L.; Ibáñez, B.; et al. Myocardial injury determination improves risk stratification and predicts mortality in COVID-19 patients. Cardiol. J. 2020, 27, 489–496. [Google Scholar] [CrossRef]
- Nickles, A.V.; Oostema, A.; Allen, J.; O’Brien, S.L.; Demel, S.L.; Reeves, M.J. Comparison of Out-of-Hospital Cardiac Arrests and Fatalities in the Metro Detroit Area During the COVID-19 Pandemic With Previous-Year Events. JAMA Netw. Open 2021, 4, e2032331. [Google Scholar] [CrossRef] [PubMed]
- Uy-Evanado, A.; Chugh, H.S.; Sargsyan, A.; Nakamura, K.; Mariani, R.; Hadduck, K.; Salvucci, A.; Jui, J.; Chugh, S.S.; Reinier, K. Out-of-Hospital Cardiac Arrest Response and Outcomes During the COVID-19 Pandemic. JAMA Cardiol. 2020. [Google Scholar] [CrossRef]
- Elmer, J.; Okubo, M.; Guyette, F.X.; Martin-Gill, C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation 2020, 156, 282–283. [Google Scholar] [CrossRef]
- Semeraro, F.; Gamberini, L.; Tartaglione, M.; Iarussi, B.; Descovich, C.; Picoco, C.; Gordini, G. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: System response to preserve performances. Resuscitation 2020, 157, 1–2. [Google Scholar] [CrossRef]
- Borkowska, M.J.; Smereka, J.; Safiejko, K.; Nadolny, K.; Maslanka, M.; Filipiak, K.J.; Jaguszewski, M.J.; Szarpak, L. Out-of-hospital cardiac arrest treated by emergency medical service teams during COVID-19 pandemic: A retrospective cohort study. Cardiol. J. 2020. [Google Scholar] [CrossRef]
- Sasson, C.; Rogers, M.A.; Dahl, J.; Kellermann, A.L. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 63–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Jeabory, M.; Safiejko, K.; Bialka, S.; Pruc, M.; Gasecka, A.; Szarpak, L. Impact of COVID-19 on bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest: Is it as bad as we think? Cardiol. J. 2020, 27, 884–885. [Google Scholar] [CrossRef] [PubMed]
| Study | Country | Study Design | COVID-19 Status | Number of Patients | Age, Years (Mean ± SD) | Sex (Male), No./Total (%) | Bystander Witnessed No./Total (%) | Bystander CPR No./Total (%) | Shockable Initial Rhythm No./Total (%) | Time from Call to Arrival (Mean ± SD) | Survival to Discharge No./Total (%) | NOS Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baert et al. 2020 [20] | France | Multi-centre retrospective study | COVID-19 | 197 | 67 ± 18 | 117/197 (59.4) | 126/197 (64.0) | 99/197 (50.3) | 8/197 (4.1) | 25 ± 22 | 0/192 (0.0) | Fair |
| Non-COVID-19 | 808 | 69 ± 16 | 559/808 (69.2) | 522/808 (64.6) | 401/808 (49.6) | 79/806 (9.8) | 23 ± 17 | 26/745 (3.5) | ||||
| Baldi et al. 2020 [21] | Italy | Single-centre retrospective study | COVID-19 | 125 | 77 ± 2.3 | 83/125 (66.4) | 25/125 (20) | 13/125 (9.6) | 8/125 (9.1) | 16.6 ± 1.7 | 2/125 (2.3) | Fair |
| Non-COVID-19 | 365 | 76.8 ± 2.8 | 238/365 (65.2) | 33/365 (9.0) | 76/365 (39.2) | 28/365 (12.4) | 14.5 ± 1.3 | 14/365 (6.2) | ||||
| Cho et al. 2020 [22] | Republic of Korea | Multi-centre retrospective study | COVID-19 | 10 | 73.3 ± 4.3 | 4/10 (40.0) | 10/10 (100) | 1/10 (10.0) | 0/10 (0) | 24.5 ± 4.6 | 0/10 (0) | Good |
| Non-COVID-19 | 161 | 72.3 ± 3.2 | 104/161 (64.6) | 120/161 (74.5) | 57/161 (35.4) | 15/161 (9.3) | 19.5 ± 1.7 | 8/161 (5.0) | ||||
| Fothergill et al. 2021 [23] | UK | Single-centre retrospective study | COVID-19 | 766 | 70 ± 18 | 468 (61.2) | 216/393 (55.0) | 257/393 (65.4) | 24/393 (6.2) | 11 ± 1.8 | 4/764 (0.5) | Good |
| Non-COVID-19 | 2356 | 71 ± 19 | 1371 (58.3) | 390/742 (52.6) | 461/742 (62.1) | 144/742 (19.5) | 9.7 ± 1.3 | 45/2331 (1.9) | ||||
| Sultanian et al. 2021 [24] | Sweden | Observational registry-based study | COVID-19 | 88 | 66.5 ± 18.4 | 59 (67.0) | 37 (42.0) | 48 (54.5) | 6 (6.8) | 11.8 ± 2.2 | 0 (0.0) | Good |
| Non-COVID-19 | 334 | 70.6 ± 16.4 | 241 (72.2) | 158 (47.3) | 188 (56.3) | 63 (18.9) | 13 ± 2.3 | 9 (2.7) |
| Parameter | No. of Studies | Cases in COVID-19 Suspected or Diagnosed Group | Cases in COVID-19 Not Suspected or Diagnosed Group | OR (95% CI) | p Value | I2 Statistics |
|---|---|---|---|---|---|---|
| Death in the field | 2 | 401/518 (77.4%) | 650/1107 (58.7%) | 2.02 (0.83, 4.92) | 0.001 | 92% |
| Transport with ongoing CPR | 1 | 11/125 (8.8%) | 23/365 (6.3%) | 1.43 (0.68, 3.03) | 0.34 | NA |
| ROSC | 5 | 108/812 (13.3%) | 637/2405 (26.5%) | 0.67 (0.55, 0.81) | <0.001 | 20% |
| Survival to hospital admission | 3 | 41/528 (7.8%) | 207/1268 (16.3%) | 0.54 (0.19, 1.52) | 0.008 | 70% |
| Favourable neurological outcome at discharge | 1 | 0/10 (0%) | 5/161 (3.1%) | 1.35 (0.07, 26.19) | 0.84 | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borkowska, M.J.; Jaguszewski, M.J.; Koda, M.; Gasecka, A.; Szarpak, A.; Gilis-Malinowska, N.; Safiejko, K.; Szarpak, L.; Filipiak, K.J.; Smereka, J. Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis. J. Clin. Med. 2021, 10, 1209. https://doi.org/10.3390/jcm10061209
Borkowska MJ, Jaguszewski MJ, Koda M, Gasecka A, Szarpak A, Gilis-Malinowska N, Safiejko K, Szarpak L, Filipiak KJ, Smereka J. Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2021; 10(6):1209. https://doi.org/10.3390/jcm10061209
Chicago/Turabian StyleBorkowska, Magdalena J., Miłosz J. Jaguszewski, Mariusz Koda, Aleksandra Gasecka, Agnieszka Szarpak, Natasza Gilis-Malinowska, Kamil Safiejko, Lukasz Szarpak, Krzysztof J. Filipiak, and Jacek Smereka. 2021. "Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis" Journal of Clinical Medicine 10, no. 6: 1209. https://doi.org/10.3390/jcm10061209
APA StyleBorkowska, M. J., Jaguszewski, M. J., Koda, M., Gasecka, A., Szarpak, A., Gilis-Malinowska, N., Safiejko, K., Szarpak, L., Filipiak, K. J., & Smereka, J. (2021). Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 10(6), 1209. https://doi.org/10.3390/jcm10061209










