Effect of a New Tele-Rehabilitation Program versus Standard Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease
Abstract
:1. Introduction
2. Methods and Materials
2.1. Design of the Research
2.2. Participants
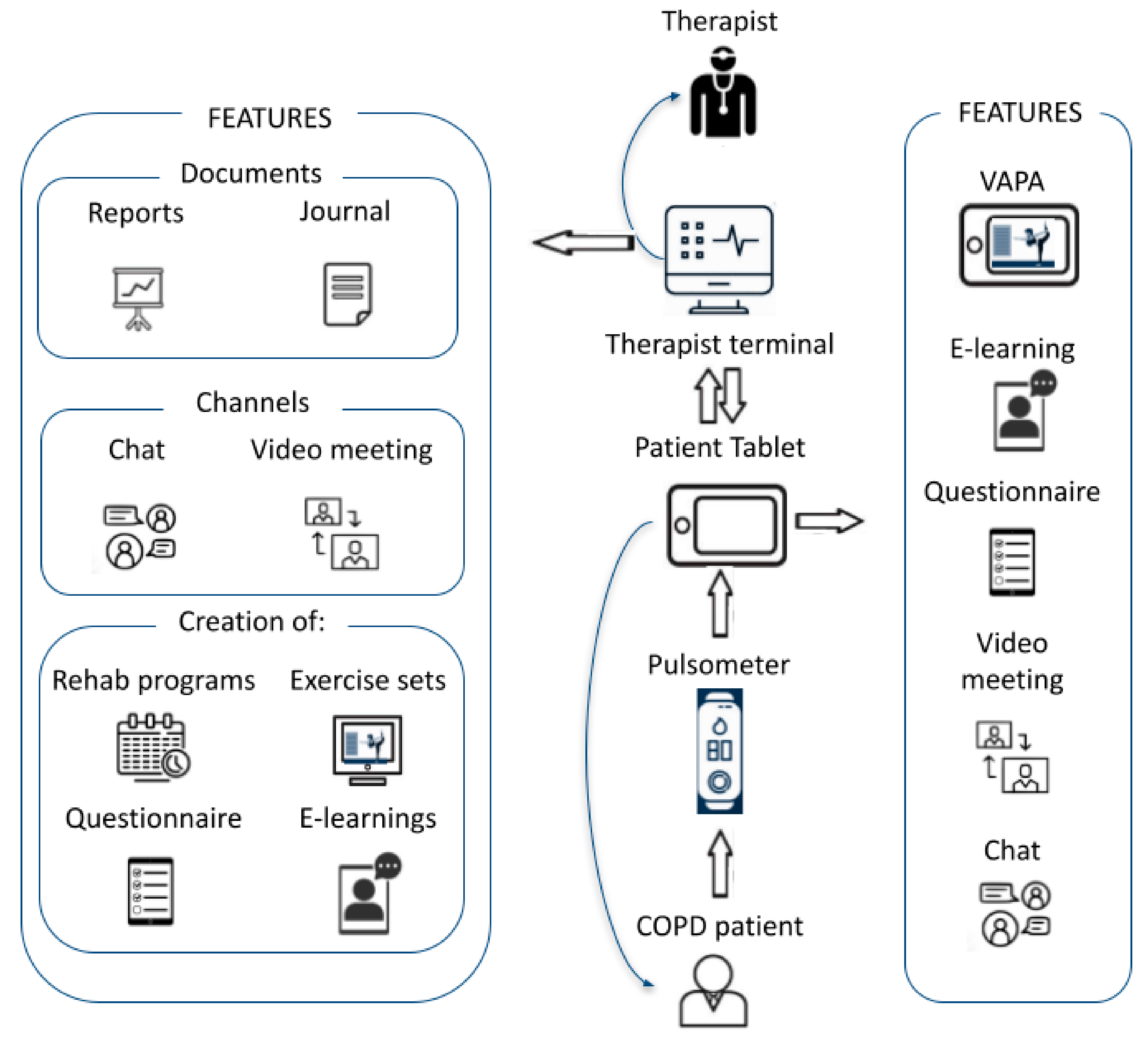
2.3. Tele-Rehabilitation
2.4. Standard Rehabilitation
2.5. Endpoints
2.6. Statistics
3. Results
3.1. Patients
3.2. 6 Min Walk Test (6MWT)
3.3. Pedometry and Quality of Life
3.4. Continued Use of VAPA in the TR with VAPA
3.5. Exercise Set Time, Adherence, Patient Satisfaction and Safety
3.6. Additional Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Sundhedsstyrelsen. Resumé Af Anbefalinger for KOL. 2007, Volume 28. Available online: https://www.sst.dk/da/udgivelser/2017/Anbefalinger-for-tvaersektorielle-forloeb-for-mennesker-med-KOL (accessed on 30 January 2021).
- Lawlor, M.; Kealy, S.; Agnew, M.; Korn, B.; Quinn, J.; Cassidy, C.; Silke, B.; O’Connell, F.; O’Donnell, R. Early Discharge Care with Ongoing Follow-up Support May Reduce Hospital Readmissions in COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2009, 4, 55–60. [Google Scholar]
- Sohanpal, R.; Hooper, R.; Hames, R.; Priebe, S.; Taylor, S. Reporting Participation Rates in Studies of Non-Pharmacological Interventions for Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review. Syst. Rev. 2012, 1, 66. [Google Scholar] [CrossRef]
- Sahin, H.; Naz, I. Why Are COPD Patients Unable to Complete the Outpatient Pulmonary Rehabilitation Program? Chron. Respir. Dis. 2018, 15, 411–418. [Google Scholar] [CrossRef] [PubMed]
- The Differences between SARS-CoV-1 and SARS-CoV-2. Available online: https://sciencemediahub.eu/2020/04/23/the-differences-between-sars-cov-1-and-sars-cov-2/ (accessed on 30 January 2021).
- Rutkowski, S. Management Challenges in Chronic Obstructive Pulmonary Disease in the COVID-19 Pandemic: Telehealth and Virtual Reality. J. Clin. Med. Res. 2021, 10, 1261. [Google Scholar] [CrossRef]
- Cox, N.S.; Dal Corso, S.; Hansen, H.; McDonald, C.F.; Hill, C.J.; Zanaboni, P.; Alison, J.A.; O’Halloran, P.; Macdonald, H.; Holland, A.E. Telerehabilitation for Chronic Respiratory Disease. Cochrane Database Syst. Rev. 2021, 1, CD013040. [Google Scholar] [CrossRef]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. JMIR Rehabil Assist Technol 2017, 4, e7511. [Google Scholar] [CrossRef]
- Why Is Telerehabilitation so Important during the COVID-19 Pandemic? Available online: https://shrs.uq.edu.au/article/2020/05/why-telerehabilitation-so-important-during-covid-19-pandemic (accessed on 3 November 2021).
- Scherrenberg, M.; Frederix, I.; De Sutter, J.; Dendale, P. Use of Cardiac Telerehabilitation during COVID-19 Pandemic in Belgium. Acta Cardiol. 2021, 76, 773–776. [Google Scholar] [CrossRef]
- Scherrenberg, M.; Wilhelm, M.; Hansen, D.; Völler, H.; Cornelissen, V.; Frederix, I.; Kemps, H.; Dendale, P. The Future Is Now: A Call for Action for Cardiac Telerehabilitation in the COVID-19 Pandemic from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2021, 28, 524–540. [Google Scholar] [CrossRef]
- de Las Heras, J.C.; Tulppo, M.; Kiviniemi, A.M.; Hilberg, O.; Løkke, A.; Ekholm, S.; Catalán-Matamoros, D.; Bendstrup, E. Augmented Reality Glasses as a New Tele-Rehabilitation Tool for Home Use: Patients’ Perception and Expectations. Disabil. Rehabil. Assist. Technol. 2020, 1–7. [Google Scholar] [CrossRef]
- Cerdan, J.; Catalan-Matamoros, D.; Berg, S.W. Online Communication in a Rehabilitation Setting: Experiences of Patients with Chronic Conditions Using a Web Portal in Denmark. Patient Educ. Couns. 2017, 100, 2283–2289. [Google Scholar] [CrossRef]
- Paneroni, M.; Colombo, F.; Papalia, A.; Colitta, A.; Borghi, G.; Saleri, M.; Cabiaglia, A.; Azzalini, E.; Vitacca, M. Is Telerehabilitation a Safe and Viable Option for Patients with COPD? A Feasibility Study. COPD: J. Chronic Obstr. Pulm. Dis. 2015, 12, 217–225. [Google Scholar] [CrossRef]
- Hansen, H.; Bieler, T.; Beyer, N.; Godtfredsen, N.; Kallemose, T.; Frølich, A. COPD Online-Rehabilitation versus Conventional COPD Rehabilitation-Rationale and Design for a Multicenter Randomized Controlled Trial Study Protocol (CORe Trial). BMC Pulm. Med. 2017, 17, 140. [Google Scholar] [CrossRef]
- Hansen, H.; Bieler, T.; Beyer, N.; Kallemose, T.; Wilcke, J.T.; Østergaard, L.M.; Frost Andeassen, H.; Martinez, G.; Lavesen, M.; Frølich, A.; et al. Supervised Pulmonary Tele-Rehabilitation versus Pulmonary Rehabilitation in Severe COPD: A Randomised Multicentre Trial. Thorax 2020, 75, 413–421. [Google Scholar] [CrossRef]
- Telehealth: Secure and HIPAA-Compliant-SimplePractice. Available online: https://www.simplepractice.com/telehealth/ (accessed on 30 January 2021).
- Rayce, K.; Rosenbek Minet, L.; Kidholm, K.; Vestbo, J.; Pedersen, C.D.; Huniche, L. Telemediated Training in the Home as a Part of the Everyday Life and Practice With Very Severe Chronic Obstructive Pulmonary Disease. Qual. Health Res. 2020, 30, 2132–2145. [Google Scholar] [CrossRef]
- Telehealth for Physical Therapy. Available online: https://www.physitrack.com/telehealth (accessed on 30 January 2021).
- Dinesen, B.; Andersen, S.K.; Hejlesen, O.; Toft, E. Interaction between COPD Patients and Healthcare Professionals in a Cross-Sector Tele-Rehabilitation Programme. Stud. Health Technol. Inform. 2011, 169, 28–32. [Google Scholar] [PubMed]
- Hill, A.; Sppath, B. Telerehabilitation in Scotland: Current Initiatives and Recommendations for Future Development. Int. J. Telerehabilitation 2010, 2, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Randomization Plans: Never the Same Thing Twice! Available online: http://www.jerrydallal.com/random/randomize.htm (accessed on 19 January 2017).
- Bolton, C.E.; Bevan-Smith, E.F.; Blakey, J.D.; Crowe, P.; Elkin, S.L.; Garrod, R.; Greening, N.J.; Heslop, K.; Hull, J.H.; Man, W.D.-C.; et al. British Thoracic Society Guideline on Pulmonary Rehabilitation in Adults: Accredited by NICE. Thorax 2013, 68, ii1–ii30. [Google Scholar] [CrossRef]
- VAPA. Available online: https://www.eurostars-eureka.eu/project/id/10287 (accessed on 18 August 2020).
- Solution. Available online: https://optimov.com/?page_id=3006 (accessed on 20 September 2020).
- Products-Optimov. Available online: https://optimov.com/?page_id=1879 (accessed on 20 September 2020).
- Cerdán-de-las-Heras, J.; Balbino, F.; Løkke, A.; Catalán-Matamoros, D.; Hilberg, O.; Bendstrup, E. Tele-Rehabilitation Program in Idiopathic Pulmonary fibrosis—A Single-Center Randomized Trial. Int. J. Environ. Res. Public Health 2021, 18, 10016. [Google Scholar]
- Creative Commons—Attribution 4.0 International—CC BY 4.0. Available online: https://creativecommons.org/licenses/by/4.0/ (accessed on 4 October 2021).
- Medicin.dk–Information Om Medicin. Available online: http://medicin.dk/ (accessed on 21 August 2020).
- Lungeforeningen. Available online: https://www.lunge.dk/ (accessed on 21 August 2020).
- Helbredsprofilen.dk. Available online: https://helbredsprofilen.dk/da (accessed on 21 August 2020).
- Spis Rigtigt-Antiinflammatorisk Kost-YouTube. Available online: https://youtube.com/embed/w5fjXI6NHec (accessed on 26 August 2020).
- Spis Rigtigt-Frugt Og Grønt-YouTube. Available online: https://youtube.com/embed/5O479Caonrc (accessed on 26 August 2020).
- Råd Til Undervægtige-YouTube. Available online: https://youtube.com/embed/t1Haq6Gf5hA (accessed on 26 August 2020).
- Råd Til Overvægtige-YouTube. Available online: https://youtube.com/embed/UKdjxpVjqFA (accessed on 26 August 2020).
- Sundhedsstyrelsen. Nationale kliniske retningslinjer for rehabilitering af patienter med KOL (kronisk obstruktiv lungelidelse). Available online: https://www.sst.dk/-/media/Udgivelser/2018/National-Klinisk-Retningslinje-for-Rehabilitering-af-patienter-med-KOL.ashx?la=da&hash=81976AC77E8FCEF659052AE0A1ED378C18AEAC47 (accessed on 28 February 2021).
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An Official European Respiratory Society/American Thoracic Society Technical Standard: Field Walking Tests in Chronic Respiratory Disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef]
- Hecht, A.; Ma, S.; Porszasz, J.; Casaburi, R. Methodology for Using Long-Term Accelerometry Monitoring to Describe Daily Activity Patterns in COPD the COPD Clinical Research Network. COPD 2009, 2, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M. The St George’s Respiratory Questionnaire. Respir. Med. 1991, 85 (Suppl. B), 25–31, discussion 33–7. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Burge, A.T.; Cox, N.S.; Abramson, M.J.; Holland, A.E. Interventions for Promoting Physical Activity in People with Chronic Obstructive Pulmonary Disease (COPD). Cochrane Database Syst. Rev. 2020, 4, CD012626. [Google Scholar] [CrossRef]
- Puhan, M.A.; Mador, M.J.; Held, U.; Goldstein, R.; Guyatt, G.H.; Schünemann, H.J. Interpretation of Treatment Changes in 6-Minute Walk Distance in Patients with COPD. Eur. Respir. J. 2008, 32, 637–643. [Google Scholar] [CrossRef]
- Sohanpal, R.; Hooper, R.L.; Hames, R.; Priebe, S.; Taylor, S. S112 Estimating Participation Rates of COPD Patients in Pulmonary Rehabilitation and Self-Management Programmes: The Importance of Defining Participation. Thorax 2012, 67, A55. [Google Scholar] [CrossRef]
- McCoy, C.E. Understanding the Intention-to-Treat Principle in Randomized Controlled Trials. West. J. Emerg. Med. 2017, 18, 1075–1078. [Google Scholar] [CrossRef]
- Vogiatzis, I.; Nanas, S.; Kastanakis, E.; Georgiadou, O.; Papazahou, O.; Roussos, C. Dynamic Hyperinflation and Tolerance to Interval Exercise in Patients with Advanced COPD. Eur. Respir. J. 2004, 24, 385–390. [Google Scholar] [CrossRef]
- Dowman, L.M.; McDonald, C.F.; Hill, C.J.; Lee, A.L.; Barker, K.; Boote, C.; Glaspole, I.; Goh, N.S.L.; Southcott, A.M.; Burge, A.T.; et al. The Evidence of Benefits of Exercise Training in Interstitial Lung Disease: A Randomised Controlled Trial. Thorax 2017, 72, 610–619. [Google Scholar] [CrossRef]
- Yuen, H.K.; Lowman, J.D.; Oster, R.A.; de Andrade, J.A. Home-Based Pulmonary Rehabilitation for Patients With Idiopathic Pulmonary Fibrosis: A PILOT STUDY. J. Cardiopulm. Rehabil. Prev. 2019, 39, 281–284. [Google Scholar] [CrossRef]
- Yu, X.; Li, X.; Wang, L.; Liu, R.; Xie, Y.; Li, S.; Li, J. Pulmonary Rehabilitation for Exercise Tolerance and Quality of Life in IPF Patients: A Systematic Review and Meta-Analysis. Biomed Res. Int. 2019, 2019, 8498603. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Qian, H.; Yu, K.; Huang, Y. Nonadherence in Home-Based Pulmonary Rehabilitation Program for COPD Patients. Can. Respir. J. 2020, 2020, 5146765. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.J.; Scharloo, M.; Abbink, J.J.; van ’t Hul, A.J.; van Ranst, D.; Rudolphus, A.; Weinman, J.; Rabe, K.F.; Kaptein, A.A. Drop-out and Attendance in Pulmonary Rehabilitation: The Role of Clinical and Psychosocial Variables. Respir. Med. 2009, 103, 1564–1571. [Google Scholar] [CrossRef] [PubMed]


| Features | Explanation |
|---|---|
| Workout Sessions with VAPA | The patients trained 10–20 min 3–5 times a week at home with their individual and tailored VAPA using training aids, such as elastics, weights and a fitness step, to reach the highest workout intensity. The VAPA provided encouragement to continue training during the workout based on a decision support system collecting real time data from a biometric sensor attached to the patient’s chest. The decision support system follows, in real time, heart rate data tracked by a biometric sensor attached to the chest of the patient, and according to different parameters, such as age, gender and medication, adjusts the training intensity with easy–difficult exercises used in hospital-based rehabilitation, adapted for home-base execution and stimulating the patient’s aerobic–anaerobic workout. |
| E-Learning Packages | The patient had access to e-learning packages addressing psychological, medical, nutritional and physical aspects of COPD—in part supplied by relevant special data sources medicin.dk [29], lunge.dk [30] and helbredsprofilen.dk. [31], or created by dietitian students after in-depth interviews with pulmonary patients [32,33,34,35]. |
| Questionnaires | The patients filled out questionnaires regarding satisfaction, breathlessness, and adverse events reporting. |
| Video Consultation Sessions | Each patient met the physiotherapist in a video consultation to plan the rehabilitation program and to evaluate previous training experience. |
| Chat Sessions | Allowed the patient to interact with and obtain prompt answers from the physiotherapist. |
| Parameters | TR with VAPA n = 27 | Standard Rehab n = 27 | p |
|---|---|---|---|
| Male, n (%) | 16 (51.6) | 15 (48.4) | - |
| Age (years) * | 67.4 (10.2) | 72.5 (7.4) | 0.04 |
| Smoking Status § | |||
| Current, n (%) | 4 (16) | 3 (14.3) | - |
| Former, n (%) | 21 (84) | 18 (85.7) | - |
| Never, n (%) | 0 (0) | 0 (0) | - |
| Long-Term Oxygen Therapy, n (%) | 2 (7.4%) | 2 (7.4%) | - |
| FVC (% predicted) * | 67.4 (19.9) | 70.2 (17.9) | 0.60 |
| FEV1 (% predicted) * | 36.1 (14.1) | 32.8 (8.5) | 0.31 |
| FEV1 Ratio (% predicted) * | 48.6 (15.4) | 39.1 (17.5) | 0.04 |
| 6MWTD (m)* | 385.5 (86.9) | 366.6 (97.8) | 0.46 |
| 7-Day Pedometry * | 8601 (4831) | 9234 (7126). | 0.71 |
| 7dVMCPM * | 282.1 (133) | 358.3 (262) | 0.19 |
| SGRQ total * | 55.6 (13.5) | 60.6 (14.1) | 0.03 |
| SGRQ, Symptoms * | 56.15 (21.1) | 61.2 (23.5) | 0.85 |
| SGRQ, Activity * | 77.5 (14.35) | 76.8 (15.4) | 0.05 |
| SGRQ, Impact * | 42.8 (15.5) | 51.2 (15.9) | 0.18 |
| IADL * | 1.1 (1.1) | 2.2 (2.3) | 0.46 |
| GAD7 * | 3.3 (3.9) | 5.9 (6.6) | 0.41 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerdán-de-las-Heras, J.; Balbino, F.; Løkke, A.; Catalán-Matamoros, D.; Hilberg, O.; Bendstrup, E. Effect of a New Tele-Rehabilitation Program versus Standard Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2022, 11, 11. https://doi.org/10.3390/jcm11010011
Cerdán-de-las-Heras J, Balbino F, Løkke A, Catalán-Matamoros D, Hilberg O, Bendstrup E. Effect of a New Tele-Rehabilitation Program versus Standard Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine. 2022; 11(1):11. https://doi.org/10.3390/jcm11010011
Chicago/Turabian StyleCerdán-de-las-Heras, Jose, Fernanda Balbino, Anders Løkke, Daniel Catalán-Matamoros, Ole Hilberg, and Elisabeth Bendstrup. 2022. "Effect of a New Tele-Rehabilitation Program versus Standard Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease" Journal of Clinical Medicine 11, no. 1: 11. https://doi.org/10.3390/jcm11010011
APA StyleCerdán-de-las-Heras, J., Balbino, F., Løkke, A., Catalán-Matamoros, D., Hilberg, O., & Bendstrup, E. (2022). Effect of a New Tele-Rehabilitation Program versus Standard Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine, 11(1), 11. https://doi.org/10.3390/jcm11010011









