Systematic Review of Psychological Interventions for Quality of Life, Mental Health, and Hair Growth in Alopecia Areata and Scarring Alopecia
Abstract
:1. Introduction
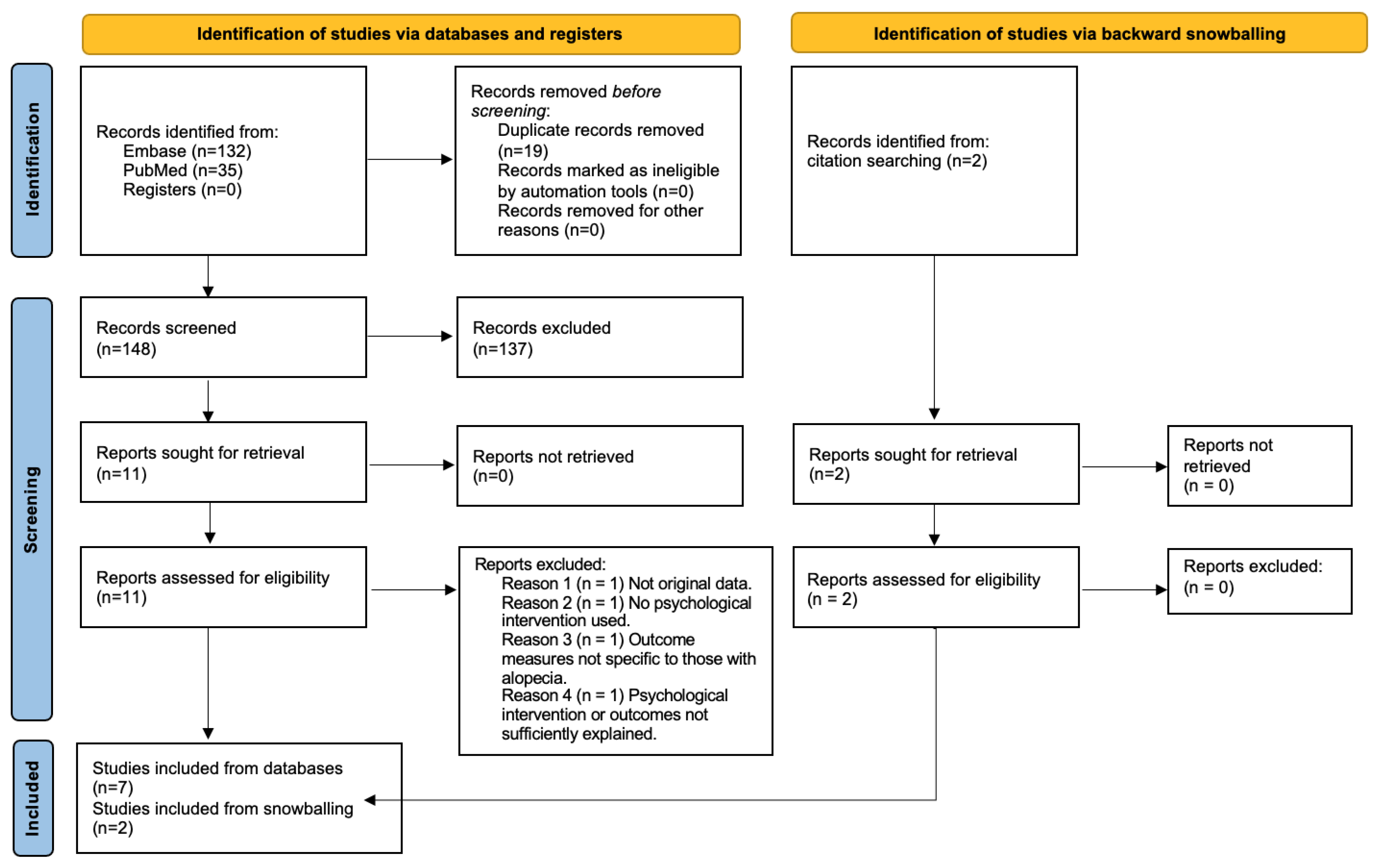
2. Methods
2.1. Search Strategy
2.2. Inclusion/Exclusion Criteria
2.3. Data Collection and Search Results
3. Results
3.1. Mindfulness
3.2. Collocated Behavioral Health Treatment
3.3. Hypnotherapy
| Study | Type of Hair Loss | Study Design | Sample Size | Intervention | Results |
|---|---|---|---|---|---|
| Gallo et al. (2017) [18] | Alopecia areata (moderate to severe) | Prospective cohort, with control | 16 (8 intervention, 8 control) | Eight-week Mindfulness-Based Stress Reduction in addition to ongoing AA medical treatment. | In MBSR group: Significant improvement in AA-QLI subjective symptoms and relationship impacts (maintained at 6 months) Significant improvement in Brief Symptom Inventory on anxiety (maintained at 6 months), phobia, overall psychological distress, and global severity index. |
| Harrison and Stepanek (1991) [32] | Refractory alopecia (scarring and non-scarring alopecia) | Pilot study | 5 | 10–12 forty-five-minute sessions of hypnotherapy over 3 months and recordings for home use. | All participants reported a feeling of well-being. Three patients: partial hair regrowth One patient: significant regrowth One patient: no change |
| Willemsen et al. (2006) [24] | 12 with extensive alopecia areata, 9 with alopecia totalis or universalis | Prospective cohort | 21 | In person hypnosis sessions every 3 weeks along with hypnosis twice weekly from a recording at home. | Significant improvement in Symptom Check List, anxiety, and depression scales. Significant hair regrowth in 12 patients. |
| Willemsen et al. (2010) [33] | Alopecia areata, alopecia totalis and universalis, all for at least 3 months prior to enrollment | Prospective cohort, with control, nonrandomized | 41 (20 intervention, 21 control) | 10 hypnotherapy sessions performed bimonthly along with daily hypnotherapy from a recording at home. No concurrent hair loss treatments. | At 6 months, the hypnotherapy group reported significantly greater reductions in depression, anxiety, and symptom burden scores. Eight patients from hypnosis group experienced (non-significant) hair growth. |
| Willemsen et al. (2011) [19] | Alopecia areata | Prospective cohort | 21 | 10 hypnotherapy sessions over 6-months and daily hypnosis recording at home. | At 6 months, the Symptom Check List, alexithymia, and Skindex-17 (dermatology related quality of life) scores all improved. This was maintained 6 months after treatment. |
| Teshima et al. (1991) [20] | Alopecia universalis (refractory) | Clinical trial, not blinded | 11 (6 intervention, 5 control) | Psychoimmunotherapy: Six patients underwent 4 months of 30-min relaxation therapy in addition to oral prednisolone and later cyclosporine given to all participants. | In the psychoimmunotherapy group, five/six participants saw hair regrowth. There was also increases in scalp blood flow. In immunotherapy only group: one/five participants had regrowth. |
| Matzer et al. (2011) [36] | Alopecia areata | Cross sectional | 45 | Interview at baseline and 6 months evaluating coping strategies and disease burden. | Active and open coping strategies were associated with reduced disease burden in chronic AA. |
| Heapy et al. (2021) [21] | Alopecia areata | Case series | 5 (data excluded from 1 due to missing data) | Eight-session mindfulness-based cognitive therapy (MBCT) intervention | Reduction in idiographic measures of social anxiety, with greater effects from baseline to follow-up than baseline to postintervention. Significant improvement in measures of well-being from baseline to follow-up in two participants who implemented MBCT exercises frequently between sessions. |
| Gorbatenko-Roth et al. (2021) [22] | Alopecia areata | Randomized, controlled pilot study | 30 (20 intervention, 10 control) | AA-specific collocated behavioral health (CLBH) treatment, involving up to 2, 30-min sessions. | CLBH group reported better psychosocial functioning than control for most outcomes, although differences were nonsignificant CLBH was perceived as beneficial; 100% reported increased dermatology care satisfaction, 90% endorsed addressing psychosocial issues during dermatology visits. |
| Item | Randomization /2 1 Point if Randomization Is Mentioned 1 Additional Point if the Method of Randomization Is Appropriate | Blinding /2 1 Point if Blinding Is Mentioned 1 Additional Point if the Method of Blinding Is Appropriate Deduct 1 Point if the Method of Blinding Is Inappropriate | An Account of All Patients /1 The Fate of All Patients in the Trial Is Known. If There Are No Data, the Reason Is Stated | Total Score /5 Max 5 Points |
|---|---|---|---|---|
| Gallo et al. (2017) [18] | 0 No randomization | 0 No mention of blinding | 1 Results were reported with eight individuals in each group, implying all 16 participants completed the study. | 1 |
| Harrison and Stepanek (1991) [32] | 0 No randomization/control group | 0 No blinding | 0 A total of 5/12 patients completed the study, but authors do not state why 7 did not complete the study. | 0 |
| Willemsen et al. (2006) [24] | 0 No randomization/control group | 0 No blinding | 1 Only 21/28 patients completed the study, but authors state that 7 patients withdrew due to lack of motivation. | 1 |
| Willemsen et al. (2010) [33] | 0 A nonrandomized controlled study protocol was selected for ethical reasons | 0 No mention of blinding | 1 Results were reported with 20 treatment patients and 21 control patients, implying all 41 participants completed the study. | 1 |
| Willemsen et al. (2011) [19] | 0 No randomization | 0 No blinding | 1 A total of 24 patients were included in the study, and 3 patients dropped out (one due to lack of motivation, two due to failure to concentrate while listening to the audiotape for self-hypnosis). | 1 |
| Teshima et al. (1991) [20] | 0 No randomization | 0 No blinding | 1 Results reported for 11/11 patients. | 1 |
| Matzer et al. (2011) [36] | 0 No randomization | 0 No blinding | 1 Results reported for 45/45 patients. Two could not be contacted for 6-month follow up. | 1 |
| Heapy et al. (2021) [21] | 0 No randomization | 0 No blinding | 1 Results reported for four/five patients (one excluded due to incomplete responses). | 1 |
| Gorbatenko-Roth et al. (2021) [22] | 2 Randomized appropriately | 0 No blinding | 0 Participation and 1-month follow-up rates were 68% and 90%, respectively. | 2 |
3.4. Psychoimmunotherapy
3.5. Coping Strategies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hunt, N.; McHale, S. The Psychological Impact of Alopecia. BMJ 2005, 331, 951–953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phillips, T.G.; Slomiany, W.P.; Allison, R. Hair Loss: Common Causes and Treatment. Am. Fam. Physician 2017, 96, 371–378. [Google Scholar] [PubMed]
- Kuty-Pachecka, M. Psychological and psychopathological factors in alopecia areata. Psychiatr. Pol. 2015, 49, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Ghanizadeh, A.; Ayoobzadehshirazi, A. A Review of Psychiatric Disorders Comorbidities in Patients with Alopecia Areata. Int. J. Trichol. 2014, 6, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koo, J.Y.; Shellow, W.V.; Hallman, C.P.; Edwards, J.E. Alopecia Areata and Increased Prevalence of Psychiatric Disorders. Int. J. Dermatol. 1994, 33, 849–850. [Google Scholar] [CrossRef]
- Liakopoulou, M.; Alifieraki, T.; Katideniou, A.; Kakourou, T.; Tselalidou, E.; Tsiantis, J.; Stratigos, J. Children with Alopecia Areata: Psychiatric Symptomatology and Life Events. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 678–684. [Google Scholar] [CrossRef]
- Aşkın, Ö.; Koyuncu, Z.; Serdaroğlu, S. Association of Alopecia with Self-Esteem in Children and Adolescents. Int. J. Adolesc. Med. Health 2020, 34, 315–318. [Google Scholar] [CrossRef]
- Gupta, S.; Goyal, I.; Mahendra, A. Quality of Life Assessment in Patients with Androgenetic Alopecia. Int. J. Trichol. 2019, 11, 147. [Google Scholar] [CrossRef]
- Chiang, Y.Z.; Bundy, C.; Griffiths, C.E.M.; Paus, R.; Harries, M.J. The Role of Beliefs: Lessons from a Pilot Study on Illness Perception, Psychological Distress and Quality of Life in Patients with Primary Cicatricial Alopecia. Br. J. Dermatol. 2015, 172, 130–137. [Google Scholar] [CrossRef]
- Mounsey, A.L.; Reed, S.W. Diagnosing and Treating Hair Loss. Am. Fam. Physician 2009, 80, 356–362. [Google Scholar]
- Salisbury, B.; Tadi, P. 5 Alpha Reductase Inhibitors; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Harries, M.J.; Sun, J.; Paus, R.; King, L.E. Management of Alopecia Areata. BMJ 2010, 341, c3671. [Google Scholar] [CrossRef]
- Simakou, T.; Butcher, J.P.; Reid, S.; Henriquez, F.L. Alopecia Areata: A Multifactorial Autoimmune Condition. J. Autoimmun. 2019, 98, 74–85. [Google Scholar] [CrossRef] [Green Version]
- Starace, M.; Orlando, G.; Alessandrini, A.; Piraccini, B.M. Female Androgenetic Alopecia: An Update on Diagnosis and Management. Am. J. Clin. Dermatol. 2020, 21, 69–84. [Google Scholar] [CrossRef]
- Pekmezci, E.; Türkoğlu, M. Minoxidil Acts as an Antiandrogen: A Study of 5α-Reductase Type 2 Gene Expression in a Human Keratinocyte Cell Line. Acta Dermatovenerol. Croat. 2017, 25, 271–275. [Google Scholar]
- Cranwell, W.; Sinclair, R. Male Androgenetic Alopecia. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A., Hershman, J.M., Kaltsas, G., Koch, C., Kopp, P., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Tosti, A.; Bellavista, S.; Iorizzo, M. Alopecia Areata: A Long Term Follow-up Study of 191 Patients. J. Am. Acad. Dermatol. 2006, 55, 438–441. [Google Scholar] [CrossRef]
- Gallo, R.; Chiorri, C.; Gasparini, G.; Signori, A.; Burroni, A.; Parodi, A. Can Mindfulness-Based Interventions Improve the Quality of Life of Patients with Moderate/Severe Alopecia Areata? A Prospective Pilot Study. J. Am. Acad. Dermatol. 2017, 76, 757–759. [Google Scholar] [CrossRef] [Green Version]
- Willemsen, R.; Haentjens, P.; Roseeuw, D.; Vanderlinden, J. Hypnosis and Alopecia Areata: Long-Term Beneficial Effects on Psychological Well-Being. Acta Derm. Venereol. 2011, 91, 35–39. [Google Scholar] [CrossRef] [Green Version]
- Teshima, H.; Sogawa, H.; Mizobe, K.; Kuroki, N.; Nakagawa, T. Application of Psychoimmunotherapy in Patients with Alopecia Universalis. Psychother. Psychosom. 1991, 56, 235–241. [Google Scholar] [CrossRef]
- Heapy, C.; Norman, P.; Cockayne, S.; Thompson, A. The Effectiveness of Mindfulness-Based Cognitive Therapy for Social Anxiety in People with Alopecia Areata: A Multiple-Baseline Single-Group Case Series Design. Br. J. Dermatol. 2021, 185, e105. [Google Scholar] [CrossRef]
- Gorbatenko-Roth, K.; Hodges, J.S.; Lifson, D.; Golm, M.; Kranz, D.; Windenburg, D.; Hordinsky, M. Integrating Colocated Behavioral Health Care into a Dermatology Clinic: A Prospective Randomized Controlled Treatment Pilot Study in Patients with Alopecia Areata. J. Am. Acad. Dermatol. 2021, 84, 1487–1489. [Google Scholar] [CrossRef]
- Cipriani, R.; Perini, G.I.; Rampinelli, S. Paroxetine in Alopecia Areata. Int. J. Dermatol. 2001, 40, 600–601. [Google Scholar] [CrossRef] [PubMed]
- Willemsen, R.; Vanderlinden, J.; Deconinck, A.; Roseeuw, D. Hypnotherapeutic Management of Alopecia Areata. J. Am. Acad. Dermatol. 2006, 55, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Perini, G.; Zara, M.; Cipriani, R.; Carraro, C.; Preti, A.; Gava, F.; Coghi, P.; Peserico, A. Imipramine in Alopecia Areata. A Double-Blind, Placebo-Controlled Study. Psychother. Psychosom. 1994, 61, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Barton, V.R.; Toussi, A.; Awasthi, S.; Kiuru, M. Treatment of Pediatric Alopecia Areata: A Systematic Review. J. Am. Acad. Dermatol. 2022, 86, 1318–1334. [Google Scholar] [CrossRef]
- Tkachenko, E.; Okhovat, J.-P.; Manjaly, P.; Huang, K.P.; Senna, M.M.; Mostaghimi, A. Complementary & Alternative Medicine for Alopecia Areata: A Systematic Review. J. Am. Acad. Dermatol. 2019, 88, 131–143. [Google Scholar] [CrossRef]
- Toussi, A.; Barton, V.R.; Le, S.T.; Agbai, O.N.; Kiuru, M. Psychosocial and Psychiatric Comorbidities and Health-Related Quality of Life in Alopecia Areata: A Systematic Review. J. Am. Acad. Dermatol. 2021, 85, 162–175. [Google Scholar] [CrossRef]
- Fabbrocini, G.; Panariello, L.; de Vita, V.; Vincenzi, C.; Lauro, C.; Nappo, D.; Ayala, F.; Tosti, A. Quality of Life in Alopecia Areata: A Disease-Specific Questionnaire. J. Eur. Acad. Dermatol. Venereol. 2013, 27, e276–e281. [Google Scholar] [CrossRef] [Green Version]
- Derogatis, L.R. BSI Brief Symptom Inventory: Administration, Scoring and Procedures Manual, 4th ed.; National Computer Systems: Minneapolis, MN, USA, 1993. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Harrison, P.V.; Stepanek, P. Hypnotherapy for Alopecia Areata. Br. J. Dermatol. 1991, 124, 509–510. [Google Scholar] [CrossRef]
- Willemsen, R.; Haentjens, P.; Roseeuw, D.; Vanderlinden, J. Hypnosis in Refractory Alopecia Areata Significantly Improves Depression, Anxiety, and Life Quality but Not Hair Regrowth. J. Am. Acad. Dermatol. 2010, 62, 517–518. [Google Scholar] [CrossRef]
- Sampogna, F.; Spagnoli, A.; Di Pietro, C.; Pagliarello, C.; Paradisi, A.; Tabolli, S.; Abeni, D. Field Performance of the Skindex-17 Quality of Life Questionnaire: A Comparison with the Skindex-29 in a Large Sample of Dermatological Outpatients. J. Investig. Dermatol. 2013, 133, 104–109. [Google Scholar] [CrossRef] [Green Version]
- Lins, L.; Carvalho, F.M. SF-36 Total Score as a Single Measure of Health-Related Quality of Life: Scoping Review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef]
- Matzer, F.; Egger, J.W.; Kopera, D. Psychosocial Stress and Coping in Alopecia Areata: A Questionnaire Survey and Qualitative Study among 45 Patients. Acta Derm. Venereol. 2011, 91, 318–327. [Google Scholar] [CrossRef] [Green Version]
- McElwee, K.J.; Gilhar, A.; Tobin, D.J.; Ramot, Y.; Sundberg, J.P.; Nakamura, M.; Bertolini, M.; Inui, S.; Tokura, Y.; King, L.E.; et al. What Causes Alopecia Areata?: Section Editors: Ralf Paus, Manchester/Lübeck and Raymond Cho, San Francisco. Exp. Dermatol. 2013, 22, 609–626. [Google Scholar] [CrossRef]
- Tobin, A.M. Unravelling the Microbiome in Psoriasis. Br. J. Dermatol. 2019, 181, 1124–1125. [Google Scholar] [CrossRef]
- Gilhar, A.; Landau, M.; Assy, B.; Shalaginov, R.; Serafimovich, S.; Kalish, R.S. Mediation of Alopecia Areata by Cooperation Between CD4+ and CD8+ T Lymphocytes: Transfer to Human Scalp Explants on Prkdc scid Mice. Arch. Dermatol. 2002, 138, 916–922. [Google Scholar] [CrossRef] [Green Version]
- McELWEE; Spiers; Oliver Partial Restoration of Hair Growth in the DEBR Model for Alopecia Areata after in Vivo Depletion of CD4+ T Cells. Br. J. Dermatol. 1999, 140, 432–437. [CrossRef]
- Black, D.S.; Slavich, G.M. Mindfulness Meditation and the Immune System: A Systematic Review of Randomized Controlled Trials. Ann. N. Y. Acad. Sci. 2016, 1373, 13–24. [Google Scholar] [CrossRef] [Green Version]
- Morgan, N.; Irwin, M.R.; Chung, M.; Wang, C. The Effects of Mind-Body Therapies on the Immune System: Meta-Analysis. PLoS ONE 2014, 9, e100903. [Google Scholar] [CrossRef] [Green Version]
- Bain, K.A.; McDonald, E.; Moffat, F.; Tutino, M.; Castelino, M.; Barton, A.; Cavanagh, J.; Ijaz, U.Z.; Siebert, S.; McInnes, I.B.; et al. Alopecia Areata Is Characterized by Dysregulation in Systemic Type 17 and Type 2 Cytokines, Which May Contribute to Disease-Associated Psychological Morbidity. Br. J. Dermatol. 2020, 182, 130–137. [Google Scholar] [CrossRef] [Green Version]
- İslamoğlu, Z.G.K.; Demirbaş, A. Evaluation of Complete Blood Cell and Inflammatory Parameters in Patients with Alopecia Areata: Their Association with Disease Severity. J. Cosmet. Dermatol. 2020, 19, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Peters, E.M.J.; Arck, P.C.; Paus, R. Hair Growth Inhibition by Psychoemotional Stress: A Mouse Model for Neural Mechanisms in Hair Growth Control. Exp. Dermatol. 2006, 15, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.Y.; Nam, Y.J.; Kang, S.; Choi, E.J.; Han, I.; Kim, J.; Kim, D.H.; An, J.H.; Lee, S.; Lee, M.H.; et al. The Local Hypothalamic-Pituitary-Adrenal Axis in Cultured Human Dermal Papilla Cells. BMC Mol. Cell Biol. 2020, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Koncz, A.; Demetrovics, Z.; Takacs, Z.K. Meditation Interventions Efficiently Reduce Cortisol Levels of At-Risk Samples: A Meta-Analysis. Health Psychol. Rev. 2021, 15, 56–84. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maloh, J.; Engel, T.; Natarelli, N.; Nong, Y.; Zufall, A.; Sivamani, R.K. Systematic Review of Psychological Interventions for Quality of Life, Mental Health, and Hair Growth in Alopecia Areata and Scarring Alopecia. J. Clin. Med. 2023, 12, 964. https://doi.org/10.3390/jcm12030964
Maloh J, Engel T, Natarelli N, Nong Y, Zufall A, Sivamani RK. Systematic Review of Psychological Interventions for Quality of Life, Mental Health, and Hair Growth in Alopecia Areata and Scarring Alopecia. Journal of Clinical Medicine. 2023; 12(3):964. https://doi.org/10.3390/jcm12030964
Chicago/Turabian StyleMaloh, Jessica, Tess Engel, Nicole Natarelli, Yvonne Nong, Alina Zufall, and Raja K. Sivamani. 2023. "Systematic Review of Psychological Interventions for Quality of Life, Mental Health, and Hair Growth in Alopecia Areata and Scarring Alopecia" Journal of Clinical Medicine 12, no. 3: 964. https://doi.org/10.3390/jcm12030964






