Outcomes of “Over the Top” Anterior Cruciate Ligament Reconstruction Associated with a Lateral Extra-Articular Tenodesis in Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
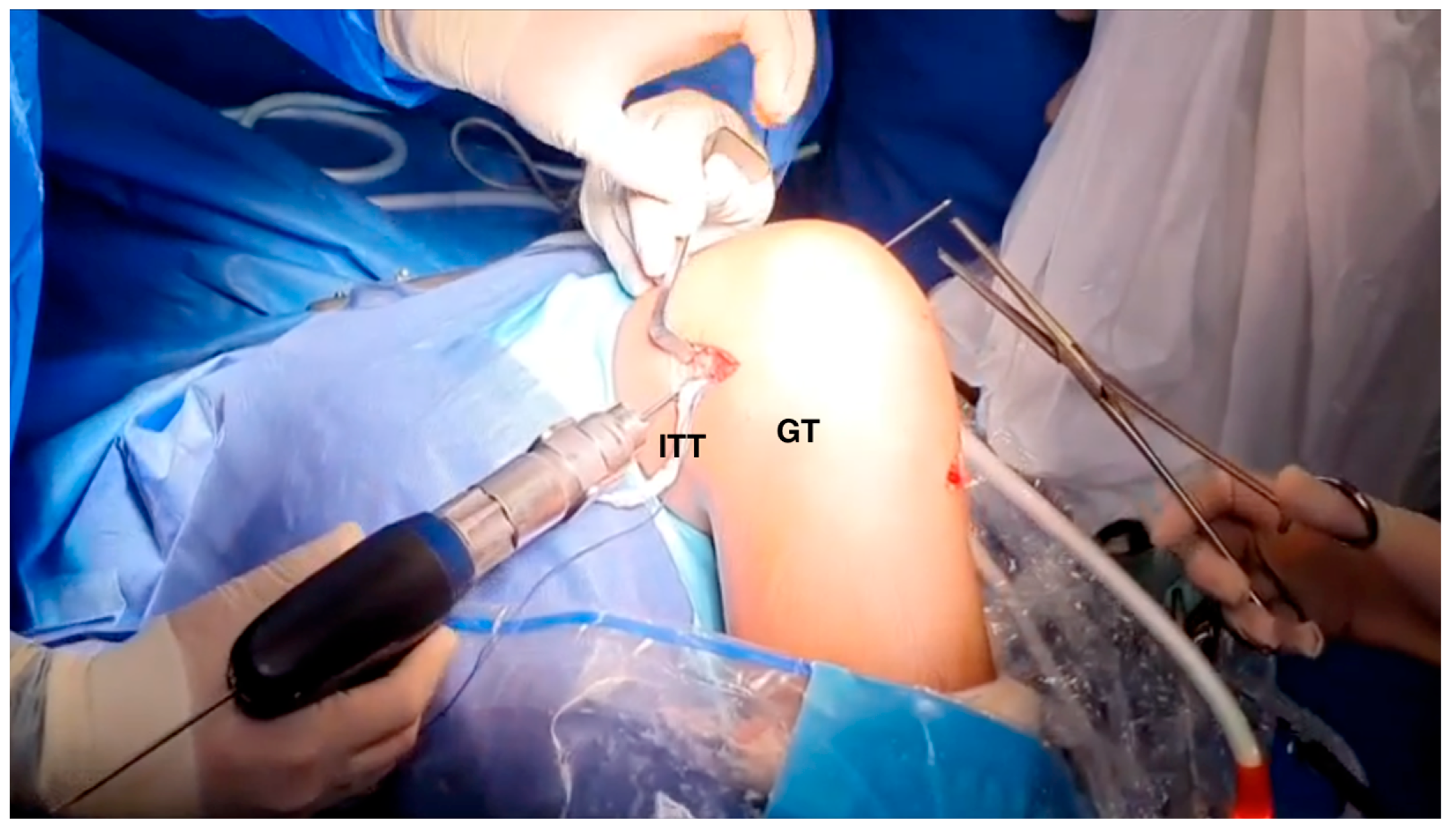
2.2. Surgical Technique
2.3. Modified Lemaire
2.4. Postoperative Protocol
2.5. Follow-Up
2.6. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- LaBella, C.R.; Hennrikus, W.; Hewett, T.E. Council on Sports Medicine and Fitness, and Section on Orthopaedics Anterior Cruciate Ligament Injuries: Diagnosis, Treatment, and Prevention. Pediatrics 2014, 133, e1437–e1450. [Google Scholar] [CrossRef]
- Pike, A.N.; Patzkowski, J.C.; Bottoni, C.R. Meniscal and Chondral Pathology Associated With Anterior Cruciate Ligament Injuries. J. Am. Acad. Orthop. Surg. 2019, 27, 75–84. [Google Scholar] [CrossRef]
- Buller, L.T.; Best, M.J.; Baraga, M.G.; Kaplan, L.D. Trends in Anterior Cruciate Ligament Reconstruction in the United States. Orthop. J. Sports Med. 2015, 3, 2325967114563664. [Google Scholar] [CrossRef]
- Tepolt, F.A.; Feldman, L.; Kocher, M.S. Trends in Pediatric ACL Reconstruction From the PHIS Database. J. Pediatr. Orthop. 2018, 38, e490–e494. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P.; Järvinen, M. Knee Ligament Injuries in Adolescents. Eight Year Follow-up of Conservative Management. J. Bone Joint Surg. Br. 1988, 70, 772–776. [Google Scholar] [CrossRef] [PubMed]
- Joseph, S.M.; Huleatt, J.B.; Vogel-Abernathie, L.A.; Pace, J.L. Treatment of ACL Tears in the Skeletally Immature Patient. Sports Med. Arthrosc. Rev. 2018, 26, 153–156. [Google Scholar] [CrossRef]
- Dingel, A.; Aoyama, J.; Ganley, T.; Shea, K. Pediatric ACL Tears: Natural History. J. Pediatr. Orthop. 2019, 39, S47–S49. [Google Scholar] [CrossRef] [PubMed]
- Ramski, D.E.; Kanj, W.W.; Franklin, C.C.; Baldwin, K.D.; Ganley, T.J. Anterior Cruciate Ligament Tears in Children and Adolescents: A Meta-Analysis of Nonoperative versus Operative Treatment. Am. J. Sports Med. 2014, 42, 2769–2776. [Google Scholar] [CrossRef] [PubMed]
- Fabricant, P.D.; Kocher, M.S. Management of ACL Injuries in Children and Adolescents. J. Bone Joint Surg. Am. 2017, 99, 600–612. [Google Scholar] [CrossRef]
- Pagliazzi, G.; Cuzzolin, M.; Pacchiarini, L.; Delcogliano, M.; Filardo, G.; Candrian, C. Physeal-Sparing ACL Reconstruction Provides Better Knee Laxity Restoration but Similar Clinical Outcomes to Partial Transphyseal and Complete Transphyseal Approaches in the Pediatric Population: A Systematic Review and Meta-Analysis. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 206–218. [Google Scholar] [CrossRef]
- Wong, S.E.; Feeley, B.T.; Pandya, N.K. Comparing Outcomes Between the Over-the-Top and All-Epiphyseal Techniques for Physeal-Sparing ACL Reconstruction: A Narrative Review. Orthop. J. Sports Med. 2019, 7, 2325967119833689. [Google Scholar] [CrossRef]
- Nagai, K.; Rothrauff, B.B.; Li, R.T.; Fu, F.H. Over-the-Top ACL Reconstruction Restores Anterior and Rotatory Knee Laxity in Skeletally Immature Individuals and Revision Settings. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 538–543. [Google Scholar] [CrossRef]
- Zaffagnini, S.; Marcheggiani Muccioli, G.M.; Grassi, A.; Roberti di Sarsina, T.; Raggi, F.; Signorelli, C.; Urrizola, F.; Spinnato, P.; Rimondi, E.; Marcacci, M. Over-the-Top ACL Reconstruction Plus Extra-Articular Lateral Tenodesis With Hamstring Tendon Grafts: Prospective Evaluation With 20-Year Minimum Follow-up. Am. J. Sports Med. 2017, 45, 3233–3242. [Google Scholar] [CrossRef]
- Roberti di Sarsina, T.; Macchiarola, L.; Signorelli, C.; Grassi, A.; Raggi, F.; Marcheggiani Muccioli, G.M.; Zaffagnini, S. Anterior Cruciate Ligament Reconstruction with an All-Epiphyseal “over-the-Top” Technique Is Safe and Shows Low Rate of Failure in Skeletally Immature Athletes. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 498–506. [Google Scholar] [CrossRef]
- Lanzetti, R.M.; Pace, V.; Ciompi, A.; Perugia, D.; Spoliti, M.; Falez, F.; Auro, C. Over the Top Anterior Cruciate Ligament Reconstruction in Patients with Open Physes: A Long-Term Follow-up Study. Int. Orthop. 2020, 44, 771–778. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Gómez Cáceres, A.; Mariño, I.T.; Martínez Malo, F.J.; Vieitez Riestra, I.; Idiart, R.P. “Over-the-Top” Anterior Cruciate Ligament Reconstruction Associated With a Lateral Extra-Articular Tenodesis in Children. Arthrosc. Tech. 2023, 12, e441–e448. [Google Scholar] [CrossRef]
- Kaeding, C.C.; Pedroza, A.D.; Reinke, E.K.; Huston, L.J.; MOON Consortium; Spindler, K.P. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am. J. Sports Med. 2015, 43, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Ho, B.; Edmonds, E.W.; Chambers, H.G.; Bastrom, T.P.; Pennock, A.T. Risk Factors for Early ACL Reconstruction Failure in Pediatric and Adolescent Patients: A Review of 561 Cases. J. Pediatr. Orthop. 2018, 38, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Littlefield, C.P.; Belk, J.W.; Houck, D.A.; Kraeutler, M.J.; LaPrade, R.F.; Chahla, J.; McCarty, E.C. The Anterolateral Ligament of the Knee: An Updated Systematic Review of Anatomy, Biomechanics, and Clinical Outcomes. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 37, 1654–1666. [Google Scholar] [CrossRef] [PubMed]
- Perelli, S.; Costa, G.G.; Terron, V.M.; Formagnana, M.; Bait, C.; Espregueira-Mendes, J.; Monllau, J.C. Combined Anterior Cruciate Ligament Reconstruction and Modified Lemaire Lateral Extra-Articular Tenodesis Better Restores Knee Stability and Reduces Failure Rates Than Isolated Anterior Cruciate Ligament Reconstruction in Skeletally Immature Patients. Am. J. Sports Med. 2022, 50, 3778–3785. [Google Scholar] [CrossRef] [PubMed]
- Sena, M.; Chen, J.; Dellamaggioria, R.; Coughlin, D.G.; Lotz, J.C.; Feeley, B.T. Dynamic Evaluation of Pivot-Shift Kinematics in Physeal-Sparing Pediatric Anterior Cruciate Ligament Reconstruction Techniques. Am. J. Sports Med. 2013, 41, 826–834. [Google Scholar] [CrossRef]
- Kang, H.; Dong, C.; Wang, F. Small Hamstring Autograft Is Defined by a Cut-off Diameter of 7 Mm and Not Recommended with Allograft Augmentation in Single-Bundle ACL Reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3650–3659. [Google Scholar] [CrossRef] [PubMed]
- Snaebjörnsson, T.; Hamrin-Senorski, E.; Svantesson, E.; Karlsson, L.; Engebretsen, L.; Karlsson, J.; Samuelsson, K. Graft Diameter and Graft Type as Predictors of Anterior Cruciate Ligament Revision: A Cohort Study Including 18,425 Patients from the Swedish and Norwegian National Knee Ligament Registries. J. Bone Joint Surg. Am. 2019, 101, 1812–1820. [Google Scholar] [CrossRef] [PubMed]
- Perkins, C.A.; Busch, M.T.; Christino, M.; Herzog, M.M.; Willimon, S.C. Allograft Augmentation of Hamstring Anterior Cruciate Ligament Autografts Is Associated With Increased Graft Failure in Children and Adolescents. Am. J. Sports Med. 2019, 47, 1576–1582. [Google Scholar] [CrossRef]
- Spragg, L.; Chen, J.; Mirzayan, R.; Love, R.; Maletis, G. The Effect of Autologous Hamstring Graft Diameter on the Likelihood for Revision of Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Helito, C.P.; da Silva, A.G.M.; Sobrado, M.F.; Guimarães, T.M.; Gobbi, R.G.; Pécora, J.R. Small Hamstring Tendon Graft for Anterior Cruciate Ligament Reconstruction Combined With Anterolateral Ligament Reconstruction Results in the Same Failure Rate as Larger Hamstring Tendon Graft Reconstruction Alone. Arthrosc. J. Arthrosc. Relat. Surg. 2023, 39, 1671–1679. [Google Scholar] [CrossRef]
- Zaffagnini, S.; Golanò, P.; Farinas, O.; Depasquale, V.; Strocchi, R.; Cortecchia, S.; Marcacci, M.; Visani, A. Vascularity and Neuroreceptors of the Pes Anserinus: Anatomic Study. Clin. Anat. 2003, 16, 19–24. [Google Scholar] [CrossRef]
- Papachristou, G.; Nikolaou, V.; Efstathopoulos, N.; Sourlas, J.; Lazarettos, J.; Frangia, K.; Papalois, A. ACL Reconstruction with Semitendinosus Tendon Autograft without Detachment of Its Tibial Insertion: A Histologic Study in a Rabbit Model. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 1175–1180. [Google Scholar] [CrossRef]
- Grassi, A.; Pizza, N.; Macchiarola, L.; Lucidi, G.A.; Stefanelli, F.; Dal Fabbro, G.; Marcacci, M.; Zaffagnini, S. Over-the-Top Anterior Cruciate Ligament (ACL) Reconstruction plus Lateral Plasty with Hamstrings in High-School Athletes: Results at 10 Years. Knee 2021, 33, 226–233. [Google Scholar] [CrossRef]
- Vari, N.; Marot, V.; Ripoll, T.; Vieira, T.D.; Martinel, V.; Bérard, E.; Cavaignac, E. Preserving the Semitendinosus Distal Attachment Is Associated With Improved Graft Remodeling After ACL Reconstruction. Am. J. Sports Med. 2023, 51, 2064–2072. [Google Scholar] [CrossRef] [PubMed]
- Ruffilli, A.; Pagliazzi, G.; Ferranti, E.; Busacca, M.; Capannelli, D.; Buda, R. Hamstring Graft Tibial Insertion Preservation versus Detachment in Anterior Cruciate Ligament Reconstruction: A Prospective Randomized Comparative Study. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2016, 26, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Beischer, S.; Gustavsson, L.; Senorski, E.H.; Karlsson, J.; Thomeé, C.; Samuelsson, K.; Thomeé, R. Young Athletes Who Return to Sport Before 9 Months After Anterior Cruciate Ligament Reconstruction Have a Rate of New Injury 7 Times That of Those Who Delay Return. J. Orthop. Sports Phys. Ther. 2020, 50, 83–90. [Google Scholar] [CrossRef]
- Ardern, C.L.; Ekås, G.; Grindem, H.; Moksnes, H.; Anderson, A.; Chotel, F.; Cohen, M.; Forssblad, M.; Ganley, T.J.; Feller, J.A.; et al. 2018 International Olympic Committee Consensus Statement on Prevention, Diagnosis and Management of Paediatric Anterior Cruciate Ligament (ACL) Injuries. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 989–1010. [Google Scholar] [CrossRef] [PubMed]
- Nagelli, C.V.; Hewett, T.E. Should Return to Sport Be Delayed Until 2 Years After Anterior Cruciate Ligament Reconstruction? Biological and Functional Considerations. Sports Med. Auckl. NZ 2017, 47, 221–232. [Google Scholar] [CrossRef]
- Gokeler, A.; Dingenen, B.; Hewett, T.E. Rehabilitation and Return to Sport Testing After Anterior Cruciate Ligament Reconstruction: Where Are We in 2022? Arthrosc. Sports Med. Rehabil. 2022, 4, e77–e82. [Google Scholar] [CrossRef]
- Felix, E.C.R.; Alonso, A.C.; Brech, G.C.; Fernandes, T.L.; de Almeida, A.M.; Luna, N.M.S.; Soares-Junior, J.M.; Baracat, E.C.; Hernandez, A.J.; Greve, J.M.D. Is 12 Months Enough to Reach Function after Athletes’ ACL Reconstruction: A Prospective Longitudinal Study. Clinics 2022, 77, 100092. [Google Scholar] [CrossRef]





| Patient | Gender | Age | Injuries | Side | Treatment | Follow-Up |
|---|---|---|---|---|---|---|
| 1 | Male | 14 | ACL + lateral meniscus tear | Right | ACL reconstruction + meniscal suture | 50 |
| 2 | Female | 14 | ACL | Left | ACL reconstruction | 44 |
| 3 | Male | 13 | ACL + medial meniscus bucket handle tear | Left | ACL reconstruction + meniscal suture | 39 |
| 4 | Male | 14 | ACL + medial meniscus tear | Left | ACL reconstruction + meniscal suture | 37 |
| 5 | Male | 13 | ACL + medial and lateral meniscal tears | Right | ACL reconstruction + meniscal suture | 32 |
| 6 | Male | 14 | ACL | Right | ACL reconstruction | 28 |
| 7 | Male | 13 | ACL | Left | ACL reconstruction | 25 |
| 8 | Male | 12 | ACL | Right | ACL reconstruction | 22 |
| 9 | Male | 14 | ACL + medial meniscus bucket handle tear | Right | ACL recunstruction + partial meniscectomy | 10 |
| 10 | Male | 13 | ACL + lateral meniscus radial tear | Left | ACL reconstruction + parcial meniscectomy | 9 |
| 11 | Male | 13 | ACL | Right | ACL reconstruction | 13 |
| 12 | Male | 11 | ACL | Right | ACL reconstruction | 6 |
| Patient | Lysholm Score | Tegner Test | IKDC Score | KT-1000 Difference | Mobility | Pivot Shift | Lachman | Anterior Drawer | Posterior Drawer |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 100 | 9 | 99.4 | −1.5 | Full ROM | - | - | - | - |
| 2 | 100 | 9 | 96.4 | 3 | Full ROM | - | - | - | - |
| 3 | 100 | 9 | 96.4 | 1.5 | Full ROM | - | - | - | - |
| 4 | 55 | 9 | 59.5 | 3 | Full ROM | slight | - | +1 | - |
| 5 | 100 | 9 | 98.2 | 0 | Full ROM | - | +1A | - | - |
| 6 | 100 | 9 | 97.6 | 3.5 | Full ROM | - | - | +1 | - |
| 7 | 100 | 9 | 90.5 | −1 | Full ROM | - | - | - | - |
| 8 | 86 | 9 | 90.5 | 0 | Full ROM | - | - | - | - |
| 9 | 100 | 9 | 99.4 | 0 | Full ROM | - | - | - | - |
| 10 | 100 | 9 | 97.6 | 2 | Full ROM | - | - | - | - |
| 11 | 100 | 9 | 97.6 | 1 | Full ROM | - | - | - | - |
| 12 | 100 | 9 | 96.4 | 0 | Full ROM- | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomez-Caceres, A.; Tamimi-Mariño, I.; Martinez-Malo, F.J.; Idiart-Charrier, R.P.; Vieitez-Riestra, I.; Medina-Porqueres, I. Outcomes of “Over the Top” Anterior Cruciate Ligament Reconstruction Associated with a Lateral Extra-Articular Tenodesis in Children. J. Clin. Med. 2024, 13, 1501. https://doi.org/10.3390/jcm13051501
Gomez-Caceres A, Tamimi-Mariño I, Martinez-Malo FJ, Idiart-Charrier RP, Vieitez-Riestra I, Medina-Porqueres I. Outcomes of “Over the Top” Anterior Cruciate Ligament Reconstruction Associated with a Lateral Extra-Articular Tenodesis in Children. Journal of Clinical Medicine. 2024; 13(5):1501. https://doi.org/10.3390/jcm13051501
Chicago/Turabian StyleGomez-Caceres, Abel, Iskandar Tamimi-Mariño, Francisco Javier Martinez-Malo, Raphael Pierre Idiart-Charrier, Ignacio Vieitez-Riestra, and Ivan Medina-Porqueres. 2024. "Outcomes of “Over the Top” Anterior Cruciate Ligament Reconstruction Associated with a Lateral Extra-Articular Tenodesis in Children" Journal of Clinical Medicine 13, no. 5: 1501. https://doi.org/10.3390/jcm13051501
APA StyleGomez-Caceres, A., Tamimi-Mariño, I., Martinez-Malo, F. J., Idiart-Charrier, R. P., Vieitez-Riestra, I., & Medina-Porqueres, I. (2024). Outcomes of “Over the Top” Anterior Cruciate Ligament Reconstruction Associated with a Lateral Extra-Articular Tenodesis in Children. Journal of Clinical Medicine, 13(5), 1501. https://doi.org/10.3390/jcm13051501





