Timing and Modality of Hemorrhoidal Prolapse Impact on Patients’ Quality of Life
Abstract
1. Introduction
2. Materials and Methods
- Study Setting and Approval
- Inclusion and Exclusion Criteria
- Data Collection and Measurements
- Hemorrhoidal Prolapse Modality
- -
- type I, if a patient had no prolapse at all (answer #1);
- -
- type II, if the prolapse occurred only at defecation, with prompt spontaneous reduction (answer #2);
- -
- type III-a, if the prolapse occurred only at defecation but needing time for spontaneous reduction (answer #3) or needing manual reduction (answer #4);
- -
- type III-b, if the prolapse occurred not only at defecation but also on other occasions during the day, reducing either spontaneously (answer #5) or by manual maneuver (answer #6);
- -
- type IV, if the prolapse was not reducible because fixed outside the anus (answer #7).
- Symptoms of HD
- Quality of life
- Statistical analysis
3. Results
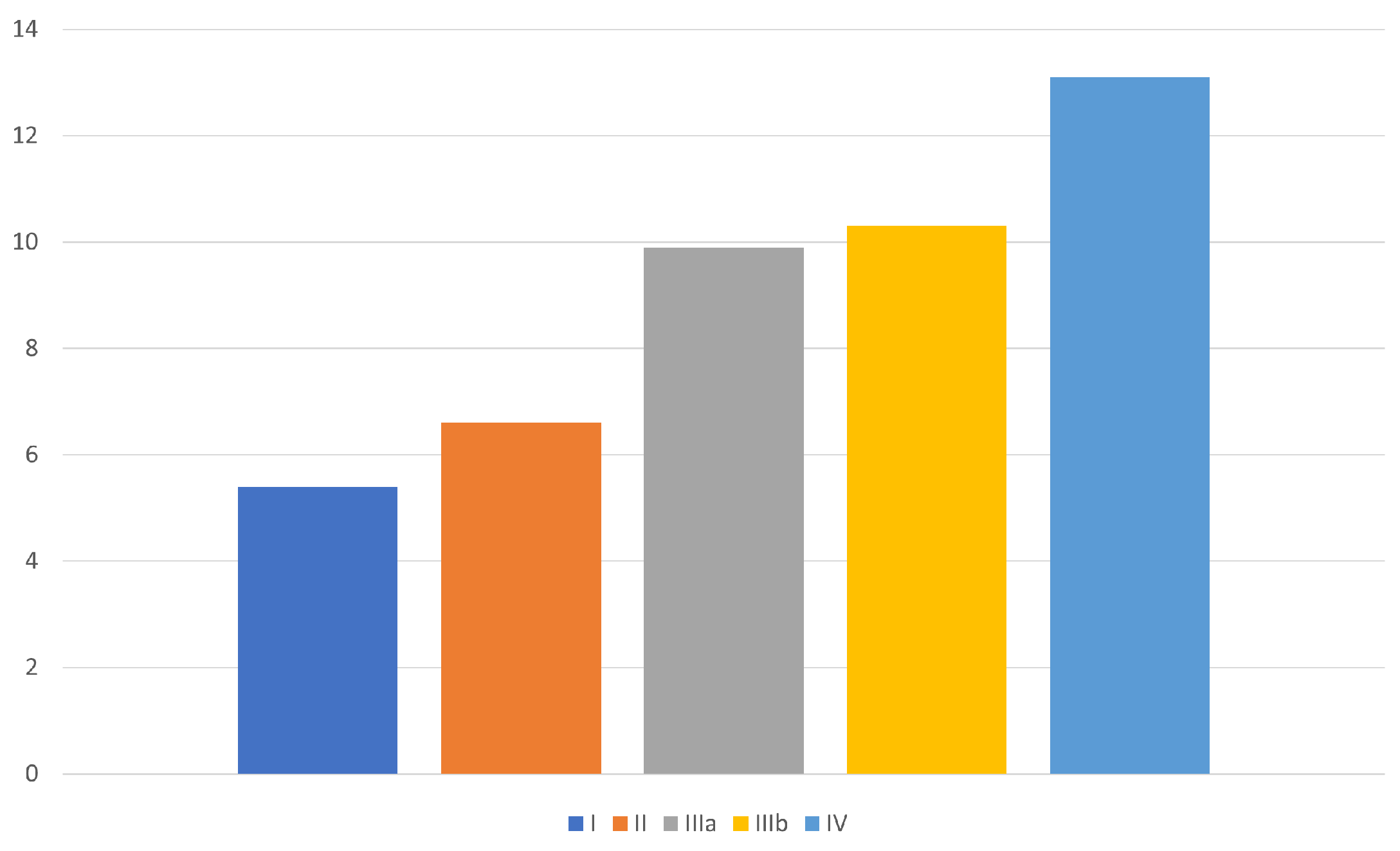
3.1. Hemorrhoidal Prolapse Modality
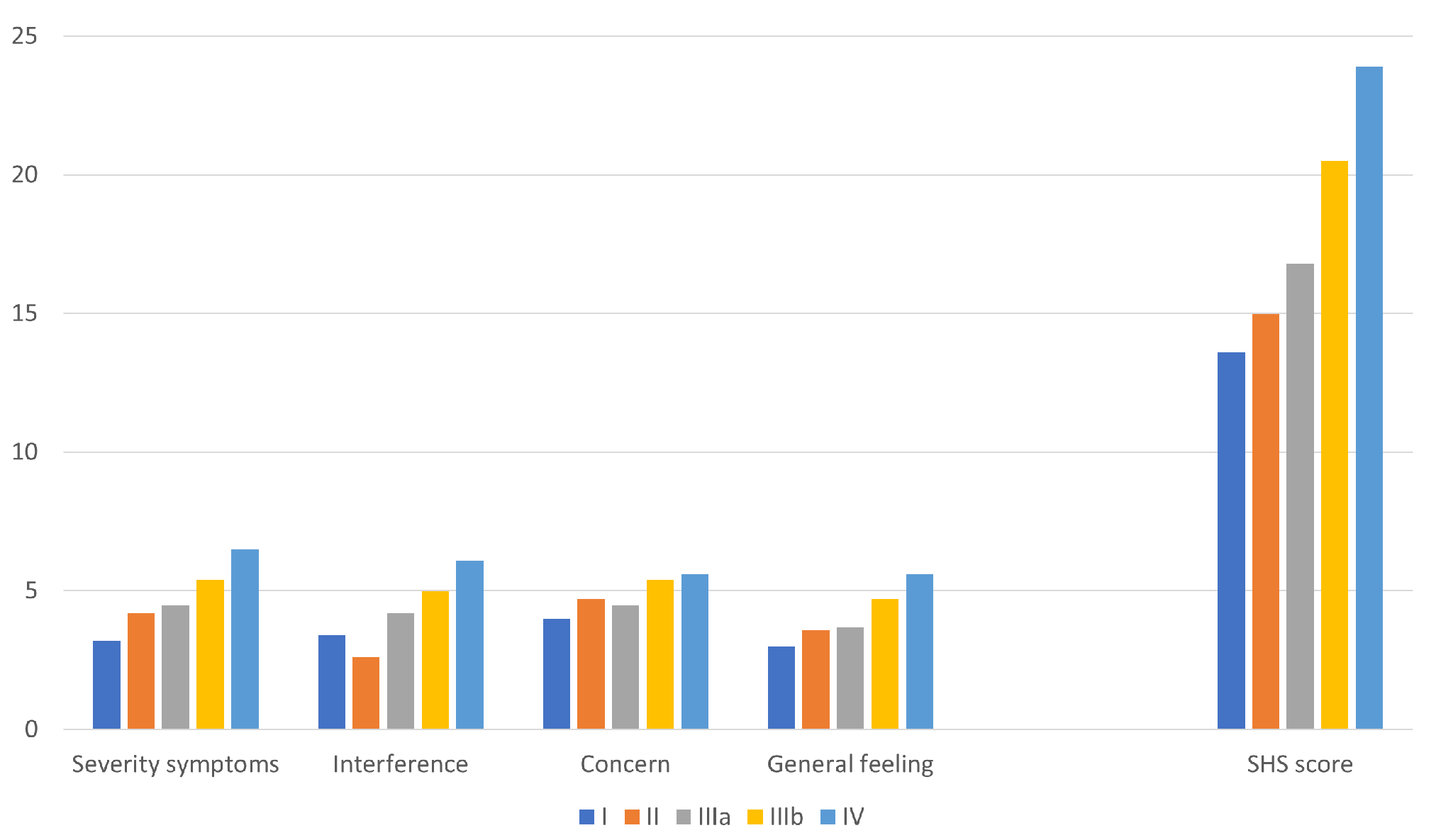
3.2. HDSS and SHSHD
3.3. Comparison between Type IIIa and IIIb Prolapse Modalities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kaidar-Person, O.; Person, B.; Wexner, S.D. Hemorrhoidal disease: A comprehensive review. J. Am. Coll. Surg. 2007, 204, 102–117. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Migaly, J. Review of Hemorrhoid Disease: Presentation and Management. Clin. Colon. Rectal Surg. 2016, 29, 22–29. [Google Scholar] [PubMed]
- Davis, B.R.; Lee-Kong, S.A.; Migaly, J.; Feingold, D.L.; Steele, S.R. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis. Colon. Rectum. 2018, 61, 284–292. [Google Scholar] [CrossRef] [PubMed]
- van Tol, R.R.; Kleijnen, J.; Watson, A.J.M.; Jongen, J.; Altomare, D.F.; Qvist, N.; Higuero, T.; Muris, J.W.M.; Breukink, S.O. European Society of ColoProctology: Guideline for haemorrhoidal disease. Colorectal Dis. 2020, 22, 650–662. [Google Scholar] [CrossRef] [PubMed]
- Goligher, J.C.; Duthie, H.L.; Nixon, H.H. Surgery of the Anus, Rectum, and Colon, 3rd ed.; Baillière Tindall: London, UK, 1975. [Google Scholar]
- Aibuedefe, B.; Kling, S.M.; Philp, M.M.; Ross, H.M.; Poggio, J.L. An update on surgical treatment of hemorrhoidal disease: A systematic review and meta-analysis. Int. J. Colorectal Dis. 2021, 36, 2041–2049. [Google Scholar] [CrossRef] [PubMed]
- Gerjy, R.; Lindhoff-Larson, A.; Nyström, P.O. Grade of prolapse and symptoms of haemorrhoids are poorly correlated: Result of a classification algorithm in 270 patients. Colorectal Dis. 2008, 10, 694–700. [Google Scholar] [CrossRef] [PubMed]
- van Tol, R.R.; Melenhorst, J.; Dirksen, C.D.; Stassen, L.P.S.; Breukink, S.O. Protocol for the development of a Core Outcome Set (COS) for hemorrhoidal disease: An international Delphi study. Int. J. Colorectal Dis. 2017, 32, 1091–1094. [Google Scholar] [CrossRef] [PubMed]
- Gaj, F.; Trecca, A. Nuovo sistema di classificazione della malattia emorroidaria “PATE 2006”: Vantaggi della revisione della “PATE 2000 Sorrento” [New “PATE 2006” system for classifying hemorrhoidal disease: Advantages resulting from revision of “PATE 2000 Sorrento”]. Chir Ital. 2007, 59, 521–526. [Google Scholar] [PubMed]
- Elbetti, C.; Giani, I.; Novelli, E.; Fucini, C.; Martellucci, J. The single pile classification: A new tool for the classification of haemorrhoidal disease and the comparison of treatment results. Updates Surg. 2015, 67, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Sobrado Júnior, C.W.; Obregon, C.A.; ESousa Júnior, A.H.D.S.; Sobrado, L.F.; Nahas, S.C.; Cecconello, I. A New Classification for Hemorrhoidal Disease: The Creation of the “BPRST”: Staging and Its Application in Clinical Practice. Ann. Coloproctol. 2020, 36, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Rørvik, H.D.; Styr, K.; Ilum, L.; McKinstry, G.L.; Dragesund, T.; Campos, A.H.; Brandstrup, B.; Olaison, G. Hemorrhoidal Disease Symptom Score and Short Health ScaleHD: New Tools to Evaluate Symptoms and Health-Related Quality of Life in Hemorrhoidal Disease. Dis. Colon. Rectum. 2019, 62, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Xia, W.; Connolly, A.; Hill, A.G. Symptom-based scoring for haemorrhoidal disease: A systematic review. Colorectal Dis. 2020, 22, 1518–1527. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Mokkink, L.B.; Knol, D.L.; Ostelo, R.W.; Bouter, L.M.; de Vet, H.C. Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual. Life Res. 2012, 21, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Kuiper, S.Z.; Kimman, M.L.; Rørvik, H.D.; Olaison, G.; Breukink, S.O. Making Use of Patient-Reported Outcome Measures for Haemorrhoidal Disease in Clinical Practice: A Perspective. Front. Surg. 2021, 8, 728532. [Google Scholar] [CrossRef] [PubMed]
| Please indicate how your hemorrhoidal prolapse usually occurs: |
|
| Hemorrhoidal Disease Symptom Score |
|---|
| The following questions deal with symptoms caused by hemorrhoids. Your answers should reflect your symptoms during the last 3 months (1 answer per question): |
| 1. How often do you feel pain from your hemorrhoids?
□ Never □ Less than once a month □ Less than once a week □ 1–6 days per week □ Every day (always) |
| 2. How often do you feel itching or discomfort of the anus? □ Never □ Less than once a month □ Less than once a week □ 1–6 days per week □ Every day (always) |
| 3. How often do you bleed when passing stool? □ Never □ Less than once a month □ Less than once a week □ 1–6 days per week □ Every day (always) |
| 4. How often do you soil your underwear (soiling from the anus)? □ Never □ Less than once a month □ Less than once a week □ 1–6 days per week □ Every day (always) |
| 5. How often do you feel a swelling or a prolapsing hemorrhoid? □ Never □ Less than once a month □ Less than once a week □ 1–6 days per week □ Every day (always) |
| Short Health ScaleHD |
| The following questions deal with how your symptoms caused by hemorrhoids affect your daily life (one answer per question): |
| 1. In your view, how severe are your symptoms caused by hemorrhoids? Please grade your symptoms on a 7-point scale, where 1 is “no symptoms” and 7 is “severe symptoms”. |
 |
| 2. Do your symptoms interfere with your daily activities? Please grade your answer on a 7-point scale, where 1 is “not at all” and 7 is “interfere to a very high degree”. |
 |
| 3. Do your symptoms cause much concern? Please grade your answer on a 7-point scale, where 1 is “no concerns” and 7 is “constant concerns”. |
 |
| 4. How is your general feeling of well-being? Please grade your answer on a 7-point scale, where 1 is “very good” and 7 is “very bad”. |
 |
| Age (mean, SD) | |
|---|---|
| <50 years | 59 (48.4) |
| >50 years | 63 (51.6) |
| Gender (n, %) | |
| female | 53 (43.4) |
| male | 69 (56.6) |
| Bristol stool scale (n, %) | |
| 1 | 11 (4.1) |
| 2 | 13 (10.7) |
| 3 | 35 (28.7) |
| 4 | 31 (25.4) |
| 5 | 17 (13.9) |
| 6 | 15 (12.3) |
| 7 | 0 |
| HDSS score (mean, SD) | |
| pain | 2.1 (1.5) |
| itching | 1.9 (1.4) |
| bleeding | 2.2 (1.2) |
| soiling | 0.6 (1.1) |
| prolapse/swelling | 3.1 (1.2) |
| TOTAL score | 9.8 (3.3) |
| SHS QoL (mean, SD) | |
| Severity symptoms | 5.0 (1.5) |
| Interference | 4.5 (1.9) |
| Concern | 4.9 (1.6) |
| General feeling | 4.2 (1.7) |
| TOTAL score | 18.6 (5.2) |
| PROLAPSE MODALITY (n, %) | |
| answer # 1 | 5 (4.1) |
| answer # 2 | 9 (7.4) |
| answer # 3 | 23 (18.9) |
| answer # 4 | 25 (20.5) |
| answer # 5 | 22 (18.0) |
| answer # 6 | 30 (24.6) |
| answer # 7 | 8 (6.6) |
| PATIENTS’ CLASSIFICATION (n, %) | |
| type I | 5 (4.1) |
| type II | 9 (7.4) |
| type IIIa | 48 (39.3) |
| type IIIb | 52 (42.6) |
| type IV | 8 (6.6) |
| TYPE IIIa | TYPE IIIb | p-Value | |
|---|---|---|---|
| Age | 52.4 (13.7) | 46.4 (10.6) | 0.012 |
| Gender (n, %) | 0.021 | ||
| female | 14 (29.2) | 27 (51.9) | |
| male | 34 (70.8) | 24 (48.1) | |
| Bristol stool scale (n, %) | 0.809 | ||
| 1 | 3 (6.3) | 5 (9.6) | |
| 2 | 4 8.3) | 7 (13.5) | |
| 3 | 15 (31.3) | 15 (28.8) | |
| 4 | 15 (31.3) | 12 (23.1) | |
| 5 | 6 12.5) | 5 (9.6) | |
| 6 | 5 (10.4) | 8 (15.4) | |
| 7 | 0 | 0 | |
| HDSS score (mean, SD) | |||
| pain | 1.8 (1.5) | 2.2 (1.5) | 0.311 |
| itching | 1.8 (1.5) | 1.9 (1.3) | 0.794 |
| bleeding | 2.4 (1.1) | 2.1 (1.2) | 0.271 |
| soiling | 0.7 (1.1) | 0.6 (1.1) | 0.916 |
| prolapse/swelling | 3.2 (1.0) | 3.5 (0.6) | 0.106 |
| TOTAL HDSS score | 9.9 (2.7) | 10.3 (3.2) | 0.747 |
| SHS QoL (mean, SD) | |||
| Severity symptoms | 4.5 (1.5) | 5.4 (1.2) | 0.004 |
| Interference | 4.2 (1.9) | 5.0 (1.4) | 0.022 |
| Concern | 4.5 (1.5) | 5.4 (1.5) | 0.003 |
| General feeling | 3.7 (1.6) | 4.7 (1.6) | 0.004 |
| TOTAL score | 16.8 (5.1) | 20.5 (4.0) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ratto, C.; Parello, A.; Marra, A.A.; Campennì, P.; De Simone, V.; Litta, F. Timing and Modality of Hemorrhoidal Prolapse Impact on Patients’ Quality of Life. J. Clin. Med. 2024, 13, 3946. https://doi.org/10.3390/jcm13133946
Ratto C, Parello A, Marra AA, Campennì P, De Simone V, Litta F. Timing and Modality of Hemorrhoidal Prolapse Impact on Patients’ Quality of Life. Journal of Clinical Medicine. 2024; 13(13):3946. https://doi.org/10.3390/jcm13133946
Chicago/Turabian StyleRatto, Carlo, Angelo Parello, Angelo Alessandro Marra, Paola Campennì, Veronica De Simone, and Francesco Litta. 2024. "Timing and Modality of Hemorrhoidal Prolapse Impact on Patients’ Quality of Life" Journal of Clinical Medicine 13, no. 13: 3946. https://doi.org/10.3390/jcm13133946
APA StyleRatto, C., Parello, A., Marra, A. A., Campennì, P., De Simone, V., & Litta, F. (2024). Timing and Modality of Hemorrhoidal Prolapse Impact on Patients’ Quality of Life. Journal of Clinical Medicine, 13(13), 3946. https://doi.org/10.3390/jcm13133946







