Baseline Psychological Inflexibility Moderates the Outcome Pain Interference in a Randomized Controlled Trial on Internet-based Acceptance and Commitment Therapy for Chronic Pain
Abstract
1. Introduction
2. Methods
2.1. Randomization
2.2. Participants
2.3. Treatment
2.4. Measures
2.5. Statistics
3. Results
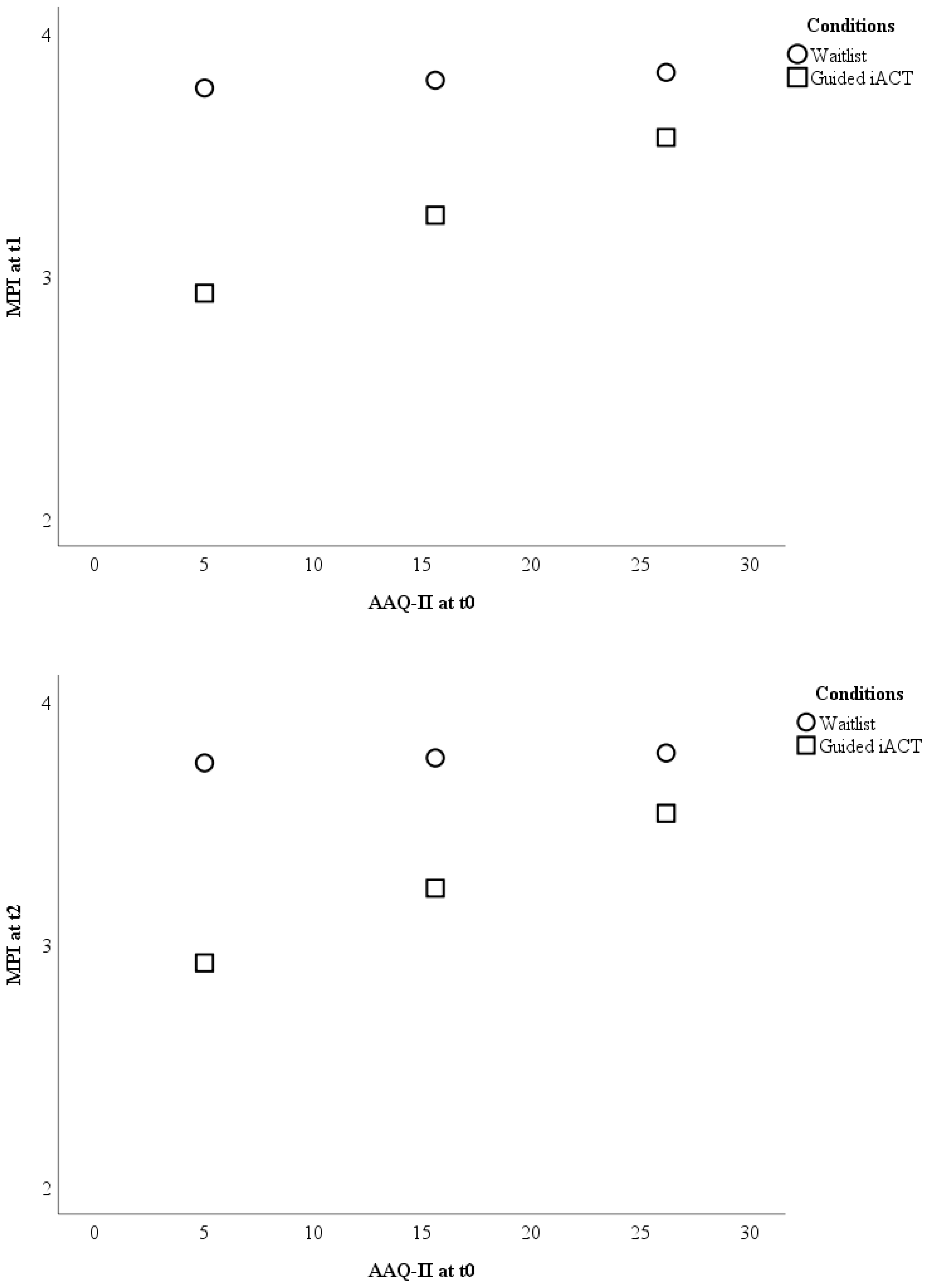
3.1. Guided Internet-based ACT vs. Waitlist
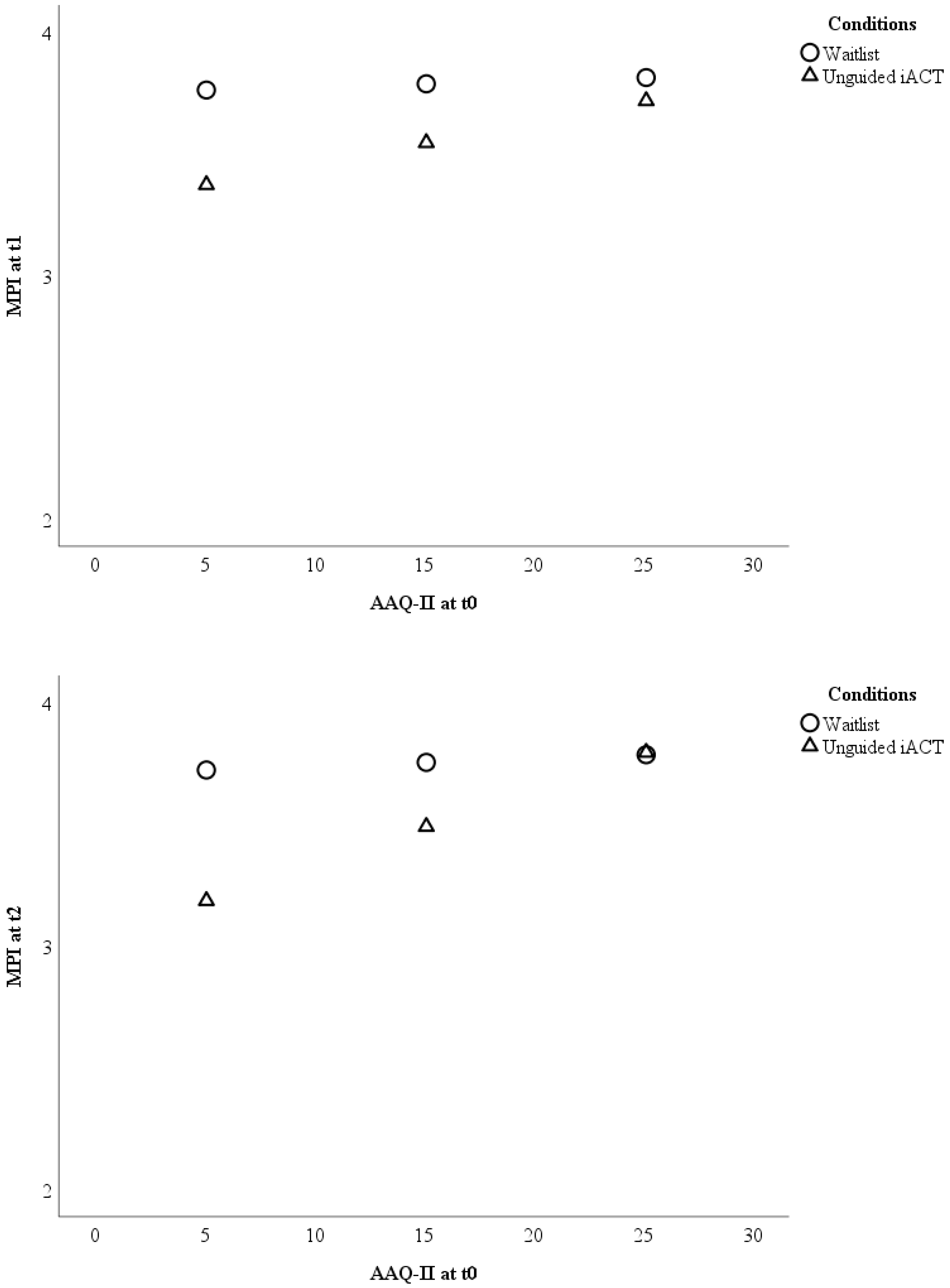
3.2. Unguided Internet-based ACT vs. Waitlist
3.3. Guided vs. Unguided Internet-based ACT
3.4. Relationship between Psychological Inflexibility and Completed Treatment Modules
4. Discussion
Author Contributions
Conflicts of Interest
References
- Steingrímsdóttir, Ó.A.; Landmark, T.; Macfarlane, G.J.; Nielsen, C.S. Defining chronic pain in epidemiological studies: A systematic review and meta-analysis. Pain 2017, 158, 2092–2107. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 328 Diseases and Injuries for 195 Countries, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Lee, H.; Hübscher, M.; Moseley, G.L.; Kamper, S.J.; Traeger, A.C.; Mansell, G.; McAuley, J.H. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain 2015, 156, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.C.; Eccleston, C.; Morley, S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2012, 11, CD007407. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.S.; Clark, J.; Colclough, J.A.; Dale, E.; McMillan, D. Acceptance and Commitment Therapy (ACT) for chronic pain: A systematic review and meta-analyses. Clin. J. Pain 2017, 33, 552–568. [Google Scholar] [CrossRef] [PubMed]
- Gilpin, H.R.; Keyes, A.; Stahl, D.R.; Greig, R.; McCracken, L.M. Predictors of treatment outcome in contextual cognitive and behavioral therapies for chronic pain: A systematic review. J. Pain 2017, 18, 1153–1164. [Google Scholar] [CrossRef]
- Gilpin, H.R.; Stahl, D.R.; McCracken, L.M. A theoretically guided approach to identifying predictors of treatment outcome in contextual CBT for chronic pain. Eur. J. Pain 2018. [Google Scholar] [CrossRef]
- Van Hoorn, R.; Tummers, M.; Booth, A.; Gerhardus, A.; Rehfuess, E.; Hind, D.; Bossuyt, P.M.; Welch, V.; Debray, T.P.; Underwood, M.; et al. The development of CHAMP: A checklist for the appraisal of moderators and predictors. BMC Med. Res. Methodol. 2017, 17, 173. [Google Scholar] [CrossRef]
- Lin, J.; Lüking, M.; Ebert, D.D.; Buhrman, M.; Andersson, G.; Baumeister, H. Effectiveness and cost-effectiveness of a guided and unguided internet-based Acceptance and Commitment Therapy for chronic pain: Study protocol for a three-armed randomised controlled trial. Internet Interv. 2015, 2, 7–16. [Google Scholar] [CrossRef]
- Lin, J.; Paganini, S.; Sander, L.; Lüking, M.; Ebert, D.D.; Buhrman, M.; Andersson, G.; Baumeister, H. An Internet-based intervention for chronic pain—A three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Deutsch. Ärztebl. Int. 2017, 114, 681–688. [Google Scholar]
- Lin, J.; Klatt, L.-I.; McCracken, L.M.; Baumeister, H. Psychological flexibility mediates the effect of an online-based acceptance and commitment therapy for chronic pain. Pain 2018, 159, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Buhrman, M.; Skoglund, A.; Husell, J.; Bergström, K.; Gordh, T.; Hursti, T.; Bendelin, N.; Furmark, T.; Andersson, G. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: A randomized controlled trial. Behav. Res. Ther. 2013, 51, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Kerns, R.D.; Turk, D.C.; Rudy, T.E. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985, 23, 345–356. [Google Scholar] [CrossRef]
- Flor, H.; Rudy, T.E.; Birbaumer, N.; Streit, B.; Schugens, M.M. Zur Anwendbarkeit des West Haven-Yale multidimensional pain inventory im Deutschen Sprachraum. Der Schmerz 1990, 4, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, J.; Gloster, A.T. Psychologische Flexibilität messen: Der Fragebogen zu Akzeptanz und Handeln II. Verhaltenstherapie 2013, 23, 42–44. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis, 2nd ed.; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Wolitzky-Taylor, K.B.; Arch, J.J.; Rosenfield, D.; Craske, M.G. Moderators and non-specific predictors of treatment outcome for anxiety disorders: A comparison of cognitive behavioral therapy to acceptance and commitment therapy. J. Consult. Clin. Psychol. 2012, 80, 786–799. [Google Scholar] [CrossRef]
- Craske, M.G.; Niles, A.N.; Burklund, L.J.; Wolitzky-Taylor, K.B.; Vilardaga, J.C.P.; Arch, J.J.; Saxbe, D.E.; Lieberman, M.D. Randomized controlled trial of cognitive behavioral therapy and acceptance and commitment therapy for social phobia: Outcomes and moderators. J. Consult. Clin. Psychol. 2014, 82, 1034–1048. [Google Scholar] [CrossRef]
- Carlbring, P.; Andersson, G.; Cuijpers, P.; Riper, H.; Hedman-Lagerlöf, E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018, 47, 1–18. [Google Scholar] [CrossRef]
- Buhrman, M.; Gordh, T.; Andersson, G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016, 4, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Kleinstäuber, M.; Weise, C.; Andersson, G.; Probst, T. Personality traits predict and moderate the outcome of Internet-based cognitive behavioural therapy for chronic tinnitus. Int. J. Audiol. 2018, 57, 538–544. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Probst, T.; Baumeister, H.; McCracken, L.M.; Lin, J. Baseline Psychological Inflexibility Moderates the Outcome Pain Interference in a Randomized Controlled Trial on Internet-based Acceptance and Commitment Therapy for Chronic Pain. J. Clin. Med. 2019, 8, 24. https://doi.org/10.3390/jcm8010024
Probst T, Baumeister H, McCracken LM, Lin J. Baseline Psychological Inflexibility Moderates the Outcome Pain Interference in a Randomized Controlled Trial on Internet-based Acceptance and Commitment Therapy for Chronic Pain. Journal of Clinical Medicine. 2019; 8(1):24. https://doi.org/10.3390/jcm8010024
Chicago/Turabian StyleProbst, Thomas, Harald Baumeister, Lance M. McCracken, and Jiaxi Lin. 2019. "Baseline Psychological Inflexibility Moderates the Outcome Pain Interference in a Randomized Controlled Trial on Internet-based Acceptance and Commitment Therapy for Chronic Pain" Journal of Clinical Medicine 8, no. 1: 24. https://doi.org/10.3390/jcm8010024
APA StyleProbst, T., Baumeister, H., McCracken, L. M., & Lin, J. (2019). Baseline Psychological Inflexibility Moderates the Outcome Pain Interference in a Randomized Controlled Trial on Internet-based Acceptance and Commitment Therapy for Chronic Pain. Journal of Clinical Medicine, 8(1), 24. https://doi.org/10.3390/jcm8010024




