Rehabilitation of Neonatal Brachial Plexus Palsy: Integrative Literature Review
Abstract
:1. Introduction
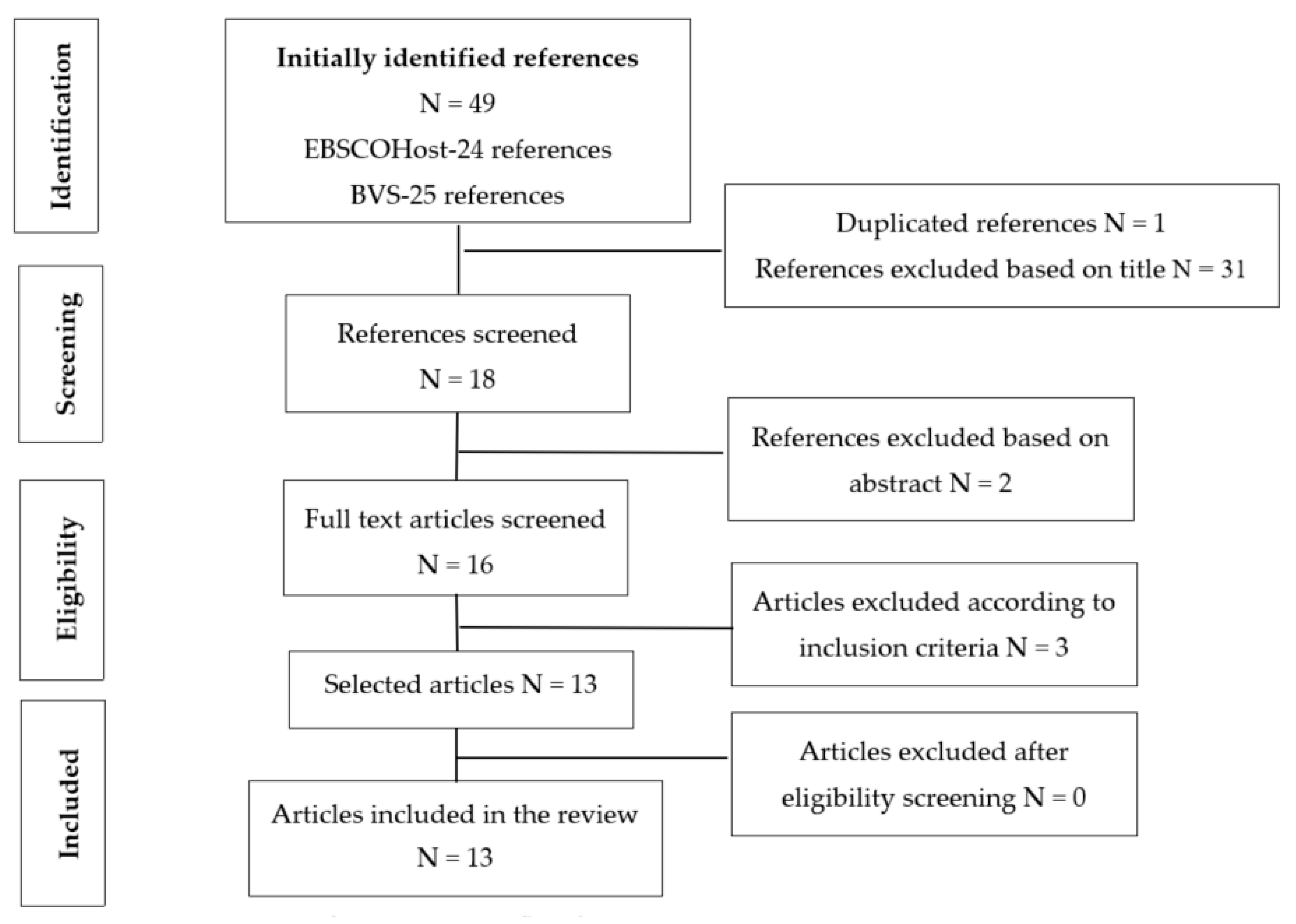
2. Experimental Section
3. Results
4. Discussion
4.1. Multidisciplinary Conservative Treatment
4.2. Surgical Treatment
4.3. Criteria for Conservative/Surgical Treatment
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Chauhan, S.P.; Blackwell, S.B.; Ananth, C.V. Neonatal brachial ple-xus palsy: Incidence, prevalence, and temporal trends. Semin Perinatol. 2014, 38, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Collado-Vázquez, S.; Jiménez-Antona, C.; Carrillo, J. Parálisis braquial obstétrica, una revisión histórica. Rev. Neurol. 2012, 55, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Abzug, J.M.; Chafetz, R.S.; Gaughan, J.P.; Ashworth, S.; Kozin, S.H. Shoulder function after medial approach and derotational humeral osteotomy in patients with brachial plexus birth palsy. J. Pediatr. Orthop. 2010, 30, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Jeyanthi, S. The effect of Nerve Branch Stimulation in Adjunct to convencional Treatment on C6-C7 Obstetric Brachial Plexus Injury: A Case Report. Indian J. Physiother Occup. Ther. 2015, 9, 150–155. [Google Scholar] [CrossRef]
- Doumouchtsis, S.K.; Arulkumaran, S. Are all brachial plexus injuries caused by shoulder dystocia? Obstet. Gynecol. Surv. 2009, 64, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Dijk, J.G.; Pondaag, W.; Malessy, M.J. Obstetric lesions of brachial plexus. Muscle Nerve. 2001, 24, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- Dogliotti, A.A. Conceptos actuales en la parálisis braquial perinatal. Parte 1: Etapa temprana. Arch. Argent. Pediatr. 2011, 109, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Waters, P.M. Update on management of pediatric brachial plexus palsy. J. Pediatr. Orthop. B. 2005, 25, 116–126. [Google Scholar]
- Birch, R. Surgical Disorders of the Peripheral Nerves, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Heise, C.O.; Martins, R.S.; Foroni, L.H.; Siqueira, M.G. Prognostic value of thumb pain sensation in birth brachial plexopathy. Arq. Neuropsiquiatr. 2012, 70, 590–592. [Google Scholar] [CrossRef] [Green Version]
- Kay, S.P. Obstetrical brachial palsy. Br. J. Plast. Surg. 1998, 51, 43–50. [Google Scholar] [CrossRef]
- Alfonso, I.; Alfonso, D.T.; Papazian, O. Focal upper extremity neuropathy in neonates. Semin. Pediatr. Neurol. 2000, 7, 4–14. [Google Scholar] [CrossRef]
- Al-Qattan, M.M.; Al-Khawashki, H. The “beggar’s” hand and the “unshakable” hand in children with total obstetric brachial plexus palsy. Plast. Reconstr. Surg. 2002, 109, 1947–1952. [Google Scholar] [CrossRef] [PubMed]
- Tavares, A.P.S.; Watanabe, B.M.N.; Oliveira, T.C. A terapia ocupacional favorecendo o desenvolvimento neuropsicomotor, ao intervir precocemente, em crianças com paralisia braquial obstétrica. [Trabalho de Conclusão de Curso de Terapia Ocupacional]; Centro Universitário Católico Salesiano Auxilium: Lins, SP, Brazil, 2008. (In Portuguese) [Google Scholar]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Socolovsky, M.; Robla, C.J.; Dominguez, P.M.; Nizzo, G.; Valbuena, S.; Varone, E. Obstetric brachial plexus palsy: Reviewing the literature comparing the results of primary versus secondary surgery. Childs Nerv. Syst. 2016, 32, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Pondaag, W.; Malessy, M. The Evidence for Nerve Repair in Obstetric Brachial Plexus Palsy Revisited. Biomed. Res. Int. 2014, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bade, S.; Lin, J.; Curtis, C.; Clarke, H. Extending the Indications for Primary Nerve Surgery in Obstetrical Brachial Plexus Palsy. Biomed. Res. Int. 2014, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Justice, D.; Awori, J. Use of Neuromuscular Electrical Stimulation in the Treatment of Neonatal Brachial Plexus Palsy: A Literature Review. Open J. Occup. Ther. 2018, 6, 1–11. [Google Scholar] [CrossRef]
- Otto, H.C.; Martins, R.; Siqueira, M. Neonatal brachial plexus palsy: A permanente challenge. Arq. Neuropsiquiatr. 2015, 73, 803–808. [Google Scholar] [CrossRef]
- Yanes, S.V.L.; Sandobal, F.E.C.; Camero, A.D.; Ojeda, D.L. Obstetric Brachial Plexus Palsy in the Context of Early Physical Rehabilitation. MediSur 2014, 12, 635–649. [Google Scholar]
- Smith, B.; Daunter, A.; Yang, L.; Wilson, T. An Update on the Management of Neonatal Brachial Plexus Palsy-Replacing Old Paradigms A Review. JAMA Pediatr. 2018, 172, 585–591. [Google Scholar] [CrossRef]
- Brown, S.H.; Napier, R.; Nelson, V.S.; Yang, L.J. Home-based movement therapy in neonatal brachial plexus palsy: A case study. J. Hand Ther. 2015, 28, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Al-Qattan, M.M.; El-Sayed, A.A.F. The use of the Phrenic Nerve Communicating Branch to the Fifth Cervical Root for Nerve Transfer to the Suprascapular Nerve in Infants with Obstetric Brachial Plexus Palsy. Biomed. Res. Int. 2014, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, R.M.; Grechi, G.; Gepp, R.A. Oberlin’s procedure in children with obstetric brachial plexus palsy. Childs Nerv. Syst. 2016, 32, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- García Ron, A.; Gallardo, R.; Huete Hermani, B. Utility of ultrasound-guided injection of botulinum toxin type A for muscle imbalance in children with obstetric brachial plexus palsy: Description of the procedure and action protocol. Neurologia 2017, 34, 1–9. [Google Scholar] [CrossRef]
- Al-Qattan, M.M.; Al-Kharfy, T.M. Median Nerve to Biceps Nerve Transfer to Restore Elbow Flexion in Obstetric Brachial Plexus Palsy. Biomed. Res. Int. 2014, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.J. Neonatal brachial plexus palsy: Management andprognostic factors. Semin Perinatol. 2014, 38, 222–234. [Google Scholar] [CrossRef]
- Amador, E.V. Trauma del plexo braquial: Conceptos actuales en el diagnóstico y tratamiento quirúrgico. Rev. Col. Med. Fis. Rehab. 2013, 23, 160–169. [Google Scholar] [CrossRef]
- Okafor, U.A.; Akinbo, S.R.; Sokunbi, O.G.; Okanlawon, A.O.; Noronha, C.C. Comparison of electrical stimulation and conventional physiotherapy in functional rehabilitation in Erb’s palsy. Nig. Q. J. Hosp. Med. 2008, 18, 202–205. [Google Scholar] [CrossRef]
- Shin, Y.B.; Shin, M.J.; Chang, J.H.; Cha, Y.S.; Ko, H.Y. Effects of botulinum toxin on reducing the co-contraction of antagonists in birthbrachial plexus palsy. Ann. Rehabil. Med. 2014, 38, 127–131. [Google Scholar] [CrossRef]
- Buesch, F.E.; Schlaepfer, B.; de Bruin, E.D.; Wohlrab, G.; Ammann-Reiffer, C.; Meyer- Heim, A. Constraint-induced movement therapy for children with obstetric brachial plexus palsy: Two single-case series. Int. J. Rehabil. Res. 2010, 33, 187–192. [Google Scholar] [CrossRef]
- Murphy, K.M.; Rasmussen, L.; Hervey-Jumper, S.L.; Justice, D.; Nelson, V.S.; Yang, L.J.-S. An assessment of the compliance and utility of a home exercise DVD for caregivers of children and adolescents with brachial plexus palsy: A pilot study. PMR 2012, 4, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.C.; Schwentker-Colizza, A.; Curtis, C.G.; Clarke, H.M. Final results of grafting versus neurolysis in obstetrical brachial plexus palsy. Plast. Reconstr. Surg. 2009, 123, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Al-Qattan, M.M. Oberlin’s ulnar nerve transfer to the bíceps nerve in Erb’s birth palsy. Plast. Reconstr. Surg. 2002, 109, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Oberlin, C.; Ameur, N.E.; Teboul, F.; Beaulieu, J.Y.; Vacher, C. Restoration of elbow flexion in brachial plexus injury by transfer of ulnar nerve fascicles to the nerve to the biceps muscle. Tech. Hand Upr. Extrem. Surg. 2002, 6, 86–90. [Google Scholar] [CrossRef]
- Sungpet, A.; Suphachatwong, C.; Kawinwonggowit, V. One fascicle median nerve transfer to biceps muscle in C5 and C6 root avulsions of brachial plexus injury. Microsurgery 2003, 23, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Murabit, A.; Gnarra, M.; O’Grady, K.; Morhart, M.; Olson, J. Functional outcome after the Hoffer procedure. Plast. Reconstr. Surg. 2013, 131, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.; Valbuena, S.; Posso, C. Obstetrical brachial plexus injuries: Late functional results of the Steindler procedure. J. Hand Surg. Eur. Vol. 2014, 39, 68–875. [Google Scholar] [CrossRef]
- Ruchelsman, D.E.; Ramos, L.E.; Price, A.E.; Grossman, L.A.; Valencia, H.; Grossman, J.A. Outcome after tendon transfers to restore wrist extension in children with brachial plexus birth injuries. J. Pediatr. Orthop. 2011, 31, 455–457. [Google Scholar] [CrossRef]
- Chin, K.F.; Misra, V.P.; Sicuri, G.M.; Fox, M.; Sinisi, M. Intra-operative neurophysiological prediction of upper trunk recovery in obstetric brachial plexus palsy with neuroma incontinuity. Bone Joint J. 2013, 95, 699–705. [Google Scholar] [CrossRef]
- Al-Qattan, M.M. The outcome of Erb’s palsy when the decision to operate is made at 4months of age. Plast. Reconstr. Surg. 2000, 106, 1461–1465. [Google Scholar] [CrossRef]
- Pondaag, W.; Malessy, M.J. Recovery of hand function following nerve grafting and transfer in obstetric brachial plexus lesions. J. Neurosurg. 2006, 105, 33–40. [Google Scholar] [CrossRef]
- Birch, R.; Ahad, N.; Kono, H.; Smith, S. Repair of obstetric brachial plexus palsy. Results in 100 children. J. Bone Jt. Surg. 2005, 87, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
| Author(s), Year, Location | Population | Aims | Methods |
|---|---|---|---|
| Socolovsky, M; et al. 2016, Argentina [16] | Articles about primary and secondary surgery. | Identify and describe the primary and secondary surgeries available for the rehabilitation of obstetric brachial plexus palsy. | Literature Review. |
| Results: Primary surgery may be unnecessary if there is spontaneous recovery of the biceps before the age of 3 months. Authors defend a wider decision window for primary surgery ranging from 3 to 9 months after birth, avoiding unnecessary surgeries and favoring conservative treatment in the event of any recovery in elbow or shoulder function. There are three primary microsurgery techniques: (1) recession and reconstruction of the neuroma using interposed grafts, (2) neurolysis, and (3) nerve transfer. Secondary surgical procedures involve tendon transfer, arthrodesis, or osteotomies, and can be used in patients who have partially recovered after primary surgery, or in patients who have not undergone primary surgery and experience some form of spontaneous recovery, but still have some deficits. Secondary surgery targets the (1) shoulder, (2) elbow, and (3) hand. | |||
| Author(s), Year, Location | Population | Aims | Method |
| Pondaag, W; Malessy, M. 2014, Netherlands [17] | Nine articles | Analyze and describe scientific evidence on conservative rehabilitation and surgical rehabilitation of obstetric brachial plexus palsy. | Systematic Literature Review |
| Results: The studies analyzed in this systematic review of the literature do not present scientific evidence favoring surgical treatment/nerve reconstruction over conservative treatment, where spontaneous recovery occurs. Most of the analyzed studies reveal surgical reconstruction of the nerves was performed in children who showed no spontaneous recovery during the first months of life. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Bade, S; et al. 2014, Canada [18] | Seventeen patients with obstetric brachial plexus palsy | Explore situations where reconstructive surgery is indicated for obstetric brachial plexus palsy. | Exploratory Study |
| Results: There is no consensus on indication and length of surgical treatment for obstetric brachial plexus palsy. It is advocated that excision of the neuroma or nerve grafting is indicated for children who do not have biceps function at the age of 3 months. Flexion and extension of the elbow combined with wrist extension, extension of the fingers, and thumb extension improve the prognosis of spontaneous recovery. Surgery is indicated if at 3 months of age there is evidence of avulsion of the nerve roots. The study shows that the biceps of children can recover at 5 months, but surgery is only counter-indicated at 3 months if upper function (shoulder) is partially recovered, especially the external rotation of the shoulder. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Justice, D; Awori, J. 2018, USA [19] | Four articles | Evaluate the efficacy of neuromuscular electrostimulation in restoring movement and function in neonatal brachial plexus palsy. | Literature Review |
| Results: Physiotherapists and occupational therapists often use neuromuscular electrostimulation to treat decreased muscle strength. Neuromuscular electrostimulation treatment involves using electrodes to deliver an electrical current to a muscle without nervous activity, with the aim of promoting functional recovery of the muscle after nerve injury. Electrostimulation is used concomitantly with exercise, massage, splinting, constraint induced movement therapy, and Ayurvedic therapy. Studies have shown that the use of electrostimulation inhibits muscle atrophy during the reinnervation period, and accelerates nerve regeneration, so an improvement in muscle strength and range of motion is associated with electrostimulation. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Jeyanthi, S; 2015, India [4] | One child with obstetric brachial plexus palsy. | Describe the benefits of electrostimulation in improving motor performance and functional performance in a child with obstetric brachial plexus injury. | Case study. |
| Results: Conventional treatment of obstetric brachial plexus injury advocates early diagnosis and follow-up accompanied by physiotherapy and occupational therapy. In these therapies, which include passive mobilization, stretches, use of anterior and posterior splints to prevent deformities, especially during sleep, and early motor training to encourage efficient movements. Tactile stimulation is provided through different materials of different textures; vibration and brushing techniques to increase sensory awareness of the affected arm; bimanual activities to prevent limb disuse; strength and coordination exercises throughout the child’s growth and development stage; and day-to-day activities that promote fine motor control. Electrostimulation is a technique used by these therapists with the aim of promoting rehabilitation, preventing muscle atrophy, promoting nerve regeneration, and increasing motor performance and joint manipulation, namely in the shoulder, elbow, and wrist, as well as increasing awareness of the limb. This study concludes that, as a complement to conventional therapies, electrical stimulation of nervous branches helps solve functional limb impairment and promotes active movement gains, especially in the biceps, and wrist and finger extensors. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Otto, HC; et al. 2015, Brazil [20] | Articles on rehabilitation of neonatal brachial plexus palsy in infants | Describe current practices for rehabilitating lactating infants with neonatal brachial plexus palsy, covering conservative and surgical therapy. | Literature Review |
| Results: Rehabilitation of neonatal brachial plexus palsy may include conventional treatment through therapies such as physiotherapy and occupational therapy, or surgery. The indication for surgery is not consensual. Some authors defend that surgery is indicated if there is no evidence of spontaneous recovery, especially of the biceps function in children up to the age of 3 months. Others defend that this assessment can be made later, up to the age of 6 months. This assessment not only covers elbow flexion, but also shoulder abduction, and elbow, wrist, and finger extension. In conventional treatment, physiotherapy and occupational therapy are of great importance, but it is essential to involve parents in the rehabilitation program, so that professionals and family members work jointly. A passive range of motion exercises are fundamental for preventing muscle contractions and should be done several times a day. It is important to include them in all day-to-day activities, such as with every nappy change, and at each meal (bottle/breast). As the child grows, develops, and gains intentional voluntary control and awareness of his/her body, it is important to promote activities that stimulate the affected limb so as to prevent apraxia. One possible strategy is to encourage bimanual activities. In children with compromised wrist extension, the use of temporary, posterior and anterior immobilizing splints can help improve hand function and prevent wrist drop. Splints are best used during sleep, so that the hand can be used during awake time activities. Excessive reinnervation of active muscles can result in co-contractions and contractures, which can be treated with botulinum toxin, allowing gains in mobility and range of motion. Regarding surgery, there are three approaches: neurolysis, nerve grafts, and nerve transfers. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Yanes, SVL; et al. 2014, Cuba [21] | Theoretical references that address frequency, risk factors, aetiology, anatomy, and pathophysiology, lesion types, prognosis, and treatments. | Describe the clinical elements related to obstetric brachial plexus palsy and present the different rehabilitation strategies. | Literature Review |
| Results: Currently, conservative treatment is recommended, i.e., physiotherapy and occupational therapy, engaging parents as important actors in the child’s rehabilitation. Authors defend that conservative treatment must be applied as early as possible (2 to 3 weeks after birth) through gentle joint movements and sensory stimulation. The aim of the therapy is to ensure the necessary conditions for functional recovery following nerve regeneration, which implies the prevention of muscle shrinkage, sagging, and joint deformities through activities adapted to the child’s development. The therapy should be administered several times a week, and at home, as frequently as possible, for example at each meal or with every nappy change. Sensory stimulation is as important as motor stimulation and can consist in suckling any finger on the injured limb and stimulating the skin with different textures, temperatures, and vibrations. The use of thermoplastic splints may be necessary to maintain wrist extension. Electrostimulation is also used in conservative treatment. As the child grows, rehabilitation remains important for integrating the limb into the body structure through integration activities and postural re-education of the upper limb and the chest. Exercises that target the recovery of muscle strength are important, even if neurological and muscle functions are not fully recovered. Surgery presents itself as an alternative for conservative treatment, with some authors defending that children who have not recovered their biceps function at the age of three months must undergo surgery. Others prefer to wait up to the age of six months if nerve root avulsion is not suspected. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Smith, B; et al. 2018, USA [22] | Articles on rehabilitation of neonatal brachial plexus palsy in infants. | Provide an update on the rehabilitation of neonatal brachial plexus palsy to replace old beliefs with new paradigms. | Literature Review |
| Results: The management of neonatal brachial plexus palsy has changed considerably in the last 25 years, leading to a paradigm shift. The old indication to immobilize the arm after diagnosis of the lesion is completely outdated. Currently, after early diagnosis of the lesion, the child is expected to undergo conservative treatment with physiotherapy and occupational therapy as soon as possible. The aim of these therapies is to promote a normal range of motion, the use of the affected limb, to strengthen muscles and develop independence. The child’s family should be involved in the rehabilitation of neonatal brachial plexus palsy and trained on exercises that can be performed at home. Various techniques are used in these therapies: stretches, passive and active movements, muscle strengthening, and use of kinesiology tapes and electrostimulation, among others. As an alternative to conservative treatment, studies performed at the University of Toronto indicate that there is a surgical option for children without bicep function at the age of 3 months. If there is any evidence of recovery at the age of three months, the situation is reassessed between the age of 6 and 9 months to assess whether there is need for surgical intervention. Assessment at these stages indicate the need of early follow-up for children with obstetric brachial plexus palsy. Surgical options for these lesions involve nerve grafts, nerve transfer, or a combination of both. The nerve graft can be extracted from the nerve itself (autologous graft). Nerve transfers reconnect a nerve from a muscle with redundant function to the target without innervations. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Brown, SH; et al. 2015, USA [23] | A 17-year-old female patient with neonatal brachial plexus palsy. | Determine the efficacy of a therapy program administered at home, where movement of the healthy arm of a 17-year-old adolescent with neonatal brachial plexus palsy was constrained. | Case Study |
| Results: This therapy consists in constraining movement of the non-injured arm to stimulate movement of the injured arm through active exercises that promote mobility, range of motion, and strength. This case study demonstrates that constraining movement therapy of the non-injured arm, administered at home through activities performed one hour per day, can improve mobility, functional capacity, speed, range of motion, and hand manipulation ability in a teenager with neonatal brachial plexus palsy. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Al-Qattan, MM; El-Sayed, AAF. 2014, Saudi Arabia [24] | A total of 15 infants underwent phrenic nerve transfer to reconstruct the suprascapular nerve, 15 lactating infants underwent accessory nerve transfer to reconstruct the suprascapular nerve, and the potential to improve external shoulder rotation was studied. | Verify if using a phrenic nerve graft to reconstruct the suprascapular nerve in case of an obstetric brachial plexus palsy contributes to improving external shoulder rotation- | Retrospective Study |
| Results: Surgery is one of the rehabilitation options for obstetric brachial plexus palsy, and there are several types of surgical procedures such as nerve grafting, among others. When the lesion affects the suprascapular nerve, shoulder function is impaired, especially abduction and external rotation. Grafts used to reconstruct the suprascapular nerve are often extracted from the proximal C5 root stump or the accessory nerve. This study introduces a communicating branch from the phrenic nerve as a potential donor for rebuilding the suprascapular nerve, when available and a suitable size. The study showed no significant improvement in the recovery of the shoulder’s external rotation when the phrenic nerve or the accessory nerve were used as grafts. Therefore, we can assume that the communicating branch from the phrenic nerve can be considered an option to rebuild the suprascapular nerve. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Figueiredo, et al; 2016, Brazil. [25] | A total of 13 children between the ages of 9 and 15 months were treated according to the Oberlin’s Procedure. | Describe the results of ulnar nerve transfer to the cutaneous nerve (Oberlin’s method) in the improvement of elbow flexion, in children with obstetric brachial plexus palsy at the C5–C6 level. | Retrospective Study |
| Results: Obstetric brachial plexus palsy may involve neuropraxia or nerve root avulsion. The C5–C6 roots are frequently affected in obstetric brachial plexus palsy, compromising shoulder abduction and external rotation, elbow flexion, and forearm supination. This type of lesion is known as Erb’s palsy. Elbow flexion is a fundamental aspect of arm function, and when absent in the affected arm, one of the treatment options is surgery. The Oberlin’s procedure involves the transfer of the ulnar nerve to the cutaneous nerve, with the aim of improving elbow flexion. In this study, thirteen children underwent the abovementioned procedure. After surgery, the arm was immobilized with the shoulder in adduction and the elbow in flexion to the right. Physiotherapy and occupational therapy were then resumed, with specific activities to develop functionality, as well as active and passive mobilization. To evaluate the efficacy of the procedure, elbow flexion, supination of the forearm, and limb function were assessed, as was the nervous function of the donor during wrist flexion. The results reveal that the Oberlin’s procedure significantly improves elbow flexion and functional use of the affected limb, without any loss of hand function, namely wrist flexion, because the ulnar nerve was used as a donor. No conclusions about supination can be drawn from the results. Nonetheless, the Oberlin’s procedure is an effective option for recovering elbow function and should be consider alongside other procedures to restore shoulder function. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| García Ron, A; et al. 2017, Spain [26] | Fifteen cases of newborns with obstetric brachial plexus palsy. | Describe the treatment of an obstetric brachial plexus palsy with ultrasound-guided botulinum toxin infiltration. | Prospective, Descriptive Study |
| Results: The severity and extent of the obstetric brachial plexus palsy determine recovery and sequelae. Some of these lesions recover spontaneously during the first 6 to 8 weeks of life. However, there are more severe cases that leave permanent motor sequelae and that are greatly disabling for limiting movement, strength and volume in the affected muscle. Permanent functional limitation is frequently found in the more severe lesions, particularly affecting the muscles involved in external shoulder rotation and abduction, elbow flexion, forearm supination, and wrist extension. The weakened state of these muscles leads to a great imbalance of strength in relation to the healthy muscles. These persisting muscle imbalances limit the strength and movement of the affected limb, leading to muscle contractures and bone deformities, particularly in the shoulder. Treatment with botulinum toxin has shown efficacy in the treatment of muscle imbalances, co-contractions, and muscle contractures. It is used to treat children with obstetric brachial plexus palsy, weakening healthy antagonistic muscles with the aim of balancing strength, and allowing the affected muscles to develop. Strength and functional improvement are addressed through occupational therapy and physiotherapy, with movement patterns suited to the ongoing nerve recovery. In this study, botulinum toxin infiltrations were started between the child’s 6th and 18th month of life, with an average of three infiltrations per child. The most frequently infiltrated muscles were the subscapular, the pectoralis major, the latissimus dorsi, and the pronator teres. Results appear 2 to 3 weeks after infiltration, and the effect has an average duration of 4 months. In this study, botulinum toxin infiltration managed to spare 3 children from undergoing surgery. All children improved functionality of the limb and abnormal postures: improvement was observed both in the shoulder joint and the elbow joint. In conclusion, it is important to use infiltration with botulinum toxin as adjuvant treatment to physiotherapy and/or surgical treatment in moderate/severe obstetric brachial plexus palsy. | |||
| Author(s), Year, Location | Population | Aims | Methods |
| Al-Qattan, MM; Al-Kharfy, TM. 2014, Saudi Arabia [27] | Ten cases of children with upper (C5–C6) obstetric brachial plexus palsy, with little or no late recovery of elbow flexion. | To describe the results of median nerve transfer to the biceps nerve, with the aim of reinnervating the biceps of children with obstetric brachial plexus palsy at the C5–C6 level, known as Erb’s palsy. | Descriptive Study |
| Results: Surgical treatment is indicated in the absence of spontaneous recovery of elbow flexion in children with obstetric brachial plexus palsy at the C5–C6 level (Erb’s paralysis), where the biceps nerve is grafted. Postoperative care includes the immobilization of the affected arm for three weeks before intensive physiotherapy is restarted. This study describes the recovery of ten children with Erb’s palsy, who underwent reconstructive surgery of the biceps nerve, using the median nerve as a donor. Reinnervation of the biceps nerve using the median nerve leads to improved elbow flexion. | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frade, F.; Gómez-Salgado, J.; Jacobsohn, L.; Florindo-Silva, F. Rehabilitation of Neonatal Brachial Plexus Palsy: Integrative Literature Review. J. Clin. Med. 2019, 8, 980. https://doi.org/10.3390/jcm8070980
Frade F, Gómez-Salgado J, Jacobsohn L, Florindo-Silva F. Rehabilitation of Neonatal Brachial Plexus Palsy: Integrative Literature Review. Journal of Clinical Medicine. 2019; 8(7):980. https://doi.org/10.3390/jcm8070980
Chicago/Turabian StyleFrade, Fátima, Juan Gómez-Salgado, Lia Jacobsohn, and Fátima Florindo-Silva. 2019. "Rehabilitation of Neonatal Brachial Plexus Palsy: Integrative Literature Review" Journal of Clinical Medicine 8, no. 7: 980. https://doi.org/10.3390/jcm8070980
APA StyleFrade, F., Gómez-Salgado, J., Jacobsohn, L., & Florindo-Silva, F. (2019). Rehabilitation of Neonatal Brachial Plexus Palsy: Integrative Literature Review. Journal of Clinical Medicine, 8(7), 980. https://doi.org/10.3390/jcm8070980






