Degenerative Cervical Myelopathy in Higher-Aged Patients: How Do They Benefit from Surgery?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Clinical Outcome
2.3. Statistical Analysis
2.4. Ethics
3. Results
3.1. Symptom Presentation
3.2. Surgical Treatment
3.3. Preoperative and Postoperative mJOA Score
3.4. Neurological Recovery Rate
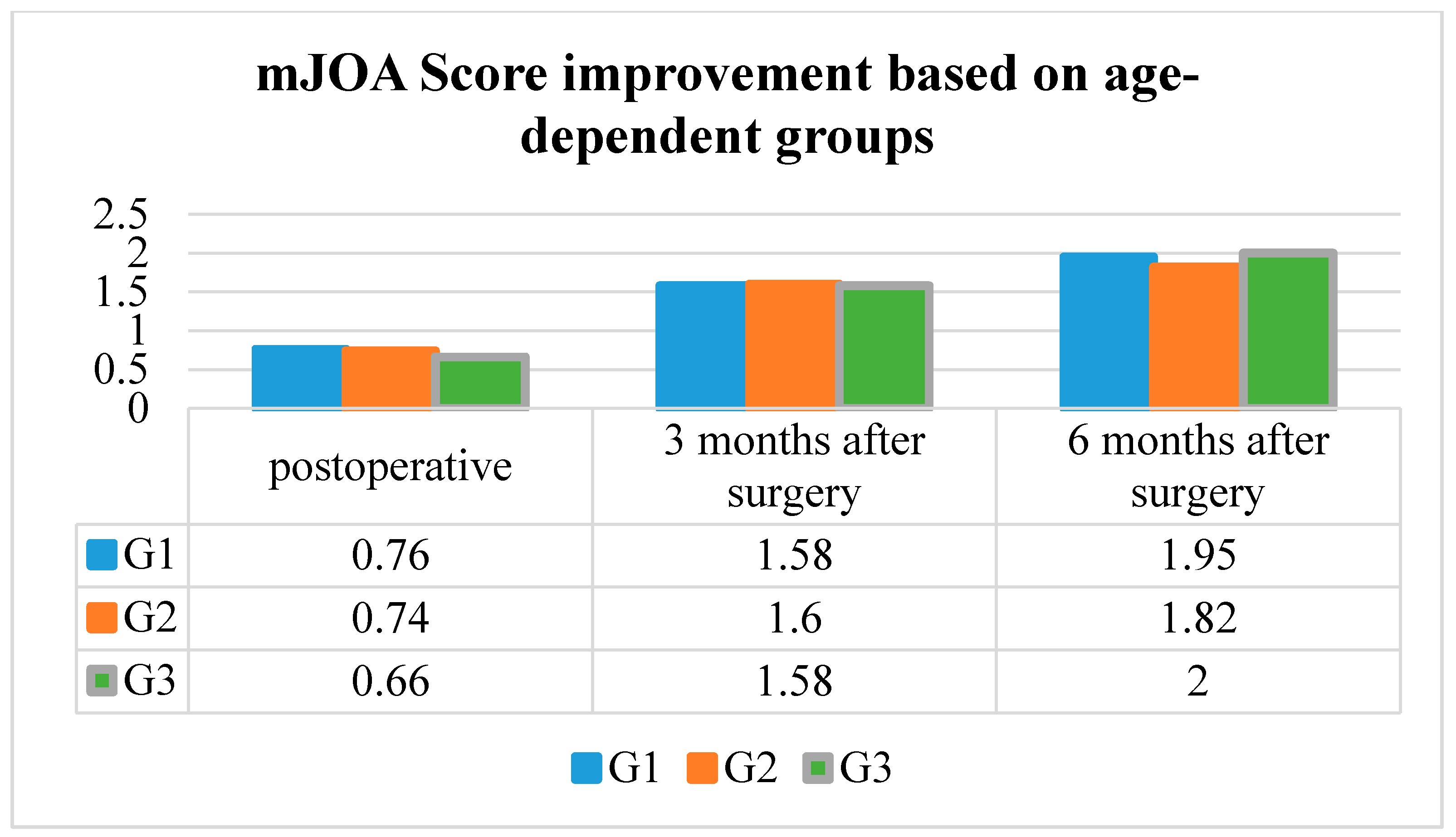
3.5. Mean mJOA Score Improvement
3.6. Minimum Clinically Important Difference
3.7. Comorbidities and the Charlson Comorbidity Index
3.8. Duration of Myelopathic Symptoms Prior to Surgery
3.9. Duration of Hospitalization
3.10. Surgical and Non-Surgical Complications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lawrence, J. Disc degeneration. Its frequency and relationship to symptoms. Ann. Rheum. Dis. 1969, 28, 121–138. [Google Scholar] [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2015 (ST/ESA/SER.A/390). Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf (accessed on 28 April 2015).
- Bevölkerung Deutschlands bis 2060. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Bevoelkerungsvorausberechnung/Publikationen/Downloads-Vorausberechnung/bevoelkerung-deutschland-2060-presse-5124204159004.pdf?__blob=publicationFile (accessed on 28 April 2015).
- Chung, S.S.; Lee, C.S.; Chung, K.H. Factors affecting the surgical results of expansive laminoplasty for cervical spondylotic myelopathy. Int. Orthop. 2002, 26, 334–338. [Google Scholar] [CrossRef]
- Suda, K.; Abumi, K.; Ito, M.; Shono, Y.; Kaneda, K.; Fujiya, M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2003, 28, 1258–1262. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Tetreault, L.A.; Riew, K.D.; Middleton, J.W.; Aarabi, B.; Arnold, P.M.; Brodke, D.S.; Burns, A.S.; Carette, S.; Chen, R.; et al. A Clinical Practice Guideline for the Management of Patients With Degenerative Cervical Myelopathy: Recommendations for Patients With Mild, Moderate, and Severe Disease and Nonmyelopathic Patients With Evidence of Cord Compression. Glob. Spine J. 2017, 7, 70S–83S. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Tetreault, L.A.; Riew, K.D.; Middleton, J.W.; Wang, J.C. A Clinical Practice Guideline for the Management of Degenerative Cervical Myelopathy: Introduction, Rationale, and Scope. Glob. Spine J. 2017, 7, 21S–27S. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Jha, N.K.; Hewson, S.M.; Massicotte, E.M.; Kopjar, B.; Kalsi-Ryan, S. Is surgery for cervical spondylotic myelopathy cost-effective? A cost-utility analysis based on data from the AOSpine North America prospective CSM study. J. Neurosurg. Spine 2012, 17, 89–93. [Google Scholar] [CrossRef]
- Jalai, C.M.; Worley, N.; Marascalchi, B.J.; Challier, V.; Vira, S.; Yang, S.; Boniello, A.J.; Bendo, J.A.; Lafage, V.; Passias, P.G. The Impact of Advanced Age on Peri-Operative Outcomes in the Surgical Treatment of Cervical Spondylotic Myelopathy: A Nationwide Study Between 2001 and 2010. Spine (Phila Pa 1976) 2016, 41, E139–E1147. [Google Scholar] [CrossRef]
- Nagashima, H.; Dokai, T.; Hashiguchi, H.; Ishii, H.; Kameyama, Y.; Katae, Y.; Morio, Y.; Morishita, T.; Murata, M.; Nanjo, Y.; et al. Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: A multi-center retrospective study. Eur. Spine J. 2011, 20, 240–246. [Google Scholar] [CrossRef]
- Yoshida, G.; Kanemura, T.; Ishikawa, Y.; Matsumoto, A.; Ito, Z.; Tauchi, R.; Muramoto, A.; Matsuyama, Y.; Ishiguro, N. The effects of surgery on locomotion in elderly patients with cervical spondylotic myelopathy. Eur. Spine J. 2013, 22, 2545–2551. [Google Scholar] [CrossRef]
- Yamazaki, T.; Yanaka, K.; Sato, H.; Uemura, K.; Tsukada, A.; Nose, T. Cervical spondylotic myelopathy: Surgical results and factors affecting outcome with special reference to age differences. Neurosurgery 2003, 52, 122–126. [Google Scholar]
- Son, D.K.; Son, D.W.; Song, G.S.; Lee, S.W. Effectiveness of the laminoplasty in the elderly patients with cervical spondylotic myelopathy. Korean J. Spine 2014, 11, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Kanamori, M.; Ishihara, H.; Ohmori, K.; Abe, Y.; Kimura, T. Pathomechanism of myelopathy and surgical results of laminoplasty in elderly patients with cervical spondylosis. Spine (Phila Pa 1976) 2003, 28, 2209–2214. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.; Shibata, T.; Oki, S.; Kawatani, Y.; Mashima, N.; Oishi, H. Outcomes of surgical treatment for cervical myelopathy in patients more than 75 years of age. Spine 1999, 24, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Benzel, E.C.; Lancon, J.; Kesterson, L.; Hadden, T. Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J. Spinal Disord. 1991, 4, 286–295. [Google Scholar] [CrossRef]
- Hirabayashi, K.; Satomi, K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976) 1988, 13, 870–876. [Google Scholar] [CrossRef]
- Tetreault, L.; Nouri, A.; Kopjar, B.; Cote, P.; Fehlings, M.G. The Minimum Clinically Important Difference of the Modified Japanese Orthopaedic Association Scale in Patients with Degenerative Cervical Myelopathy. Spine (Phila Pa 1976) 2015, 40, 1653–1659. [Google Scholar] [CrossRef]
- Tetreault, L.A.; Karpova, A.; Fehlings, M.G. Predictors of outcome in patients with degenerative cervical spondylotic myelopathy undergoing surgical treatment: Results of a systematic review. Eur. Spine J. 2015, 24 (Suppl. 2), 236–251. [Google Scholar] [CrossRef]
- Holly, L.T.; Matz, P.G.; Anderson, P.A.; Groff, M.W.; Heary, R.F.; Kaiser, M.G.; Mummaneni, P.V.; Ryken, T.C.; Choudhri, T.F.; Vresilovic, E.J.; et al. Clinical prognostic indicators of surgical outcome in cervical spondylotic myelopathy. J. Neurosurg. Spine 2009, 11, 112–118. [Google Scholar] [CrossRef]
- Tanaka, J.; Seki, N.; Tokimura, F.; Doi, K.; Inoue, S. Operative results of canal-expansive laminoplasty for cervical spondylotic myelopathy in elderly patients. Spine (Phila Pa 1976) 1999, 24, 2308–2312. [Google Scholar] [CrossRef]
- Machino, M.; Yukawa, Y.; Hida, T.; Ito, K.; Nakashima, H.; Kanbara, S.; Morita, D.; Kato, F. Can elderly patients recover adequately after laminoplasty? A comparative study of 520 patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012, 37, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Madhavan, K.; Chieng, L.O.; Foong, H.; Wang, M.Y. Surgical outcomes of elderly patients with cervical spondylotic myelopathy: A meta-analysis of studies reporting on 2868 patients. Neurosurg. Focus 2016, 40, E13. [Google Scholar] [CrossRef] [PubMed]


| G1 | G2 | G3 | p-Value | |
|---|---|---|---|---|
| Median Age | 44.45 ± 4.57 | 60.34 ± 5.61 | 75.66 ± 5.06 | - |
| Male | 42 | 144 | 77 | - |
| Female | 32 | 60 | 56 | - |
| Charlson Comorbidity Index (%) | 95.7 ± 11.6 | 86.5 ± 13.5 | 50.8 ± 26.2 | p < 0.001 |
| Symptom duration (weeks) | 22.19 ± 22.08 | 33.3 ± 43.62 | 45.88 ± 66.02 | p = 0.003 |
| Stay at the hospital (days) | 8.6 ± 3.8 | 9.6 ± 4.0 | 10.5 ± 4.7 | p < 0.001 |
| Neurological Outcome | G1 | G2 | G3 | p-Value |
|---|---|---|---|---|
| mJOA Score preoperative | 14.99 ± 2.17 | 14.57 ± 2.27 | 13.57 ± 2.51 | p < 0.001 |
| mJOA Score postoperative | 15.78 ± 2.22 | 15.32 ± 2.47 | 14.23 ± 2.56 | p < 0.001 |
| mJOA Score 3 months postoperative | 16.58 ± 1.90 | 16.30 ± 1.92 | 15.45 ± 2.02 | p < 0.001 |
| mJOA Score 6 months postoperative | 17.25 ± 1.36 | 16.99 ± 1.39 | 16.32 ± 1.69 | p < 0.001 |
| NRR (%) postoperative | 37.6 | 32.9 | 19.5 | p < 0.001 |
| NRR (%) 3 months postoperative | 65.2 | 60.3 | 46.2 | p < 0.001 |
| NRR (%) 6 months postoperative | 83.4 | 75.8 | 61.9 | p < 0.001 |
| Mean mJOA Score improvement postoperative | 0.76 ± 0.79 | 0.74 ± 0.97 | 0.66 ± 1.02 | p = 0.186 |
| Mean mJOA Score improvement 3 months postoperative | 1.58 ± 0.90 | 1.60 ± 0.89 | 1.58 ± 1.13 | p = 0.948 |
| Mean mJOA Score improvement 6 months postoperative | 1.95 ± 1.04 | 2.01 ± 1.04 | 2.00 ± 0.91 | p = 0.835 |
| MCID postoperative | 39/74 (52.7%) | 100/204 (49.0%) | 46/133 (34.6%) | p = 0.011 |
| MCID 3 months postoperative | 64/72 (88.9%) | 155/192 (80.7%) | 86/120 (71.7%) | p = 0.014 |
| MCID 6 months postoperative | 60/61 (98.4%) | 153/164 (93.3%) | 78/91 (85.7%) | p = 0.012 |
| First Symptom | G1 | G2 | G3 |
|---|---|---|---|
| Cervicobrachial neuralgia | 36 (48.6%) | 88 (43.1%) | 40 (30.1%) |
| Sensory deficit | 18 (24.3%) | 38 (18.6%) | 23 (17.3%) |
| Paresis | 5 (6.8%) | 17 (8.4%) | 16 (12.0%) |
| Ataxia | 15 (20.3%) | 61 (29.9%) | 54 (40.6%) |
| G1 | G2 | G3 | ||
|---|---|---|---|---|
| Surgical Treatment | ACDF | 64 | 130 | 49 |
| Laminoplasty | 9 | 61 | 47 | |
| Laminectomy | 1 | 13 | 37 | |
| Complications | Surgical | 1/74 (1.4%) | 5/204 (2.5%) | 9/133 (6.8%) |
| Non-surgical | 1/74 (1.4%) | 3/204 (1.5%) | 8/133 (6.0%) | |
| MCID Achievement 6 Months Postoperative | p-Value | |||
|---|---|---|---|---|
| Yes | No | |||
| Approach | ventral | 181 | 14 | p = 0.669 |
| dorsal | 110 | 11 | ||
| Number of operated levels | monosegmental | 162 | 11 | p = 0.521 |
| bisegmental | 69 | 7 | ||
| multisegmental | 60 | 7 | ||
| Surgical treatment | ACDF | 178 | 14 | p = 0.282 |
| Laminoplasty | 84 | 6 | ||
| Laminectomy | 29 | 5 | ||
| Surgical Treatment | Preoperative | Postoperative | 3 Months Postoperative | 6 Months Postoperative | p-Value | |
|---|---|---|---|---|---|---|
| mJOA Score | ACDF | 14.8 ± 2.3 | 15.6 ± 2.4 | 16.6 ± 1.7 | 17.2 ± 1.3 | <0.001 |
| Laminoplasty | 13.9 ± 2.4 | 14.7 ± 2.4 | 15.7 ± 2.2 | 16.6 ± 1.6 | <0.001 | |
| Laminectomy | 12.9 ± 2.3 | 13.8 ± 2.2 | 14.9 ± 1.8 | 15.7 ± 1.7 | <0.001 | |
| mJOA Score improvement | ACDF | 0.8 ± 06 | 1.5 ± 0.8 | 1.9 ± 1.0 | <0.001 | |
| Laminoplasty | 0.8 ± 0.7 | 1.8 ± 0.9 | 2.3 ± 0.9 | <0.001 | ||
| Laminectomy | 0.8 ± 0.8 | 1.8 ± 1.0 | 2.1 ± 0.8 | <0.001 | ||
| NRR | ACDF | 33.8 ± 33.6 | 61.9 ± 33.4 | 76.9 ± 30.2 | <0.001 | |
| Laminoplasty | 25.0 ± 26.9 | 53.6 ± 31.4 | 71.6 ± 27.0 | <0.001 | ||
| Laminectomy | 21.4 ± 24.6 | 41.6 ± 23.5 | 54.1 ± 24.5 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gembruch, O.; Jabbarli, R.; Rashidi, A.; Chihi, M.; El Hindy, N.; Wetter, A.; Hütter, B.-O.; Sure, U.; Dammann, P.; Özkan, N. Degenerative Cervical Myelopathy in Higher-Aged Patients: How Do They Benefit from Surgery? J. Clin. Med. 2020, 9, 62. https://doi.org/10.3390/jcm9010062
Gembruch O, Jabbarli R, Rashidi A, Chihi M, El Hindy N, Wetter A, Hütter B-O, Sure U, Dammann P, Özkan N. Degenerative Cervical Myelopathy in Higher-Aged Patients: How Do They Benefit from Surgery? Journal of Clinical Medicine. 2020; 9(1):62. https://doi.org/10.3390/jcm9010062
Chicago/Turabian StyleGembruch, Oliver, Ramazan Jabbarli, Ali Rashidi, Mehdi Chihi, Nicolai El Hindy, Axel Wetter, Bernd-Otto Hütter, Ulrich Sure, Philipp Dammann, and Neriman Özkan. 2020. "Degenerative Cervical Myelopathy in Higher-Aged Patients: How Do They Benefit from Surgery?" Journal of Clinical Medicine 9, no. 1: 62. https://doi.org/10.3390/jcm9010062
APA StyleGembruch, O., Jabbarli, R., Rashidi, A., Chihi, M., El Hindy, N., Wetter, A., Hütter, B.-O., Sure, U., Dammann, P., & Özkan, N. (2020). Degenerative Cervical Myelopathy in Higher-Aged Patients: How Do They Benefit from Surgery? Journal of Clinical Medicine, 9(1), 62. https://doi.org/10.3390/jcm9010062






