Prediction of Recurrent Emergency Department Visits among Patients with Crohn’s Disease: A Retrospective Study
Abstract
:1. Introduction
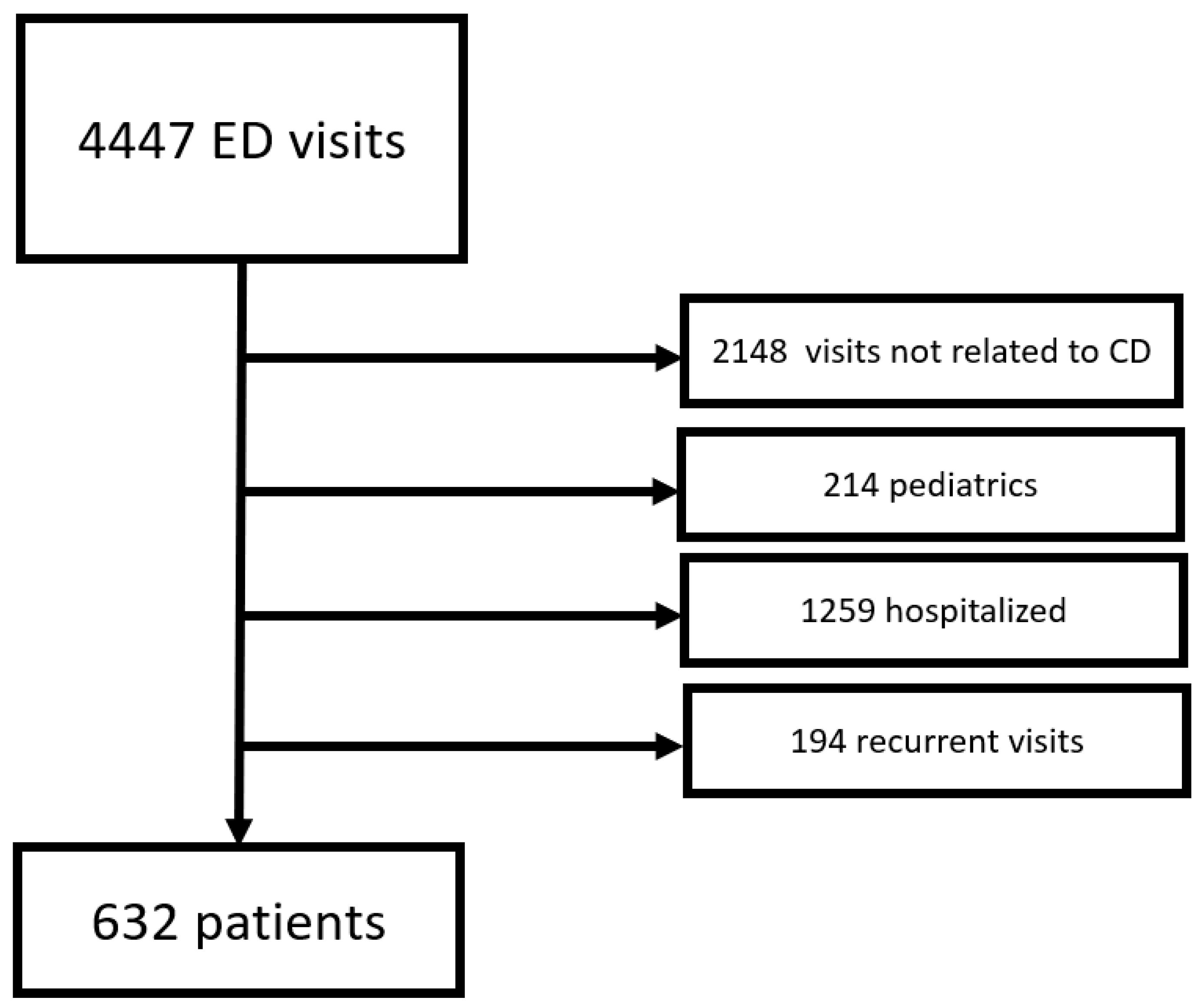
2. Experimental Section
2.1. Statistical Analysis
2.2. Ethical Approval
3. Results
3.1. Re-Visiting ED within 7 Days
3.2. Re-Visiting ED within 30 Days
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Danese, S.; Fiocchi, C. Etiopathogenesis of inflammatory bowel diseases. World J. Gastroenterol. 2006, 12, 4807–4812. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.K.; Wong, S.H.; Ng, S.C. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest. Res. 2016, 14, 111–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molodecky, N.A.; Soon, I.S.; Rabi, D.M.; Ghali, W.A.; Ferris, M.; Chernoff, G.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Barkema, H.W.; et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef]
- Kappelman, M.D.; Rifas-Shiman, S.L.; Porter, C.Q.; Ollendorf, D.A.; Sandler, R.S.; Galanko, J.A.; Finkelstein, J.A. Direct Health Care Costs of Crohn’s Disease and Ulcerative Colitis in US Children and Adults. Gastroenterology 2008, 135, 1907–1913. [Google Scholar] [CrossRef] [Green Version]
- Prenzler, A.; Bokemeyer, B.; Von Der Schulenburg, J.M.; Mittendorf, T. Health care costs and their predictors of inflammatory bowel diseases in Germany. Eur. J. Health Econ. 2011, 12, 273–283. [Google Scholar] [CrossRef]
- Scott, F.I.; Johnson, F.R.; Bewtra, M.; Brensinger, C.M.; Roy, J.A.; Reed, S.D.; Osterman, M.T.; Mamtani, R.; Chen, L.; Yun, H.; et al. Improved Quality of Life with Anti-TNF Therapy Compared with Continued Corticosteroid Utilization in Crohn’s Disease. Inflamm. Bowel Dis. 2019, 25, 925–936. [Google Scholar] [CrossRef]
- Frolkis, A.D.; Dykeman, J.; Negrón, M.E.; Debruyn, J.; Jette, N.; Fiest, K.M.; Frolkis, T.; Barkema, H.W.; Rioux, K.P.; Panaccione, R.; et al. Risk of surgery for inflammatory bowel diseases has decreased over time: A systematic review and meta-analysis of population-based studies. Gastroenterology 2013, 145, 996–1006. [Google Scholar] [CrossRef]
- Abraham, N.S.; Richardson, P.; Castillo, D.; Kane, S.V. Dual therapy with infliximab and immunomodulator reduces one-year rates of hospitalization and surgery among veterans with inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 2013, 11, 1281–1287. [Google Scholar] [CrossRef]
- Huh, G.; Yoon, H.; Choi, Y.J.; Shin, C.M.; Park, Y.S.; Kim, N.; Lee, D.H.; Kim, J.S. Trends in emergency department visits and hospitalization rates for inflammatory bowel disease in the era of biologics. PLoS ONE 2019, 14. [Google Scholar] [CrossRef]
- Nugent, Z.; Singh, H.; Targownik, L.E.; Strome, T.; Snider, C.; Bernstein, C.N. Predictors of emergency department use by persons with inflammatory bowel diseases: A population-based study. Inflamm. Bowel Dis. 2016, 22, 2907–2916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gajendran, M.; Umapathy, C.; Loganathan, P.; Hashash, J.G.; Koutroubakis, I.E.; Binion, D.G. Analysis of Hospital-Based Emergency Department Visits for Inflammatory Bowel Disease in the USA. Dig. Dis. Sci. 2016, 61, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Ballou, S.; Hirsch, W.; Singh, P.; Rangan, V.; Nee, J.; Iturrino, J.; Sommers, T.; Zubiago, J.; Sengupta, N.; Bollom, A.; et al. Emergency department utilisation for inflammatory bowel disease in the United States from 2006 to 2014. Aliment. Pharmacol. Ther. 2018, 47, 913–921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longobardi, T.; Jacobs, P.; Bernstein, C.N. Utilization of Health Care Resources by Individuals with Inflammatory Bowel Disease in the United States: A Profile of Time since Diagnosis. Am. J. Gastroenterol. 2004, 99, 650–655. [Google Scholar] [CrossRef]
- Kappelman, M.D.; Porter, C.Q.; Galanko, J.A.; Rifas-Shiman, S.L.; Ollendorf, D.A.; Sandler, R.S.; Finkelstein, J.A. Utilization of healthcare resources by U.S. children and adults with inflammatory bowel disease. Inflamm. Bowel Dis. 2011, 17, 62–68. [Google Scholar] [CrossRef]
- Pant, C.; Deshpande, A.; Fraga-Lovejoy, C.; O’connor, J.; Gilroy, R.; Olyaee, M. Emergency department visits related to inflammatory bowel disease: Results from nationwide emergency department sample. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 282–284. [Google Scholar] [CrossRef]
- Jung, Y.S.; Park, D.I.; Hong, S.N.; Kim, E.R.; Kim, Y.H.; Cheon, J.H.; Eun, C.S.; Han, D.S.; Lee, C.K.; Kim, J.H.; et al. Predictors of Urgent Findings on Abdominopelvic CT in Patients with Crohn’s Disease Presenting to the Emergency Department. Dig. Dis. Sci. 2015, 60, 929–935. [Google Scholar] [CrossRef]
- Yarur, A.J.; Mandalia, A.B.; Dauer, R.M.; Czul, F.; Deshpande, A.R.; Kerman, D.H.; Abreu, M.T.; Sussman, D.A. Predictive factors for clinically actionable computed tomography findings in inflammatory bowel disease patients seen in the emergency department with acute gastrointestinal symptoms. J. Crohn’s Colitis 2014, 8, 504–512. [Google Scholar] [CrossRef] [Green Version]
- Long, G.H.; Tatro, A.R.; Oh, Y.S.; Reddy, S.R.; Ananthakrishnan, A.N. Analysis of Safety, Medical Resource Utilization, and Treatment Costs by Drug Class for Management of Inflammatory Bowel Disease in the United States Based on Insurance Claims Data. Adv. Ther. 2019, 36, 3079–3095. [Google Scholar] [CrossRef] [Green Version]
- Hoffenberg, E.J.; Park, K.T.; Dykes, D.M.; Fridge, J.; Kappelman, M.D.; Leibowitz, I.H.; Tsou, V.M.; Colletti, R.B. Appropriateness of emergency department use in pediatric inflammatory bowel disease: A quality improvement opportunity. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 324–326. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, G.C.; Bouchard, S.; Diong, C. Access to Specialists and Emergency Department Visits in Inflammatory Bowel Disease: A Population-Based Study. J. Crohn’s Colitis 2018, 13, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Nene, S.; Gonczi, L.; Kurti, Z.; Morin, I.; Chavez, K.; Verdon, C.; Reinglas, J.; Kohen, R.; Bessissow, T.; Afif, W.; et al. Benefits of implementing a rapid access clinic in a high-volume inflammatory bowel disease center: Access, resource utilization and outcomes. World J. Gastroenterol. 2020, 26, 759–769. [Google Scholar] [CrossRef] [PubMed]
| Variable | Study Population n = 632 | No Recurrent ED Visit in 7 Days (n = 579) | Recurrent ED Visit within 7 Days (n = 53) | p-Value |
|---|---|---|---|---|
| Gender (Male) | 279 (47%) | 45.8% | 60.4% | 0.045 |
| Age (y) | 36 (26, 48.7) | 36 (25, 49) | 39 (31.5, 47.5) | 0.19 |
| Comorbidities | ||||
| Smoker | 14 (2.2%) | 2.4% | 0.0% | 0.252 |
| Hyperlipidemia | 31 (4.9%) | 4.8% | 5.7% | 0.790 |
| Hypertension | 31 (4.9%) | 6.9% | 7.5% | 0.861 |
| Diabetes mellitus | 33 (5.2%) | 5.4% | 3.8% | 0.621 |
| IBD treatments | ||||
| Prednisone | 60 (9.5%) | 9.2% | 13.2% | 0.335 |
| Biologics | 122 (19.3%) | 19.7% | 15.1% | 0.473 |
| immunomodulators | 100 (15.8%) | 16.1% | 13.2% | 0.697 |
| Time of ED visits | ||||
| day of arrival (Sunday–Thursday) | 503 (79%) | 80.1% | 73.6% | 0.285 |
| morning shift | 323 (51.1%) | 51.8% | 43.4% | 0.413 |
| afternoon shift | 212 (33.5%) | 32.8% | 41.5% | |
| night shift | 97 (15.3%) | 15.4% | 15.1% | |
| Clinical features | ||||
| Tachycardia | 15.2% | 13.8% | 30.2% | 0.001 |
| Fever | 36.8 ± 0.4 | 36.8 ± 0.38 | 36.8 ± 0.43 | 0.65 |
| Pain > 3 | 45.1% | 44.0% | 57.1% | 0.134 |
| Laboratory tests | ||||
| WBC | 9.3 ± 3.1 | 9.20 ± 3.11 | 10.15 ± 3.27 | 0.501 |
| Anemia | 42.4% | 42.0% | 47.2% | 0.463 |
| PLT | 266 (219, 335) | 267 (221, 338) | 257 (212, 318) | 0.531 |
| Creatinine | 0.8 (0.67, 0.96) | 0.8 (0.67, 0.96) | 0.82 (0.69, 0.93) | 0.49 |
| Hypoalbuminemia | 15.6% | 14.6% | 25.0% | 0.124 |
| Bilirubin | 0.48 (0.34, 0.67) | 0.48 (0.34, 0.66) | 0.49 (0.32, 0.79) | 0.49 |
| Elevated ALP | 17.1% | 15.8% | 30.6% | 0.009 |
| Abnormal AST | 16.9% | 16.6% | 20.8% | 0.44 |
| Abnormal ALT | 17.2% | 16.9% | 20.8% | 0.48 |
| LDH | 186 (155.5, 228) | 184.0 (155.0, 225.0) | 212.0 (164.0, 254.0) | 0.086 |
| Hyponatremia | 13.4% | 12.0% | 28.3% | 0.001 |
| CRP | 11.0 (3.9, 26.0) | 10.9 (3.8, 26.9) | 12.1 (7.6, 19.6) | 0.581 |
| OR | 95% CI | p-Value | ||
|---|---|---|---|---|
| Tachycardia | 2.194 | 1.111 | 4.334 | 0.024 |
| Elevated ALP | 2.088 | 1.070 | 4.072 | 0.031 |
| Hyponatremia | 2.516 | 1.241 | 5.102 | 0.010 |
| Variable | Study Population n = 632 | No Recurrent ED Visit in 30 Days (n = 531) | No Recurrent ED Visit in 30 Days (n = 101) | p-Value |
|---|---|---|---|---|
| Gender (Male) | 279 (47%) | 43.9% | 63.4% | <0.001 |
| Age (year) | 36 (26, 48.7) | 36 (25, 47) | 39 (28, 50) | 0.09 |
| Comorbidities | ||||
| Smoker | 14 (2.2%) | 2.4% | 1.0% | 0.710 |
| Hyperlipidemia | 31 (4.9%) | 1.1% | 2.0% | 0.620 |
| Hypertension | 31 (4.9%) | 6.6% | 8.9% | 0.401 |
| Diabetes mellitus | 33 (5.2%) | 5.1% | 5.9% | 0.723 |
| IBD treatments | ||||
| Prednisone | 60 (9.5%) | 8.7% | 13.9% | 0.102 |
| Biologics | 20.0% | 15.8% | 0.336 | |
| Immunomodulators | 16.4% | 12.9% | 0.375 | |
| Time of ED visits | ||||
| Day of arrival (Sunday–Thursday) | 503 (79%) | 80.8% | 73.3% | 0.086 |
| Morning shift | 323 (51.1%) | 52.7% | 42.6% | 0.064 |
| Afternoon shift | 212 (33.5%) | 31.6% | 43.6% | |
| Night shift | 97 (15.3%) | 15.6% | 13.9% | |
| Clinical features | ||||
| Pulse > 100 (bpm) | 15.2% | 12.9% | 27.0% | <0.001 |
| Fever | 36.8 ± 0.4 | 36.8 ± 0.38 | 36.87 ± 0.41 | 0.180 |
| Pain > 3 | 45.1% | 42.4% | 60.0% | 0.009 |
| Laboratory tests | ||||
| WBC | 9.3 ± 3.1 | 9.24 ± 3.15 | 9.47 ± 3.06 | 0.501 |
| Anemia | 42.4% | 40.5% | 52.5% | 0.025 |
| PLT | 266 (219, 335) | 265 (221, 332) | 269 (215, 362) | 0.511 |
| Creatinine | 0.8 (0.67, 0.96) | 0.79 (0.67, 0.95) | 0.69 (0.83, 0.96) | 0.123 |
| Hypoalbuminemia | 15.6% | 13.6% | 25.5% | 0.027 |
| Bilirubin | 0.48 (0.34, 0.67) | 0.48 (0.34, 0.66) | 0.46 (0.33, 0.73) | 0.919 |
| Alkaline phosphatase > 120 | 17.1% | 14.9% | 28.3% | 0.002 |
| Abnormal AST | 16.9% | 16.4% | 19.8% | 0.40 |
| Abnormal ALT | 17.2% | 16.9% | 18.8% | 0.65 |
| LDH | 186 (155.5, 228) | 185.0 (155.7, 225.0) | 189.0 (149.0, 250.0) | 0.624 |
| Hyponatremia | 13.4% | 11.8% | 21.8% | 0.007 |
| CRP | 11.0 (3.9, 26.0) | 10.6 (3.8, 25.8) | 12.4 (7.7, 28.9) | 0.341 |
| OR | 95% CI | p-Value | ||
|---|---|---|---|---|
| Tachycardia | 2.756 | 1.275 | 5.958 | 0.010 |
| Anemia | 2.177 | 1.118 | 4.240 | 0.022 |
| Elevated alkaline phosphatase | 2.614 | 1.226 | 5.573 | 0.013 |
| Pain intensity >3 (in numeric pain intensity scale 1–10) | 1.892 | 0.894 | 4.006 | 0.095 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahajna, H.; Barash, Y.; Ungar, B.; Soffer, S.; Albshesh, A.; Levartovsky, A.; Ben-Horin, S.; Klang, E.; Kopylov, U. Prediction of Recurrent Emergency Department Visits among Patients with Crohn’s Disease: A Retrospective Study. J. Clin. Med. 2020, 9, 3651. https://doi.org/10.3390/jcm9113651
Mahajna H, Barash Y, Ungar B, Soffer S, Albshesh A, Levartovsky A, Ben-Horin S, Klang E, Kopylov U. Prediction of Recurrent Emergency Department Visits among Patients with Crohn’s Disease: A Retrospective Study. Journal of Clinical Medicine. 2020; 9(11):3651. https://doi.org/10.3390/jcm9113651
Chicago/Turabian StyleMahajna, Hussein, Yiftach Barash, Bella Ungar, Shelly Soffer, Ahmad Albshesh, Asaf Levartovsky, Shomron Ben-Horin, Eyal Klang, and Uri Kopylov. 2020. "Prediction of Recurrent Emergency Department Visits among Patients with Crohn’s Disease: A Retrospective Study" Journal of Clinical Medicine 9, no. 11: 3651. https://doi.org/10.3390/jcm9113651
APA StyleMahajna, H., Barash, Y., Ungar, B., Soffer, S., Albshesh, A., Levartovsky, A., Ben-Horin, S., Klang, E., & Kopylov, U. (2020). Prediction of Recurrent Emergency Department Visits among Patients with Crohn’s Disease: A Retrospective Study. Journal of Clinical Medicine, 9(11), 3651. https://doi.org/10.3390/jcm9113651






