Use of Technology-Based Interventions in the Treatment of Patients with Overweight and Obesity: A Systematic Review
Abstract
1. Introduction
2. Methodology and Quality Assessment
2.1. Data Sources
2.2. Search Strategy
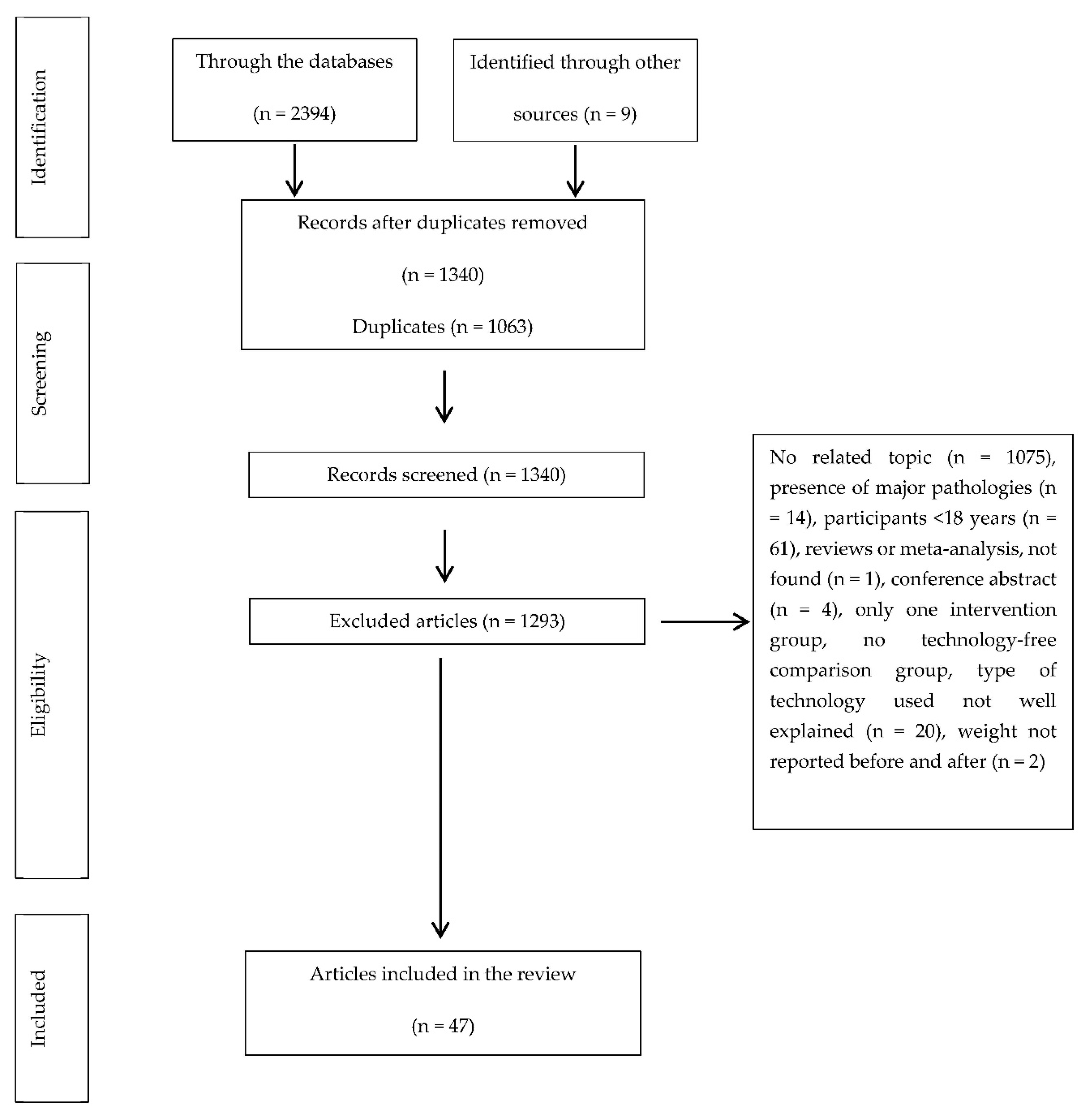
2.3. Selection of Articles
2.4. Inclusion and Exclusion Criteria
2.5. Extracted Data
2.6. Synthesis of Results
3. Results
3.1. Descriptive Data and Types of Studies
3.2. Type of Technology and Provision of Feedback
3.2.1. Smartphone
3.2.2. Virtual Reality
3.2.3. Website
3.2.4. Personal Digital Assistant (PDA) or Electronic Journal (EJ)
3.2.5. Other Types of Technology
3.3. Effectiveness of Each Type of Technology in Weight Loss and/or Maintenance and Adherence
3.3.1. Smartphone
- APPs
- SMS and/or calls
3.3.2. Virtual Reality
3.3.3. Website
3.3.4. Personal Digital Assistant (PDA) or Electronic Journal (EJ)
3.3.5. Other Types of Technology
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Bazán, M.J.A.; Trujillo, M.I.J.; Wärnberg, J.; Fernández, S.D.; Lopez-De-Andrés, A.; Farinós, N.P. Differences in the prevalence of diagnosis of overweight-obesity in Spanish children according to the diagnostic criteria set used. Gac. Sanit. 2018, 32, 477–480. [Google Scholar] [CrossRef]
- Agha, M.; Agha, R. The rising prevalence of obesity. Int. J. Surg. Oncol. 2017, 2, e19. [Google Scholar] [CrossRef]
- Demir, D.; Bektas, M. The effect of childrens’ eating behaviors and parental feeding style on childhood obesity. Eat. Behav. 2017, 26, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Arroyo-Johnson, C.; Mincey, K. Obesity epidemiology trends by race/ethnicity, gender, and education: National Health Interview Survey, 1997–2012. Gastroenterol. Clin. N. Am. 2016, 45, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Meldrum, D.R.; Morris, M.A.; Gambone, J.C. Obesity pandemic: Causes, consequences, and solutions—But do we have the will? Fertil. Steril. 2017, 107, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Aranceta, J.; Pérez-Rodrigo, C.; Alberdi-Aresti, G.; Ramos-Carrera, N.; Lázaro-Masedo, S. Prevalence of General Obesity and Abdominal Obesity in the Spanish Adult Population (Aged 25–64 Years) 2014–2015: The ENPE Study. Rev. Española Cardiol. 2016, 69, 579–587. [Google Scholar] [CrossRef]
- Hernáez, Á.; Zomeño, M.D.; Dégano, I.R.; Pérez-Fernández, S.; Goday, A.; Vila, J.; Civeira, F.; Moure, R.; Marrugat, J. Excess Weight in Spain: Current Situation, Projections for 2030, and Estimated Direct Extra Cost for the Spanish Health System. Rev. Española Cardiol. 2019, 72, 916–924. [Google Scholar] [CrossRef]
- Tanaka, K.; Sasai, H.; Wakaba, K.; Murakami, S.; Ueda, M.; Yamagata, F.; Sawada, M.; Takekoshi, K. Professional dietary coaching within a group chat using a smartphone application for weight loss: A randomized controlled trial. J. Multidiscip. Health 2018, 11, 339–347. [Google Scholar] [CrossRef]
- Coons, M.J.; Roehrig, M.; Spring, B. The potential of virtual reality technologies to improve adherence to weight loss behaviors. J. Diabetes Sci. Technol. 2011, 5, 340–344. [Google Scholar] [CrossRef]
- Napolitano, M.A.; Hayes, S.; Bennett, G.G.; Ives, A.K.; Foster, G.D. Using facebook and text messaging to deliver a weight loss program to college students. Obesity 2013, 21, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.M.; Cesa, G.L.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual Reality–Enhanced Cognitive–Behavioral Therapy for Morbid Obesity: A Randomized Controlled Study with 1 Year Follow-Up. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 134–140. [Google Scholar] [CrossRef]
- Apiñaniz, A.; Cobos-Campos, R.; De Lafuente-Moríñigo, A.S.; Parraza, N.; Aizpuru, F.; Pérez, I.; Goicoechea, E.; Trápaga, N.; García, L. Effectiveness of randomized controlled trial of a mobile app to promote healthy lifestyle in obese and overweight patients. Fam. Pract. 2019, 36, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Horne, M.; Hill, A.; Murells, T.; Ugail, H.; Chinnadorai, R.; Hardy, M. Irving Using avatars in weight management settings: A systematic review. Internet Interv. 2020, 19, 100295. [Google Scholar] [CrossRef] [PubMed]
- Johnston, J.D.; Massey, A.P.; De Vaneaux, C.A. Innovation in Weight Loss Programs: A 3-Dimensional Virtual-World Approach. J. Med. Internet Res. 2012, 14, e120. [Google Scholar] [CrossRef]
- Wharton, C.; Johnston, C.S.; Cunningham, B.K.; Sterner, D. Dietary Self-Monitoring, But Not Dietary Quality, Improves With Use of Smartphone App Technology in an 8-Week Weight Loss Trial. J. Nutr. Educ. Behav. 2014, 46, 440–444. [Google Scholar] [CrossRef]
- Ross, K.M.; Wing, R.R. Impact of newer self-monitoring technology and brief phone-based intervention on weight loss: A randomized pilot study. Obesity 2016, 24, 1653–1659. [Google Scholar] [CrossRef]
- Thomas, J.G.; Raynor, H.A.; Bond, D.S.; Luke, A.; Cardoso, C.C.; Wojtanowski, A.C.; Veur, S.V.; Tate, D.; Wing, R.R.; Foster, G.D. Weight loss and frequency of body-weight self-monitoring in an online commercial weight management program with and without a cellular-connected ‘smart’ scale: A randomized pilot study. Obes. Sci. Pract. 2017, 3, 365–372. [Google Scholar] [CrossRef]
- Hutchesson, M.J.; Tan, C.Y.; Morgan, P.J.; Callister, R.; Collins, C.E. Enhancement of Self-Monitoring in a Web-Based Weight Loss Program by Extra Individualized Feedback and Reminders: Randomized Trial. J. Med. Internet Res. 2016, 18, e82. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Petticrew, M.; Roberts, H. Systematic Reviews in the Social Sciences: A Practical Guide; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- He, C.; Wu, S.; Zhao, Y.; Li, Z.; Zhang, Y.; Le, J.; Wang, L.; Wan, S.; Li, C.; Li, Y.; et al. Social Media–Promoted Weight Loss Among an Occupational Population: Cohort Study Using a WeChat Mobile Phone App-Based Campaign. J. Med. Internet Res. 2017, 19, e357. [Google Scholar] [CrossRef] [PubMed]
- Spring, B.; Pellegrini, C.A.; Pfammatter, A.; Duncan, J.M.; Pictor, A.; McFadden, H.G.; Siddique, J.; Hedeker, D. Effects of an abbreviated obesity intervention supported by mobile technology: The ENGAGED randomized clinical trial. Obesity 2017, 25, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.G.; Bond, D.S.; Raynor, H.A.; Papandonatos, G.D.; Wing, R.R. Comparison of Smartphone-Based Behavioral Obesity Treatment with Gold Standard Group Treatment and Control: A Randomized Trial. Obesity 2019, 27, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Svetkey, L.P.; Batch, B.C.; Lin, P.-H.; Intille, S.S.; Corsino, L.; Tyson, C.C.; Bosworth, H.B.; Grambow, S.C.; Voils, C.; Loria, C.; et al. Cell phone intervention for you (CITY): A randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology. Obesity 2015, 23, 2133–2141. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.K.; Stephens, J.; Himmelfarb, C.R.D.; Stewart, K.J.; Hauck, S. Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment. J. Obes. 2013, 2013, 1–7. [Google Scholar] [CrossRef]
- Turner-McGrievy, G.; Tate, D.; Hurling, R. Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention Among Adults. J. Med. Internet Res. 2011, 13, e120. [Google Scholar] [CrossRef]
- Lee, W.; Chae, Y.M.; Kim, S.; Ho, S.H.; Choi, I. Evaluation of a mobile phone-based diet game for weight control. J. Telemed. Telecare 2010, 16, 270–275. [Google Scholar] [CrossRef]
- Laing, B.Y.; Mangione, C.M.; Tseng, C.-H.; Leng, M.; Vaisberg, E.; Mahida, M.; Bholat, M.; Glazier, E.; Morisky, D.E.; Bell, D.S. Effectiveness of a Smartphone Application for Weight Loss Compared With Usual Care in Overweight Primary Care Patients. Ann. Intern. Med. 2014, 161, S5–S12. [Google Scholar] [CrossRef]
- Stephens, J.D.; Yager, A.M.; Allen, J. Smartphone Technology and Text Messaging for Weight Loss in Young Adults. J. Cardiovasc. Nurs. 2017, 32, 39–46. [Google Scholar] [CrossRef]
- Martin, C.K.; Miller, A.C.; Thomas, D.M.; Champagne, C.M.; Han, H.; Church, T. Efficacy of SmartLossSM, a smartphone-based weight loss intervention: Results from a randomized controlled trial. Obesity 2015, 23, 935–942. [Google Scholar] [CrossRef]
- Carter, M.C.; Burley, V.J.; Nykjaer, C.; Cade, J.E. Adherence to a Smartphone Application for Weight Loss Compared to Website and Paper Diary: Pilot Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e32. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Reyes, A.; Cámara-Martos, F.; Molina-Recio, G.; Molina-Luque, R.; Romero-Saldaña, M.; Moreno-Rojas, R.; Pérez, C.T.; Pitti, J.A.; Carrion, C.; Ciptaningtyas, R.; et al. Push Notifications From a Mobile App to Improve the Body Composition of Overweight or Obese Women: Randomized Controlled Trial. JMIR mHealth uHealth 2020, 8, e13747. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.J.; Lang, W.; Gibbs, B.B.; Davis, K.K.; Burke, L.E.; Kovács, S.J.; Portzer, L.A.; Jakicic, J.M. Applying a technology-based system for weight loss in adults with obesity. Obes. Sci. Pract. 2016, 2, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Alencar, M.K.; Johnson, K.; Mullur, R.; Gray, V.; Gutierrez, E.; Korosteleva, O. The efficacy of a telemedicine-based weight loss program with video conference health coaching support. J. Telemed. Telecare 2017, 25, 151–157. [Google Scholar] [CrossRef]
- Lewis, E.; Huang, H.C.; Hassmén, P.; Welvaert, M.; Pumpa, K.L. Adding Telephone and Text Support to an Obesity Management Program Improves Behavioral Adherence and Clinical Outcomes. A Randomized Controlled Crossover Trial. Int. J. Behav. Med. 2019, 26, 580–590. [Google Scholar] [CrossRef]
- Steinberg, D.M.; Levine, E.L.; Askew, S.; Foley, P.; Bennett, G.G.; Wolin, K.; Davy, B. Daily Text Messaging for Weight Control Among Racial and Ethnic Minority Women: Randomized Controlled Pilot Study. J. Med. Internet Res. 2013, 15, e244. [Google Scholar] [CrossRef]
- Shapiro, J.R.; Koro, T.; Doran, N.; Thompson, S.; Sallis, J.F.; Calfas, K.; Patrick, K. Text4Diet: A randomized controlled study using text messaging for weight loss behaviors. Prev. Med. 2012, 55, 412–417. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Davis, K.K.; Rogers, R.J.; King, W.C.; Marcus, M.D.; Helsel, D.; Rickman, A.D.; Wahed, A.S.; Belle, S.H. Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: The IDEA randomized clinical trial. JAMA 2016, 316, 1161–1171. [Google Scholar] [CrossRef]
- Godino, J.; Golaszewski, N.M.; Norman, G.J.; Rock, C.L.; Griswold, W.G.; Arredondo, E.; Marshall, S.; Kolodziejczyk, J.; Dillon, L.; Raab, F.; et al. Text messaging and brief phone calls for weight loss in overweight and obese English- and Spanish-speaking adults: A 1-year, parallel-group, randomized controlled trial. PLoS Med. 2019, 16, e1002917. [Google Scholar] [CrossRef]
- Newton, R.L., Jr.; Carter, L.; Johnson, W.; Zhang, D.; Larrivée, S.; Kennedy, B.M.; Harris, M.; Hsia, D.S. A Church-Based Weight Loss Intervention in African American Adults using Text Messages (LEAN Study): Cluster Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e256. [Google Scholar] [CrossRef]
- Bouhaidar, C.M.; DeShazo, J.P.; Puri, P.; Gray, P.; Robins, J.L.W.; Salyer, J. Text Messaging as Adjunct to Community-Based Weight Management Program. Comput. Inform. Nurs. 2013, 31, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.-H.; Wang, Y.; Levine, E.; Askew, S.; Lin, S.; Chang, C.; Sun, J.; Foley, P.; Wang, H.; Li, X.; et al. A text messaging-assisted randomized lifestyle weight loss clinical trial among overweight adults in Beijing. Obesity 2014, 22, E29–E37. [Google Scholar] [CrossRef] [PubMed]
- Haapala, I.; Barengo, N.C.; Biggs, S.; Surakka, L.; Manninen, P. Weight loss by mobile phone: A 1-year effectiveness study. Public Health Nutr. 2009, 12, 2382–2391. [Google Scholar] [CrossRef] [PubMed]
- Patrick, K.; Raab, F.; Adams, M.A.; Dillon, L.; Zabinski, M.; Rock, C.L.; Griswold, W.G.; Norman, G.J. A Text Message-Based Intervention for Weight Loss: Randomized Controlled Trial. J. Med. Internet Res. 2009, 11, e1. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, D.K.; Goetz, J.R.; Gibson, C.A.; Washburn, R.A.; Smith, B.K.; Lee, J.; Gerald, S.; Fincham, T.; Donnelly, J.E. Improving Weight Maintenance Using Virtual Reality (Second Life). J. Nutr. Educ. Behav. 2013, 45, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Behm-Morawitz, E.; Lewallen, J.; Choi, G. A Second Chance at Health: How a 3D Virtual World Can Improve Health Self-Efficacy for Weight Loss Management Among Adults. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 74–79. [Google Scholar] [CrossRef]
- Morgan, P.J.; Scott, H.; Young, M.D.; Plotnikoff, R.; Collins, C.E.; Callister, R. Associations between program outcomes and adherence to Social Cognitive Theory tasks: Process evaluation of the SHED-IT community weight loss trial for men. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 89. [Google Scholar] [CrossRef]
- Azar, K.M.J.; Aurora, M.; Wang, E.J.; Muzaffar, A.; Pressman, A.; Palaniappan, L.P. Virtual small groups for weight management: An innovative delivery mechanism for evidence-based lifestyle interventions among obese men. Transl. Behav. Med. 2015, 5, 37–44. [Google Scholar] [CrossRef]
- Abdi, J.; Eftekhar, H.; Mahmoodi, M.; Shojayzadeh, D.; Sadeghi, R.; Saber, M. Effect of the Intervention Based on New Communication Technologies and the Social-Cognitive Theory on the Weight Control of the Employees with Overweight and Obesity. J. Res. Health Sci. 2015, 15, 256–261. [Google Scholar]
- Morgan, P.J.; Lubans, D.R.; Collins, C.E.; Warren, J.M.; Callister, R. 12-Month Outcomes and Process Evaluation of the SHED-IT RCT: An Internet-Based Weight Loss Program Targeting Men. Obesity 2011, 19, 142–151. [Google Scholar] [CrossRef]
- Burke, L.E.; Styn, M.A.; Sereika, S.M.; Conroy, M.B.; Ye, L.; Glanz, K.; Sevick, M.A.; Ewing, L.J. Using mHealth Technology to Enhance Self-Monitoring for Weight Loss. Am. J. Prev. Med. 2012, 43, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Sereika, S.M.; Chasens, E.R.; Ewing, L.J.; Matthews, J.T.; Burke, L.E. Effect of adherence to self-monitoring of diet and physical activity on weight loss in a technology-supported behavioral intervention. Patient Prefer. Adherence 2012, 6, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Chung, L.M.-Y.; Law, Q.P.S.; Fong, S.S.M.; Chung, J.W.-Y. Teledietetics Improves Weight Reduction by Modifying Eating Behavior: A Randomized Controlled Trial. Telemed. e-Health 2014, 20, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Spring, B.; Duncan, J.M.; Janke, E.A.; Kozak, A.T.; McFadden, H.G.; DeMott, A.; Pictor, A.; Epstein, L.H.; Siddique, J.; Pellegrini, C.A.; et al. Integrating Technology Into Standard Weight Loss Treatment. JAMA Intern. Med. 2013, 173, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Unick, J.L.; O’Leary, K.C.; Bond, D.S.; Wing, R.R. Physical Activity Enhancement to a Behavioral Weight Loss Program for Severely Obese Individuals: A Preliminary Investigation. ISRN Obes. 2012, 2012, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Shuger, S.L.; Barry, V.W.; Sui, X.; McClain, A.; Hand, G.A.; Wilcox, S.; Meriwether, R.A.; Hardin, J.W.; Blair, S.N. Electronic feedback in a diet- and physical activity-based lifestyle intervention for weight loss: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 41–48. [Google Scholar] [CrossRef]
- Pellegrini, C.A.; Verba, S.D.; Otto, A.D.; Helsel, D.L.; Davis, K.K.; Jakicic, J.M. The Comparison of a Technology-Based System and an In-Person Behavioral Weight Loss Intervention. Obesity 2012, 20, 356–363. [Google Scholar] [CrossRef]
- Dunn, C.; Whetstone, L.M.; Kolasa, K.M.; Jayaratne, K.; Thomas, C.; Aggarwal, S.; Nordby, K.; Riley, K.E. Using Synchronous Distance-Education Technology to Deliver a Weight Management Intervention. J. Nutr. Educ. Behav. 2014, 46, 602–609. [Google Scholar] [CrossRef]
- Chambliss, H.O.; Huber, R.C.; Finley, C.E.; McDoniel, S.O.; Kitzman-Ulrich, H.; Wilkinson, W.J. Computerized self-monitoring and technology-assisted feedback for weight loss with and without an enhanced behavioral component. Patient Educ. Couns. 2011, 85, 375–382. [Google Scholar] [CrossRef]
- Ing, C.T.; Miyamoto, R.E.S.; Fang, R.; Antonio, M.; Paloma, D.; Braun, K.L.; Kaholokula, J.K. Comparing Weight Loss–Maintenance Outcomes of a Worksite-Based Lifestyle Program Delivered via DVD and Face-to-Face: A Randomized Trial. Health Educ. Behav. 2018, 45, 569–580. [Google Scholar] [CrossRef]
- Godino, J.G.; Merchant, G.; Norman, G.J.; Donohue, M.C.; Marshall, S.J.; Fowler, J.H.; Calfas, K.J.; Huang, J.S.; Rock, C.L.; Griswold, W.G.; et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): A 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes Endocrinol. 2016, 4, 747–755. [Google Scholar] [CrossRef]
- Raaijmakers, L.C.; Pouwels, S.; Berghuis, K.A.; Nienhuijs, S.W. Technology-based interventions in the treatment of overweight and obesity: A systematic review. Appetite 2015, 95, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.K.; Stephens, J.; Patel, A. Technology-Assisted Weight Management Interventions: Systematic Review of Clinical Trials. Telemed. e-Health 2014, 20, 1103–1120. [Google Scholar] [CrossRef] [PubMed]
- Hutchesson, M.J.; Rollo, M.E.; Krukowski, R.; Ells, L.; Harvey, J.; Morgan, P.J.; Callister, R.; Plotnikoff, R.; Collins, C.E. eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 2015, 16, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Turk, M.W.; Elci, O.U.; Wang, J.; Sereika, S.M.; Ewing, L.J.; Acharya, S.D.; Glanz, K.; Burke, L.E. Self-Monitoring as a Mediator of Weight Loss in the SMART Randomized Clinical Trial. Int. J. Behav. Med. 2013, 20, 556–561. [Google Scholar] [CrossRef]
- Sherrington, A.; Newham, J.J.; Bell, R.; Adamson, A.J.; McColl, E.; Araujo-Soares, V. Systematic review and meta-analysis of internet-delivered interventions providing personalized feedback for weight loss in overweight and obese adults. Obes. Rev. 2016, 17, 541–551. [Google Scholar] [CrossRef]
- Ahrendt, A.; Kattelmann, K.; Rector, T.S.; Maddox, D.A. The Effectiveness of Telemedicine for Weight Management in theMOVE!Program. J. Rural Health 2013, 30, 113–119. [Google Scholar] [CrossRef]
- Semper, H.; Povey, R.; Clark-Carter, D. A systematic review of the effectiveness of smartphone applications that encourage dietary self-regulatory strategies for weight loss in overweight and obese adults. Obes. Rev. 2016, 17, 895–906. [Google Scholar] [CrossRef]
| Search Strategy | |
|---|---|
| #1. | (“virtual reality exposure therapy” [MeSH * Terms] OR “virtual reality” [Title/Abstract] OR “virtual world” [Title/Abstract] OR “virtual environment” [Title/Abstract] OR “3D vision” [Title/Abstract] OR “smartphone” [Title/Abstract] OR “cell phone” [Title/Abstract] OR “technology” [Title/Abstract]) |
| #2. | (“obesity” [MeSH Terms] OR “obesity” [Title/Abstract] OR “overweight” [MeSH Terms] OR “overweight” [Title/Abstract]) |
| #3. | (“diet therapy” [MeSH Terms] OR “diet therapy” [Title/Abstract] OR “weight loss” [MeSH Terms] OR “weight loss” [Title/Abstract]) |
| #4. | #1. AND #2. AND #3. |
| Authors, Year, [Reference] | Country | Year | Mean Age (Years) | Nr Sample (n) | Objective | Study Type |
|---|---|---|---|---|---|---|
| He et al., 2017, [22] | China | 2017 | 37 | Total: 15,310 | Assess the effectiveness of a mobile app (WeChat) as an intervention in weight loss behavior. | Cohort study |
| Men: 9282 | ||||||
| Women: 6028 | ||||||
| Spring et al., 2017 [23] | USA | 2017 | 39.3 | Total: 96 | Determine the effects on weight loss from three brief behavioral weight loss interventions with and without coaching and mobile technology. | Three-month randomized controlled efficacy study of weight loss |
| Men: 15 | ||||||
| Women: 81 | ||||||
| Ross & Wing., 2016 [17] | USA | 2016 | 51.1 | Total: 80 | Investigate the impact of new self-monitoring technology (compared to traditional self-monitoring tools), provided with and without brief telephone intervention, on weight loss in overweight and obese adults | Randomized pilot study |
| Men: 11 | ||||||
| Women: 69 | ||||||
| Apiñaniz et al., 2019 [13] | Spain | 2019 | 38.55 | Total: 110 | Evaluate the effectiveness of a mobile app to support the provision of health advice for weight loss | Randomized controlled trial |
| Men: 31 | ||||||
| Women: 79 | ||||||
| Wharton et al., 2014 [16] | USA | 2014 | 42 | Total: 47 | Evaluate the use of a smartphone app for diet and weight loss self-monitoring against traditional diet counseling and self-monitoring methods. | Pilot study |
| Men: 12 | ||||||
| Women: 35 | ||||||
| Thomas et al., 2019 [24] | USA | 2019 | 55.1 | Total: 276 | Determine whether the weight losses of a smartphone-based (SMART) behavioral obesity treatment differed from those of more intensive group behavioral obesity treatment (GROUP) and a control condition (CONTROL). | Randomized clinical trial |
| Men: 47 | ||||||
| Women: 229 | ||||||
| Svetkey et al., 2015 [25] | USA | 2015 | 29.4 | Total: 365 | Determine the effect on weight of two mobile technology-based (mHealth) behavioral weight loss interventions in young adults. | Randomized controlled trial |
| Men: 111 | ||||||
| Women: 254 | ||||||
| Allen et al., 2013 [26] | USA | 2013 | 44.9 | Total: 68 | Assess the feasibility, acceptability, and preliminary effectiveness of theory-based behavioral interventions performed with smartphone technology. | Randomized controlled pilot study |
| Men: 15 | ||||||
| Women: 53 | ||||||
| Turner-McGrievy & Tate., 2011 [27] | USA | 2011 | 42.9 | Total: 96 | Examine whether a combination of podcasting, mobile support communication, and mobile diet monitoring can help people lose weight. | Randomized trial |
| Men: 24 | ||||||
| Women: 72 | ||||||
| Lee et a., 2010 [28] | Corea | 2010 | 28.85 | Total: 36 | Evaluate the effectiveness of the SmartDiet mobile phone app compared with the acquisition of dietary information, weight management, and user satisfaction. | Case study control |
| Men: - | ||||||
| Women: - | ||||||
| Laing et al., 2014 [29] | USA | 2014 | 43.3 | Total: 212 | Assess the effect of providing this application of a free and widely used smartphone for weight loss to patients in their primary care clinic. | Randomized controlled trial |
| Men: 154 | ||||||
| Women: 58 | ||||||
| Napolitano et al., 2013 [11] | USA | 2013 | 2 0.47 | Total: 52 | Evaluate the feasibility, acceptability and preliminary effectiveness of a novel technology-based weight loss intervention for college students using adapted evidence-based weight loss content. | Randomized controlled trial |
| Men: 7 | ||||||
| Women: 45 | ||||||
| Stephens et al., 2017 [30] | USA | 2017 | 20 | Total: 62 | Evaluate the effectiveness of a smartphone app, based on behavior for weight loss combined with text messages from a weight-health coach, body mass index, and waist circumference in young adults compared to a control condition. | Randomized controlled trial |
| Men: 18 | ||||||
| Women: 44 | ||||||
| Martin et al., 2015 [31] | USA | 2015 | 44.4 | Total: 40 | Evaluate the effectiveness of SmartLoss, a smartphone-based weight-loss intervention. | Randomized controlled trial |
| Men: 7 | ||||||
| Women: 33 | ||||||
| Carter et al., 2013 [32] | Reino Unido | 2013 | 42 | Total: 128 | Report the acceptability and feasibility of a weight management self-monitoring intervention performed with a smartphone app, compared to a website and a written diary. | Randomized controlled pilot study |
| Men: 29 | ||||||
| Women: 99 | ||||||
| Hernández-Reyes et al., 2020 [33] | Spain | 2020 | 41.5 | 60 Women | Evaluate the effectiveness of "push notifications" in an intervention to improve body composition of overweight or obese adult women, through a dietary procedure, and analyze the evolution of body composition based on push notifications and prescribed physical activity (PA). | Randomized controlled trial |
| Rogers et al., 2016 [34] | USA | 2016 | 39.9 | Total: 39 | Compare a group of behavioral weight loss in-person intervention with technological interventions in obese adults. | Randomized pretest posttest design |
| Men: 8 | ||||||
| Women: 31 | ||||||
| Alencar et al., 2019 [35] | USA | 2019 | 46.8 | Total: 25 | Determine the effectiveness of a medically controlled weight management program with weekly health training versus no health training through weight loss video-conferences using mobile health devices. | Randomized controlled trial |
| Men: 12 | ||||||
| Women: 13 | ||||||
| Lewis et al., 2019 [36] | Australia | 2019 | 49 | Total: 61 | Investigate the effectiveness and optimal timing of using phone calls and text messages as complementary tools to support a community obesity management program. | Randomized cross-controlled trial |
| Men: 14 | ||||||
| Women: 47 | ||||||
| Steinberg et al., 2013 [37] | USA | 2013 | 38.3 | 50 Women | Assess the feasibility of a text message intervention for weight loss among predominantly Black women. | Randomized controlled pilot study |
| Shapiro et al., 2012 [38] | USA | 2012 | 41.9 | Total: 170 | Evaluate a daily intervention of weight loss through text messages | Randomized controlled trial |
| Men: 111 | ||||||
| Women: 59 | ||||||
| Jakicic et al., 2016 [39] | USA | 2016 | 3 0.9 | Total: 470 | Assess whether adding portable technology to a behavioral intervention would improve weight loss for 24 months among 18- to 35-year-olds | Randomized controlled trial |
| Men: 136 | ||||||
| Women: 334 | ||||||
| Godino et al., 2019 [40] | USA | 2019 | 41.7 | Total: 298 | Examine the effectiveness of a 1-year intervention designed to reduce weight among overweight and obese English- and Spanish-speaking adults via SMS (ConTxt) alone or in combination with short monthly health coaching calls. | Randomized controlled trial |
| Men: 70 | ||||||
| Women: 228 | ||||||
| Newton et al., 2018 [41] | USA | 2018 | 56 | Total: 97 | Evaluate the feasibility (tolerance and satisfaction of SMS text messages) and the effectiveness (compared to a control group) of using SMS text messages to promote weight loss in African-American adults enrolled in a church-based weight loss program. | Randomized controlled trial |
| Men: 8 | ||||||
| Women: 89 | ||||||
| Bouhaidar et al., 2013 [42] | USA | 2013 | 45 | Total: 28 | Evaluate the effect of personalized text messages on body weight change in overweight and obese adults in a community-based weight management program. | Quasi-experimental analysis with pretest and posttest |
| Men: 2 | ||||||
| Women: 26 | ||||||
| Lin et al., 2014 [43] | China | 2014 | 38.21 | Total: 123 | Test the impact on weight change of a trial of a 6-month text-assisted weight loss intervention in overweight adults in Beijing. | Randomized clinical trial |
| Men: 49 | ||||||
| Women: 74 | ||||||
| Haapala et al., 2009 [44] | United Kingdom | 2009 | 38 | Total: 124 | Investigate short- and long-term effectiveness and weight loss predictors in a mobile phone weight loss program among healthy overweight adults. | Randomized controlled trial |
| Men: 28 | ||||||
| Women: 96 | ||||||
| Patrick et al., 2009 [45] | USA | 2009 | 44.9 | Total: 65 | Determine whether text messages were a useful and effective strategy to help adults control their weight and improve their results. | Randomized controlled trial |
| Men: 13 | ||||||
| Women: 52 | ||||||
| Sullivan et al., 2013 [46] | USA | 2013 | 31.1 | Total: 20 | Evaluate Second Life’s effectiveness for weight loss and maintenance | Randomized trial |
| Men: 3 | ||||||
| Women: 17 | ||||||
| Behm-Morawitz et al., 2016 [47] | USA | 2016 | 25 | Total: 92 | Examine the effectiveness of virtual realization and play in a virtual social world (Second Life) to increase health self-efficacy among overweight adults | Randomized controlled trial |
| Men: 2 | ||||||
| Women: 90 | ||||||
| Johnston et al., 2012 [15] | USA | 2012 | 41.9 | Total: 54 | Explore the effectiveness of a weight loss program in the virtual world in relation to weight loss and behavior change | Quasi experimental |
| Men: 9 | ||||||
| Women: 45 | ||||||
| Manzoni et al., 2016 [12] | Italy | 2016 | 35.63 | 163 Women | Test the long-term effectiveness of enhanced cognitive behavioral obesity therapy (CBT), which includes a virtual reality (VR) module aimed at unlocking the body’s negative memory and modifying its behavioral and emotional correlates | Randomized controlled trial |
| Morgan et al., 2014 [48] | Australia | 2014 | 47.3 | 159 Men | Provide a comprehensive assessment of the SHED-IT (self-help, exercise and diet using information technology) weight loss program process for men | Randomized trial, controlled blinded by the evaluator |
| Azar et al., 2015 [49] | USA | 2015 | 46.3 | 64 Men | Assess whether group interventions using web-based group video conference (VC) technology are effective for weight loss. | Randomized pilot study |
| Abdi et al., 2015 [50] | Iran | 2015 | 42 | Total: 435 | Evaluate the effect of intervention based on new communication technologies and social cognitive theory on weight management in government employees in the city of Hamadan, western Iran, in 2014. | Randomized controlled trial |
| Men: 125 | ||||||
| Women: 310 | ||||||
| Morgan et al., 2011 [51] | Australia | 2011 | 35.9 | 65 Men | Examine the 12-month results of the SHED-IT Internet-based program (Self-Help, Exercise, and Diet Using Information Technology) for overweight men to determine whether they could maintain weight loss. | Randomized controlled trial |
| Burke et al., 2012 [52] | USA | 2012 | 46.8 | Total: 210 | Determine whether diet monitoring using only one PDA or PDA+daily personalized feedback was superior to using a conventional paper diary on weight loss and weight maintenance in a 24-month study. Examine whether weight loss would be greater for those who adhere to self-control (monitoring). | Randomized controlled trial |
| Men: 32 | ||||||
| Women: 178 | ||||||
| Wang et al., 2012 [53] | USA | 2012 | 46.8 | Total: 210 | Report the mediation effect of self-monitoring diet adherence and physical activity on weight loss in overweight or obese participants after 12 months in a technology-based behavioral weight loss program. | Randomized clinical trial |
| Men: 32 | ||||||
| Women: 178 | ||||||
| Chung et al., 2014 [54] | China | 2014 | 37.4 | Total: 60 | Test the effectiveness of dietary TV as an intervention for weight reduction. | Double-blind randomized controlled trial |
| Men: 22 | ||||||
| Women: 38 | ||||||
| Spring et al., 2013 [55] | USA | 2013 | 57.7 | Total: 69 | Test whether a connective mobile technology system, telephone training and standard treatment for obesity improved weight loss outcomes compared to standard group treatment alone for obesity. | Randomized controlled trial |
| Men: 59 | ||||||
| Women: 10 | ||||||
| Unick et al., 2012 [56] | USA | 2012 | 42.4 | Total: 29 | Examine whether the addition of portable PA monitors to the SBWL (standard behavioral weight loss program) treatment for people with severe obesity improved PA and self-control after a 6-month intervention. | Randomized pilot study |
| Men: 5 | ||||||
| Women: 24 | ||||||
| Shuger et al., 2011 [57] | USA | 2011 | 46.8 | Total: 197 | Determine the effectiveness of continuous self-monitoring and technology feedback (achieved through SWA automation) alone and in combination with GWL (group weight loss) to improve weight loss and reduce waist circumference over a 9-month period in sedentary overweight or obese adults. | Randomized controlled trial |
| Men: 36 | ||||||
| Women: 161 | ||||||
| Pellegrini et al., 2012 [58] | USA | 2012 | 44.2 | Total: 51 | Evaluate the effectiveness of a technology-based system (TECH) in weight loss when used alone or in combination with a 6-month in-person behavioral weight loss intervention in overweight and obese adults. | Randomized trial |
| Men: 7 | ||||||
| Women: 44 | ||||||
| Dunn et al., 2014 [59] | USA | 2014 | 48.96 | Total: 1711 | Compare the effectiveness of online delivery of a weight management program using synchronous (real-time) distance education technology with in-person delivery. | Pre- and post-study |
| Men: 173 | ||||||
| Women: 1538 | ||||||
| Chambliss et al., 2011 [60] | USA | 2011 | 45 | Total: 120 | Develop and evaluate a 12-week weight management intervention that involves computer self-monitoring and technology-assisted feedback with and without an improved behavioral component. | Randomized trial |
| Men: 21 | ||||||
| Women: 99 | ||||||
| Ing et al., 2018 [61] | USA | 2018 | 45.95 | Total: 217 | Compare the effectiveness of a 9-month workplace-based weight loss maintenance intervention delivered on DVD versus face-to-face. | Randomized controlled trial |
| Men: 28 | ||||||
| Women: 189 | ||||||
| Godino et al., 2016 [62] | USA | 2016 | 22.7 | Total: 404 | Evaluate the effectiveness of a 2-year, theory-based weight loss intervention that was delivered remotely and adaptively through user experiences integrated with Facebook, mobile apps, text messages, emails, a website, and technology-mediated communication with a health coach. | Randomized controlled trial |
| Men: 120 | ||||||
| Women: 284 |
| Authors, Year, [Reference] | Intervention | Duration Intervention | Nr. of Groups | Technology | Feedback |
|---|---|---|---|---|---|
| He et al., 2017 [22] | Diet and physical activity | 6 months | 2 (technology group and control group) | Mobile App (WeChat) | Yes |
| Spring et al., 2017 [23] | Diet and physical activity | 12 months | 3 (self-guided, standard and technology) | Mobile App + Accelerometer | Yes |
| Ross & Wing., 2016 [17] | Diet and physical activity | 6 months | 3 (standard, technology and technology + phone) | App (Fibit), Fibit Activity Monitor Zip, Fibit Aria Smart Scale | Yes |
| Apiñaniz et al., 2019 [13] | Diet and physical activity | 6 months | 2 (control group and intervention group) | Mobile App (Aktidiet) | Yes |
| Wharton et al., 2014 [16] | Diet and physical activity | 8 weeks | 3 (control group (paper), “memo” group (mobile notes) and app) | Mobile App (“Lose it”) | Yes |
| Thomas et al., 2019 [24] | Diet and physical activity | 18 months | 3 (control group, “Group” sessions, and “Smart” sessions + App) | App (MyFitnessPal) | Yes |
| Svetkey et al., 2015 [25] | Diet and physical activity | 24 months | 3 (control group, cell phone group (CP) and “personal coaching” group (PC) | CP: App PC: Smartphone (self-monitoring) | Yes |
| Allen et al., 2013 [26] | Diet and physical activity | 6 months | 4 (intensive counseling group (IC), intensive counseling group + smartphone (IC + SP), less intensive counseling group + smartphone (LIC + SP) and smartphone group (SP) | App (Lose It!) | Yes |
| Turner-McGrievy & Tate., 2011 [27] | Diet and physical activity | 6 months | 2 (Podscat group and Podscat+Mobile group) | Podscat and mobile (App FatSecret’s) | Yes |
| Lee et a., 2010 [28] | Diet and physical activity | 6 weeks | 2 (control group and intervention group) | App (SmartDiet) | No |
| Laing et al., 2014 [29] | Diet and physical activity | 6 months | 2 (control group and intervention group) | App (MyFitnessPal) | Yes |
| Napolitano et al., 2013 [11] | Diet and physical activity | 8 weeks | 3 (Facebook group, Facebook plus group, and control group) | App (Facebook) | Yes |
| Stephens et al., 2017 [30] | Diet and physical activity | 3 months | 2 (Smartphone+health coach group and control group) | App (Lose It!) | Yes |
| Martin et al., 2015 [31] | Diet and physical activity | 12 weeks | 2 (technology group and “health education” group) | Mobile app, weight scale and activity measurer | Yes |
| Carter et al., 2013 [32] | Diet and physical activity | 6 months | 2 (intervention group and face-to-face group) | Mobile App (My Meal Mate) Website | Yes |
| Hernández-Reyes et al., 2020 [33] | Diet and physical activity | 6 months | 2 (control group and intervention group) | App + pedometer | Yes |
| Rogers et al., 2016 [34] | Diet and physical activity | 6 months | 3 (standard group, TECH group and EN-TECH) group | Smartphone+physical activity monitor | Yes |
| Alencar et al., 2019 [35] | Diet and physical activity | 12 weeks | 2 (control group and intervention group) | “American Well” App: Video-conference MyFitnessPal App: self-monitoring | Yes |
| Lewis et al., 2019 [36] | Diet, physical activity, stress/mood and sleep- and lifestyle-related habits. | 8 months | 2 (technology and control group) | Phone (calls and text messages) | Yes |
| Steinberg et al., 2013 [37] | Diet and physical activity | 6 months | 2 (intervention group and control group) | Automated system which includes daily text messages. | Yes |
| Shapiro et al., 2012 [38] | Diet and physical activity | 12 months | 2 (control group and intervention group) | Phone (SMS and MMS (multimedia messaging service) | Yes |
| Jakicic et al., 2016 [39] | Diet and physical activity | 24 months | 2 (SWBI group and EWLI group) | Phone sessions, messages, website, PA monitor | Yes |
| Godino et al., 2019 [40] | Diet and physical activity | 12 months | 3 (control group, SMS group, and SMS + coaching group) | SMS | Yes |
| Newton et al., 2018 [41] | Diet and physical activity | 6 months | 2 (control group and intervention group) | SMS | Yes |
| Bouhaidar et al., 2013 [42] | Diet and physical activity | 12 weeks | 2 (control group and intervention group) | SMS | Yes |
| Lin et al., 2014 [43] | Diet and physical activity | 6 months | 2 (control group and intervention group) | Text messages | Yes |
| Haapala et al., 2009 [44] | Diet and physical activity | 12 months | 2 (control group and intervention group) | SMS | Yes |
| Patrick et al., 2009 [45] | Diet and physical activity | 4 months | 2 (comparison group and intervention group) | SMS | Yes |
| Sullivan et al., 2013 [46] | Diet and physical activity | 9 months | 2 (virtual reality group and face-to-face group) | Virtual Reality (Second Life) | Yes |
| Behm-Morawitz et al., 2016 [47] | Diet and physical activity | 4 weeks | 3 (3D group, 2D group, and non-intervention group) | 3D virtual world, 2D website | No |
| Johnston et al., 2012 [15] | Diet and physical activity | 12 weeks | 2 (virtual reality group and face-to-face group) | Virtual reality (Club One Island via Linden Lab’s Second Life) | No |
| Manzoni et al., 2016 [12] | Diet and physical activity | 12 months | 3 groups (SBP group, SBP-CBT group, and SBP + VR-CBT group) | Virtual reality (NeuroVR open source software) | Yes |
| Morgan et al., 2014 [48] | Diet and physical activity | 6 months | 3 (“shed it resources” group, “shed it online”, and control) | Web plus pedometer | Yes |
| Azar et al., 2015 [49] | - | 3 months | 2 (control group and intervention group) | Video conferencing technology via web | Yes |
| Abdi et al., 2015 [50] | Diet and physical activity | 9 months | 3 (control group, web group, phone group) | Website (“Healthy employee), cell phone | Yes |
| Morgan et al., 2011 [51] | Diet and physical activity | 12 months | 2 (internet group and control group) | Web | Yes |
| Burke et al., 2012 [52] | Diet and physical activity | 24 months | 3 (paper diary group, PDA group, and PDA + Feedback group) | PDA | Yes |
| Wang et al., 2012 [53] | Diet and physical activity | 12 months | 3 (paper diary group, PDA group, and PDA + Feedback group) | PDA | Yes |
| Chung et al., 2014 [54] | Diet | 12 weeks | 3 (“food diary” group, “electronic diary” group, and control group) | Electronic diary | Yes |
| Spring et al., 2013 [55] | Diet and physical activity | 12 months | 2 (standard group and +mobile group) | PDA | Yes |
| Unick et al., 2012 [56] | Physical activity and diet changes | 6 months | 2 (SBWL group and SBWL + Technology group | Sensewear bracelet | Yes |
| Shuger et al., 2011 [57] | Diet and physical activity | 9 months | 4 (standard group, GWL group, SWA group, and GWL+SWA group) | SenseWear Armband | Yes |
| Pellegrini et al., 2012 [58] | Diet and physical activity | 6 months | 3 (SBWL group, SBWL+TECH group, and TECH group) | Monitoring armband | Yes |
| Dunn et al., 2014 [59] | Diet and physical activity | 15 weeks | 2 (online group and in-person group) | Online teaching software (Elluminate Live!) | Yes |
| Chambliss et al., 2011 [60] | Diet and physical activity | 12 weeks | 3 (basic feedback group, enhanced feedback group, and control group) | Software (BalanceLog) | Yes |
| Ing et al., 2018 [61] | Diet and physical activity | 9 months | 2 (DVD group and face-to-face group) | DVDs | No |
| Godino et al., 2016 [62] | Diet and physical activity | 24 months | 2 (Smart group and control group) | Facebook, App, text messages, emails, a website and technology-mediated communication with a health coach | Yes |
| Authors, Year. [Reference] | Weight Results | Adherence Results |
|---|---|---|
| He et al., 2017 [22] | Weight loss: the control group lost (−1.78 kg) and the intervention group (−2.09 kg). | - |
| Significant weight loss at 6 months for men, but not for women (p < 0.001). | ||
| Men in WeChat group: higher probability of maintaining weight, Weight loss of 1 to 2 kg or Weight loss 1 of more than 2 kg than the control group. | ||
| Spring et al., 2017 [23] | At 12 months, weight loss in standard group (−5.6 kg), in technology group (−3.1 kg), and in self (control) group (−2.7 kg). | Adherence to self-monitoring: larger in App group than in standard (p < 0.001) and it covaried with weight loss (r(84) = 0.36–0.51, p < 0.001). Correlations did not differ depending on the treatment condition. |
| No significant differences between technology group and self-group (control). | ||
| (p-value not specified). | ||
| Ross & Wing RR., 2016 [17] | Weight loss 6 months later: TECH + PHONE group (−6.4 kg), TECH group (−4.1 kg) and ST group (−1.3 kg). | Adherence to self-monitoring: greater in Tech + Phone group than in Tech and standard (p < 0.05), and standard group showed lower adherence. In both technology groups: Significant association between the percentage change in weight and adherence to intake control (r = −0.48, p < 0.001) and weight (r = −0.42, p = 0.002). No association between adherence to the use of the activity monitor and weight change (p = 0.085). |
| Significant group differences (p = 0.042). | ||
| Apiñaniz et al., 2019 [13] | No significant group differences in weight (0.357 kg, p = 0.7). | Increased adherence in App Group for dietary intake and PA recommendations. No significant group differences (dietary intake: p = 0.413 and PA: p = 0.145). |
| Wharton et al., 2014 [16] | Significant weight loss at 8 weeks in groups (app: −3.5 lb; Memo: −6.5 lb, and diary: −4.4 lb). | The App group registered more frequently than the paper group (p = 0.042). |
| No significant group differences (p = 0.19). | ||
| Thomas et al., 2019 [24] | Weight loss | The Smart Group (App) had the highest rate of weight self-control (3.7%) but did not differ significantly from the control group (29.7%). |
| CONTROL: 18M −6.4 kg | ||
| GROUP: 18M −5.9 kg | ||
| SMART: 18M −5.5 kg | ||
| No significant group differences (p > 0.05) | ||
| Svetkey et al., 2015 [25] | Weight loss: App group (−0.99 kg) vs. control group (−1.44 kg). | - |
| No significant differences (p-value not specified) | ||
| Smartphone group (coaching) (−2.45 kg) | ||
| No significant differences between the App group and control. (p-value not specified). | ||
| Allen et al., 2013 [26] | Weight loss 6 months later: intensive counseling (IC) (−2.5 kg); intensive counseling+smartphone (IC + SP) (−5.4 kg); less intensive counseling +smartphone (LIC + SP) (−3.3 kg); smartphone (SP) (−1.8 kg); | Larger in group intensive counseling + smartphone: they attended an average of 72% of the 14 counseling sessions and recorded their diet an average of 53% and PA 32% of the days. Very similar percentages for less intensive counseling group + smartphone and smartphone group. |
| No significant group differences (p = 0.89). | ||
| Turner-McGrievy & Tate., 2011 [27] | Weight loss 6 months later: podcast group (−2.6 kg) vs. podcast + mobile goup(−2.6 kg); Non-significant group differences (p = 0.88) | - |
| Lee et al., 2010 [28] | Changes in weight: Intervention group (−2.2 kg) vs. control group (−0.5 kg). (p < 0.05). | - |
| Laing et al., 2014 [29] | Weight, changes from the start: | - |
| Control: 6M: + 0.27 kg | ||
| Intervention: 6M: −0.03 kg | ||
| Group differences: 6M: −0.30 kg (p = 0.63) | ||
| Napolitano et al., 2013 [11] | Weight: | Neither the fast response time nor the number of text responses were associated with weight loss at week 4 or week 8. |
| Facebook: 8 weeks: −0.63 kg | ||
| Facebook plus: 8 weeks: −2.4 kg | ||
| Control: 8 weeks: −0.24 kg | ||
| Significant group differences (8 weeks) (p < 0.05) | ||
| Stephens et al., 2017 [30] | Weight, Smartphone + HC group: Beginning: 82.8 kg; 3 months: 8.1 kg. Difference: 2.1 kg. | - |
| Control group: Beginning: 75.8 kg; 3 months: 77.3 kg. Difference: +1.5 kg. | ||
| Significant group differences (p = 0.026) | ||
| Martin et al., 2015 [31] | Weight loss 12 weeks: the smartloss group lost (−7.08 kg) and the education group health care lost (−0.6 kg). | - |
| Significant group differences (p = 0.001). | ||
| Carter et al., 2013 [32] | Weight loss 6 months later: the App group lost (−4.6 kg), the diary group lost (−2.9 kg), and the web group lost (−1.3 kg). | Adherence was significantly higher in the App group (92 days) compared to the web group (35 days), and the paper group (29 days). (p < 0.001). |
| No significant differences between App group and paper diary group (p = 0.12) | ||
| Hernández-Reyes et al., 2020 [33] | Weight loss: intervention group lost (−7.9 kg), and the control group lost (−7.1 kg). | - |
| No significant group differences (p > 0.05). | ||
| Rogers et al., 2016 [34] | Weight loss 6 months later: the standard group lost (−6.57 kg), the improved tech group (en-tech) lost (−6.25 kg), and the tech group (−5.18 kg). | The standard group monitored their diet an average of 84.6 days, the technology group 80.0 days, and the enhanced technology group 70.1 days. |
| No significant group differences (p = 0.0997). | ||
| Alencar et al., 2019 [35] | Weight loss: the App group lost (−7.3 kg), and the control group lost (−1.5 kg). | - |
| Significant group differences (p < 0.05). | ||
| Lewis et al., 2019 [36] | Participants who started the intervention achieved significant decreases in: weight (−4.87 kg) at 4 months, maintaining these losses after switching to the control group. | The addition of telephone and texting support to a community obesity management program improved behavioral adherence compared to standard care. |
| In participants who started the control group, no significant changes were observed at 4 months. After the intervention, significant reductions were achieved in: weight (−2.76 kg), at 8 months. | ||
| Significant group differences (p = 0.01) | ||
| Steinberg et al., 2013 [37] | Changes in weight: Control group participants gained an average of 1.14 kg, while intervention group lost an average of 1.27 kg. | Trend towards greater adherence to text messages associated with a higher percentage of weight loss (r = −0.36, p = 0.08), but this did not reach statistical significance. |
| Significant group differences (p = 0.09) | ||
| Shapiro et al., 2012 [38] | Weight loss 12 months later: control group (−2.27 lb) and intervention group (−3.64 lb); control group lost an average of 0.8% of the weight, and the intervention group 1.8%. | Adherence to text messages was moderately strong (60-69%). Participants with higher adherence lost more weight at 6 (p = 0.039) and 12 months (p = 0.023) than those who adhered less. |
| Non-significant group differences (p = 0.394). | ||
| Jakicic et al., 2016 [39] | Weight loss 24 months later: the standard group (SBWI) lost −5.9 kg and the technology group (EWLI) lost −3.2 kg. | - |
| Significant group differences (p = 0.002). | ||
| Godino et al., 2019 [40] | Weight loss 12 months later: control group (−.61%), SMS group (−1.6%), and SMS+Coaching group (−3.63%). | The median of the average daily commitment rate decreased slightly over time: 28.69 at 6 months and 24.91 at 12 months. A unit increase in the average percentage of daily participation throughout the study was associated with a higher percentage of weight loss (−0.08%, p < 0.05). |
| At 12 months, Weight loss the average percentage, adjusted for baseline BMI, was significantly different between SMS + coaching and the control group −3.0, but not between SMS alone and the control group −1.07; (p = 0.291). | ||
| Newton et al., 2018 [41] | Weight loss: intervention group lost (−1.4 kg), and the control group gained (0.2 kg). | The correlation between the number of SMS text messages sent and the change in weight loss was not statistically significant. |
| Significant group difference in the Weight loss (p = 0.03). | ||
| Bouhaidar et al., 2013 [42] | Weight loss: intervention group lost (−5.96 lb) and the control group (−1.41 lb). | At the beginning of the intervention, participants’ response rate to SMS requests was 66%. This percentage decreased to 52% at the end of the intervention. |
| Significant group differences (no p-value is specified). | ||
| Lin et al., 2014 [43] | Weight changes at 6 months: g. intervention lost (−1.6 kg) and control group gained (+0.24 kg), with a group difference of 1.83 kg. Significant group differences (p < 0.0001) | No significant correlation between weight loss at 6 months and total follow-up days (r = 0.14, p = 0.27), nor did it correlate significantly with the average percentage of follow-up days (r = 0.14, p = 0.27). |
| Haapala et al., 2009 [44] | Weight loss at 12 months, the intervention group lost (−4.5 kg), and the control group (−1.1 kg) | The overall frequency of use of the program decreased from 8 times per week to 3–4 times per week in 12 months. Those with more than 5% weight loss at 12 months reported more frequent weekly contact at 3 months than those who had lost less than 5%. |
| Significant group differences (p = 0.006). | ||
| Patrick et al., 2009 [45] | Intervention group: Beginning: 89.79 kg; Month 4: 85.17. Difference: 4.62 kg. | During the first week, participants responded to all messages that requested a response. At week 16, participants responded to approximately two out of every three messages. |
| Comparison group: Beginning: 88.02 kg; Month 4: 87.85 kg. Difference: 0.17 kg). | ||
| Weight loss adjusted comparison group vs. Weight loss adjusted intervention group (−2.88 kg). | ||
| Significant group differences (p = 0.02) | ||
| Sullivan et al., 2013 [46] | Weight loss: the face-to-face group lost (−1.8%), and the virtual reality group (−7.6%). | - |
| Significant group differences (p < 0.05). | ||
| Weight maintenance: virtual reality group (14%) compared to face-to-face group (9.5%). Significant group differences (p < 0.05). | ||
| Behm-Morawitz et al., 2016 [47] | Weight Loss: experimental groups lost (−1.75 lb), and the control group (−0.91 lb). Significant group differences (p = 0.04). | - |
| Johnston et al., 2012 [15] | Weight loss: virtual world group (−3.9 kg) and face-to-face group (−2.8 kg). | - |
| No significant group differences (p = 0.29). | ||
| Manzoni et al., 2016 [12] | Weight loss: the SBP group lost (−6.2%), the CBT group lost (−7.4%) and the virtual reality group lost (−6.25%). | - |
| No significant group differences (p > 0.05) | ||
| The RV group is more likely to maintain or further improve weight loss at the 1-year follow-up than the SBP group (48% vs. 11%; p = 0.004) and than the CBT group (48% vs. 29%; p = 08). | ||
| Morgan et al., 2014 [48] | Weight loss 6 months later: the online group lost (−4.7 kg) and the resources group (pedometer) (−3.7 kg) compared to the control group (−0.5 kg). | The number of objectives established (β = −0.3, 95% CI [−0.6, −0.1], p = 0.01) and the number of documented weight records (β = −0.21, 95% CI [−0.39, −0.02], p = 0.03) were independently associated with weight loss, so each additional goal set and the recorded weight measurement were associated with increased weight loss of 0.32 kg and 0.21 kg, respectively (R2 = 0.37, p < 0.001). |
| Significant differences between the two intervention groups with technology and the control group (p < 0.001) but no significant differences in the intervention groups (p > 0.05). | ||
| Azar et al., 2015 [49] | Weight loss: the intervention group lost (−3.6 kg), and the control group (−0.4 kg). Intervention group lost on average 3.2 kg more than the control group. | While not statistically significant, the downward slope of both the assistance/weight loss and self-monitoring/weight loss curves suggests a weight loss trend with greater participation. |
| Significant group differences (p = 0.0002). | ||
| Abdi et al., 2015 [50] | Weight: | − |
| Web Group: Beginning: 79.44 kg; Month 9: 78.04 kg. Difference: 1.4 kg. | ||
| Phone Group: Beginning: 83.01 kg; Month 9: 82.02 kg. Difference: 0.99 kg. | ||
| Control group: Beginning: 78.63 kg; Month 9: 78.83 kg. Difference: +0.2 kg. | ||
| Significant group differences (p = 0.001). | ||
| Morgan et al., 2011 [51] | Weight loss 12 months later: web group lost (−5.3 kg), and the control group lost (−3.1 kg) | Significant correlation between weight change at 12 months and the number of days of diet entries (weight: r = 0.69, p < 0.001), number of diary entries (weight: r = 0.54, p = 0.004) and number of weekly weight entries (weight: r = 0.56, p = 0.004). |
| No significant group differences (p = 0.408). | ||
| Burke et al., 2012 [52] | Weight loss 24 months later: the PDA+FEEDBACK group lost (−2.17 kg), the paper group lost (−1.77 kg), and the PDA group lost (−1.18 kg). | Significant differences between PDA and PDA + Feedback groups and paper group (p = 0.03). No significant differences between PDA + Feedback groups and PDA group (p = 0.49). A higher proportion of the PDA groups, compared to the paper group was adherent 60% or more of the time (PDA + Feedback vs. paper, p = 0.01) and (PDA vs. paper, p = 0.03). 18 months: 19−20% of PDA groups remained adherent 30% or more of the time, compared to 8% of the paper group. |
| No significant group differences (p = 0.33). | ||
| Wang et al., 2012 [53] | Weight loss 12 months later: paper diary group (−5.19 lb), PDA group (−3.92 lb) and PDA+FB group (−5.30 lb) | Compared to paper register, the PDA to control diet (p = 0.027) and PA (p = 0.014) had significant direct effects on weight loss at 12 months. And a significant indirect effect on results through better adherence to self-monitoring (p < 0.001). |
| No reference to whether there are significant group differences. | ||
| Chung et al., 2014 [54] | Weight loss: | - |
| Control: Beginning: 71.7 kg; SEM.12: 7 kg. Difference (−1.5 kg) | ||
| “Food diary”: Beginning: 71.4 kg; SEM.12: 69.7 kg. Difference (−1.7 kg) | ||
| “Electronic diary”: Beginning: 7 kg; SEM.12: 68.4 kg. Difference (−1.6 kg) | ||
| No significant differences between the intervention groups and the control group (p = 0.159). | ||
| Spring et al., 2013 [55] | Weight loss12 months later: the PDA group lost (−2.9 kg), and the standard group lost (−0.02 kg). | No difference in how often participants in any group attended the MOVE! groups. (Group +mobile: mean of 6.2 meetings vs. Standard Group: mean of 5.9 meetings (p = 0.54). The +mobile participants who attended 80% or more of the treatment sessions lost significantly more weight than the less adherent participants of the +mobile group and, than the adherent or non-adherent participants of the standard group. |
| Significant group differences (no p-values). | ||
| Unick et al., 2012 [56] | Weight loss: standard group + technology (SBWL + tech) lost (−10%), and the standard group (SBWL) lost (−7.8%). | The self-monitoring of food intake was considerably higher in technology compared to standard group (86.2% vs. 71.5%), but did not reach significance (p = 0.098). The technology group wore the bracelet for 91.3% of the days. |
| No significant group differences (p = 0.46). | ||
| Shuger et al., 2011 [57] | Weight loss: | Adherence to wearing the bracelet was greater than 55%, suggesting that weight loss participants may adhere better to self-monitoring protocols that use technology, compared to standard protocols. |
| Standard group: beginning: 102.2 kg; Month 9: 101.32 kg. Difference: 0.88 kg. | ||
| GWL group: beginning: 101.84 kg; Month 9: 99.98 kg. Difference: 1.86 kg. | ||
| SWA group: beginning: 101.15 kg; Month 9: 97.60 kg. Difference: −3.55 kg | ||
| GWL + SWA group: beginning: 10.32 kg; Month 9: 93.73 kg. Difference: −6.59 kg | ||
| Significant group differences (p = 0.0001). Difference: | ||
| Pellegrini et al., 2012 [58] | Weight loss: SBWL group: beginning: 88.6 kg; Month 6: 84.9 kg. Difference: 3.7 kg.SBWL + TECH group: beginning: 102.1 kg; Month 6: 93.3 kg. Difference: 8.8 kg. | SBWL+TECH group self-monitors dietary intake significantly more days (5.9 days/week) than SBWL group (5.3 days/week; p < 0.05) or the TECH group (5.2 days/week; p = 0.001). The self-monitoring of dietary intake was significantly related to weight loss at 6 months when the intervention groups were combined (r = −0.57, p < 0.001) and when analyzed separately for TECH (r = −0.64, p = 0.02). |
| TECH group: beginning: 92.3 kg; Month 6: 86.4 kg. Difference: 5.9 kg | ||
| Significant group differences (p = 0.044) | ||
| Dunn et al., 2014 [59] | Weight loss: | - |
| Online group: Beginning: 197.85 lb; End: 189.81 lb. Difference: 8.04 lb. | ||
| In-person group: Beginning: 197.02 lb; End: 191.07 lb. Difference: 5.95 lb | ||
| Significant differences (p = 0.02) | ||
| Chambliss et al., 2011 [60] | Weight loss: Basic and Improved groups lost (−2.7 kg and −2.5 kg, respectively) and the Control group (−0.3 kg) | - |
| Significant differences (p < 0.05). | ||
| Ing et al., 2018 [61] | Weight Loss: the DVD group lost (−0.48 kg) and face-to-face group (−0.07 kg). | - |
| Non-significant differences (p = 0.46). | ||
| Weight Maintenance: 64.5% in the DVD group and 52.4% in the face-to-face group. | ||
| No significant differences (p = 0.58). | ||
| Godino et al., 2016 [62] | No significant differences in weight between groups (−0.79 kg, p = 0.204). | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rumbo-Rodríguez, L.; Sánchez-SanSegundo, M.; Ruiz-Robledillo, N.; Albaladejo-Blázquez, N.; Ferrer-Cascales, R.; Zaragoza-Martí, A. Use of Technology-Based Interventions in the Treatment of Patients with Overweight and Obesity: A Systematic Review. Nutrients 2020, 12, 3634. https://doi.org/10.3390/nu12123634
Rumbo-Rodríguez L, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Ferrer-Cascales R, Zaragoza-Martí A. Use of Technology-Based Interventions in the Treatment of Patients with Overweight and Obesity: A Systematic Review. Nutrients. 2020; 12(12):3634. https://doi.org/10.3390/nu12123634
Chicago/Turabian StyleRumbo-Rodríguez, Lorena, Miriam Sánchez-SanSegundo, Nicolás Ruiz-Robledillo, Natalia Albaladejo-Blázquez, Rosario Ferrer-Cascales, and Ana Zaragoza-Martí. 2020. "Use of Technology-Based Interventions in the Treatment of Patients with Overweight and Obesity: A Systematic Review" Nutrients 12, no. 12: 3634. https://doi.org/10.3390/nu12123634
APA StyleRumbo-Rodríguez, L., Sánchez-SanSegundo, M., Ruiz-Robledillo, N., Albaladejo-Blázquez, N., Ferrer-Cascales, R., & Zaragoza-Martí, A. (2020). Use of Technology-Based Interventions in the Treatment of Patients with Overweight and Obesity: A Systematic Review. Nutrients, 12(12), 3634. https://doi.org/10.3390/nu12123634







