Associations between Digital Health Intervention Engagement and Dietary Intake: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.2.1. Types of Studies
2.2.2. Types of Participants
2.2.3. Exposure (Independent Variable)
2.2.4. Outcome (Dependent Variable)
2.3. Exclusion Criteria
- Case studies, letters to the editor and non-empirical studies.
- Those which purposely sampled or recruited individuals on the basis of pre-existing health-related conditions, including chronic health conditions such as chronic pain, a chronic disease diagnosis, communicable disease or mental illness given our interest in generalizing the findings to general community samples.
- Those which targeted children (<18 years of age) through children’s use of a DHI.
- Those that used, in full or part, a non-DHI component (e.g., those with both face-to-face and digital intervention components). Studies that included a non-DHI component were excluded due to the difficulty in determining the effect between non-DHI and the DHI-exclusive intervention components on participant engagement.
- Studies that only reported qualitative assessments of engagement (e.g., focus groups).
- Studies that reported engagement with text messaging interventions with no other online component, e.g., CD-ROM and computer-based interventions not functioning in an online capacity;
- As this review was only focused on dietary intake, studies that targeted multiple health behaviors for prevention of chronic disease (e.g., sleep and diet, or diet and physical activity) were excluded to reduce the risk of other health behaviors confounding the association between engagement and dietary intake;
- Studies in which the full text was not available (e.g., where authors were unable to access full text online and/or after contact with the corresponding author).
2.4. Data Collection and Analysis
2.4.1. Selection of Studies
2.4.2. Data Extraction and Management
- Study characteristics, including authors’ names, publication year, overall study design, participant characteristics, study eligibility, and sample size.
- Characteristics of the intervention, including type of DHI, length of exposure to the DHI, location of the DHI, target users of the DHI, and a description of the DHI including complexity and additional intervention strategies used.
- Outcomes, including a description of the association, measures of dietary and engagement outcome and their validity; study design; analysis method used (including adjustments for confounds); magnitude of the association (odds ratio [OR] or regression coefficient or estimate; 95% confidence intervals [CI] or standard deviation [SD] or standard error [SE] and; p-values), the direction and favorability of effect; and information allowing quality assessment.
2.4.3. Critical Appraisal
2.4.4. Data Synthesis and Analysis
- If a study had multiple associations using the same engagement measure and same dietary outcome, preference was given to the dietary outcome assessed using the instrument judged by the authors (in the absence of published reliability or validity data) to be most comprehensive. For example, if a study reported two associations including i) ‘time on website’ using an ‘all day’ fruit-and-vegetable screener and ii) ‘time on website’ using a ‘single-item’ fruit-and-vegetable screener, preference was given to the ‘all day screener’ as it is the more comprehensive outcome measure for fruit-and-vegetable intake.
- If multiple models were presented assessing the association between the same dietary outcome and same engagement measure (e.g., unadjusted and adjusted) we gave preference to the adjusted model.
- If multiple engagement measures were used and they all assessed the same type of engagement outcome (e.g., time on site) we selected the most complete and inclusive. For example, ‘total time on website’ was given preference to ‘time on a specific website feature’.
3. Results
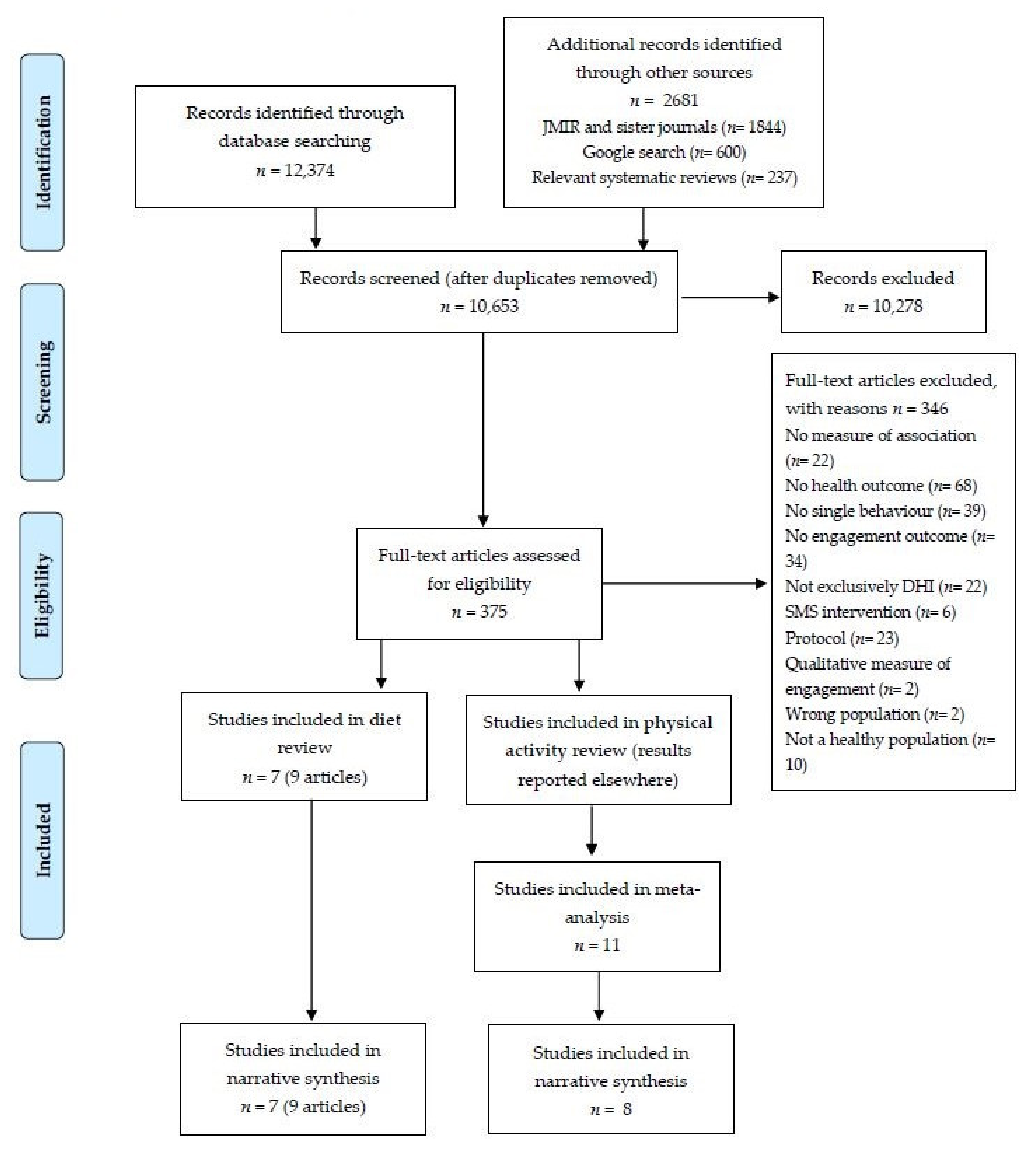
3.1. Search Results
3.2. Methodological Quality of Studies
3.3. Primary Outcomes
3.3.1. Usage
Logins
Time on Site
Composite Usage Measures
Activities Completed
3.3.2. Subjective Experience
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Australian Bureau Of Statistics. Australian Health Survey: Consumption of Food Groups from the Australian Dietary Guidelines; Australian Bureau of Statistics: Canberra, Australia, 2016. [Google Scholar]
- Bates, B.; Lennox, A.; Prentice, A. National Diet and Nutrition Survey: Results from Years 1–4 (Combined) of the Rolling Programme (2008/2009–2011/12): Executive Summary; Public Health England: London, UK, 2014. [Google Scholar]
- Usual Dietary Intakes: Food Intakes, U.S. Population 2007-2010; Epidemiology and Genomics Research Program Website; National Cancer Institute: Bethesda, MD, USA, 2019.
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. 2004. Available online: http://www.who.int/dietphysicalactivity/goals/en/index.html (accessed on 8 December 2013).
- World Health Organization. Digital Health. 2019. Available online: https://www.who.int/behealthy/digital-health (accessed on 10 April 2019).
- World Health Organization. Monitoring and Evaluating Digital Health Interventions: A Practical Guide to Conducting Research and Assessment; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Donkin, L.; Christensen, H.; Naismith, S.; Neal, B.; Hickie, I.B.; Glozier, N. A Systematic Review of the Impact of Adherence on the Effectiveness of e-Therapies. J. Med. Internet Res. 2011, 13, e52. [Google Scholar] [CrossRef] [PubMed]
- International Telecommunications Union. Statistics. 2018. Available online: https://www.itu.int/en/ITU-D/Statistics/Pages/stat/default.aspx (accessed on 20 August 2019).
- Bastawrous, A.; Armstrong, M. Mobile health use in low- and high-income countries: An overview of the peer-reviewed literature. J. R. Soc. Med. 2013, 106, 130–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoeppe, S.; Alley, S.; Van Lippevelde, W.; Bray, N.A.; Williams, S.L.; Duncan, M.J.; Vandelanotte, C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohl, L.F.M.; Crutzen, R.; De Vries, N.K. Online Prevention Aimed at Lifestyle Behaviors: A Systematic Review of Reviews. J. Med. Internet Res. 2013, 15, e146. [Google Scholar] [CrossRef] [Green Version]
- Grady, A.; Yoong, S.L.; Sutherland, R.; Lee, H.; Nathan, N.; Wolfenden, L. Improving the public health impact of eHealth and mHealth interventions. Aust. N. Z. J. Public Health 2018, 42, 118–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cole-Lewis, H.; Ezeanochie, N.; Turgiss, J. Understanding Health Behavior Technology Engagement: Pathway to Measuring Digital Behavior Change Interventions. JMIR Form. Res. 2019, 3, e14052. [Google Scholar] [CrossRef] [PubMed]
- Perski, O.; Blandford, A.; West, R.; Michie, S. Conceptualising engagement with digital behaviour change interventions: A systematic review using principles from critical interpretive synthesis. Transl. Behav. Med. 2017, 7, 254–267. [Google Scholar] [CrossRef] [Green Version]
- Pham, Q.; Graham, G.; Carrion, C.; Morita, P.P.; Seto, E.; Stinson, J.N.; A Cafazzo, J. A Library of Analytic Indicators to Evaluate Effective Engagement with Consumer mHealth Apps for Chronic Conditions: Scoping Review. JMIR mHealth uHealth 2019, 7, e11941. [Google Scholar] [CrossRef]
- Alexander, G.L.; McClure, J.B.; Calvi, J.H.; Divine, G.W.; Stopponi, M.A.; Rolnick, S.J.; Heimendinger, J.; Tolsma, D.; Resnicow, K.; Campbell, M.K.; et al. A Randomized Clinical Trial Evaluating Online Interventions to Improve Fruit and Vegetable Consumption. Am. J. Public Health 2010, 100, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Young, C.; Campolonghi, S.; Ponsonby, S.; Dawson, S.L.; O’Neil, A.; Kay-Lambkin, F.; McNaughton, S.; Berk, M.; Jacka, F.N. Supporting Engagement, Adherence, and Behavior Change in Online Dietary Interventions. J. Nutr. Educ. Behav. 2019, 51, 719–739. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid.-Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Mclaughlin, M.; Delaney, T.; Hall, A.; Byaruhanga, J.; Mackie, P.; Grady, A.; Reilly, K.; Campbell, E.; Sutherland, R.; Wiggers, J.; et al. Associations between digital health intervention engagement and physical activity and sedentary behaviour: A Systematic Review and Meta-Analysis. J. Med. Internet Res. 2021, 23, e23180. [Google Scholar] [CrossRef] [PubMed]
- Dobbins, M.; Husson, H.; DeCorby, K.; LaRocca, R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013, 2013, CD007651. [Google Scholar] [CrossRef] [PubMed]
- Wolfenden, L.; Nathan, N.K.; Sutherland, R.; Yoong, S.L.; Hodder, R.K.; Wyse, R.J.; Delaney, T.; Grady, A.; Fielding, A.; Tzelepis, F.; et al. Strategies for enhancing the implementation of school-based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst. Rev. 2017, 11, CD011677. [Google Scholar] [CrossRef] [PubMed]
- AlKhaldi, G.; Hamilton, F.L.; Lau, R.; Webster, R.; Michie, S.; Murray, E.; Karnes, S.; Keller, C.; Vigano, N.; Crutzen, R. The Effectiveness of Prompts to Promote Engagement With Digital Interventions: A Systematic Review. J. Med. Internet Res. 2016, 18, e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milward, J.; Drummond, C.; Fincham-Campbell, S.; DeLuca, P. What makes online substance-use interventions engaging? A systematic review and narrative synthesis. Digit. Health 2018, 4. [Google Scholar] [CrossRef] [PubMed]
- Bangor, A.; Kortum, P.; Miller, J. The system usability scale (SUS): An empirical evaluation. Int. J. Hum.-Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Perski, O.; Blandford, A.; Garnett, C.; Crane, D.; West, R.; Michie, S. A self-report measure of engagement with digital behavior change interventions (DBCIs): Development and psychometric evaluation of the “DBCI Engagement Scale”. Transl. Behav. Med. 2020, 10, 267–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, H.L.; Cairns, P.; Hall, M. A practical approach to measuring user engagement with the refined user engagement scale (UES) and new UES short form. Int. J. Hum.-Comput. Stud. 2018, 112, 28–39. [Google Scholar] [CrossRef]
- Lefebvre, R.C.; Tada, Y.; Hilfiker, S.W.; Baur, C. The Assessment of User Engagement with eHealth Content: The eHealth Engagement Scale1. J. Comput. Commun. 2010, 15, 666–681. [Google Scholar] [CrossRef]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and Promoting Effective Engagement With Digital Behavior Change Interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Livingstone, K.M.; Celis-Morales, C.; Navas-Carretero, S.; San-Cristobal, R.; Macready, A.L.; Fallaize, R.; Forster, H.; Woolhead, C.; O’Donovan, C.B.; Marsaux, C.F.; et al. Effect of an Internet-based, personalized nutrition randomized trial on dietary changes associated with the Mediterranean diet: The Food4Me Study. Am. J. Clin. Nutr. 2016, 104, 288–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfenden, L.; Goldman, S.; Stacey, F.G.; Grady, A.; Kingsland, M.; Williams, C.M.; Wiggers, J.; Milat, A.; Rissel, C.; Bauman, A.; et al. Strategies to improve the implementation of workplace-based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity. Cochrane Database Syst. Rev. 2018, 11, CD012439. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. Newcastle-Ottawa Quality Assessment Scale Cohort Studies; University of Ottawa: Ottawa, ON, Canada, 2014. [Google Scholar]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G.; ESH Working Group on CV Risk in Low Resource Settings. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef] [Green Version]
- Campbell, M.; E McKenzie, J.; Sowden, A.; Katikireddi, S.; Brennan, S.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [Green Version]
- Buller, D.B.; Woodall, W.G.; Zimmerman, D.E.; Slater, M.D.; Heimendinger, J.; Waters, E.; Hines, J.M.; Starling, R.; Hau, B.; Burris-Woodall, P.; et al. Randomized Trial on the 5 a Day, the Rio Grande Way Website, A Web-based Program to Improve Fruit and Vegetable Consumption in Rural Communities. J. Health Commun. 2008, 13, 230–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lippke, S.; Corbet, J.M.; Lange, D.; Parschau, L.; Schwarzer, R. Intervention Engagement Moderates the Dose–Response Relationships in a Dietary Intervention. Dose-Response 2016, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, T.J.; Alsabeeh, N.; Apovian, C.; Murphy, M.C.; Coffman, G.; Cullum-Dugan, D.; Jenkins, M.; Cabral, H. Weight, Blood Pressure, and Dietary Benefits After 12 Months of a Web-based Nutrition Education Program (DASH for Health): Longitudinal Observational Study. J. Med. Internet Res. 2008, 10, e52. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, R.F.; Pernal, W.; Matsumoto, A.; Shiyko, M.; Intille, S.; Franko, D.L. Capitalizing on mobile technology to support healthy eating in ethnic minority college students. J. Am. Coll. Health 2016, 64, 125–132. [Google Scholar] [CrossRef]
- Nour, M.; Chen, J.; Allman-Farinelli, M.; Leung, M.; Fazzino, T. Young Adults’ Engagement With a Self-Monitoring App for Vegetable Intake and the Impact of Social Media and Gamification: Feasibility Study. JMIR Form. Res. 2019, 3, e13324. [Google Scholar] [CrossRef] [PubMed]
- Kothe, E.J.; Mullan, B.A. Factors affecting acceptability of an email-based intervention to increase fruit and vegetable consumption. BMC Public Health 2014, 14, 1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Couper, M.P.; Alexander, G.L.; Zhang, N.; Little, R.J.A.; Maddy, N.; Nowak, M.A.; McClure, J.B.; Calvi, J.J.; Rolnick, S.J.; Stopponi, M.A.; et al. Engagement and Retention: Measuring Breadth and Depth of Participant Use of an Online Intervention. J. Med. Internet Res. 2010, 12, e52. [Google Scholar] [CrossRef] [PubMed]
- Woodall, W.G.; Buller, D.B.; Saba, L.; Zimmerman, N.; Waters, E.; Hines, J.M.; Cutter, G.R.; Starling, R.; Campbell, M.; Kirk, S. Effect of Emailed Messages on Return Use of a Nutrition Education Website and Subsequent Changes in Dietary Behavior. J. Med. Internet Res. 2007, 9, e27. [Google Scholar] [CrossRef] [PubMed]
- Yoong, S.L.; Grady, A.; Wiggers, J.H.; Stacey, F.G.; Rissel, C.; Flood, V.; Finch, M.; Wyse, R.; Sutherland, R.; Salajan, D.; et al. Child-level evaluation of a web-based intervention to improve dietary guideline implementation in childcare centers: A cluster-randomized controlled trial. Am. J. Clin. Nutr. 2020, 111, 854–863. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Smith, A.D.; Chadwick, P.; Croker, H.; Llewellyn, C.H. Exclusively Digital Health Interventions Targeting Diet, Physical Activity, and Weight Gain in Pregnant Women: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2020, 8, e18255. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Ortiz, L.; Recio-Rodríguez, J.I.; Agudo-Conde, C.; Patino-Alonso, M.C.; Maderuelo-Fernandez, J.-A.; Gento, I.R.; Puig, E.P.; González-Viejo, N.; Arietaleanizbeaskoa, M.S.; Schmolling-Guinovart, Y.; et al. Long-Term Effectiveness of a Smartphone App for Improving Healthy Lifestyles in General Population in Primary Care: Randomized Controlled Trial (Evident II Study). JMIR mHealth uHealth 2018, 6, e107. [Google Scholar] [CrossRef] [Green Version]
| Author and Study Characteristics | Description of Digital Health Intervention | Engagement Outcome/s | Dietary Outcome/s | Association (b) | Direction of Association (c) | Favorable (d) |
|---|---|---|---|---|---|---|
| Author: Alexander 2010; (also reported by Couper 2010) Design (a): cohort N = 2513 (baseline) Age: 46.3 (SD 10.8) Female = 69% | Type: Website Description: Three-arm website intervention, all arms included access to a basic website with varying levels of tailoring. Arm 1 was the basic site, Arm 2 was a tailored website, Arm 3 was a tailored website with motivational interviewing via email. Web sessions were delivered at 1, 3, 13, and 15 weeks. Participants received $2 incentive prior to entering study & $20 for completing study Intervention target: Adults (21–65 years) with no existing health conditions who were registered in a health care system database Total duration of DHI: 12 months * | Logins dichotomized into high (>14 logins); medium (7–13 logins); and low (<7 logins) groups | Change in mean servings of fruit and vegetables from baseline to 12 months using a 16-item valid FFQ | low (mean change 2.1); medium (mean change 2.5); high (mean change 3.1) p < 0.001 | + | √ |
| Breadth-the sum of four measures, standardized by dividing by their standard deviation. including: total session accesses, unique session access, total special feature accesses, total time online in minutes | Change in mean servings of fruit and vegetables from baseline to 12 months usinga 16-item valid FFQ | Coefficients not presented; p < 0.001 | + | √ | ||
| Change in mean servings of fruit and vegetables from baseline to 12 months usinga 2-item valid FFQ | Coefficients not presented; p < 0.001 | + | √ | |||
| Depth-sum of average total special features sessions; standardized minutes spent online subtracted by twice total number (standardized) of unique sessions | Change in mean servings of fruit and vegetables from baseline to 12 months using a 16-item valid FFQ | Coefficients not presented; p = 0.83 | 0 | N/A | ||
| Change in mean servings of fruit and vegetables from baseline to 12 months using a 2-item valid FFQ | Coefficients not presented; p = 0.92 | 0 | N/A | |||
| Author: Buller 2008; (also reported by Woodall 2007) Design (a): cohort N = 380 (baseline) Age (c): <29 years = 35% Female = 88% | Type: Website Description: Fruit and vegetable nutrition education website (password protected), participants were contacted by research team to log onto website once each month, every 2 months participants received ‘small gift’ as a reminder to visit website, routine email notifications were sent announcing new content. Intervention target: Adults (>18 years old), English speaking and living in Southwestern USA for at least 6 months. Total duration of DHI: 4 months | Time on website (mean minutes) | Change in mean servings of fruit-and-vegetable intake from baseline to 4 months using valid all day screener (ranked pre- and post-test) | Unadjusted: R = 0.14, p = 0.004 | + | √ |
| Adjusted: Estimate = 0.74, SD = 0.19, t(df = 414) = 3.87, p = 0.001 | + | √ | ||||
| Time on website (mean minutes) | Change in mean servings of fruit-and-vegetable intake from baseline to 4 months using single item screener (ranked pre- and post-test) | OR (95% CI) 1.010 (1.003, 1.018) per minute of use | + | √ | ||
| Time on website features (mean minutes) | Change in mean servings of fruit-and-vegetable intake from baseline to 4 months using valid all day screener (ranked pre- and post-test) | 17 associations Range of means (SD): 0.009 (0.096) to 13.745 (21.203) Range of Spearman correlation: −0.076 to 0.185 Range of p value: 0.0064 to 0.9189 (only 3 significant) | N/A (e) | N/A | ||
| Number of logins within 5 days of an email | Change in mean servings of fruit-and-vegetable intake from baseline to 4 months using valid FFQ | coefficient = 0.14, p = 0.049 | + | √ | ||
| Proportion of logins after email | Change in mean servings of fruit-and-vegetable intake from baseline to 4 months using valid FFQ | coefficient = 0.11, p = 0.12 | 0 | N/A | ||
| Author: Kothe 2014 Design (a): cohort N = 217 (baseline) Age: 18.92 (SD 1.37) Female = 77.3% | Type: Email intervention Description: Email intervention with two levels of message frequency. Participants in high frequency intervention arm received emails daily (27 emails in total) and those in low frequency arm received emails every 3 days (9 emails in total). Course credit was provided for participating students Intervention target: Adults (>18 years) who were an undergraduate psychology student at an Australian University Total duration of DHI: 30 days | Subjective experience using Likert scale: Interest | Change in fruit-and-vegetable intake scores (servings/day) from baseline to 30 days using self-report e.g., “How many servings of fruit did you eat yesterday?” | Correlation = 0.163, p < 0.05 | + | √ |
| - Credibility | Correlation = 0.002, p = ‘not significant’ | 0 | N/A | |||
| - Logical | Correlation = −0.034, p = ‘not significant’ | 0 | N/A | |||
| - Easy to understand | Correlation = 0.021, p = ‘not significant’ | 0 | N/A | |||
| - Relevant | Correlation = 0.102, p = ‘not significant’ | 0 | N/A | |||
| - Useful | Correlation = 0.149, p < 0.05 | + | √ | |||
| - Complete | Correlation = 0.146, p < 0.05 | + | √ | |||
| - Too long | Correlation = −0.032, p = ‘not significant’ | 0 | N/A | |||
| - Annoying | Correlation = −0.104, p = ‘not significant’ | 0 | N/A | |||
| - Too many emails | Correlation = −0.078, p = ‘not significant’ | 0 | N/A | |||
| - Confusing | Correlation = 0.067, p = ‘not significant’ | 0 | N/A | |||
| Author: Lippke 2016 Design of association(a): cohort N = 701 (at association) Age: 38.71 Female = 84% | Type: Website Description: One-off action-planning and coping-planning website aimed to improve fruit-and-vegetable intake. As an incentive for study participation, individuals were able to take part in an optional raffle in which they could win attractive gift certificates for an online bookstore Intervention target: Adults Total duration of DHI: 1 month | Engagement survey score using Likert scale | Change in fruit-and-vegetable intake scores from baseline to one month (servings/day) using valid ‘open answer’ questionnaire e.g., “how many servings of (a) fruit…and (b) vegetables…do you eat on average per day?” | Correlation = 0.01, p = ‘not significant’,non-linear relationship observed | 0 | N/A |
| Author: Moore 2008 Design (a): cohort N = 181 (at association) Age: not reported Female = 59% # | Type: Website Description: Password-protected website on healthy eating, content was posted each Friday with weekly reminder emails sent to participants. Dietary advice was based on the DASH diet (Dietary Approaches to Stop Hypertension). Intervention target: Adult employees of a US based infrastructure company Total duration of DHI: 12 months | Number of logins | Change in fruit servings from baseline to 12 months using valid FFQ | p = 0.03 | + | √ |
| Change in vegetable servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Change in grains servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Change in dairy servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Change in meat & fish servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Change in nut & beans servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Change in added fats servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Change in sweets servings from baseline to 12 months using valid FFQ | p = ‘not significant’ | 0 | N/A | |||
| Author: Nour 2019 Design (a): Cross-sectional N = 97 (baseline) Age: 24.8 (SD 3.4) Female = 60% | Type Standard App OR gamified app +/- Facebook Description: Standard app of goal setting and self-monitoring with feedback on vegetable intake, Gamified app included rewards as incentivization. Facebook included cooking videos addressing known barriers shared by a dietician daily. Intervention target: Adults 18–30 years, who owned a smartphone and lived in New South Wales, Australia Total duration of DHI: 4 weeks | Total days of app engagement via recorded logins in standard app | Change in vegetable intake (servings/ day) from baseline to 4 weeks using valid short questionnaires | r = 1; n = 23; p < 0.00001 | + | √ |
| Total days of app engagement via recorded logins in gamified app | r = 0.64; n = 24; p = 0.001 | + | √ | |||
| Frequency of recording vegetable intake via app analytics in standard app | r = 0.49; n = 23; p = 0.02 | + | √ | |||
| Frequency of recording vegetable intake via app analytics in gamified app | r = 0.35; n = 24; p = 0.09 | 0 | N/A | |||
| Author: Rodgers 2016 Design (a): cohort N = 46 (baseline) Age: 18.96 (SD 0.76) Female = 100% | Type: Website + SMS Description: Participants were encouraged to take photos of meals using their mobile phone and upload them to a website (Photobucket) and received 3 x motivational text messages/day at mealtimes to encourage healthy eating. Intervention target: Full time female undergraduate college students (>18 years) Total duration of DHI: 3 weeks | Number of photos posted (logins) | Vegetable intake (servings/day) using a valid 2-item FFQ | Estimate = 0.012, SE = 0.008, p = ‘not significant’ | 0 | N/A |
| Fruit intake (servings/day) using a valid 2-item FFQ | Estimate = 0.017, SE = 0.008, p < 0.05 | + | √ | |||
| Log of calories from sugar-sweetened beverages using a ‘beverage intake questionnaire’ | Estimate = 0.007, SE = 0.009, p = ‘not significant’ | 0 | N/A |
| Selection | Comparability | Outcome | Quality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Representativeness of the Exposed Cohort | Selection of Non-Exposed Cohort | Ascertainment of Exposure | Outcome of Interest | Cohort Statistical Analysis | Assessment of Outcome | Length of Follow Up | Adequacy of Follow Up | |
| Alexander (2010) & Couper (2010) | ★ | ★ | ★ | ★ | - | - | ★ | ★ | Good |
| Buller (2008) & Woodall (2007) | ★ | ★ | ★ | - | ★ | - | ★ | - | Poor |
| Kothe (2014) | - | ★ | - | ★ | - | - | ★ | - | Poor |
| Lippke (2016) | ★ | ★ | - | ★ | ★ | - | - | - | Poor |
| Moore (2008) | ★ | ★ | ★ | ★ | - | - | ★ | - | Poor |
| Rodgers (2016) | ★ | ★ | ★ | ★ | ★ | - | - | - | Poor |
| Selection | Comparability | Outcome | Quality | |||||
|---|---|---|---|---|---|---|---|---|
| Study | Representativeness of the Sample | Sample Size | Non Respondent | Ascertainment of Exposure | Statistical Analysis Design Features | Assessment of Outcome | Statistical Test | |
| Nour (2019) | ★ | - | - | ★ | ★ ★ | ★ | ★ | Fair |
| Study | Diet Measure | Engagement Measure (a) | Analysis | Association | Direction (b) | Favorable (c) |
|---|---|---|---|---|---|---|
| Alexander 2010 & Couper 2010 [17,42] | fruit and vegetables | logins | Kruskal—Wallis test | p < 0.001 | + | √ |
| fruit and vegetables | composite usage measure | ordinary least squares regression | 2 associations: adjusted model p < 0.001; adjusted model p = 0.83 | 0 | N/A | |
| Buller 2008 & Woodall 2007 [36,43] | fruit and vegetables | time on website | unclear | adjusted model estimate = 0.74, SD = 0.19 p = 0.001 | + | √ |
| fruit and vegetables | logins | non-parametric spearman partial correlation | 2 associations: coefficient = 0.14, p = 0.049; coefficient = 0.11, p = 0.12 | 0 | N/A | |
| Kothe 2014 [41] | fruit and vegetables | subjective experience | Pearson correlation | 11 associations: Pearson correlation (range) = 0.002 to 0.163 p value (range) = ‘not significant’ to p < 0.05 | 0 | N/A |
| Lippke 2016 [37] | fruit and vegetables | subjective experience | Pearson correlation | Pearson correlation = 0.01, p = ‘not significant’ | 0 | N/A |
| Moore 2008 [38] | fruit | logins | unclear | p = 0.03 | + | √ |
| vegetables | logins | unclear | p = ‘not significant’ | 0 | N/A | |
| other food groups | logins | unclear | p = ‘not significant’ | 0 | N/A | |
| Nour 2019 [40] | vegetables | logins | spearman correlation | 2 associations: r = 1; n = 23; p < 0.00001. r = 0.64; n = 24; p = 0.001 | + | √ |
| vegetables | activities completed | spearman correlation | 2 associations: r = 0.49; n = 23; p = 0.02. r = 0.35; n = 24; p = 0.09 | 0 | N/A | |
| Rodgers 2016 [39] | vegetables | logins | mixed effects modelling | estimate = 0.012, SE = 0.008, p = ‘not significant’ | 0 | N/A |
| fruit | logins | mixed effects modelling | estimate = 0.017, SE = 0.008, p < 0.05 | + | √ | |
| calories from sugar-sweetened drinks | logins | mixed effects modelling | estimate = 0.007, SE = 0.009, p = ‘not significant’ | 0 | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delaney, T.; Mclaughlin, M.; Hall, A.; Yoong, S.L.; Brown, A.; O'Brien, K.; Dray, J.; Barnes, C.; Hollis, J.; Wyse, R.; et al. Associations between Digital Health Intervention Engagement and Dietary Intake: A Systematic Review. Nutrients 2021, 13, 3281. https://doi.org/10.3390/nu13093281
Delaney T, Mclaughlin M, Hall A, Yoong SL, Brown A, O'Brien K, Dray J, Barnes C, Hollis J, Wyse R, et al. Associations between Digital Health Intervention Engagement and Dietary Intake: A Systematic Review. Nutrients. 2021; 13(9):3281. https://doi.org/10.3390/nu13093281
Chicago/Turabian StyleDelaney, Tessa, Matthew Mclaughlin, Alix Hall, Sze Lin Yoong, Alison Brown, Kate O'Brien, Julia Dray, Courtney Barnes, Jenna Hollis, Rebecca Wyse, and et al. 2021. "Associations between Digital Health Intervention Engagement and Dietary Intake: A Systematic Review" Nutrients 13, no. 9: 3281. https://doi.org/10.3390/nu13093281
APA StyleDelaney, T., Mclaughlin, M., Hall, A., Yoong, S. L., Brown, A., O'Brien, K., Dray, J., Barnes, C., Hollis, J., Wyse, R., Wiggers, J., Sutherland, R., & Wolfenden, L. (2021). Associations between Digital Health Intervention Engagement and Dietary Intake: A Systematic Review. Nutrients, 13(9), 3281. https://doi.org/10.3390/nu13093281








