Pressure Sensor System for Customized Scoliosis Braces
Abstract
1. Introduction
2. Materials and Methods
2.1. Rationale of Study Design and Methodology
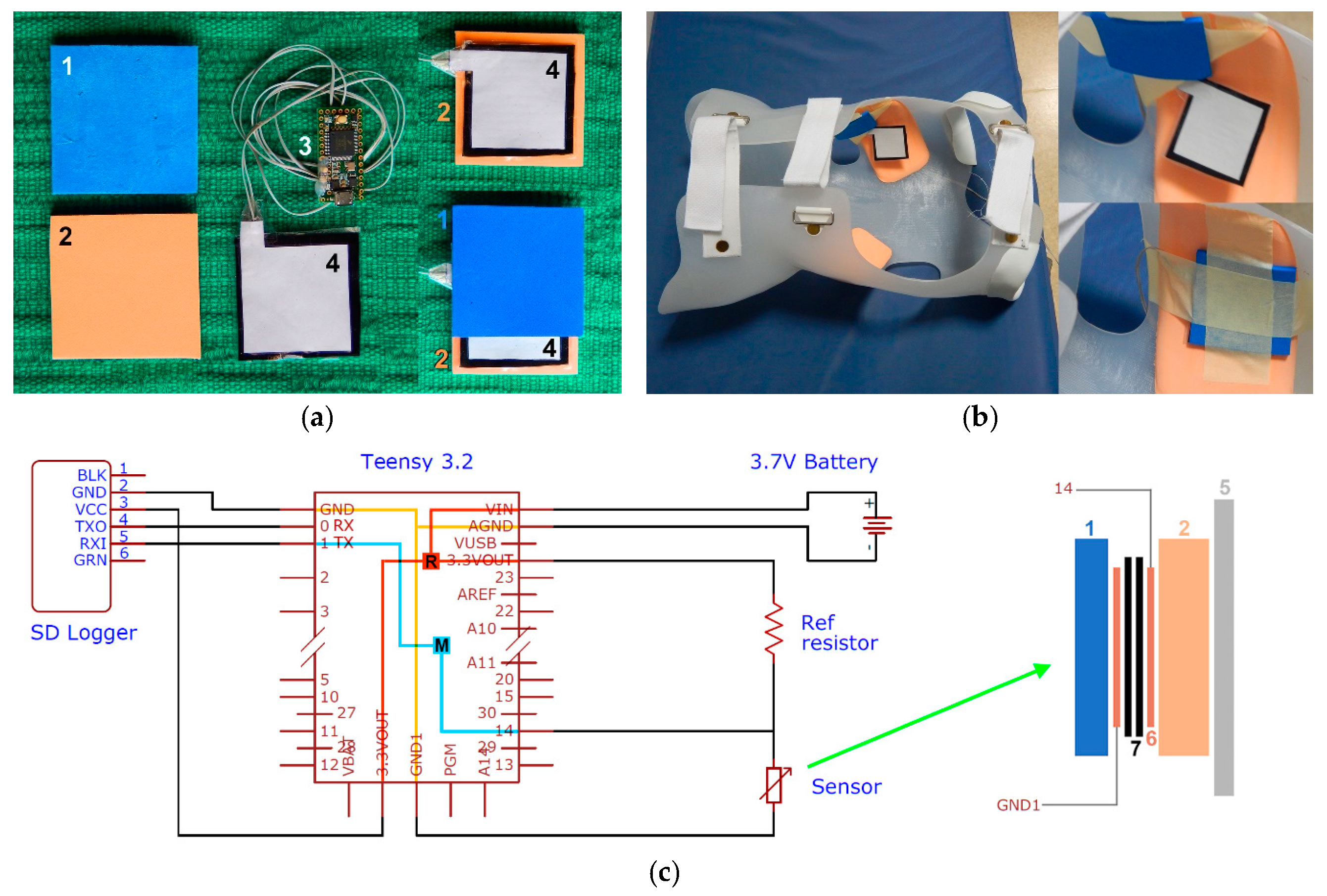
2.2. Sensor Design and Assembly
2.3. Foam Properties
2.4. Sensor Evaluation
- sensor without any foam layer;
- sensor placed on foam A;
- sensor placed on foam B;
- sensor sandwiched between foams A and B (configuration used inside a scoliosis brace).
2.5. Sensor Calibration and Validation
- 1
- It was already known from the sensor evaluation exercise that configuration 4 showed the greatest hysteresis; it was therefore decided to use only peak data to establish the calibration curve.
- 2
- To prevent any method-related influence, it was decided to calibrate and validate the sensor with exactly the same method, using a force plate (Kistler, 9260AA6, Winterthur, Switzerland) as a gold standard. The force readings were converted to pressures because the area applied to the sensor was constant.
- 3
- Sensors used in scoliosis braces do not undergo fast and repetitive high-frequency changes of pressure; the only cyclic pressure change would be the respiration frequency and, other than this, the pressure data would be more static. Accordingly, the sensor was loaded manually on the force plate with impulses ranging between sinusoidal and trapezoidal shapes of intended durations between 2 and 8 s (actually 1.7–8.7 s during the experiments).
2.6. Pressure Measurements
- Test 1:
- the pressure was applied with a leather belt, with the buckle at the 3rd and then at the 4th hole (from the end of the belt);
- Test 2:
- a softer, elastic belt (A300, Polar, Kempele, Finland);
- Test 3:
- increasing the pressure with the elastic belt (A300, Polar, Kempele, Finland);
- Test 4:
- with the leather belt at the 3rd hole.
3. Results
3.1. Foam Properties
3.2. Sensor Evaluation
3.3. Sensor Calibration and Validation
3.4. Pressure Measurements
3.4.1. Sensor Testing
3.4.2. Sensor Application
4. Discussion
4.1. The Calibration Problem and the Sensor Accuracy
- (1)
- using the loading segment only;
- (2)
- using the unloading segment only;
- (3)
- using the average of loading and unloading segments at any specific conductance value;
- (4)
- using both loading and unloading segments and applying them depending on the sign function of the pressure rate (loading if positive pressure rate and vice versa);
- (5)
- using only peak data for calibration.
4.2. Foam Properties Affecting the Conductance of the Sensor
4.3. Brace Pressure Data
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weinstein, S.L.; Dolan, L.A.; Cheng, J.C.Y.; Danielsson, A.; Morcuende, J.A. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef]
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Hitosugi, M.; Shigeta, A.; Takatsu, A. 1. An Autopsy Case of Sudden Death in a Patient with Idiopathic Scoliosis. Med. Sci. Law 2000, 40, 175–178. [Google Scholar] [CrossRef]
- Danielsson, A.J.; Hasserius, R.; Ohlin, A.; Nachemson, A.L. Health-Related Quality of Life in Untreated Versus Brace-Treated Patients with Adolescent Idiopathic Scoliosis. Spine 2010, 35, 199–205. [Google Scholar] [CrossRef]
- Meng, Z.-D.; Li, T.-P.; Xie, X.-H.; Luo, C.; Lian, X.-Y.; Wang, Z.-Y. Quality of life in adolescent patients with idiopathic scoliosis after brace treatment. Medicine 2017, 96, e6828. [Google Scholar] [CrossRef]
- Bernard, J.-C.; Lecante, C.; Deceuninck, J.; Notin, G.; Journoud, L.; Barral, F. The carbon brace. Scoliosis 2013, 8, 3. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.S.; Evans, J.H. Biomechanical evaluation of the Milwaukee brace. Prosthet. Orthot. Int. 1998, 22, 54–67. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van den Hout, J.; Van Rhijn, L.; van den Munckhof, R.; Van Ooy, A. Interface corrective force measurements in Boston brace treatment. Eur. Spine J. 2002, 11, 332–335. [Google Scholar] [CrossRef]
- Pham, V.M.; Houilliez, A.; Schill, A.; Carpentier, A.; Herbaux, B.; Thevenon, A. Study of the pressures applied by a Chêneau brace for correction of adolescent idiopathic scoliosis. Prosthet. Orthot. Int. 2008, 32, 345–355. [Google Scholar] [CrossRef]
- Ahmad, A.; Abu Osman, N.A.; Mokhtar, H.; Mehmood, W.; Kadri, N.A. Analysis of the interface pressure exerted by the Chêneau brace in patients with double-curve adolescent idiopathic scoliosis. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2019, 233, 901–908. [Google Scholar] [CrossRef]
- Belbasis, A.; Fuss, F.K. Development of next-generation smart compression apparel. Proc. Technol. 2015, 20, 85–90. [Google Scholar] [CrossRef]
- Belbasis, A.; Fuss, F.K. Muscle Performance Investigated with a Novel Smart Compression Garment Based on Pressure Sensor Force Myography and Its Validation against EMG. Front. Physiol. 2018, 9, 408. [Google Scholar] [CrossRef] [PubMed]
- Belbasis, A.; Fuss, F.K.; Sidhu, J. Muscle Activity Analysis with a Smart Compression Garment. Procedia Eng. 2015, 112, 163–168. [Google Scholar] [CrossRef]
- Belbasis, A.; Fuss, F.K.; Sidhu, J. Estimation of Cruciate Ligament Forces via Smart Compression Garments. Procedia Eng. 2015, 112, 169–174. [Google Scholar] [CrossRef]
- Ogris, G.; Kreil, M.; Lukowicz, P. Using FSR based muscule activity monitoring to recognize manipulative arm gestures. In Proceedings of the 2007 11th IEEE International Symposium on Wearable Computers, Boston, MA, USA, 11–13 October 2007; pp. 45–48. [Google Scholar]
- Wininger, M. Pressure signature of forearm as predictor of grip force. J. Rehabil. Res. Dev. 2008, 45, 883–892. [Google Scholar] [CrossRef] [PubMed]
- McLaren, J.; Helmer, R.; Horne, S.; Blanchonette, I. Preliminary development of a wearable device for dynamic pressure measurement in garments. Procedia Eng. 2010, 2, 3041–3046. [Google Scholar] [CrossRef]
- Li, N.; Yang, D.; Jiang, L.; Liu, H.; Cai, H. Combined Use of FSR Sensor Array and SVM Classifier for Finger Motion Recognition Based on Pressure Distribution Map. J. Bionic Eng. 2012, 9, 39–47. [Google Scholar] [CrossRef]
- Connan, M.; Ramírez, E.R.; Vodermayer, B.; Castellini, C. Assessment of a Wearable Force- and Electromyography Device and Comparison of the Related Signals for Myocontrol. Front. Neurorobot. 2016, 10, 17. [Google Scholar] [CrossRef]
- Zhou, B.; Sundholm, M.; Cheng, J.; Cruz, H.; Lukowicz, P. Measuring muscle activities during gym exercises with textile pressure mapping sensors. Pervasive Mob. Comput. 2017, 38, 331–345. [Google Scholar] [CrossRef]
- Weizman, Y.; Fuss, F.K. Development of Instrumented Soccer Footwear for Kicking Analysis and Training Purposes. Procedia Eng. 2015, 112, 157–162. [Google Scholar] [CrossRef]
- Fuss, F.K.; Düking, P.; Weizman, Y. Discovery of a Sweet Spot on the Foot with a Smart Wearable Soccer Boot Sensor That Maximizes the Chances of Scoring a Curved Kick in Soccer. Front. Physiol. 2018, 9, 63. [Google Scholar] [CrossRef]
- Tan, A.M.; Fuss, F.K.; Weizman, Y.; Woudstra, Y.; Troynikov, O. Design of Low Cost Smart Insole for Real Time Measurement of Plantar Pressure. Procedia Technol. 2015, 20, 117–122. [Google Scholar] [CrossRef]
- Weizman, Y.; Tan, A.M.; Fuss, F.K. Benchmarking study of the forces and centre of pressure derived from a novel smart-insole against an existing pressure measuring insole and force plate. Measurement 2019, 142, 48–59. [Google Scholar] [CrossRef]
- Fuss, F.K.; Tan, A.M.; Weizman, Y. ‘Electrical viscosity’ of piezoresistive sensors: Novel signal processing method, assessment of manufacturing quality, and proposal of an industrial standard. Biosens. Bioelectron. 2019, 141, 111408. [Google Scholar] [CrossRef] [PubMed]
- Fuss, F.K.; Fundel, S.; Weizman, Y.; Smith, R.M. Smart Oar Blade for Hydrodynamic Analysis of Rowing. Procedia Eng. 2016, 147, 735–740. [Google Scholar] [CrossRef][Green Version]
- Moeyersons, B.; Fuss, F.K.; Tan, A.M.; Weizman, Y. Biofeedback System for Novice Snowboarding. Procedia Eng. 2016, 147, 781–786. [Google Scholar] [CrossRef][Green Version]
- Hopkins, M.; Vaidyanathan, R.; McGregor, A. Examination of the Performance Characteristics of Velostat as an In-Socket Pressure Sensor. IEEE Sens. J. 2020, 20, 6992–7000. [Google Scholar] [CrossRef]
- Fuss, F.K. The Design Strain and Dead Mass of Energy Absorbing Materials and Structures: Mathematical Principles and Experimental Determination. Procedia Eng. 2015, 112, 116–121. [Google Scholar] [CrossRef]
- International Organization for Standardization (ISO). ISO 3386-1:1986, Polymeric Materials, Cellular Flexible—Determination of Stress-Strain Characteristics in Compression—Part 1: Low-Density Materials. 2018. Available online: https://www.iso.org/standard/8683.html (accessed on 7 January 2021).
- ASTM (American Society for Testing and Materials). ASTM D3574 C Foam Force Deflection Testing. 2020. Available online: https://www.admet.com/testing-applications/testing-standards/astm-d3574-c-foam-force-deflection-testing/ (accessed on 7 January 2021).









| Properties | Average Data of Foam B (Pink) | Average Data of Foam A (Blue) | Ratio (B/A) | Comments |
|---|---|---|---|---|
| maximum W/σ (-) | 0.2948 | 0.3066 | 0.9615 | same |
| ε (-) at maximum W/σ | 0.5496 | 0.5596 | 0.9822 | same |
| maximum E (MPa) at linear elastic segment | 7.1613 | 3.6154 | 1.9808 | B = twice as stiff |
| minimum E (MPa) at the collapse plateau | 0.3655 | 0.1457 | 2.5082 | B = 2.5 times as stiff |
| thickness (mm) | 6.15 | 3.17 | 1.9400 | B = twice as thick |
| maximum F (N) | 5000 | 2500 | 2 | depends on test conditions, FB = 2 FA |
| maximum σ (MPa) at maximum F | 2.0382 | 1.0407 | 1.9585 | depends on test conditions |
| maximum W (kJ/m3) at maximum F | 443.457 | 245.416 | 1.8070 | depends on test conditions |
| maximum ε (-) at maximum F | 0.7411 | 0.7571 | 0.9789 | same; depends on test conditions and on stiffness (foam B is approximately twice as stiff as foam A) |
| Strain rate (s−1) | 0.032 | 0.032 | 1 | =test condition |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuss, F.K.; Ahmad, A.; Tan, A.M.; Razman, R.; Weizman, Y. Pressure Sensor System for Customized Scoliosis Braces. Sensors 2021, 21, 1153. https://doi.org/10.3390/s21041153
Fuss FK, Ahmad A, Tan AM, Razman R, Weizman Y. Pressure Sensor System for Customized Scoliosis Braces. Sensors. 2021; 21(4):1153. https://doi.org/10.3390/s21041153
Chicago/Turabian StyleFuss, Franz Konstantin, Asliza Ahmad, Adin Ming Tan, Rizal Razman, and Yehuda Weizman. 2021. "Pressure Sensor System for Customized Scoliosis Braces" Sensors 21, no. 4: 1153. https://doi.org/10.3390/s21041153
APA StyleFuss, F. K., Ahmad, A., Tan, A. M., Razman, R., & Weizman, Y. (2021). Pressure Sensor System for Customized Scoliosis Braces. Sensors, 21(4), 1153. https://doi.org/10.3390/s21041153








