Assessing Upper Limb Function in Breast Cancer Survivors Using Wearable Sensors and Machine Learning in a Free-Living Environment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Test Protocol in the Home Environment
2.3. Data Analysis
2.3.1. Video Annotation, i.e., Ground Truth
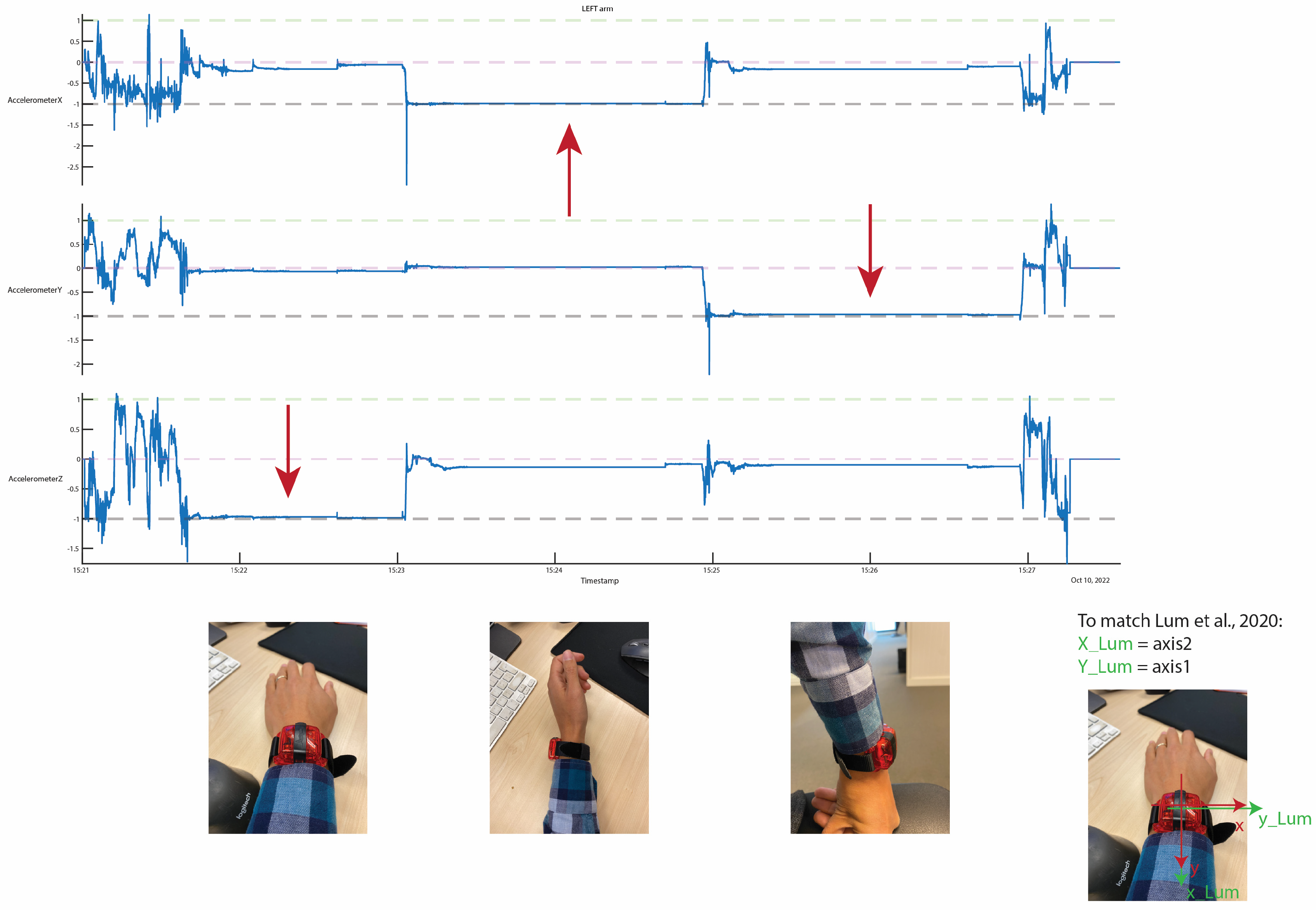
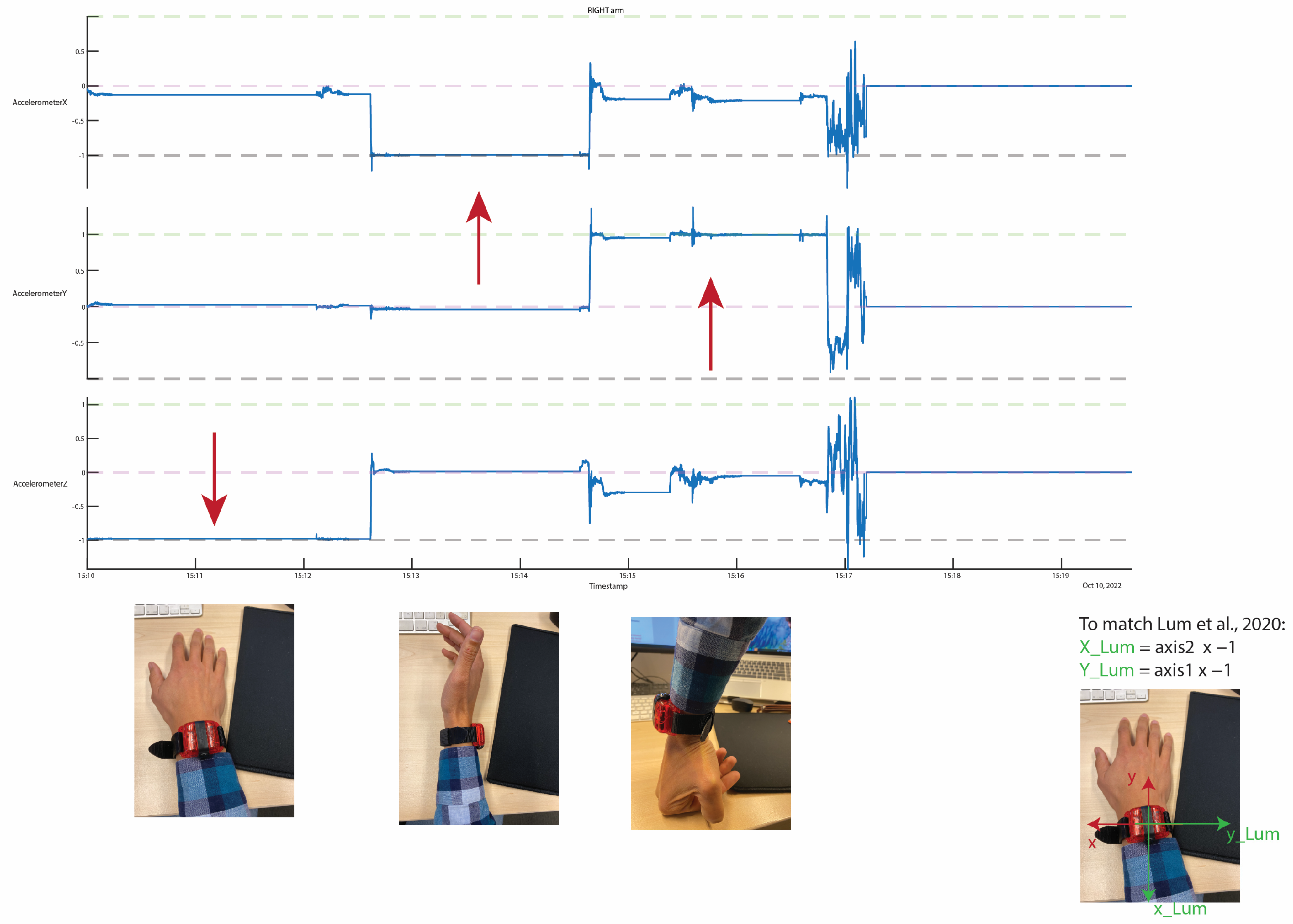
2.3.2. Accelerometer Data Pre-Processing
2.3.3. Counts Threshold Method
2.3.4. Machine Learning Pipeline
2.4. Outcomes
2.5. Statistical Analyses
3. Results
3.1. Demographic Data
3.2. Prediction Accuracy
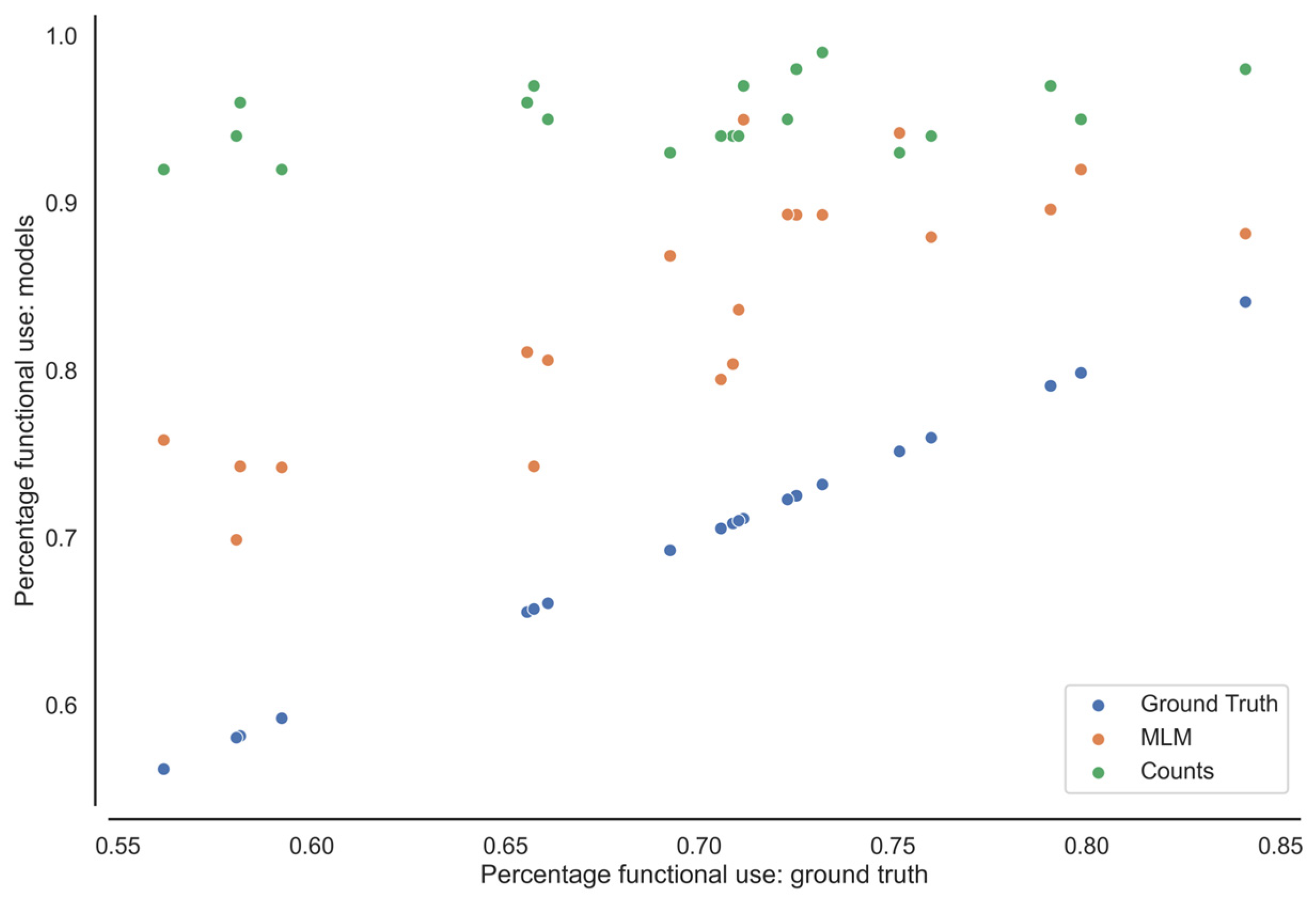
3.3. Minutes Active and Percentage Functional
3.4. Correlation Accuracy and DASH Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beaton, D.E.; Wright, J.G.; Katz, J.N. Development of the Quickdash: Comparison of Three Item-Reduction Approaches. J. Bone Jt. Surg. Am. 2005, 87, 1038–1046. [Google Scholar]
- De Baets, L.; van der Straaten, R.; Matheve, T.; Timmermans, A. Shoulder assessment according to the international classification of functioning by means of inertial sensor technologies: A systematic review. Gait Posture 2017, 57, 278–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Groef, A.; Van der Gucht, L.; Dams, M.; Evenepoel, L.; Teppers, J.; Toppet-Hoegars, L.; De Baets, L. The Association between Upper Limb Function and Variables at the Different Domains of the International Classification of Functioning, Disability and Health in Women after Breast Cancer Surgery: A Systematic Review. Disabil. Rehabil. 2020, 44, 1176–1189. [Google Scholar] [CrossRef] [PubMed]
- Roy, J.-S.; MacDermid, J.C.; Woodhouse, L.J. Measuring shoulder function: A systematic review of four questionnaires. Arthritis Rheum. 2009, 61, 623–632. [Google Scholar] [CrossRef]
- Garner, B.A.; Pandy, M.G. Musculoskeletal Model of the Upper Limb Based on the Visible Human Male Dataset. Comput. Methods Biomech. Biomed. Eng. 2001, 4, 93–126. [Google Scholar] [CrossRef]
- Ong, W.L.; Schouwenburg, M.G.; van Bommel, A.C.M.; Stowell, C.; Allison, K.H.; Benn, K.E.; Browne, J.P.; Cooter, R.D.; Delaney, G.P.; Duhox, F.; et al. A Standard Set of Value-Based Patient-Centered Outcomes for Breast Cancer: The International Consortium for Health Outcomes Measurement (Ichom) Initiative. JAMA Oncol. 2017, 3, 677–685. [Google Scholar] [CrossRef]
- LeBlanc, M.; Stineman, M.; DeMichele, A.; Stricker, C.; Mao, J.J. Validation of QuickDASH Outcome Measure in Breast Cancer Survivors for Upper Extremity Disability. Arch. Phys. Med. Rehabil. 2014, 95, 493–498. [Google Scholar] [CrossRef] [Green Version]
- Fisher, M.I.; Davies, C.C.; Uhl, T.L. A quantitative comparison of arm activity between survivors of breast cancer and healthy controls: Use of accelerometry. Support. Care Cancer 2020, 28, 5307–5313. [Google Scholar] [CrossRef]
- Lum, P.S.; Shu, L.; Bochniewicz, E.M.; Tran, T.; Chang, L.-C.; Barth, J.; Dromerick, A.W. Improving Accelerometry-Based Measurement of Functional Use of the Upper Extremity After Stroke: Machine Learning versus Counts Threshold Method. Neurorehabilit. Neural Repair 2020, 34, 1078–1087. [Google Scholar] [CrossRef]
- Uswatte, G.; Hobbs Qadri, L. A behavioral observation system for quantifying arm activity in daily life after stroke. Rehabil. Psychol. 2009, 54, 398–403. [Google Scholar] [CrossRef] [Green Version]
- Uswatte, G.; Miltner, W.H.R.; Foo, B.; Varma, M.; Moran, S.; Taub, E. Objective measurement of functional upper-extremity movement using accelerometer recordings transformed with a threshold filter. Stroke 2000, 31, 662–667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lang, C.E.; Waddell, K.J.; Klaesner, J.W.; Bland, M.D. A Method for Quantifying Upper Limb Performance in Daily Life Using Accelerometers. J. Vis. Exp. 2017, 122, 55673. [Google Scholar]
- Pohl, J.; Ryser, A.; Veerbeek, J.M.; Verheyden, G.; Vogt, J.E.; Luft, A.R.; Easthope, C.A. Classification of functional and non-functional arm use by inertial measurement units in individuals with upper limb impairment after stroke. Front. Physiol. 2022, 13, 952757. [Google Scholar] [CrossRef]
- David, A.; Subash, T.; Varadhan, S.K.M.; Melendez-Calderon, A.; Balasubramanian, S. A Framework for Sensor-Based Assessment of Upper-Limb Functioning in Hemiparesis. Front. Hum. Neurosci. 2021, 15, 667509. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.A.; Kondrashova, O.; Bradley, A.; Williams, E.D.; Pearson, J.V.; Waddell, N. Deep Learning in Cancer Diagnosis, Prognosis and Treatment Selection. Genome Med. 2021, 13, 152. [Google Scholar] [CrossRef]
- Schambra, H.M.; Parnandi, A.; Pandit, N.G.; Uddin, J.; Wirtanen, A.; Nilsen, D.M. A Taxonomy of Functional Upper Extremity Motion. Front. Neurol. 2019, 10, 857. [Google Scholar] [CrossRef] [Green Version]
- Neishabouri, A.; Nguyen, J.; Samuelsson, J.; Guthrie, T.; Biggs, M.; Wyatt, J.; Cross, D.; Karas, M.; Migueles, J.H.; Khan, S.; et al. Quantification of acceleration as activity counts in ActiGraph wearable. Sci. Rep. 2022, 12, 11958. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R.; Taylor, J. An Introduction to Statistical Learning, 2nd ed.; Springer: Berlin, Germany, 2021. [Google Scholar]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning: With Applications in R; Springer Texts in Statistics; Springer: New York, NY, USA, 2013. [Google Scholar]
- Lang, A.E.; Card, A.; Barden, J.; Kim, S.Y. Effect of Breast Reconstruction on Kinematics and Performance during Upper Limb–Focused Functional Tasks. Plast. Reconstr. Surg. 2022, 150, 747e–756e. [Google Scholar] [CrossRef]
- Lang, A.E.; Dickerson, C.R.; Kim, S.Y.; Stobart, J.; Milosavljevic, S. Impingement pain affects kinematics of breast cancer survivors in work-related functional tasks. Clin. Biomech. 2019, 70, 223–230. [Google Scholar] [CrossRef]
- De Groef, A.; Van Kampen, M.; Dieltjens, E.; Christiaens, M.-R.; Neven, P.; Geraerts, I.; Devoogdt, N. Effectiveness of Postoperative Physical Therapy for Upper-Limb Impairments After Breast Cancer Treatment: A Systematic Review. Arch. Phys. Med. Rehabil. 2015, 96, 1140–1153. [Google Scholar] [CrossRef]
- Olsson Möller, U.; Beck, I.; Rydén, L.; Malmström, M. A comprehensive approach to rehabilitation interventions following breast cancer treatment—A systematic review of systematic reviews. BMC Cancer 2019, 19, 472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Activities | Description |
|---|---|
| Laundry activity | Participants were instructed to (1) move clothes from a closet or basket into a washer and close the washer, (2) remove the clothes from the washer, put them in the dryer, and close the door, and (3) remove the clothes from the dryer and fold them or hang them back in the closet. |
| Kitchen activity | Participants were instructed to (1) load and unload four or five items from the dishwasher, (2) cut an apple, (3) pick up one item from the floor, and (4) use a broom or a dust mop for home to sweep the floor. |
| Shopping activity | Participants were instructed to (1) gather four or five items out of the supply closet in their grocery store bag or box, (2) place them into the car, step into the car, then step out, and remove the groceries from the car, and (3) put the groceries back in the supply closet. |
| Bed making activity | Participants were instructed to (1) remove the sheets and pillowcases from their bed and (2) replace them. |
| Reality | |||
|---|---|---|---|
| Functional Activity | Non-Functional Activity | ||
| Prediction | Functional activity | True Positive (TP) | False Positive (FP) |
| Non-functional activity | False Negative (FN) | True Negative (TN) | |
| Subj ID | Age (Years/Old) | BMI (kg/cm2) | Operated Side | Surgery | (Neo-)Adjuvant Treatment | QuickDASH Score |
|---|---|---|---|---|---|---|
| P_001 | 44 | 31.87 | R | ME + SN | TAM. | 0 |
| P_002 | 48 | 19.69 | L | ME + SN | Adj. CT +TAM | 9.1 |
| P_003 | 50 | 25.09 | R | BCS + SN | Adj. RT + TAM | 38.6 |
| P_004 | 53 | 29.29 | L | ME + SN | / | 4.5 |
| P_005 | 52 | 26.29 | L | BCS + SN | Adj. RT + TAM | 13.6 |
| P_006 | 45 | 24.6 | L | ME + ALND | Neo-adj. CT +Adj. RT +AI | 11.4 |
| P_007 | 52 | 27.88 | R | ME + ALND | Neo-adj. CT +Adj. RT | 15.9 |
| P_008 | 43 | 23.52 | R | ME + SN | TAM | 0 |
| P_009 | 65 | 28.37 | R | BCS + SN | Adj. RT + AI | 15.9 |
| P_010 | 72 | 19.83 | L | BCS + ALND | Neo-adj. CT +Adj. RT + AI | 11.4 |
| Median [IQR] | 50.5 [43.8–56.0] | 25.7 [22.6–28.6] | 11.4 [3.38–15.9] |
| Left Arm | Right Arm | |||||||
|---|---|---|---|---|---|---|---|---|
| Subj ID | acc | Recall | Spec | f1 | acc | Recall | spec | f1 |
| P_001 | 0.82 | 0.96 | 0.80 | 0.47 | 0.82 | 0.75 | 0.83 | 0.45 |
| P_002 | 0.82 | 1.00 | 0.80 | 0.53 | 0.87 | 0.94 | 0.86 | 0.63 |
| P_003 | 0.90 | 0.89 | 0.90 | 0.30 | 0.89 | 0.30 | 0.93 | 0.25 |
| P_004 | 0.83 | 0.94 | 0.83 | 0.32 | 0.83 | 0.87 | 0.82 | 0.57 |
| P_005 | 0.77 | 1.00 | 0.76 | 0.23 | 0.78 | 0.74 | 0.79 | 0.45 |
| P_006 | 0.80 | 0.85 | 0.80 | 0.31 | 0.88 | 0.82 | 0.89 | 0.55 |
| P_007 | 0.85 | 1.00 | 0.84 | 0.36 | 0.88 | 1.00 | 0.87 | 0.63 |
| P_008 | 0.81 | 1.00 | 0.80 | 0.33 | 0.83 | 0.72 | 0.84 | 0.44 |
| P_009 | 0.88 | 0.95 | 0.88 | 0.55 | 0.86 | 0.75 | 0.86 | 0.47 |
| P_010 | 0.83 | 1.00 | 0.82 | 0.12 | 0.81 | 0.75 | 0.82 | 0.32 |
| avg | 0.83 | 0.96 | 0.82 | 0.35 | 0.85 | 0.77 | 0.85 | 0.47 |
| Left Arm | Right Arm | |||||
|---|---|---|---|---|---|---|
| Subj ID | Ground Truth | MLM | Counts Threshold | Ground Truth | MLM | Counts Threshold |
| Total minutes of functional activity | ||||||
| P_001 | 15.93 | 19.73 | 26.28 | 16.80 | 19.60 | 26.22 |
| P_002 | 12.33 | 15.47 | 16.60 | 13.53 | 15.67 | 16.70 |
| P_003 | 21.87 | 24.27 | 26.88 | 23.27 | 23.93 | 27.13 |
| P_004 | 19.73 | 23.80 | 28.43 | 17.33 | 20.60 | 27.98 |
| P_005 | 12.53 | 16.53 | 17.05 | 12.73 | 15.47 | 16.82 |
| P_006 | 12.20 | 15.13 | 20.27 | 13.80 | 15.27 | 20.50 |
| P_007 | 10.40 | 12.33 | 15.15 | 11.27 | 12.93 | 14.87 |
| P_008 | 16.07 | 20.07 | 19.77 | 17.07 | 19.60 | 20.35 |
| P_009 | 15.40 | 17.47 | 20.33 | 15.33 | 17.27 | 20.32 |
| P_010 | 14.40 | 17.47 | 19.42 | 14.53 | 17.47 | 19.57 |
| Percentage of functionally active | ||||||
| P_001 | 0.56 | 0.69 | 0.92 | 0.59 | 0.69 | 0.92 |
| P_002 | 0.69 | 0.87 | 0.93 | 0.76 | 0.88 | 0.94 |
| P_003 | 0.79 | 0.87 | 0.97 | 0.84 | 0.86 | 0.98 |
| P_004 | 0.66 | 0.80 | 0.95 | 0.58 | 0.69 | 0.94 |
| P_005 | 0.71 | 0.94 | 0.97 | 0.72 | 0.88 | 0.95 |
| P_006 | 0.58 | 0.72 | 0.96 | 0.65 | 0.72 | 0.97 |
| P_007 | 0.66 | 0.78 | 0.96 | 0.71 | 0.82 | 0.94 |
| P_008 | 0.75 | 0.94 | 0.93 | 0.80 | 0.92 | 0.95 |
| P_009 | 0.71 | 0.80 | 0.94 | 0.71 | 0.79 | 0.94 |
| P_010 | 0.73 | 0.88 | 0.98 | 0.73 | 0.88 | 0.99 |
| Mean difference [SD] | 0.14 [0.04] | 0.27 [0.07] | 0.10 [0.04] | 0.24 [0.07] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vets, N.; De Groef, A.; Verbeelen, K.; Devoogdt, N.; Smeets, A.; Van Assche, D.; De Baets, L.; Emmerzaal, J. Assessing Upper Limb Function in Breast Cancer Survivors Using Wearable Sensors and Machine Learning in a Free-Living Environment. Sensors 2023, 23, 6100. https://doi.org/10.3390/s23136100
Vets N, De Groef A, Verbeelen K, Devoogdt N, Smeets A, Van Assche D, De Baets L, Emmerzaal J. Assessing Upper Limb Function in Breast Cancer Survivors Using Wearable Sensors and Machine Learning in a Free-Living Environment. Sensors. 2023; 23(13):6100. https://doi.org/10.3390/s23136100
Chicago/Turabian StyleVets, Nieke, An De Groef, Kaat Verbeelen, Nele Devoogdt, Ann Smeets, Dieter Van Assche, Liesbet De Baets, and Jill Emmerzaal. 2023. "Assessing Upper Limb Function in Breast Cancer Survivors Using Wearable Sensors and Machine Learning in a Free-Living Environment" Sensors 23, no. 13: 6100. https://doi.org/10.3390/s23136100
APA StyleVets, N., De Groef, A., Verbeelen, K., Devoogdt, N., Smeets, A., Van Assche, D., De Baets, L., & Emmerzaal, J. (2023). Assessing Upper Limb Function in Breast Cancer Survivors Using Wearable Sensors and Machine Learning in a Free-Living Environment. Sensors, 23(13), 6100. https://doi.org/10.3390/s23136100









