Non-EPI Vaccine Hesitancy among Chinese Adults: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measures
2.2. Statistical Analysis
2.3. Factors Affecting Vaccine Hesitancy
3. Results
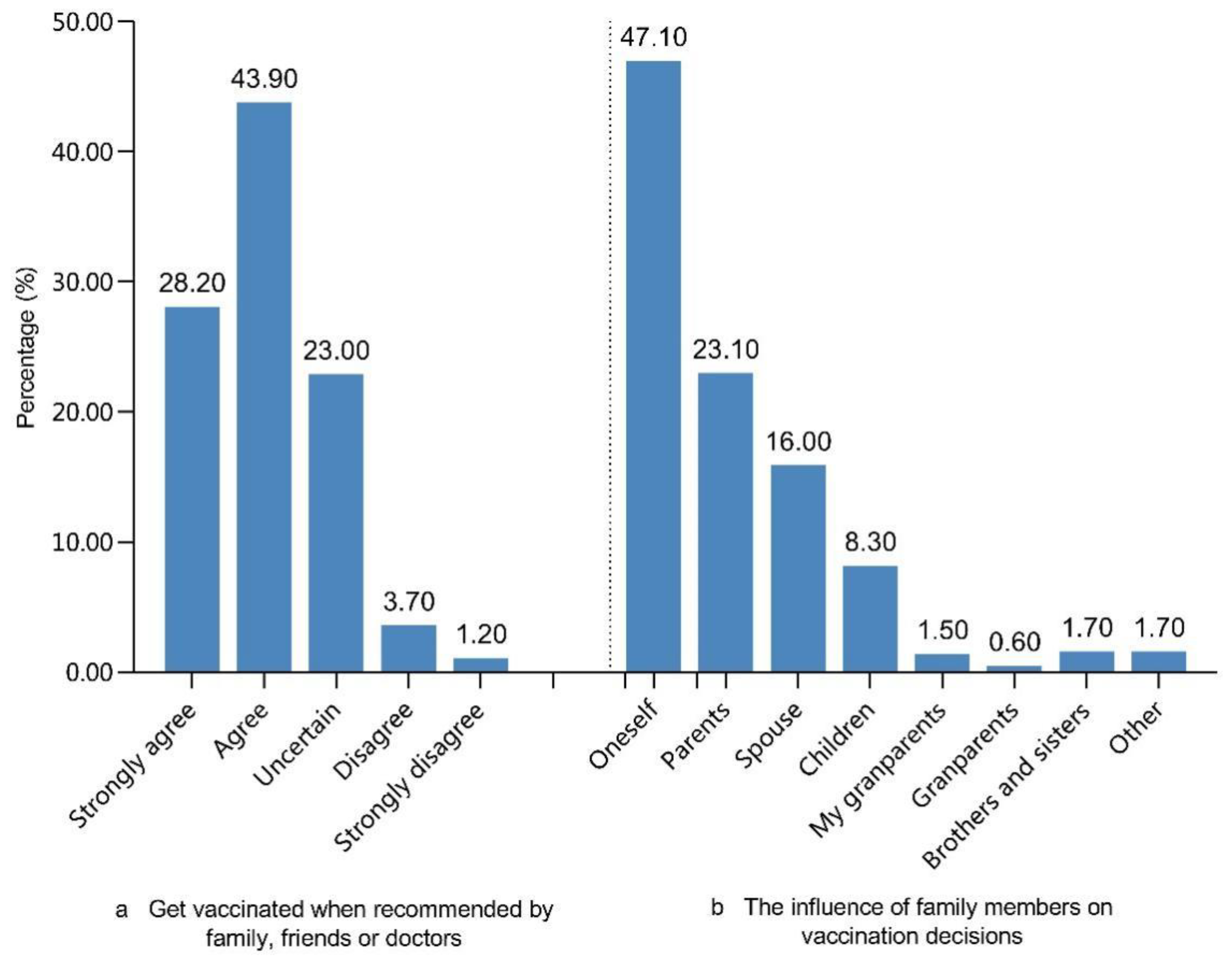
3.1. Non-EPI Vaccine Willingness among Adults
3.2. Willingness to Take the COVID-19 Vaccine among Adults
3.3. Factors Associated with Vaccine Hesitancy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Wilson, R.; Hanley, S.; Parys, A.; Paterson, P. Tracking the global spread of vaccine sentiments: The global response to Japan’s suspension of its HPV vaccine recommendation. Hum. Vaccines Immunother. 2014, 10, 2543–2550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jama, A.; Lindstrand, A.; Ali, M.; Butler, R.; Kulane, A. Nurses’ Perceptions Of MMR Vaccine Hesitancy In An Area With Low Vaccination Coverage. Pediatr. Health Med. Ther. 2019, 10, 177–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, L.P.; Wong, P.F.; AbuBakar, S. Vaccine hesitancy and the resurgence of vaccine preventable diseases: The way forward for Malaysia, a Southeast Asian country. Hum. Vaccines Immunother. 2020, 16, 1511–1520. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Wang, H.; Ma, Y.; Wang, Z.; Zhang, Z.; Li, T.; Yang, Z. Changes in parents’ decisions pertaining to vaccination of their children after the Changchun Changsheng vaccine scandal in Guangzhou, China. Vaccine 2020, 38, 6751–6756. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Liu, X.-J.; Mesch, G.S. The Adoption of Preventive Behaviors during the COVID-19 Pandemic in China and Israel. Int. J. Environ. Res. Public Health 2020, 17, 7170. [Google Scholar] [CrossRef] [PubMed]
- Haq, K.; McElhaney, J.E. Immunosenescence: Influenza vaccination and the elderly. Curr. Opin. Immunol. 2014, 29, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Krueger, P.; Amant, O.S.; Loeb, M. Predictors of pneumococcal vaccination among older adults with pneumonia: Findings from the Community Acquired Pneumonia Impact Study. BMC Geriatr. 2010, 10, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, W.; Wu, Q.; Yang, J.; Dong, K.; Chen, X.; Bai, X.; Chen, X.; Chen, Z.; Viboud, C.; Ajelli, M.; et al. Global, regional, and national estimates of target population sizes for covid-19 vaccination: Descriptive study. BMJ 2020, 371, m4704. [Google Scholar] [CrossRef] [PubMed]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of US adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 vaccination intention in the UK: Results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Wang, J.; Lu, X.; Lai, X.; Lyu, Y.; Zhang, H.; Fenghuang, Y.; Jing, R.; Li, L.; Yu, W.; Fang, H. The Changing Acceptance of COVID-19 Vaccination in Different Epidemic Phases in China: A Longitudinal Study. Vaccines 2021, 9, 191. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 11, 1–15. [Google Scholar] [CrossRef]
- Wyatt, J. When to Use Web-Based Surveys. J. Am. Med Inform. Assoc. 2000, 7, 426–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eysenbach, G. Improving the quality of web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e132. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.J.; Choi, W.S.; Seong, H.; Choi, J.Y.; Kim, J.-H.; Kim, Y.-J.; Cho, E.Y.; Park, H.; Lee, H.; Kim, N.J.; et al. Developing a Framework for Pandemic COVID-19 Vaccine Allocation: A Modified Delphi Consensus Study in Korea. J. Korean Med. Sci. 2021, 36, e166. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Han, B.; Zhao, T.; Liu, H.; Liu, B.; Chen, L.; Xie, M.; Liu, J.; Zheng, H.; Zhang, S.; et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: A national cross-sectional study. Vaccine 2021, 39, 2833–2842. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Chandra, R.; Mathur, M.; Samdariya, S.; Kapoor, N. Vaccine hesitancy: Understanding better to address better. Isr. J. Health Policy Res. 2016, 5, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogart, L.M.; Ojikutu, B.O.; Tyagi, K.; Klein, D.J.; Mutchler, M.G.; Dong, L.; Lawrence, S.J.; Thomas, D.R.; Kellman, S. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. JAIDS J. Acquir. Immune Defic. Syndr. 2021, 86, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Horne, Z.; Powell, D.; Hummel, J.E.; Holyoak, K. Countering antivaccination attitudes. Proc. Natl. Acad. Sci. USA 2015, 112, 10321–10324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miton, H.; Mercier, H. Cognitive Obstacles to Pro-Vaccination Beliefs. Trends Cogn. Sci. 2015, 19, 633–636. [Google Scholar] [CrossRef] [PubMed]
- Zizzo, J. The Missing Link in the Covid-19 Vaccine Race. Hum. Vaccines Immunother. 2021, 17, 1326–1328. [Google Scholar] [CrossRef] [PubMed]
- Carter, S. Humanitarian Programme Recommendations for COVID-19 Based on Social Sciences Evidence from the DRC Ebola Outbreak Response, CELLULE D’ANALYSE EN SCIENCES SOCIALES|CASS. 2020. Available online: https://reliefweb.int/report/world/social-science-support-covid-19-lessons-learned-brief-3-humanitarian-programme.
- Opel, D.J.; Diekema, D.S.; Lee, N.R.; Marcuse, E.K. Social Marketing as a Strategy to Increase Immunization Rates. Arch. Pediatr. Adolesc. Med. 2009, 163, 432–437. [Google Scholar] [CrossRef] [Green Version]
- Lin, L.; Sun, R.; Yao, T.; Zhou, X.; Harbarth, S. Factors influencing inappropriate use of antibiotics in outpatient and community settings in China: A mixed-methods systematic review. BMJ Glob. Health 2020, 5, e003599. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Srivastav, A.; Razzaghi, H.; Williams, W.; Lindley, M.C.; Jorgensen, C.; Abad, N.; Singleton, J.A. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinating Among Groups Prioritized for Early Vaccination—United States, September and December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 217–222. [Google Scholar] [CrossRef]
- Bogart, L.M.; Dong, L.; Gandhi, P.; Ryan, S.; Smith, T.L.; Klein, D.J.; Fuller, L.A.; Ojikutu, B.O. What Contributes to COVID-19 Vaccine Hesitancy in Black Communities, and How Can It Be Addressed? RAND Corp. 2021. [Google Scholar] [CrossRef]
- Wilson, R.; Zaytseva, A.; Bocquier, A.; Nokri, A.; Fressard, L.; Chamboredon, P.; Carbonaro, C.; Bernardi, S.; Dubé, E.; Verger, P. Vaccine hesitancy and self-vaccination behaviors among nurses in southeastern France. Vaccine 2020, 38, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, G.; Di Giovanni, P.; Di Girolamo, A.; Scampoli, P.; Cedrone, F.; D’Addezio, M.; Meo, F.; Romano, F.; Di Sciascio, M.B.; Staniscia, T. Knowledge and Attitude towards Vaccination among Healthcare Workers: A Multicenter Cross-Sectional Study in a Southern Italian Region. Vaccines 2020, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Iten, A.; Bonfillon, C.; Bouvard, T.; Siegrist, C.-A.; Pittet, D. P037: Nosocomial influenza prevention using multi-modal intervention strategies; 20-years of experience. Antimicrob. Resist. Infect. Control. 2013, 2, P37. [Google Scholar] [CrossRef] [Green Version]
- Riphagen-Dalhuisen, J.; Burgerhof, J.G.; Frijstein, G.; van der Geest-Blankert, A.D.; Danhof-Pont, M.B.; de Jager, H.J.; Bos, A.A.; Smeets, E.E.; de Vries, M.J.; Gallee, P.M.; et al. Hospital-Based cluster randomised controlled trial to assess effects of a multi-faceted programme on influenza vaccine coverage among hospital healthcare workers and nosocomial influenza in the Netherlands, 2009 to 2011. Eurosurveillance 2013, 18, 20512. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Lin, D.; Operario, D. Interest in COVID-19 vaccine trials participation among young adults in China: Willingness, reasons for hesitancy, and demographic and psychosocial determinants. Prev. Med. Rep. 2021, 22, 101350. [Google Scholar] [CrossRef] [PubMed]
- Rashid, H.; Yin, J.K.; Ward, K.; King, C.; Seale, H.; Booy, R. Assessing Interventions To Improve Influenza Vaccine Uptake Among Health Care Workers. Health Aff. 2016, 35, 284–292. [Google Scholar] [CrossRef]
- Bish, A.; Michie, S. Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. Br. J. Health Psychol. 2010, 15, 797–824. [Google Scholar] [CrossRef] [Green Version]
- Bish, A.; Yardley, L.; Nicoll, A.; Michie, S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine 2011, 29, 6472–6484. [Google Scholar] [CrossRef]




| Variable Meaning | Assignment |
|---|---|
| Q1. Generally, I think the vaccine is safe Q2. Generally, I think the vaccine is effective Q3. I think vaccines are very important for my health Q4. Generally, I think the whole chain (whole process, from production to vaccination) management of vaccine is safe and effective Q6. Please evaluate your trust in the vaccination information provided by the government Q8. In my opinion, immunity from natural diseases is better than vaccination Q9. Because of the low risk of disease, there is no need for vaccination Q10. Even if I have a disease, I can resist it, so I don’t need a vaccine Q12. Generally, it’s very convenient and time-consuming for me to get vaccinated Q13. Generally, I was able to get the vaccine I wanted Q14. Generally, I can afford the vaccine | 1 = very agree; 2 = agree; 3 = uncertain; 4 = disagree; 5 = very disagree |
| Vaccination hesitancy | 1 = very hesitant; 2 = hesitant; 3 = uncertain; 4 = not hesitant; 5 = very not hesitant |
| Demographic Characteristics | Number | Proportion (%) | Non-EPI Vaccine Hesitancy | COVID-19 Vaccine Hesitancy | ||||
|---|---|---|---|---|---|---|---|---|
| Yes Frequency (%) | No Frequency (%) | p Value | Yes Frequency (%) | No Frequency (%) | p Value | |||
| Age, years | ||||||||
| 18~25 | 2409 | 32.90 | 1771 (73.5) | 638 (26.5) | <0.001 | 600 (24.9) | 1809 (75.1) | <0.001 |
| 26~35 | 2784 | 38.00 | 1814 (65.2) | 970 (34.8) | 615 (22.1) | 2169 (77.9) | ||
| 36~45 | 1264 | 17.30 | 811 (64.2) | 453 (35.8) | 320 (25.3) | 944 (74.7) | ||
| ≥46 | 861 | 11.80 | 549 (63.8) | 312 (36.2) | 272 (31.6) | 589 (68.4) | ||
| Gender | ||||||||
| Male | 3565 | 48.70 | 2382 (66.8) | 1183 (33.2) | 0.178 | 741 (20.8) | 2824 (79.2) | <0.001 |
| Female | 3753 | 51.30 | 2563 (68.3) | 1190 (31.7) | 1066 (28.4) | 2687 (71.6) | ||
| Nationality | ||||||||
| Han | 6979 | 95.40 | 4714 (67.5) | 2265 (32.5) | 0.819 | 1719 (24.6) | 5260 (75.4) | 0.580 |
| Non-Han | 339 | 4.60 | 231 (68.1) | 108 (31.9) | 88 (26.0) | 251 (74.0) | ||
| Place of residence | ||||||||
| East | 4292 | 58.60 | 2938 (68.5) | 1354 (31.5) | 0.160 | 1160 (27.0) | 3132 (73.0) | <0.001 |
| Central | 1559 | 21.30 | 1034 (66.3) | 525 (33.7) | 277 (17.8) | 1282 (82.2) | ||
| West | 1467 | 20.00 | 973 (66.3) | 494 (33.7) | 370 (25.2) | 1097 (74.8) | ||
| Education level | ||||||||
| ≤Junior high school | 436 | 6.00 | 310 (71.1) | 126 (28.9) | 0.041 | 103 (23.6) | 333 (76.4) | <0.001 |
| High school or equivalent | 1193 | 16.30 | 786 (65.9) | 407 (34.1) | 246 (20.6) | 947 (79.4) | ||
| College or equivalent | 4692 | 64.10 | 3147 (67.1) | 1545 (32.9) | 1148 (24.5) | 3544 (75.5) | ||
| ≥Master’s degree | 997 | 13.60 | 702 (70.4) | 295 (29.6) | 310 (31.1) | 687 (68.9) | ||
| Occupation | ||||||||
| Government agencies and institutions | ||||||||
| 1681 | 23.00 | 1088 (64.7) | 593 (35.3) | <0.001 | 415 (24.7) | 1266 (75.3) | <0.001 | |
| Enterprise/business/service industry | ||||||||
| 2616 | 35.70 | 1724 (65.9) | 892 (34.1) | 561 (21.4) | 2055 (78.6) | |||
| Agricultural/forestry/animal husbandry/fishery/water conservancy production personnel | ||||||||
| 765 | 10.50 | 526 (68.8) | 239 (31.2) | 125 (16.3) | 640 (83.7) | |||
| Soldier | 123 | 1.70 | 60 (48.8) | 63 (51.2) | 13 (10.6) | 110 (89.4) | ||
| Full-time student | 1326 | 18.10 | 981 (74.0) | 345 (26.0) | 402 (30.3) | 924 (69.7) | ||
| Other | 807 | 11.00 | 566 (70.1) | 241 (29.9) | 291 (36.1) | 516 (63.9) | ||
| Healthcare occupation | ||||||||
| Yes | 2386 | 32.60 | 1666 (69.8) | 720 (30.2) | 0.004 | 402 (16.8) | 1984 (83.2) | <0.001 |
| No | 4932 | 67.40 | 3279 (66.5) | 1653 (33.5) | 1405 (28.5) | 3527 (71.5) | ||
| Annual family income (RMB 10,000) | ||||||||
| <5 | 1481 | 20.20 | 1045 (70.6) | 436 (29.4) | 0.005 | 333 (22.5) | 1148 (77.5) | <0.001 |
| 5–10 | 2524 | 34.50 | 1656 (65.6) | 868 (34.4) | 587 (23.3) | 1937 (76.7) | ||
| 11–15 | 1738 | 23.70 | 1157 (66.6) | 581 (33.4) | 359 (20.7) | 1379 (79.3) | ||
| ≥16 | 1575 | 21.50 | 1087 (69.0) | 488 (31.0) | 528 (33.5) | 1047 (66.5) | ||
| Number of people in residence | ||||||||
| 1 | 477 | 6.50 | 329 (69.0) | 148 (31.0) | 0.364 | 121 (25.4) | 356 (74.6) | 0.752 |
| 2–5 | 6466 | 88.40 | 4374 (67.6) | 2092 (32.4) | 1599 (24.7) | 4867 (75.3) | ||
| ≥6 | 375 | 5.10 | 242 (64.5) | 133 (35.5) | 87 (23.2) | 288 (76.8) | ||
| Number of contacts per day | ||||||||
| 1–10 | 4684 | 64.00 | 3176 (67.8) | 1508 (32.2) | 0.002 | 1224 (26.1) | 3460 (73.9) | 0.001 |
| 11–20 | 1824 | 24.90 | 1264 (69.3) | 560 (30.7) | 400 (21.9) | 1424 (78.1) | ||
| ≥21 | 810 | 11.10 | 505 (62.3) | 305 (37.7) | 183 (22.6) | 627 (77.4) | ||
| Self-reported health | ||||||||
| Very good | 3508 | 47.90 | 2275 (64.9) | 1233 (35.1) | <0.001 | 614 (17.5) | 2894 (82.5) | <0.001 |
| Good | 2813 | 38.40 | 1929 (68.6) | 884 (31.4) | 848 (30.1) | 1965 (69.9) | ||
| Common | 921 | 12.60 | 688 (74.7) | 233 (25.3) | 320 (34.7) | 601 (65.3) | ||
| Bad | 56 | 0.80 | 43 (76.8) | 13 (23.2) | 20 (35.7) | 36 (64.3) | ||
| Very bad | 20 | 0.30 | 10 (50.0) | 10 (50.0) | 5 (25.0) | 15 (75.0) | ||
| Have you ever been obtained the influenza vaccination? | ||||||||
| Yes | 2293 | 31.30 | 1398 (61.0) | 895 (39.0) | <0.001 | 223 (9.7) | 2070 (90.3) | <0.001 |
| No | 5025 | 68.70 | 3547 (70.6) | 1478 (29.4) | 1584 (31.5) | 3441 (68.5) | ||
| Total | 7318 | 100.00 | 4945 (67.6) | 2373 (32.4) | 1807 (24.7) | 5511 (75.3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Zhang, Y.; Long, S.; Fu, X.; Zhang, X.; Zhao, S.; Xiu, S.; Wang, X.; Lu, B.; Jin, H. Non-EPI Vaccine Hesitancy among Chinese Adults: A Cross-Sectional Study. Vaccines 2021, 9, 772. https://doi.org/10.3390/vaccines9070772
Wang J, Zhang Y, Long S, Fu X, Zhang X, Zhao S, Xiu S, Wang X, Lu B, Jin H. Non-EPI Vaccine Hesitancy among Chinese Adults: A Cross-Sectional Study. Vaccines. 2021; 9(7):772. https://doi.org/10.3390/vaccines9070772
Chicago/Turabian StyleWang, Jianli, Yan Zhang, Sigui Long, Xin Fu, Xiaoxuan Zhang, Shuangyu Zhao, Shixin Xiu, Xuwen Wang, Bing Lu, and Hui Jin. 2021. "Non-EPI Vaccine Hesitancy among Chinese Adults: A Cross-Sectional Study" Vaccines 9, no. 7: 772. https://doi.org/10.3390/vaccines9070772
APA StyleWang, J., Zhang, Y., Long, S., Fu, X., Zhang, X., Zhao, S., Xiu, S., Wang, X., Lu, B., & Jin, H. (2021). Non-EPI Vaccine Hesitancy among Chinese Adults: A Cross-Sectional Study. Vaccines, 9(7), 772. https://doi.org/10.3390/vaccines9070772





