Fuzzy and Sample Entropies as Predictors of Patient Survival Using Short Ventricular Fibrillation Recordings during out of Hospital Cardiac Arrest
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection and Labeling
2.2. Shock Outcome Predictors
2.2.1. Shock Outcome Predictors from the Literature
2.2.2. Quantification of VF Waveform Regularity-Based on Entropy Measures
2.3. Optimal Parameters for SampEn and FuzzyEn
2.4. Evaluation of Shock Outcome Prediction
2.5. Complementary Analyses
3. Results
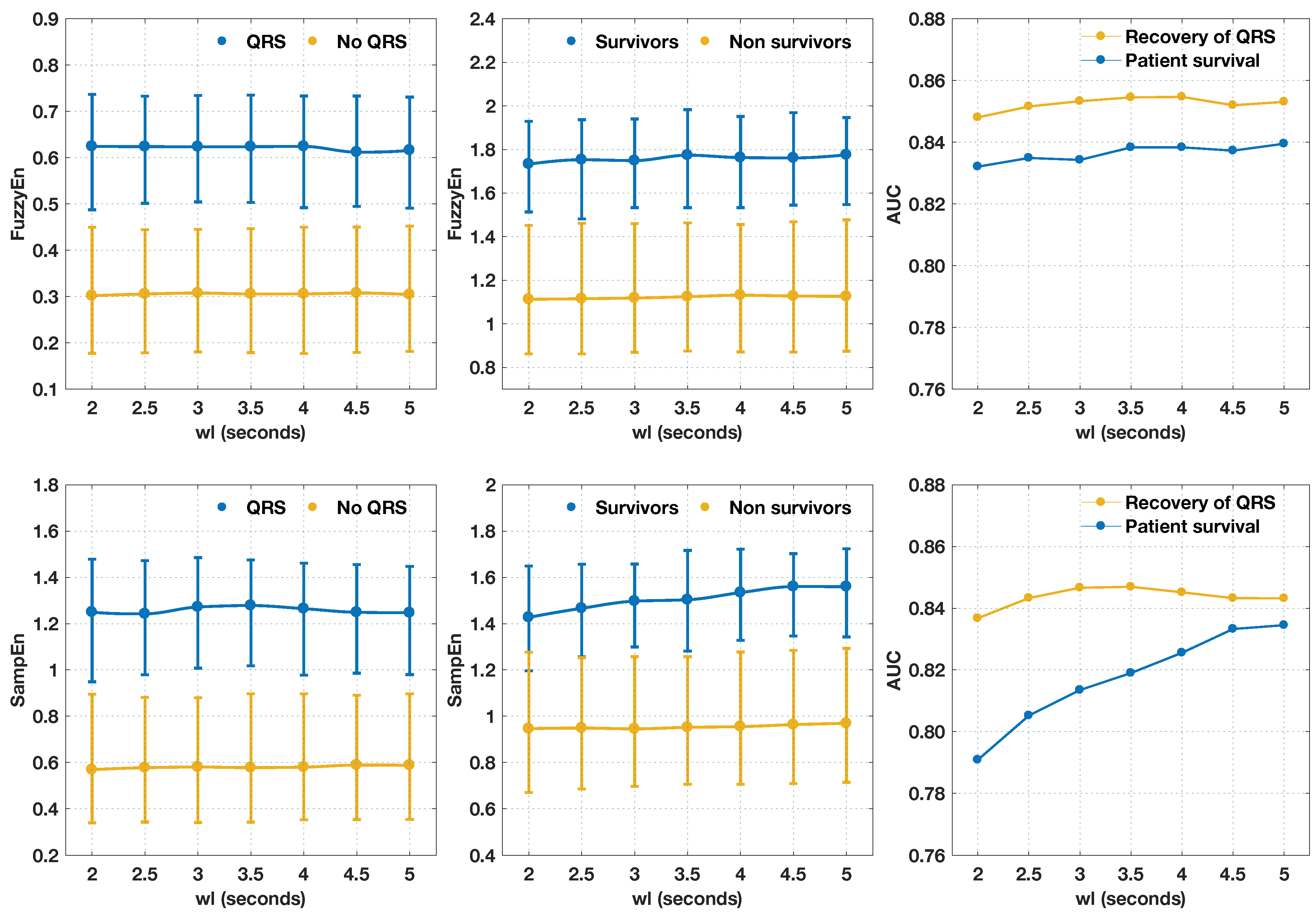
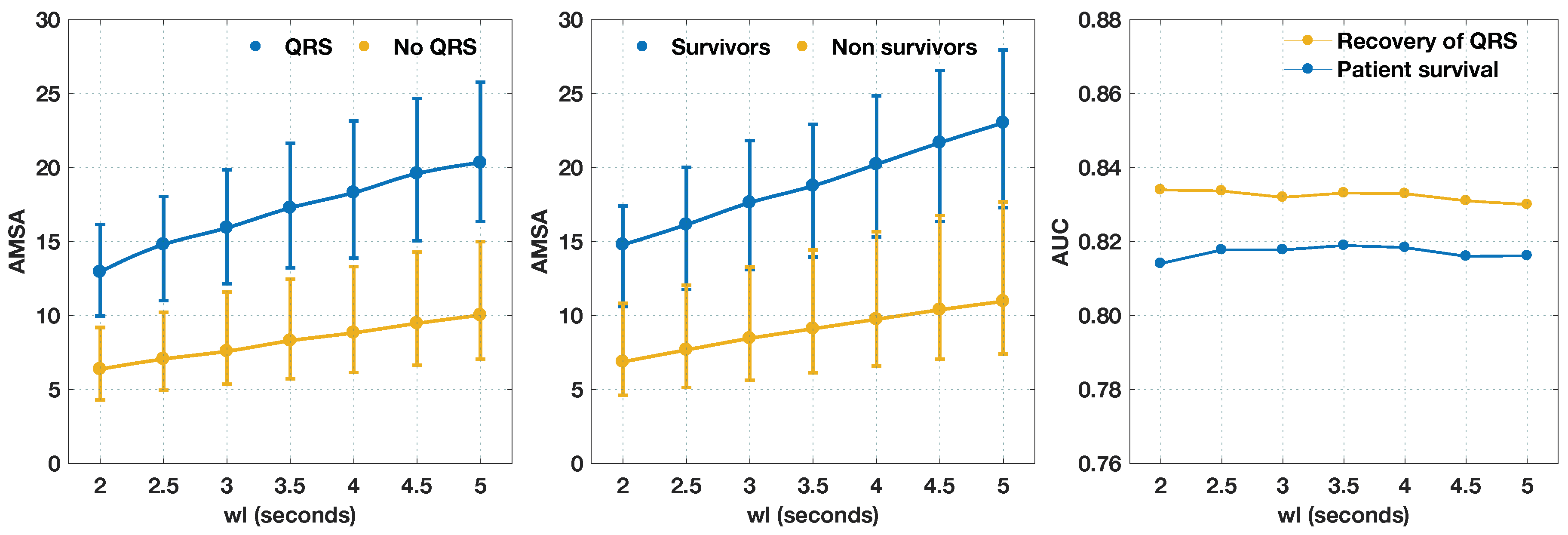
3.1. Optimal Parameters to Compute Entropy Measures
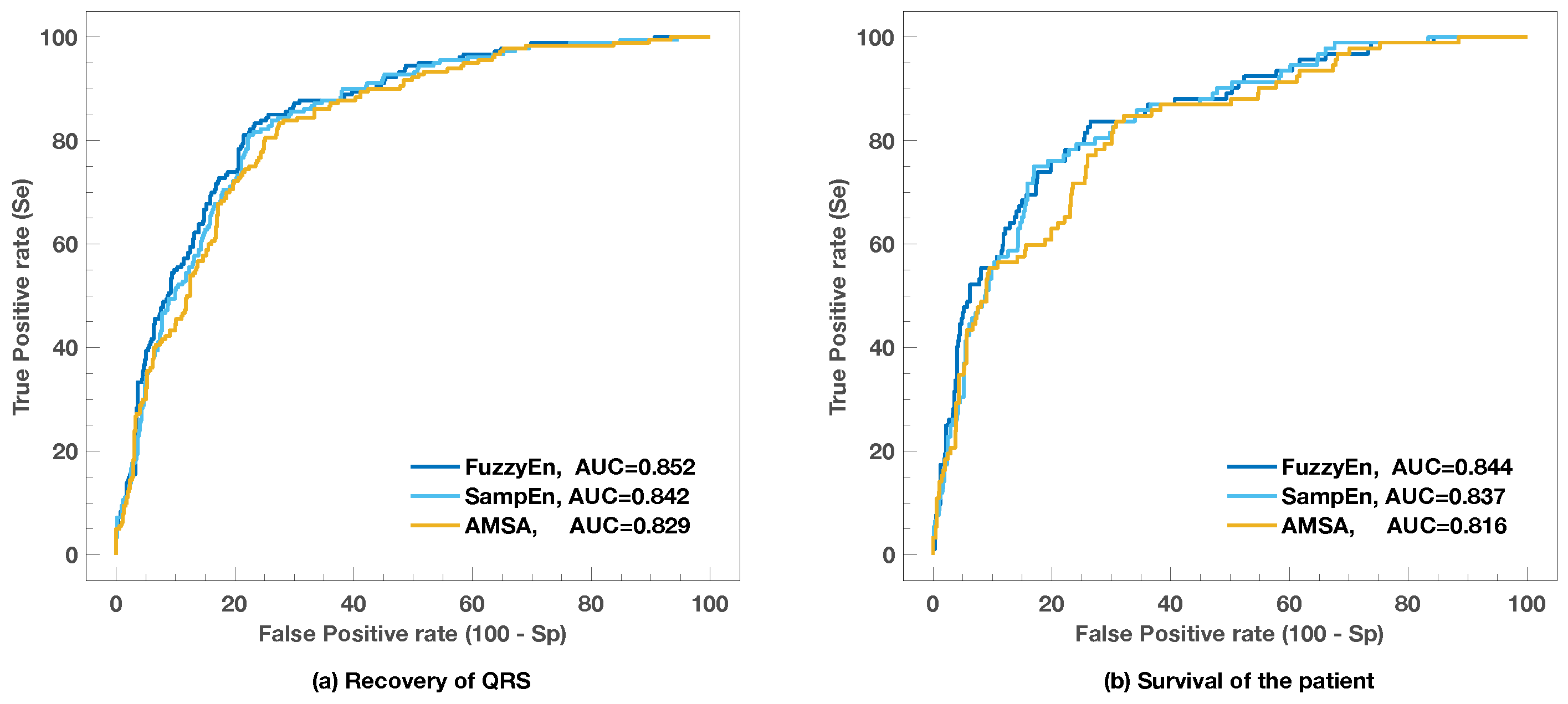
3.2. Comparison with Other Shock Outcome Predictors
3.3. Shortening the Analysis Interval
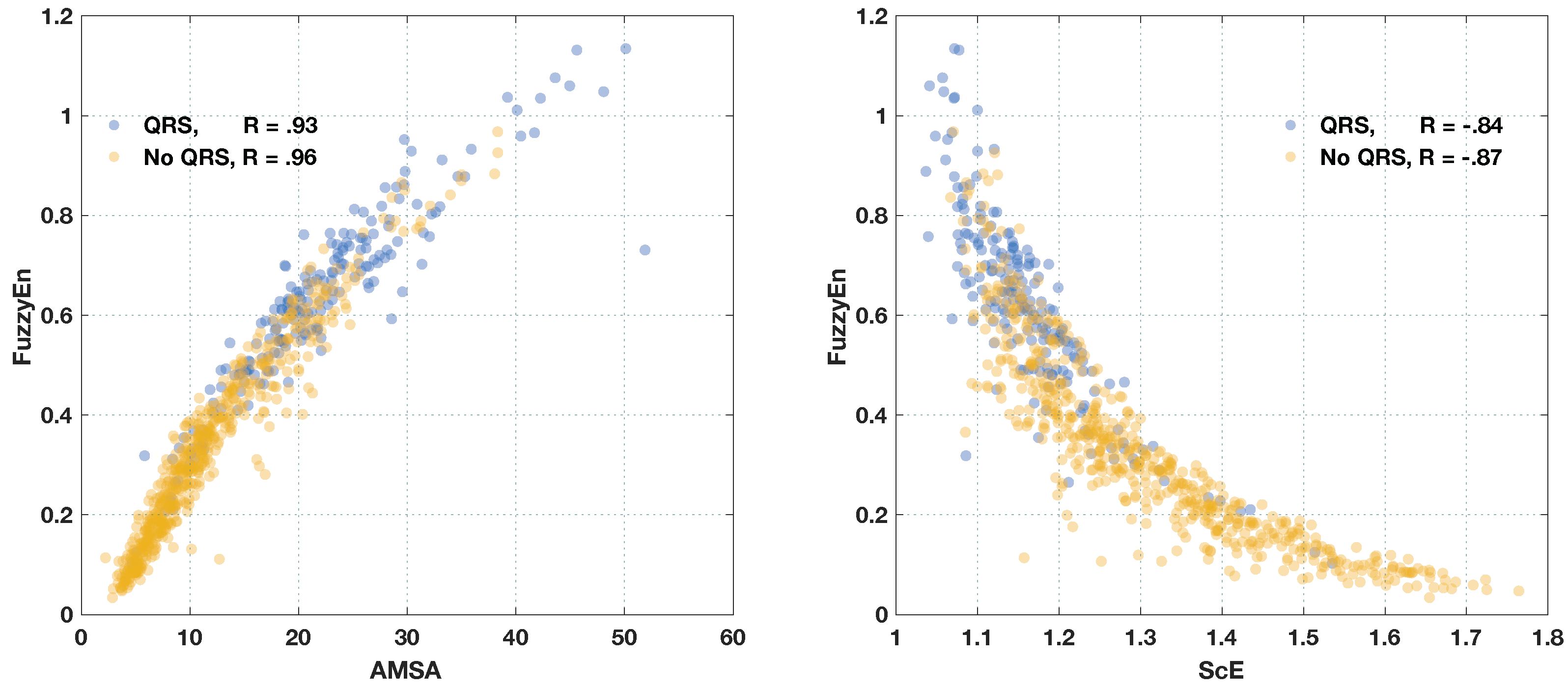
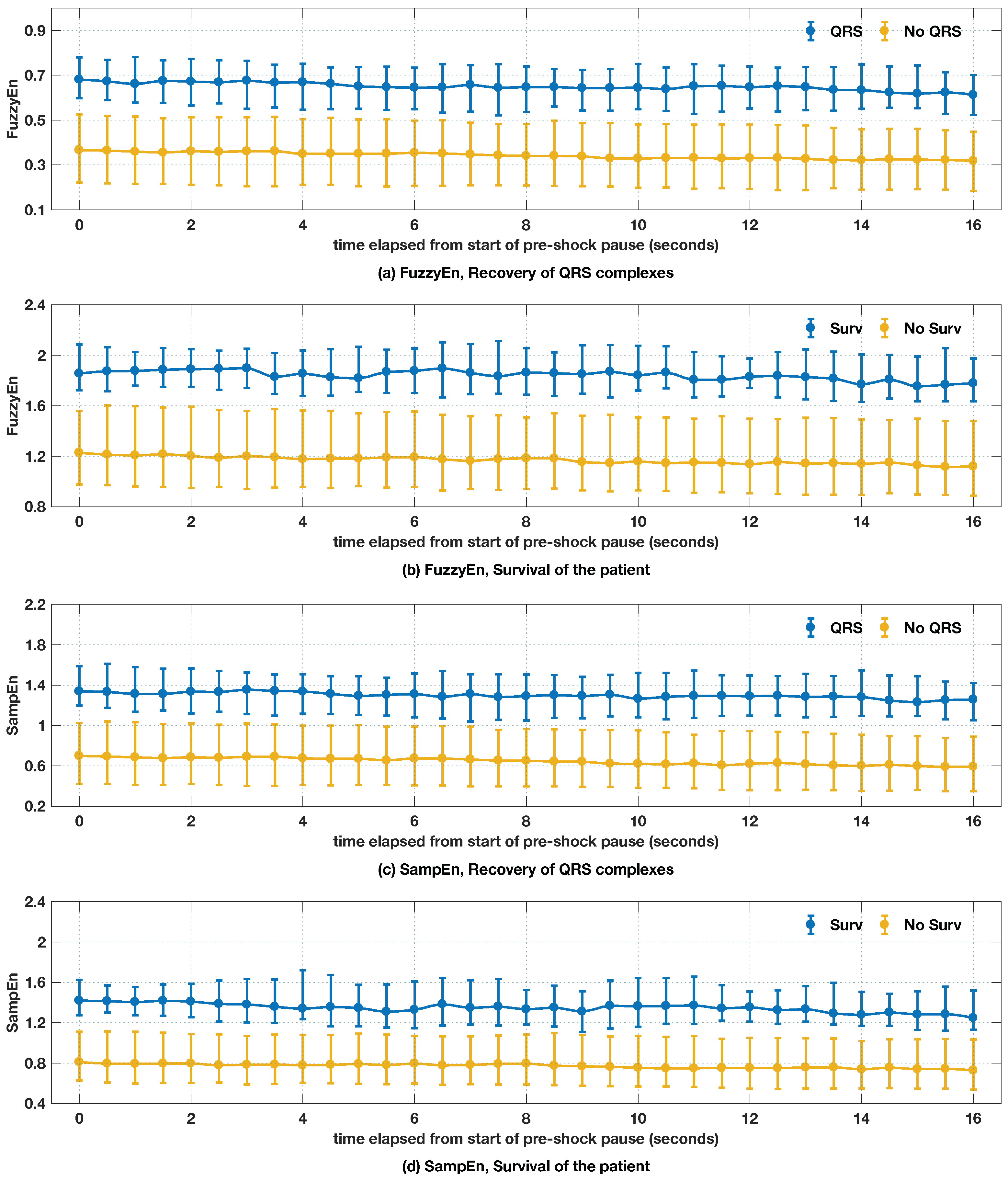
3.4. Evolution of Entropy Values During the Preshock Pause
4. Discussion and Conclusions
Author Contributions
Funding
Conflicts of Interest
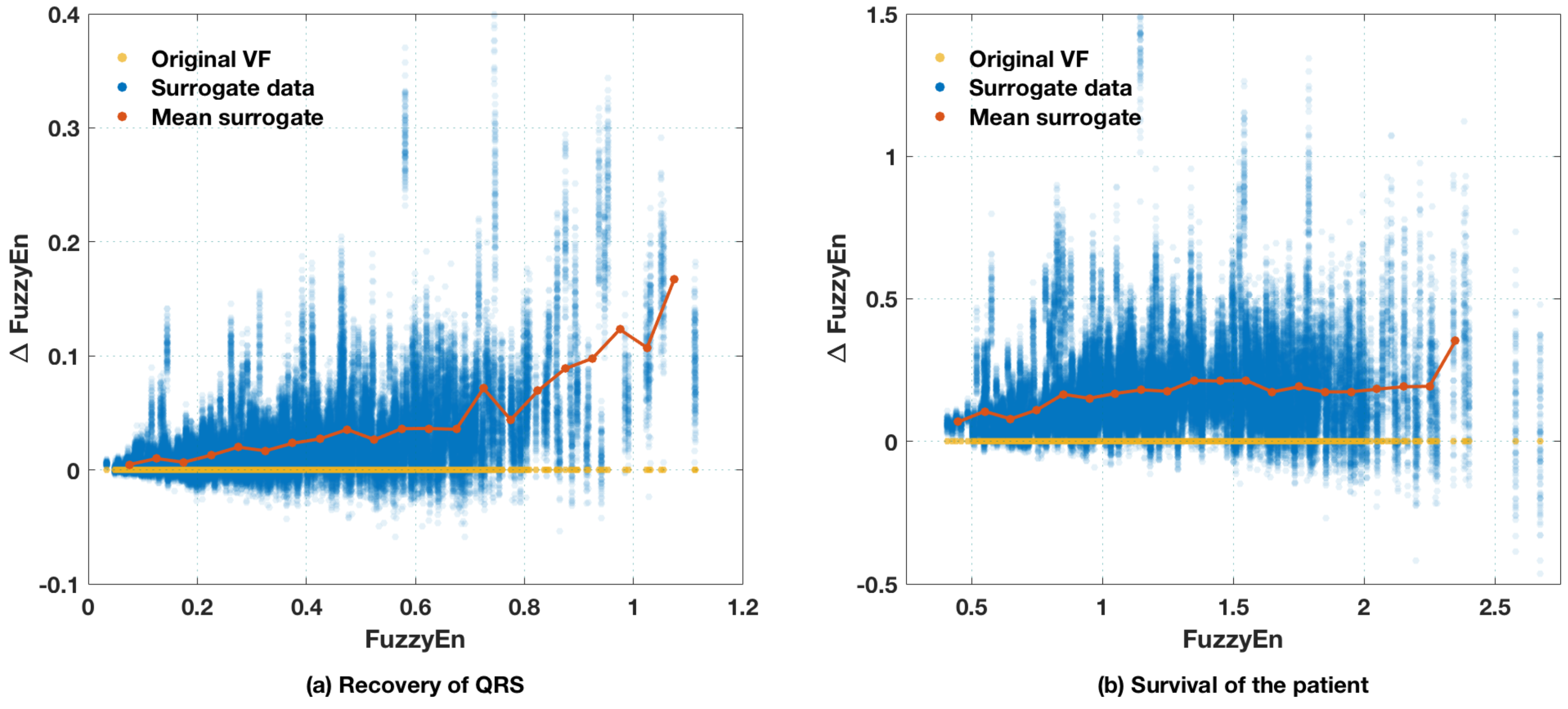
Appendix A. Surrogate Data Testing
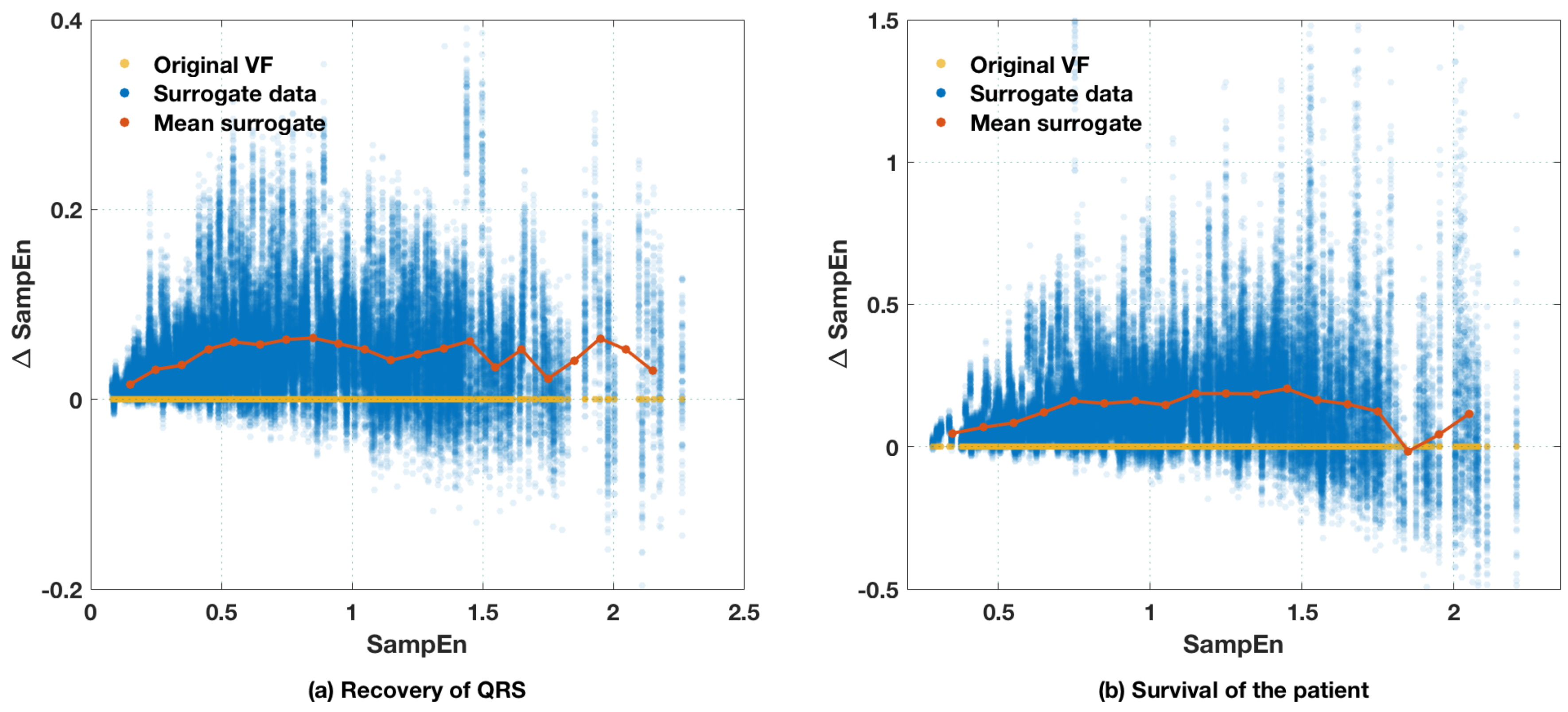
Appendix B. Time Delayed Entropies and Sampling Frequency


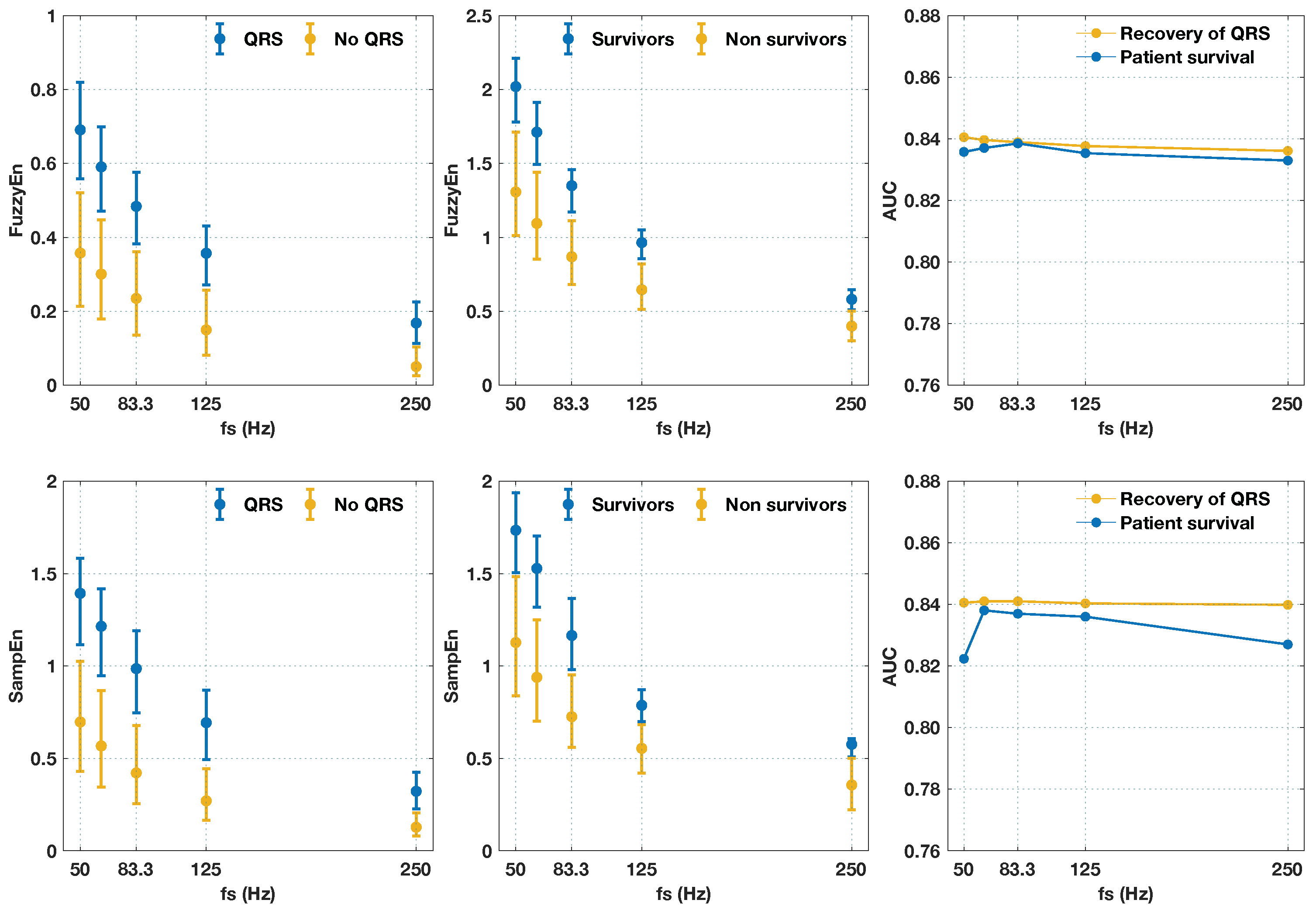
Appendix C. Relations Between FuzzyEn and Other Predictors
References
- Gräsner, J.T.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, B.M.; Ortiz, F.R. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Rubart, M.; Zipes, D.P. Mechanisms of sudden cardiac death. J. Clin. Investig. 2005, 115, 2305–2315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zoll, P.M. Resuscitation of the heart in ventricular standstill by external electric stimulation. N. Engl. J. Med. 1952, 247, 768–771. [Google Scholar] [CrossRef] [PubMed]
- Cobb, L.A.; Fahrenbruch, C.E.; Walsh, T.R.; Copass, M.K.; Olsufka, M.; Breskin, M.; Hallstrom, A.P. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA 1999, 281, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- Wik, L.; Hansen, T.B.; Fylling, F.; Steen, T.; Vaagenes, P.; Auestad, B.H.; Steen, P.A. Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with out-of-hospital ventricular fibrillation: A randomized trial. JAMA 2003, 289, 1389–1395. [Google Scholar] [CrossRef] [PubMed]
- Link, M.S.; Atkins, D.L.; Passman, R.S.; Halperin, H.R.; Samson, R.A.; White, R.D.; Cudnik, M.T.; Berg, M.D.; Kudenchuk, P.J.; Kerber, R.E. Part 6: Electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010, 122, S706–S719. [Google Scholar] [CrossRef] [PubMed]
- Takata, T.S.; Page, R.L.; Joglar, J.A. Automated external defibrillators: technical considerations and clinical promise. Ann. Int. Med. 2001, 135, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Figuera, C.; Irusta, U.; Morgado, E.; Aramendi, E.; Ayala, U.; Wik, L.; Kramer-Johansen, J.; Eftestøl, T.; Alonso-Atienza, F. Machine Learning Techniques for the Detection of Shockable Rhythms in Automated External Defibrillators. PLoS ONE 2016, 11, e0159654. [Google Scholar] [CrossRef] [PubMed]
- Telesz, B.J.; Hess, E.P.; Atkinson, E.; White, R.D. Recurrent ventricular fibrillation: experience with first responders prior to advanced life support interventions. Resuscitation 2015, 88, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Weil, M.H.; Sun, S.; Tang, W.; Sato, Y.; Jin, X.; Bisera, J. High-energy defibrillation increases the severity of postresuscitation myocardial dysfunction. Circulation 1997, 96, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Cheskes, S.; Schmicker, R.H.; Christenson, J.; Salcido, D.D.; Rea, T.; Powell, J.; Edelson, D.P.; Sell, R.; May, S.; Menegazzi, J.J.; et al. Perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation 2011, 124, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.J.; Clegg, G.R.; Robertson, C.E. Analysing the ventricular fibrillation waveform. Resuscitation 2003, 57, 11–20. [Google Scholar] [CrossRef]
- Firoozabadi, R.; Nakagawa, M.; Helfenbein, E.D.; Babaeizadeh, S. Predicting defibrillation success in sudden cardiac arrest patients. J. Electrocardiol. 2013, 46, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Ristagno, G.; Li, Y.; Fumagalli, F.; Finzi, A.; Quan, W. Amplitude spectrum area to guide resuscitation-a retrospective analysis during out-of-hospital cardiopulmonary resuscitation in 609 patients with ventricular fibrillation cardiac arrest. Resuscitation 2013, 84, 1697–1703. [Google Scholar] [CrossRef] [PubMed]
- Callaway, C.W.; Menegazzi, J.J. Waveform analysis of ventricular fibrillation to predict defibrillation. Curr. Opin. Crit. Care 2005, 11, 192–199. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Gong, Y.; Li, Y.; Mauri, T.; Fumagalli, F.; Bozzola, M.; Cesana, G.; Latini, R.; Pesenti, A.; Ristagno, G. Combining multiple ECG features does not improve prediction of defibrillation outcome compared to single features in a large population of out-of-hospital cardiac arrests. Crit. Care 2015, 19, 425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, C.G.; Dzwonczyk, R. Signal analysis of the human electrocardiogram during ventricular fibrillation: frequency and amplitude parameters as predictors of successful countershock. Ann. Emerg. Med. 1996, 27, 184–188. [Google Scholar] [CrossRef]
- Sherman, L.D.; Callaway, C.W.; Menegazzi, J.J. Ventricular fibrillation exhibits dynamical properties and self-similarity. Resuscitation 2000, 47, 163–173. [Google Scholar] [CrossRef]
- Weaver, W.D.; Cobb, L.A.; Dennis, D.; Ray, R.; Hallstrom, A.P.; Copass, M.K. Amplitude of ventricular fibrillation waveform and outcome after cardiac arrest. Ann. Int. Med. 1985, 102, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Jekova, I.; Mougeolle, F.; Valance, A. Defibrillation shock success estimation by a set of six parameters derived from the electrocardiogram. Phys. Meas 2004, 25, 1179. [Google Scholar] [CrossRef]
- Wu, X.; Bisera, J.; Tang, W. Signal integral for optimizing the timing of defibrillation. Resuscitation 2013, 84, 1704–1707. [Google Scholar] [CrossRef] [PubMed]
- Hamprecht, F.A.; Jost, D.; Rüttimann, M.; Calamai, F.; Kowalski, J.J. Preliminary results on the prediction of countershock success with fibrillation power. Resuscitation 2001, 50, 297–299. [Google Scholar] [CrossRef] [Green Version]
- Neurauter, A.; Eftestøl, T.; Kramer-Johansen, J.; Abella, B.S.; Sunde, K.; Wenzel, V.; Lindner, K.H.; Eilevstjønn, J.; Myklebust, H.; Steen, P.A.; et al. Prediction of countershock success using single features from multiple ventricular fibrillation frequency bands and feature combinations using neural networks. Resuscitation 2007, 73, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Ristagno, G.; Mauri, T.; Cesana, G.; Li, Y.; Finzi, A.; Fumagalli, F.; Rossi, G.; Grieco, N.; Migliori, M.; Andreassi, A.; et al. Amplitude spectrum area to guide defibrillation: a validation on 1617 patients with ventricular fibrillation. Circulation 2015, 131, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Eftestol, T.; Sunde, K.; Ole Aase, S.; Husoy, J.H.; Steen, P.A. Predicting outcome of defibrillation by spectral characterization and nonparametric classification of ventricular fibrillation in patients with out-of-hospital cardiac arrest. Circulation 2000, 102, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Povoas, H.P.; Bisera, J. Electrocardiographic waveform analysis for predicting the success of defibrillation. Crit. Care Med. 2000, 28, N210–N211. [Google Scholar] [CrossRef] [PubMed]
- Podbregar, M.; Kovačič, M.; Podbregar-Marš, A.; Brezocnik, M. Predicting defibrillation success by ‘genetic’ programming in patients with out-of-hospital cardiac arrest. Resuscitation 2003, 57, 153–159. [Google Scholar] [CrossRef]
- Callaway, C.W.; Sherman, L.D.; Mosesso, V.N.; Dietrich, T.J.; Holt, E.; Clarkson, M.C. Scaling exponent predicts defibrillation success for out-of-hospital ventricular fibrillation cardiac arrest. Circulation 2001, 103, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Sherman, L.D.; Rea, T.D.; Waters, J.D.; Menegazzi, J.J.; Callaway, C.W. Logarithm of the absolute correlations of the ECG waveform estimates duration of ventricular fibrillation and predicts successful defibrillation. Resuscitation 2008, 78, 346–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, L.Y.; Lo, M.T.; Ko, P.C.I.; Lin, C.; Chiang, W.C.; Liu, Y.B.; Hu, K.; Lin, J.L.; Chen, W.J.; Ma, M.H.M. Detrended fluctuation analysis predicts successful defibrillation for out-of-hospital ventricular fibrillation cardiac arrest. Resuscitation 2010, 81, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Lu, Y.; Zhang, L.; Zhang, H.; Li, Y. Predict Defibrillation Outcome Using Stepping Increment of Poincare Plot for Out-of-Hospital Ventricular Fibrillation Cardiac Arrest. Biom. Res. Int. 2015, 2015, 493472. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.N.; Uchaipichat, N.; Addison, P.S.; Clegg, G.R.; Robertson, C.E.; Eftestol, T.; Steen, P.A. Improved prediction of defibrillation success for out-of-hospital VF cardiac arrest using wavelet transform methods. Resuscitation 2004, 63, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, K.; Kvaløy, J.T.; Kramer-Johansen, J.; Eftestøl, T. Identifying approaches to improve the accuracy of shock outcome prediction for out-of-hospital cardiac arrest. Resuscitation 2008, 76, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Howe, A.; Escalona, O.J.; Di Maio, R.; Massot, B.; Cromie, N.A.; Darragh, K.M.; Adgey, J.; McEneaney, D.J. A support vector machine for predicting defibrillation outcomes from waveform metrics. Resuscitation 2014, 85, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Indik, J.H.; Conover, Z.; McGovern, M.; Silver, A.E.; Spaite, D.W.; Bobrow, B.J.; Kern, K.B. Association of amplitude spectral area of the ventricular fibrillation waveform with survival of out-of-hospital ventricular fibrillation cardiac arrest. J. Am. Coll. Cardiol. 2014, 64, 1362–1369. [Google Scholar] [CrossRef] [PubMed]
- Coult, J.; Sherman, L.; Kwok, H.; Blackwood, J.; Kudenchuk, P.J.; Rea, T.D. Short ECG segments predict defibrillation outcome using quantitative waveform measures. Resuscitation 2016, 109, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Endoh, H.; Hida, S.; Oohashi, S.; Hayashi, Y.; Kinoshita, H.; Honda, T. Prompt prediction of successful defibrillation from 1-s ventricular fibrillation waveform in patients with out-of-hospital sudden cardiac arrest. J. Anesth. 2011, 25, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Chicote, B.; Irusta, U.; Alcaraz, R.; Rieta, J.J.; Aramendi, E.; Isasi, I.; Alonso, D.; Ibarguren, K. Application of Entropy-Based Features to Predict Defibrillation Outcome in Cardiac Arrest. Entropy 2016, 18, 313. [Google Scholar] [CrossRef]
- Richman, J.S.; Moorman, J.R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Phys. Heart Circ. Phys. 2000, 278, H2039–H2049. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Wang, Z.; Xie, H.; Yu, W. Characterization of surface EMG signal based on fuzzy entropy. IEEE Trans. Neural. Syst. Rehabil. Eng. 2007, 15, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Xiao-Feng, L.; Yue, W. Fine-grained permutation entropy as a measure of natural complexity for time series. Chin. Phys. B 2009, 18, 2690. [Google Scholar] [CrossRef]
- Fadlallah, B.; Chen, B.; Keil, A.; Príncipe, J. Weighted-permutation entropy: a complexity measure for time series incorporating amplitude information. Phys. Rev. E Stat. Nonlin Soft Matter Phys. 2013, 87, 022911. [Google Scholar] [CrossRef] [PubMed]
- Eftestøl, T.; Sunde, K.; Steen, P.A. Effects of interrupting precordial compressions on the calculated probability of defibrillation success during out-of-hospital cardiac arrest. Circulation 2002, 105, 2270–2273. [Google Scholar] [CrossRef] [PubMed]
- Edelson, D.P.; Abella, B.S.; Kramer-Johansen, J.; Wik, L.; Myklebust, H.; Barry, A.M.; Merchant, R.M.; Hoek, T.L.V.; Steen, P.A.; Becker, L.B. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation 2006, 71, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Ibarguren, K.; Unanue, J.M.; Alonso, D.; Vaqueriza, I.; Irusta, U.; Aramendi, E.; Chicote, B. Difference in survival from pre-hospital cardiac arrest between cities and villages in the Basque Autonomous Community. Resuscitation 2015, 96, 114. [Google Scholar] [CrossRef]
- Jacobs, I.; Nadkarni, V.; Bahr, J.; Berg, R.A.; Billi, J.E.; Bossaert, L.; Cassan, P.; Coovadia, A.; D’Este, K.; Finn, J.; et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries.: A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation 2004, 63, 233–249. [Google Scholar] [PubMed]
- Rittenberger, J.C.; Raina, K.; Holm, M.B.; Kim, Y.J.; Callaway, C.W. Association between Cerebral Performance Category, Modified Rankin Scale, and discharge disposition after cardiac arrest. Resuscitation 2011, 82, 1036–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chicote, B.; Irusta, U.; Aramendi, E.; Isasi, I.; Alonso, D.; Vicente, F.; Sanchez, M. Nonlinear energy operators for defibrillation shock outcome prediction. In Proceedings of the Computing in Cardiology Conference (CinC), Vancouver, BC, Canada, 11–14 September 2016; pp. 61–64. [Google Scholar]
- Marn-Pernat, A.; Weil, M.H.; Tang, W.; Pernat, A.; Bisera, J. Optimizing timing of ventricular defibrillation. Crit. Care Med. 2001, 29, 2360–2365. [Google Scholar] [CrossRef] [PubMed]
- Pincus, S.M. Approximate entropy as a measure of system complexity. Proc. Natl. Acad Sci. USA 1991, 88, 2297–2301. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhuang, J.; Yu, W.; Wang, Z. Measuring complexity using FuzzyEn, ApEn, and SampEn. Med. Eng. Phys. 2009, 31, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Alcaraz, R.; Abásolo, D.; Hornero, R.; Rieta, J.J. Optimal parameters study for sample entropy-based atrial fibrillation organization analysis. Comput. Meth. Prog. Biomed. 2010, 99, 124–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zou, K.H.; O’Malley, A.J.; Mauri, L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 2007, 115, 654–657. [Google Scholar] [CrossRef] [PubMed]
- Perkins, N.J.; Schisterman, E.F. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am. J. Epidemiol. 2006, 163, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Monsieurs, K.G.; Nolan, J.P.; Bossaert, L.L.; Greif, R.; Maconochie, I.K.; Nikolaou, N.I.; Perkins, G.D.; Soar, J.; Truhlář, A.; Wyllie, J.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015, 95, 1–80. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.; Ayala, U.; Ruiz de Gauna, S.; Irusta, U.; González-Otero, D.; Alonso, E.; Kramer-Johansen, J.; Eftestøl, T. Feasibility of automated rhythm assessment in chest compression pauses during cardiopulmonary resuscitation. Resuscitation 2013, 84, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Ayala, U.; Irusta, U.; Ruiz, J.; de Gauna, S.R.; González-Otero, D.; Alonso, E.; Kramer-Johansen, J.; Naas, H.; Eftestøl, T. Fully automatic rhythm analysis during chest compression pauses. Resuscitation 2015, 89, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Saini, B.S.; Singh, D. An alternative approach to approximate entropy threshold value (r) selection: application to heart rate variability and systolic blood pressure variability under postural challenge. Med. Biol. Eng. Comput. 2016, 54, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Neurauter, A.; Eftestøl, T.; Kramer-Johansen, J.; Abella, B.S.; Wenzel, V.; Lindner, K.H.; Eilevstjønn, J.; Myklebust, H.; Steen, P.A.; Sterz, F.; et al. Improving countershock success prediction during cardiopulmonary resuscitation using ventricular fibrillation features from higher ECG frequency bands. Resuscitation 2008, 79, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Rosso, O.A.; Blanco, S.; Yordanova, J.; Kolev, V.; Figliola, A.; Schürmann, M.; Başar, E. Wavelet entropy: A new tool for analysis of short duration brain electrical signals. J. Neurosci. Meth. 2001, 105, 65–75. [Google Scholar] [CrossRef]
- Weaver, B.; Wuensch, K.L. SPSS and SAS programs for comparing Pearson correlations and OLS regression coefficients. Behav. Res. Meth. 2013, 45, 880–895. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherman, L.D. The frequency ratio: An improved method to estimate ventricular fibrillation duration based on Fourier analysis of the waveform. Resuscitation 2006, 69, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Weisfeldt, M.L.; Becker, L.B. Resuscitation after cardiac arrest: a 3-phase time-sensitive model. JAMA 2002, 288, 3035–3038. [Google Scholar] [CrossRef] [PubMed]
- Gazmuri, R.J.; Berkowitz, M.; Cajigas, H. Myocardial effects of ventricular fibrillation in the isolated rat heart. Crit. Care Med. 1999, 27, 1542–1550. [Google Scholar] [CrossRef] [PubMed]
- Jardetzky, O.; Greene, E.A.; Lorber, V. Oxygen consumption of the completely isolated dog heart in fibrillation. Circul. Res. 1956, 4, 144–147. [Google Scholar] [CrossRef]
- Hoogendijk, M.G.; Schumacher, C.A.; Belterman, C.N.W.; Boukens, B.J.; Berdowski, J.; de Bakker, J.M.T.; Koster, R.W.; Coronel, R. Ventricular fibrillation hampers the restoration of creatine-phosphate levels during simulated cardiopulmonary resuscitations. Europace 2012, 14, 1518–1523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neumar, R.W.; Brown, C.G.; Van Ligten, P.; Hoekstra, J.; Altschuld, R.A.; Baker, P. Estimation of myocardial ischemic injury during ventricular fibrillation with total circulatory arrest using high-energy phosphates and lactate as metabolic markers. Ann. Emerg. Med. 1991, 20, 222–229. [Google Scholar] [CrossRef]
- Kern, K.B.; Garewal, H.S.; Sanders, A.B.; Janas, W.; Nelson, J.; Sloan, D.; Tacker, W.A.; Ewy, G.A. Depletion of myocardial adenosine triphosphate during prolonged untreated ventricular fibrillation: Effect on defibrillation success. Resuscitation 1990, 20, 221–229. [Google Scholar] [CrossRef]
- Choi, H.J.; Nguyen, T.; Park, K.S.; Cha, K.C.; Kim, H.; Lee, K.H.; Hwang, S.O. Effect of cardiopulmonary resuscitation on restoration of myocardial ATP in prolonged ventricular fibrillation. Resuscitation 2013, 84, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Salcido, D.D.; Menegazzi, J.J.; Suffoletto, B.P.; Logue, E.S.; Sherman, L.D. Association of intramyocardial high energy phosphate concentrations with quantitative measures of the ventricular fibrillation electrocardiogram waveform. Resuscitation 2009, 80, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, J.C.; Salcido, D.D.; Menegazzi, J.J. Correlation between coronary perfusion pressure and quantitative ECG waveform measures during resuscitation of prolonged ventricular fibrillation. Resuscitation 2012, 83, 1497–1502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Didon, J.P.; Krasteva, V.; Ménétré, S.; Stoyanov, T.; Jekova, I. Shock advisory system with minimal delay triggering after end of chest compressions: accuracy and gained hands-off time. Resuscitation 2011, 82 (Suppl. 2), S8–S15. [Google Scholar] [CrossRef]
- Ruiz de Gauna, S.; Irusta, U.; Ruiz, J.; Ayala, U.; Aramendi, E.; Eftestøl, T. Rhythm analysis during cardiopulmonary resuscitation: Past, present, and future. Biomed. Res. Int. 2014, 2014, 386010. [Google Scholar] [CrossRef] [PubMed]
- Manis, G.; Aktaruzzaman, M.; Sassi, R. Low Computational Cost for Sample Entropy. Entropy 2018, 20, 61. [Google Scholar] [CrossRef]
- Snyder, D.; Morgan, C. Wide variation in cardiopulmonary resuscitation interruption intervals among commercially available automated external defibrillators may affect survival despite high defibrillation efficacy. Criti. Care Med. 2004, 32, S421–S424. [Google Scholar] [CrossRef]
- Menegazzi, J.J.; Callaway, C.W.; Sherman, L.D.; Hostler, D.P.; Wang, H.E.; Fertig, K.C.; Logue, E.S. Ventricular fibrillation scaling exponent can guide timing of defibrillation and other therapies. Circulation 2004, 109, 926–931. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Lin, Z.; Zhang, T.T.; Liu, N.; Liu, T.; Ser, W.; Koh, Z.X.; Ong, M.E.H. Effects of two new features of approximate entropy and sample entropy on cardiac arrest prediction. In Proceedings of the 2015 IEEE International Symposium on Circuits and Systems (ISCAS), Lisbon, Portugal, 24–27 May 2015; pp. 65–68. [Google Scholar]
- Lombardi, F.; Mäkikallio, T.H.; Myerburg, R.J.; Huikuri, H.V. Sudden cardiac death: role of heart rate variability to identify patients at risk. Cardiovasc. Res. 2001, 50, 210–217. [Google Scholar] [CrossRef] [Green Version]
- Moorman, J.R.; Carlo, W.A.; Kattwinkel, J.; Schelonka, R.L.; Porcelli, P.J.; Navarrete, C.T.; Bancalari, E.; Aschner, J.L.; Whit Walker, M.; Perez, J.A.; et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 2011, 159, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Sessa, F.; Anna, V.; Messina, G.; Cibelli, G.; Monda, V.; Marsala, G.; Ruberto, M.; Biondi, A.; Cascio, O.; Bertozzi, G.; et al. Heart rate variability as predictive factor for sudden cardiac death. Aging 2018, 10, 166–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Indik, J.H.; Allen, D.; Gura, M.; Dameff, C.; Hilwig, R.W.; Kern, K.B. Utility of the ventricular fibrillation waveform to predict a return of spontaneous circulation and distinguish acute from post myocardial infarction or normal Swine in ventricular fibrillation cardiac arrest. Circ. Arrhythm. Electrophysiol. 2011, 4, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Theiler, J.; Eubank, S.; Longtin, A.; Galdrikian, B.; Farmer, J.D. Testing for nonlinearity in time series: The method of surrogate data. Phys. D Nonlinear Phenom. 1992, 58, 77–94. [Google Scholar] [CrossRef]
- Schreiber, T.; Schmitz, A. Improved Surrogate Data for Nonlinearity Tests. Phys. Rev. Lett. 1996, 77, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Kaffashi, F.; Foglyano, R.; Wilson, C.G.; Loparo, K.A. The effect of time delay on approximate & sample entropy calculations. Phys. D Nonlinear Phenom. 2008, 237, 3069–3074. [Google Scholar]


| Criterion for Success | ||
|---|---|---|
| Electrical | Clinical | |
| SampEn | ||
| Range | , V | , V |
| Optimum | , V | , V |
| FuzzyEn | ||
| Range | , V | , V |
| Optimum | , V | , V |
| ROC Cutoff Point | ||||
|---|---|---|---|---|
| Se | Sp | Se/Sp (J) | Se/Sp (0,1) | |
| Electrical | ||||
| FuzzyEn | 55.0 | 56.1 | 83.3/76.7 | 81.1/78.5 |
| SampEn | 51.1 | 57.9 | 81.1/77.6 | 81.1/77.6 |
| AMSA | 44.4 | 52.2 | 83.3/72.6 | 80.6/74.9 |
| Survival | ||||
| FuzzyEn | 55.4 | 49.7 | 83.7/73.5 | 76.1/80.2 |
| SampEn | 53.3 | 52.2 | 75.0/83.0 | 75.0/83.0 |
| AMSA | 54.3 | 45.2 | 83.7/77.2 | 77.2/74.0 |
| Recovery of QRS | ||||
|---|---|---|---|---|
| Optimal Point | ||||
| Feature | AUC | BAC | Se/Sp | |
| FuzzyEn | [39] | 0.852 | 80.0 | 83.3/76.7 |
| SampEn | [39] | 0.842 | 79.4 | 81.1/77.6 |
| MdS | [24] | 0.839 | 78.0 | 81.7/74.4 |
| MSI | [32] | 0.838 | 78.4 | 82.2/74.5 |
| MS | [24] | 0.836 | 78.0 | 83.9/72.2 |
| PPA | [60] | 0.833 | 77.6 | 87.2/68.1 |
| SNEO | [49] | 0.829 | 77.1 | 77.8/76.4 |
| AMSA | [50] | 0.829 | 77.9 | 83.3/72.6 |
| PSA | [24] | 0.829 | 77.3 | 90.0/64.6 |
| ScE | [29] | 0.812 | 75.5 | 87.8/63.2 |
| AR | [21] | 0.797 | 76.0 | 87.2/64.8 |
| ENRG | [24] | 0.797 | 75.0 | 89.4/60.5 |
| RMS1 | [17] | 0.794 | 75.3 | 82.8/67.9 |
| RMS2 | [31] | 0.794 | 74.5 | 84.4/64.6 |
| MA | [18] | 0.793 | 74.6 | 90.6/58.7 |
| SigInt | [22] | 0.793 | 74.6 | 90.6/58.7 |
| LAC | [30] | 0.765 | 71.4 | 75.6/67.3 |
| MP | [24] | 0.764 | 71.0 | 72.8/69.3 |
| CP | [24] | 0.759 | 71.0 | 73.3/68.6 |
| DFA2 | [31] | 0.731 | 69.8 | 63.3/76.4 |
| Hu | [28] | 0.729 | 69.1 | 71.1/67.1 |
| PF | [26] | 0.724 | 70.0 | 76.1/63.9 |
| CF | [26] | 0.688 | 66.8 | 81.7/52.0 |
| WE | [61] | 0.683 | 66.3 | 78.9/53.8 |
| SFM | [26] | 0.658 | 62.8 | 54.4/71.1 |
| SEN | [17] | 0.644 | 61.6 | 61.7/61.6 |
| DFA1 | [31] | 0.532 | 55.2 | 46.7/63.7 |
| Survival of the Patient | ||||
| Optimal Point | ||||
| Feature | AUC | BAC | Se/Sp | |
| FuzzyEn | 0.844 | 78.6 | 83.7/73.5 | |
| SampEn | 0.837 | 79.0 | 75.0/83.0 | |
| MSI | 0.816 | 76.1 | 81.5/70.7 | |
| MdS | 0.816 | 76.3 | 81.5/71.0 | |
| AMSA | 0.816 | 76.4 | 83.7/69.2 | |
| MS | 0.812 | 76.0 | 81.5/70.6 | |
| PPA | 0.788 | 74.6 | 82.6/66.7 | |
| PSA | 0.781 | 73.5 | 88.0/58.9 | |
| SNEO | 0.779 | 72.5 | 85.9/59.0 | |
| ScE | 0.748 | 70.3 | 84.8/55.8 | |
| AR | 0.739 | 70.6 | 88.0/53.1 | |
| ENRG | 0.735 | 70.7 | 85.9/55.5 | |
| RMS1 | 0.735 | 69.4 | 79.3/59.5 | |
| RMS2 | 0.734 | 69.4 | 79.3/59.5 | |
| MA | 0.734 | 69.6 | 79.3/59.8 | |
| SigInt | 0.734 | 69.6 | 79.3/59.8 | |
| WE | 0.728 | 69.6 | 66.3/72.9 | |
| CF | 0.717 | 68.3 | 73.9/62.6 | |
| LAC | 0.701 | 65.5 | 78.3/52.8 | |
| PF | 0.698 | 66.7 | 57.6/75.7 | |
| MP | 0.695 | 65.6 | 59.8/71.3 | |
| Hu | 0.691 | 65.4 | 59.8/71.0 | |
| CP | 0.686 | 64.7 | 67.4/62.0 | |
| DFA2 | 0.652 | 63.7 | 52.2/75.2 | |
| DFA1 | 0.593 | 57.8 | 64.1/51.6 | |
| SFM | 0.544 | 55.4 | 22.8/88.0 | |
| SEN | 0.534 | 54.3 | 54.3/54.2 | |
| Recovery of QRS | Survival of Patient | |||||
|---|---|---|---|---|---|---|
| No | Yes | p-Value | No | Yes | p-Value | |
| FuzzyEn | ||||||
| Intercept | 0.389 | 0.664 | <0.01 | 1.280 | 1.917 | <0.01 |
| Slope (min−1) | −0.167 | −0.194 | 0.54 | −0.398 | −0.362 | 0.74 |
| SampEn | ||||||
| Intercept | 0.761 | 1.334 | <0.01 | 0.866 | 1.417 | <0.01 |
| Slope (min−1) | −0.351 | −0.385 | 0.72 | −0.279 | −0.432 | 0.15 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chicote, B.; Irusta, U.; Aramendi, E.; Alcaraz, R.; Rieta, J.J.; Isasi, I.; Alonso, D.; Baqueriza, M.D.M.; Ibarguren, K. Fuzzy and Sample Entropies as Predictors of Patient Survival Using Short Ventricular Fibrillation Recordings during out of Hospital Cardiac Arrest. Entropy 2018, 20, 591. https://doi.org/10.3390/e20080591
Chicote B, Irusta U, Aramendi E, Alcaraz R, Rieta JJ, Isasi I, Alonso D, Baqueriza MDM, Ibarguren K. Fuzzy and Sample Entropies as Predictors of Patient Survival Using Short Ventricular Fibrillation Recordings during out of Hospital Cardiac Arrest. Entropy. 2018; 20(8):591. https://doi.org/10.3390/e20080591
Chicago/Turabian StyleChicote, Beatriz, Unai Irusta, Elisabete Aramendi, Raúl Alcaraz, José Joaquín Rieta, Iraia Isasi, Daniel Alonso, María Del Mar Baqueriza, and Karlos Ibarguren. 2018. "Fuzzy and Sample Entropies as Predictors of Patient Survival Using Short Ventricular Fibrillation Recordings during out of Hospital Cardiac Arrest" Entropy 20, no. 8: 591. https://doi.org/10.3390/e20080591






