Distribution Assessments of Coumarins from Angelicae Pubescentis Radix in Rat Cerebrospinal Fluid and Brain by Liquid Chromatography Tandem Mass Spectrometry Analysis
Abstract
:1. Introduction
2. Results and Discussion
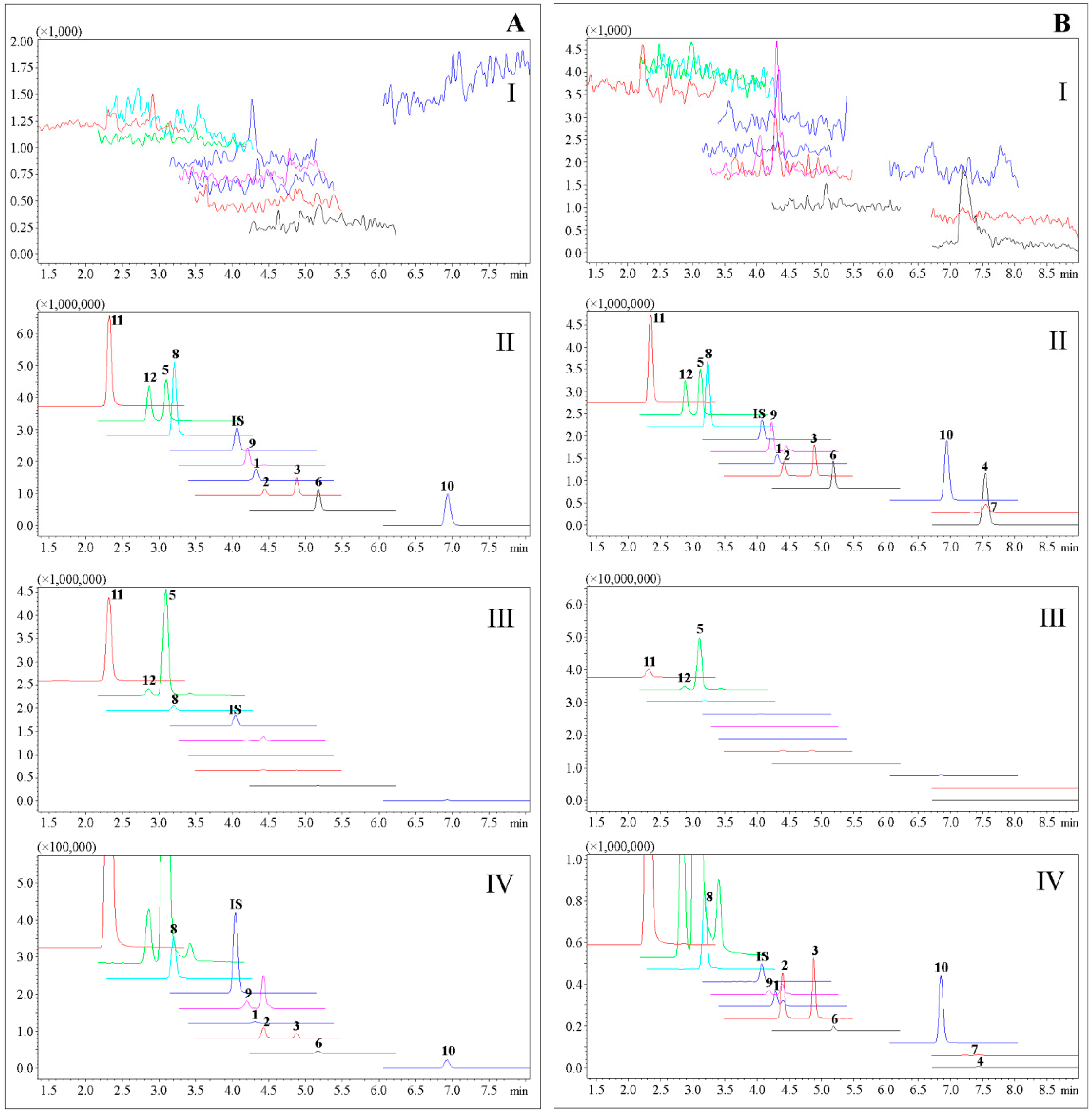
2.1. Analytical Method Validation
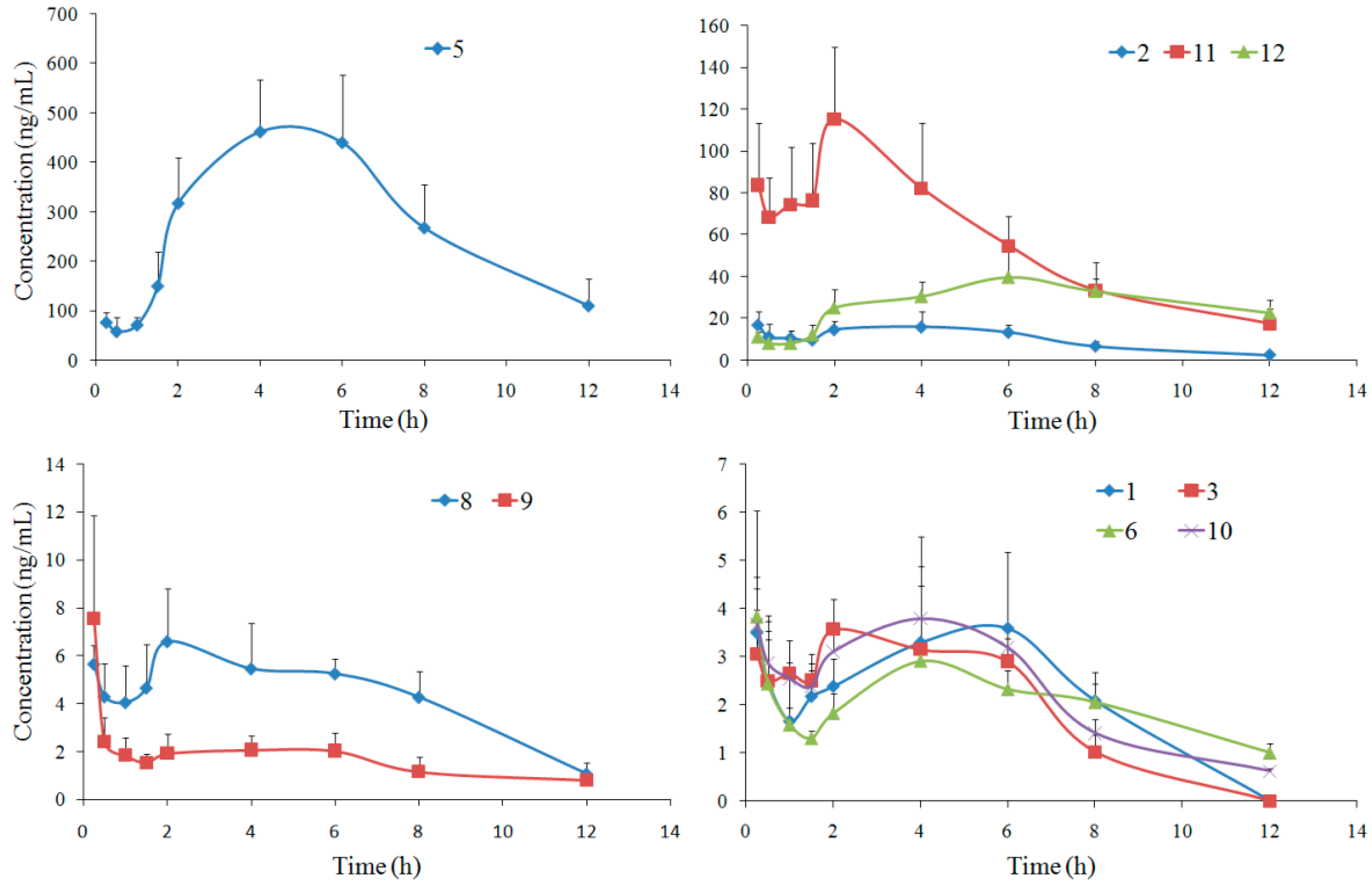
2.2. Rat CSF Distribution
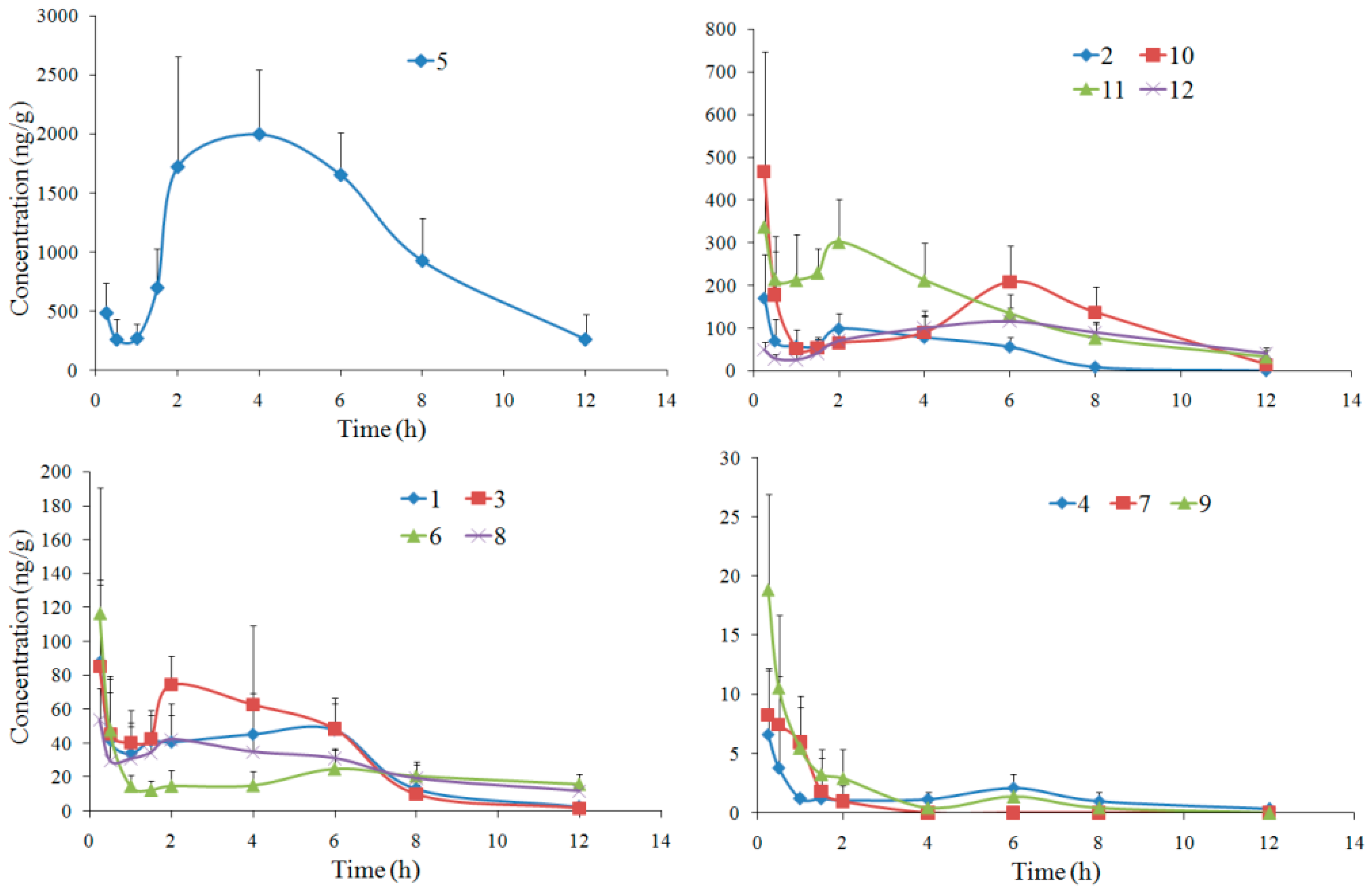
2.3. Rat Brain Distribution
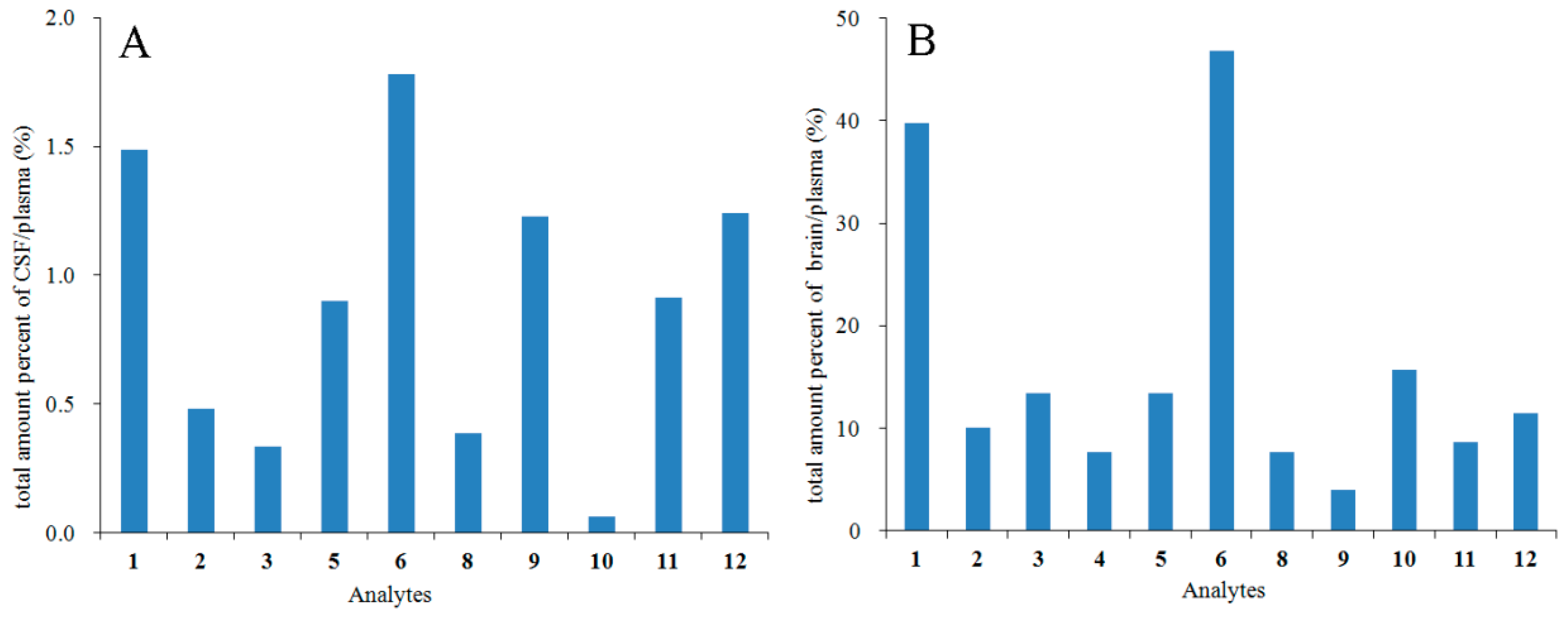
2.4. Relationship between the Pharmacokinetics and CSF/Brain Distribution
2.5. Relationship between the In Vivo and In Vitro BBB Penetration
3. Experimental Section
3.1. Chemicals and Reagents
3.2. Preparation of Calibration Standards and Quality Control Solutions
3.3. Preparation of Rat CSF and Brain Samples
3.4. UPLC-MS/MS Analysis
3.5. Animals and Dosing
3.6. Rat CSF and Brain Collections
3.7. Data Analysis
4. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China; China Medical Science and Technology Press: Bejing, China, 2015; Volume I, p. 263. [Google Scholar]
- Liu, J.H.; Xu, S.X.; Yao, X.S. Review of the chemical constituents and pharmacology research of Angelicae Pubescentis Radix. J. Shenyang Coll. Pharm. 1994, 11, 143–150. [Google Scholar]
- Yang, X.W.; Guo, Q.M.; Wang, Y. Absorption and transport of six coumarins isolated from the roots of Angelica pubescens f. biserrata in human Caco-2 cell monolayer model. J. Chin. Integr. Med. 2008, 6, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Long, J.; Li, S.N.; Yang, X.W. Absorption characteristics of four linear furocoumarins across human intestinal epithelial in a model of Caco-2 cell monolayer. Chin. J. New Drugs 2009, 18, 1865–1871. [Google Scholar]
- Li, S.N.; Yang, X.W. Absorption and transportation characteristic of six linear furocoumarins in a model of Caco-2 cell monolayer in human intestine. Chin. Tradit. Herb. Drugs 2011, 42, 96–102. [Google Scholar]
- Yang, Y.F.; Zhang, L.; Zhang, Y.B.; Yang, X.W. Simultaneous assessment of absorption characteristics of coumarins from Angelicae Pubescentis Radix: In Vitro transport across Caco-2 cell and In Vivo pharmacokinetics in rats after oral administration. J. Chromatogr. B 2017, 1060, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.F.; Jan, Y.M.; Huang, S.Y.; Wang, H.H.; Yu, L.L.; Chen, C.F. Evaluation with receptor binding assay on the water extracts of ten CNS-active Chinese herbal drugs. Proc. Natl. Sci. Counc. Repub. China B 1995, 19, 151–158. [Google Scholar] [PubMed]
- Pei, Y.; Li, D.X.; Sun, S.H. Experimental study on the effect of Radix Angelicae Pubescentis and its alcohol extract on apoptosis of brain cells in nature aging mice. Chin. J. Gerontol. 2005, 25, 959. [Google Scholar]
- Zhu, M.D.; Cui, J.P.; Wang, C.X. The experimental study of the intervention effect of Duhuo on immune damage of model rats suffering from Alzheimer. Liaoning J. Tradit. Chin. Med. 2011, 38, 2085–2086. [Google Scholar]
- Hu, Y.; Zhao, D.; Zhang, X.D.; Sun, D.; Hao, H.G.; Yang, J.X. Different extracts of Angelica pubescens inhibit H2O2-induced SH-SY5Y cells injury. Chin. J. Exp. Tradit. Med. Formulae 2013, 19, 184–188. [Google Scholar]
- Hu, Y.; Wen, Q.P.; Liang, W.B.; Kang, T.G.; Ren, L.; Zhang, N.; Zhao, D.; Sun, D.; Yang, J.X. Osthole reverses beta-amyloid peptide cytotoxicity on neural cells by enhancing cyclic AMP response element-binding protein phosphorylation. Biol. Pharm. Bull. 2013, 36, 1950–1958. [Google Scholar] [CrossRef] [PubMed]
- He, Y.L.; Qu, S.Y.; Wang, J.; He, X.S.; Lin, W.; Zhen, H.N.; Zhang, X. Neuroprotective effects of osthole pretreatment against traumatic brain injury in rats. Brain Res. 2012, 1433, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Hornick, A.; Lieb, A.; Vo, N.P.; Rollinger, J.M.; Stuppner, H.; Prast, H. The coumarin scopoletin potentiates acetylcholine release from synaptosomes, amplifies hippocampal long-term potentiation and ameliorates anticholinergic- and age-impaired memory. Neuroscience 2011, 197, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.K.; Lim, J.P.; Yang, J.H.; Eom, D.O.; Eun, J.S.; Leem, K.H. Acetylcholinesterase inhibitors from the roots of Angelica dahurica. Arch. Pharm. Res. 2002, 25, 856–859. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, S.; Gudbjarnason, S. Inhibition of acetylcholinesterase by extracts and constituents from Angelica archangelica and Geranium sylvaticum. Z. Naturforschung C 2007, 62, 689–693. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Veterinary Medicine. Guidance for Industry, Bioanalytical Method Validation. USA, 2013. Available online: http://www.fda.gov/ucm/groups/fdagov-public/@fdagov-drugs-gen/documents/document/ucm368107.pdf (accessed on 25 October 2017).
- Pardridge, W.M. CSF, blood-brain barrier, and brain drug delivery. Expert Opin. Drug Deliv. 2016, 13, 963–975. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.M.; Mohamed, Z.; Alshawsh, M.A.; Chik, Z. Evaluation of pharmacokinetics and blood-brain barrier permeability of mitragynine using in vivo microdialysis technique. J. Pharm. Biomed. Anal. 2017, 143, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.L.; Smith, P.M.; Lamm, W.J.; Hildebrandt, J. Sampling and analysis of cerebrospinal fluid for chronic studies in awake rats. J. Appl. Physiol. 1983, 54, 1754–1757. [Google Scholar] [CrossRef] [PubMed]
- Diehl, K.H.; Hull, R.; Morton, D.; Pfister, R.; Rabemampianina, Y.; Smith, D.; Vidal, J.M.; van de Vorstenbosch, C. A good practice guide to the administration of substances and removal of blood, including routes and volumes. J. Appl. Toxicol. 2001, 21, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.E. Rapid calculation of polar molecular surface area and its application to the prediction of transport phenomena. 2. Prediction of blood-brain barrier penetration. J. Pharm. Sci. 1999, 88, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Abraham, M.H.; Takács-Novák, K.; Mitchell, R.C. On the partition of Ampholytes: Application to blood-brain distribution. J. Pharm. Sci. 1997, 86, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.F.; Xu, W.; Song, W.; Ye, M.; Yang, X.W. Transport of twelve coumarins from Angelicae Pubescentis Radix across a MDCK-pHaMDR cell monolayer-an in vitro model for blood-brain barrier permeability. Molecules 2015, 20, 11719–11732. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.Y.; Zhang, B.G.; Yang, X.W. Studies on the chemical constituents of the root of Angelica pubescens f. biserrata. Pharm. J. Chin. PLA 2007, 23, 241–245. [Google Scholar]
- Yang, X.W.; Zhang, C.Y.; Zhang, B.G.; Lu, Y.; Luan, J.W.; Zheng, Q.T. Novel coumarin and furan from the roots of Angelica pubescens f. biserrata. J. Asian Nat. Prod. Res. 2009, 11, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Yang, X.W. Studies on chemical constituents in roots and rhizomes of Notopterygium incisum. China J. Chin. Mater. Med. 2008, 33, 2918–2921. [Google Scholar]
- Brégère, C.; Fisch, U.; Sailer, M.H.; Lieb, W.S.; Chicha, L.; Goepfert, F.; Kremer, T.; Guzman, R. Neonatal hypoxia-ischemia in rat increases doublecortin concentration in the cerebrospinal fluid. Eur. J. Neurosci. 2017, 46, 1758–1767. [Google Scholar] [CrossRef] [PubMed]
Sample Availability: Samples are not available from the authors. |

| Compound | MW | Precursor Ion | Product Ion | Q1 (V) | Q3 (V) | CE (V) | DT (msec) | RT (min) |
|---|---|---|---|---|---|---|---|---|
| 1 | 186 | 187 | 131.1 | −14 | −24 | −25 | 47 | 4.3 |
| 2 | 216 | 217 | 202.1 | −16 | −21 | −21 | 47 | 4.4 |
| 3 | 216 | 217 | 89.1 | −26 | −16 | −49 | 47 | 4.9 |
| 4 | 270 | 271 | 203.0 | −20 | −21 | −15 | 51 | 7.5 |
| 5 | 246 | 247 | 175.1 | −19 | −18 | −23 | 47 | 3.1 |
| 6 | 288 | 289 | 229.1 | −22 | −24 | −10 | 51 | 5.2 |
| 7 | 328 | 329 | 229.1 | −30 | −24 | −12 | 51 | 7.5 |
| 8 | 304 | 305 | 203.0 | −24 | −21 | −22 | 47 | 3.2 |
| 9 | 376 | 377 | 191.0 | −28 | −19 | −39 | 47 | 4.2 |
| 10 | 244 | 245 | 189.1 | −18 | −19 | −15 | 51 | 6.9 |
| 11 | 278 | 261 | 189.0 | −20 | −19 | −18 | 47 | 2.3 |
| 12 | 246 | 247 | 175.1 | −19 | −18 | −24 | 47 | 2.8 |
| IS | 254 | 255 | 199.1 | −19 | −20 | −24 | 100 | 4.1 |
| Compound | AUC0→t µg/L·h | AUC0→∞ µg/L·h | t1/2z h | Tmax h | CLz/F L/h/kg | Vz/F L/kg | Cmax µg/L |
|---|---|---|---|---|---|---|---|
| 1 | 20.40 ± 6.16 | 51.28 ± 17.49 | 3.52 ± 2.04 | 4.67 ± 1.63 | 22.80 ± 9.30 | 75.49 ± 28.52 | 4.49 ± 1.05 |
| 2 | 120.75 ± 19.00 | 129.46 ± 15.65 | 2.57 ± 0.89 | 1.50 ± 1.48 | 19.88 ± 2.56 | 76.01 ± 35.34 | 20.28 ± 5.13 |
| 3 | 27.08 ± 2.26 | 41.34 ± 5.77 | 6.72 ± 1.95 | 1.46 ± 0.84 | 34.09 ± 5.69 | 319.33 ± 65.49 | 3.95 ± 0.24 |
| 5 | 3374.64 ± 604.02 | 4142.82 ± 602.33 | 4.06 ± 2.42 | 5.00 ± 1.10 | 0.44 ± 0.06 | 2.52 ± 1.42 | 485.36 ± 91.4 |
| 6 | 24.16 ± 3.44 | 43.63 ± 22.07 | 7.68 ± 3.28 | 0.30 ± 0.11 | 102.68 ± 34.34 | 1030.65 ± 388.37 | 4.49 ± 1.91 |
| 8 | 54.03 ± 8.20 | 73.64 ± 11.84 | 6.32 ± 1.95 | 2.00 ± 1.14 | 11.02 ± 2.02 | 97.70 ± 24.17 | 7.47 ± 1.69 |
| 9 | 20.01 ± 3.35 | 28.17 ± 3.94 | 7.02 ± 2.51 | 0.38 ± 0.31 | 251.74 ± 39.96 | 2507.26 ± 843.89 | 7.65 ± 4.14 |
| 10 | 27.70 ± 2.88 | 30.51 ± 1.53 | 3.19 ± 1.16 | 2.83 ± 2.84 | 766.97 ± 36.55 | 3573.87 ± 1393.27 | 4.31 ± 1.49 |
| 11 | 675.91 ± 107.84 | 753.71 ± 141.64 | 3.37 ± 0.75 | 2.17 ± 0.98 | 2.24 ± 0.38 | 10.70 ± 1.87 | 128.51 ± 20.19 |
| 12 | 330.91 ± 43.19 | 624.72 ± 249.36 | 6.69 ± 2.25 | 6.33 ± 0.82 | 1.89 ± 0.61 | 16.76 ± 2.68 | 43.50 ± 5.98 |
| Compound | AUC0→t µg/kg·h | AUC0→∞ µg/kg·h | t1/2z h | Tmax h | CLz/F g/h/kg | Vz/F g/kg | Cmax µg/g |
|---|---|---|---|---|---|---|---|
| 1 | 351.63 ± 65.06 | 371.95 ± 69.76 | 2.15 ± 0.67 | 0.33 ± 0.13 | 2.88 ± 0.58 | 8.86 ± 3.08 | 99.93 ± 30.91 |
| 2 | 519.05 ± 151.70 | 732.88 ± 450.63 | 1.88 ± 0.96 | 0.33 ± 0.13 | 4.26 ± 1.71 | 16.48 ± 11.23 | 192.74 ± 74.07 |
| 3 | 418.20 ± 93.60 | 449.85 ± 97.52 | 2.34 ± 1.04 | 1.21 ± 1.53 | 3.22 ± 0.85 | 10.76 ± 4.73 | 104.59 ± 36.22 |
| 4 | 15.51 ± 4.82 | 21.56 ± 14.56 | 3.54 ± 1.35 | 0.33 ± 0.13 | 52.86 ± 24.79 | 245.44 ± 108.54 | 8.32 ± 4.75 |
| 5 | 13,438.17 ± 2016.06 | 16,664.04 ± 3662.67 | 3.92 ± 3.33 | 4.00 ± 1.79 | 0.11 ± 0.02 | 0.57 ± 0.39 | 2245.65 ± 638.71 |
| 6 | 251.98 ± 58.91 | 489.71 ± 222.11 | 8.22 ± 4.54 | 0.33 ± 0.13 | 9.77 ± 5.25 | 95.22 ± 25.54 | 128.03 ± 63.26 |
| 8 | 313.39 ± 59.25 | 397.36 ± 66.83 | 4.91 ± 0.91 | 0.96 ± 0.86 | 2.04 ± 0.34 | 14.45 ± 3.95 | 62.56 ± 13.78 |
| 9 | 21.06 ± 8.70 | 25.06 ± 8.03 | 2.77 ± 1.15 | 0.29 ± 0.10 | 301.26 ± 92.33 | 1299.16 ± 842.00 | 19.74 ± 7.52 |
| 10 | 1327.91 ± 341.99 | 2105.63 ± 1100.15 | 5.36 ± 2.15 | 0.35 ± 0.14 | 13.96 ± 7.04 | 60.18 ± 25.11 | 448.58 ± 206.25 |
| 11 | 1752.16 ± 249.82 | 1948.10 ± 305.84 | 3.64 ± 1.40 | 1.29 ± 1.50 | 0.86 ± 0.13 | 4.46 ± 1.60 | 396.56 ± 63.09 |
| 12 | 933.83 ± 66.51 | 1560.07 ± 730.91 | 6.27 ± 3.19 | 5.33 ± 1.03 | 0.779 ± 0.26 | 6.30 ± 2.22 | 129.97 ± 15.50 |
| Analytes | 1 | 2 | 3 | 4 | 5 | 6 | 7 * | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| log P | 2.08 | 2.17 | 2.17 | 3.70 | 1.67 | 2.54 | 4.28 | 1.11 | 2.04 | 4.08 | 1.10 | 1.59 |
| PSA | 39.44 | 48.67 | 48.67 | 48.67 | 55.76 | 61.83 | 61.83 | 89.13 | 102.29 | 35.53 | 75.99 | 55.76 |
| log BBpred. | −0.13 | −0.25 | −0.25 | −0.02 | −0.43 | −0.39 | −0.13 | −1.01 | −1.06 | 0.23 | −0.82 | −0.44 |
| log BBexpt. | 0.56 | −0.04 | 0.08 | −0.16 | 0.08 | 0.63 | – | −0.16 | −0.44 | 0.15 | −0.10 | 0.01 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.-F.; Zhang, L.; Yang, X.-W. Distribution Assessments of Coumarins from Angelicae Pubescentis Radix in Rat Cerebrospinal Fluid and Brain by Liquid Chromatography Tandem Mass Spectrometry Analysis. Molecules 2018, 23, 225. https://doi.org/10.3390/molecules23010225
Yang Y-F, Zhang L, Yang X-W. Distribution Assessments of Coumarins from Angelicae Pubescentis Radix in Rat Cerebrospinal Fluid and Brain by Liquid Chromatography Tandem Mass Spectrometry Analysis. Molecules. 2018; 23(1):225. https://doi.org/10.3390/molecules23010225
Chicago/Turabian StyleYang, Yan-Fang, Lei Zhang, and Xiu-Wei Yang. 2018. "Distribution Assessments of Coumarins from Angelicae Pubescentis Radix in Rat Cerebrospinal Fluid and Brain by Liquid Chromatography Tandem Mass Spectrometry Analysis" Molecules 23, no. 1: 225. https://doi.org/10.3390/molecules23010225




