Fortification of Fermented Camel Milk with Salvia officinalis L. or Mentha piperita Leaves Powder and Its Biological Effects on Diabetic Rats
Abstract
:1. Introduction
2. Results
2.1. Proximate Chemical Composition of Peppermint and Sage Leaves Powder and Their Antioxidant Activity
2.2. Chemical Composition of Sage and Mint Extracts Using Liquid Chromatography–Electrospray Ionization–Tandem Mass Spectrometry of Sage and Mint Extracts (LC-MS)
2.3. Effect of Fermented Camel Milk on Alloxan-Induced Diabetic Rats
2.3.1. Serum Glucose and Insulin Determination
2.3.2. Lipid Profile
2.4. Liver Functions
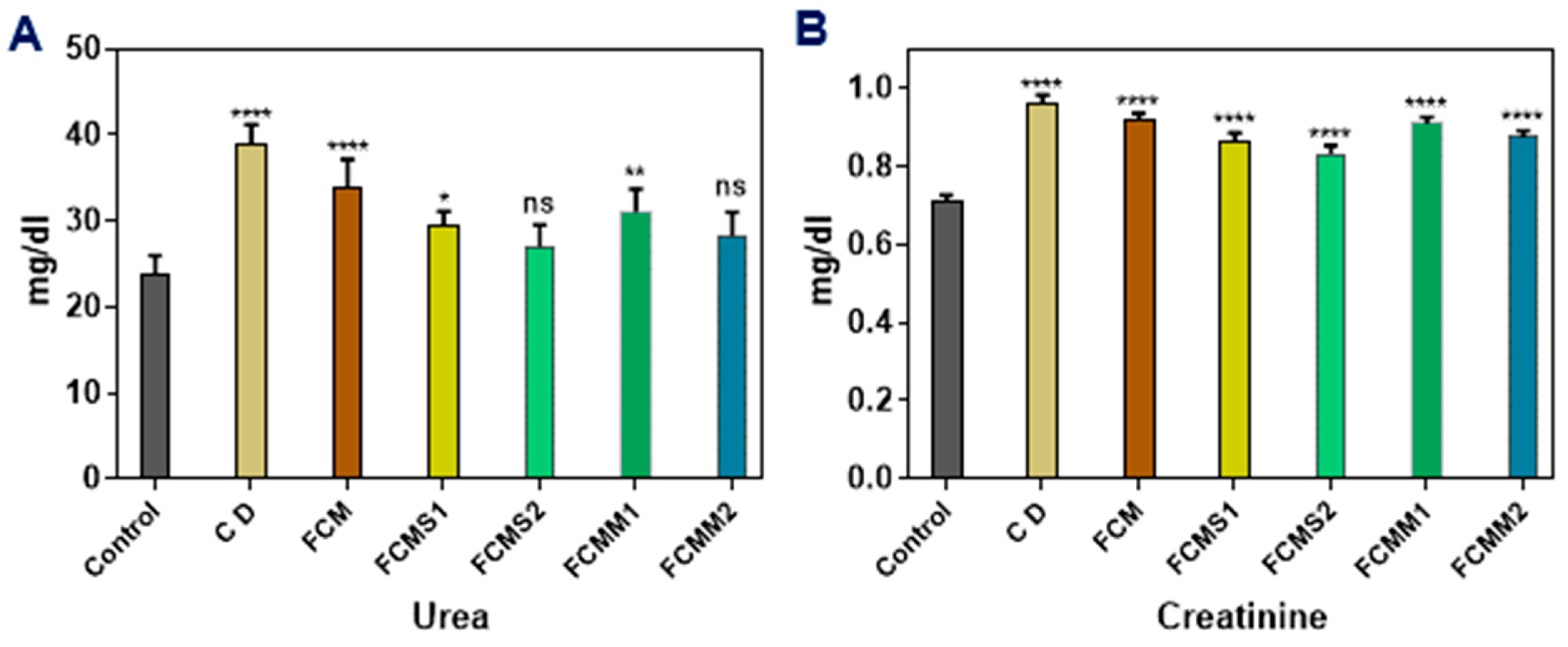
2.5. Kidney Functions
3. Discussion
4. Material and Methods
4.1. Materials and Chemicals
4.2. Methods
4.2.1. Preparation of Mint and Sage Leaves Powder
4.2.2. Preparation of Sage and Mint Extracts for Proximate Chemical Analysis
4.2.3. Preparation of Standard Compounds and Extract Samples Solutions and Identification of Their Chemical Composition of Sage and Mint Extracts and Their Compounds Using LC-ESI-MS/MS
4.2.4. Antioxidant Activity of Sage and Mint Extracts
Determination of Total Phenolic Contents (TPC) of Sage and Mint Extracts
Determination of Total Flavonoids (TF)
DPPH Scavenging Activity %
Ferric Reducing Antioxidant Power (FRAP)
4.2.5. Physicochemical Analysis of Camel Milk
4.2.6. Preparation of Fermented Camel Milk (FCMs)
4.2.7. Animals and Treatments
The Induction of Experimental Diabetes
Experimental Design
Blood Biochemical and Enzymes Activities
Determination of Blood Insulin Level
4.2.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
List of Abbreviations
References
- Korish, A.A.; Abdel Gader, A.G.; Korashy, H.M.; Al-Drees, A.M.; Alhaider, A.A.; Arafah, M.M. Camel milk attenuates the biochemical and morphological features of diabetic nephropathy: Inhibition of Smad1 and collagen type IV synthesis. Chem.-Biol. Interact. 2015, 229, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Al Kury, L.T.; Abdoh, A.; Ikbariah, K.; Sadek, B.; Mahgoub, M. In Vitro and In Vivo Antidiabetic Potential of Monoterpenoids: An Update. Molecules 2021, 27, 182. [Google Scholar] [CrossRef] [PubMed]
- Federation, I.D. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021; Available online: https://diabetesatlas.org/atlas/tenth-edition/ (accessed on 31 December 2021).
- Sharma, S.; Kulkarni, S.K.; Chopra, K. Curcumin, the active principle of turmeric (Curcuma longa), ameliorates diabetic nephropathy in rats. Clin. Exp. Pharmacol. Physiol. 2006, 33, 940–945. [Google Scholar] [CrossRef]
- FAO Stat. 2019. Available online: http://www.fao.org/faostat/en/#home (accessed on 30 November 2006).
- Ereifej, K.; Aludatt, M.; Alkhalidy, H.; Alli, I.; Rababah, T. Comparison and characterisation of fat and protein composition for camel milk from eight Jordanian locations. Food Chem. Food Chem. 2011, 127, 282–289. [Google Scholar] [CrossRef]
- Mati, A.; Senoussi-Ghezali, C.; Si Ahmed Zennia, S.; Almi-Sebbane, D.; El-Hatmi, H.; Girardet, J.-M. Dromedary camel milk proteins, a source of peptides having biological activities—A review. Int. Dairy J. 2017, 73, 25–37. [Google Scholar] [CrossRef]
- Kamal, M.; Karoui, R. Monitoring of mild heat treatment of camel milk by front-face fluorescence spectroscopy. LWT Food Sci. Technol. 2017, 79, 586–593. [Google Scholar] [CrossRef]
- Swelum, A.A.; El-Saadony, M.T.; Abdo, M.; Ombarak, R.A.; Hussein, E.O.S.; Suliman, G.; Alhimaidi, A.R.; Ammari, A.A.; Ba-Awadh, H.; Taha, A.E.; et al. Nutritional, antimicrobial and medicinal properties of Camel’s milk: A review. Saudi J. Biol. Sci. 2021, 28, 3126–3136. [Google Scholar] [CrossRef]
- Quan, S.; Tsuda, H.; Miyamoto, T. Angiotensin I-converting enzyme inhibitory peptides in skim milk fermented with Lactobacillus helveticus 130B4 from camel milk in Inner Mongolia, China. J. Sci. Food Agric. 2008, 88, 2688–2692. [Google Scholar] [CrossRef]
- Agrawal, R.P.; Tantia, P.; Jain, S.; Agrawal, R.; Agrawal, V. Camel milk: A possible boon for type 1 diabetic patients. Cell. Mol. Biol. 2013, 59, 99–107. [Google Scholar] [PubMed]
- Kamal, H.; Jafar, S.; Mudgil, P.; Murali, C.; Amin, A.; Maqsood, S. Inhibitory properties of camel whey protein hydrolysates toward liver cancer cells, dipeptidyl peptidase-IV, and inflammation. J. Dairy Sci. 2018, 101, 8711–8720. [Google Scholar] [CrossRef] [Green Version]
- Solanki, D.; Hati, S. Fermented camel milk: A Review on its bio-functional properties. Emir. J. Food Agric. 2018, 30, 268–274. [Google Scholar]
- El-Sayed, M.; Awad, S.; Abou-Soliman, N. Improving the Antioxidant Properties of Fermented Camel Milk Using Some Strains of Lactobacillus. Food Nutr. Sci. 2021, 12, 352–371. [Google Scholar] [CrossRef]
- Mohammadabadi, T. The unique effects of camel milk as adjunctive super food on the health. World J. Pharm. Sci. 2021, 9, 97–106. [Google Scholar]
- Rasheed, Z. Medicinal values of bioactive constituents of camel milk: A concise report. Int. J. Health Sci. 2017, 11, 1–2. [Google Scholar]
- Meena, S.; Rajput, Y.S.; Pandey, A.K.; Sharma, R.; Singh, R. Camel milk ameliorates hyperglycaemia and oxidative damage in type-1 diabetic experimental rats. J. Dairy Res. 2016, 83, 412–419. [Google Scholar] [CrossRef]
- Badr, G.; Sayed, L.H.; Omar, H.E.M.; Abd El-Rahim, A.M.; Ahmed, E.A.; Mahmoud, M.H. Camel Whey Protein Protects B and T Cells from Apoptosis by Suppressing Activating Transcription Factor-3 (ATF-3)-Mediated Oxidative Stress and Enhancing Phosphorylation of AKT and IκB-α in Type I Diabetic Mice. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2017, 41, 41–54. [Google Scholar] [CrossRef]
- Agrawal, R.P.; Saran, S.; Sharma, P.; Gupta, R.P.; Kochar, D.K.; Sahani, M.S. Effect of camel milk on residual beta-cell function in recent onset type 1 diabetes. Diabetes Res. Clin. Pract. 2007, 77, 494–495. [Google Scholar] [CrossRef] [PubMed]
- Fallah, Z.; Feizi, A.; Hashemipour, M.; Kelishadi, R. Effect of fermented camel milk on glucose metabolism, insulin resistance, and inflammatory biomarkers of adolescents with metabolic syndrome: A double-blind, randomized, crossover trial. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2018, 23, 32. [Google Scholar] [CrossRef]
- Atwaa, E.S.H.; Shahein, M.R.; El-Sattar, E.S.A.; Hijazy, H.H.A.; Albrakati, A.; Elmahallawy, E.K. Bioactivity, Physicochemical and Sensory Properties of Probiotic Yoghurt Made from Whole Milk Powder Reconstituted in Aqueous Fennel Extract. Fermentation 2022, 8, 52. [Google Scholar] [CrossRef]
- Atwaa, E.S.H.; Shahein, M.R.; Radwan, H.A.; Mohammed, N.S.; Aloraini, M.A.; Albezrah, N.K.A.; Alharbi, M.A.; Sayed, H.H.; Daoud, M.A.; Elmahallawy, E.K. Antimicrobial Activity of Some Plant Extracts and Their Applications in Homemade Tomato Paste and Pasteurized Cow Milk as Natural Preservatives. Fermentation 2022, 8, 428. [Google Scholar] [CrossRef]
- Shahein, M.R.; Atwaa, E.S.H.; Alrashdi, B.M.; Ramadan, M.F.; Abd El-Sattar, E.S.; Siam, A.A.H.; Alblihed, M.A.; Elmahallawy, E.K. Effect of Fermented Camel Milk Containing Pumpkin Seed Milk on the Oxidative Stress Induced by Carbon Tetrachloride in Experimental Rats. Fermentation 2022, 8, 223. [Google Scholar] [CrossRef]
- Shahein, M.R.; Atwaa, E.S.H.; Elkot, W.F.; Hijazy, H.H.A.; Kassab, R.B.; Alblihed, M.A.; Elmahallawy, E.K. The Impact of Date Syrup on the Physicochemical, Microbiological, and Sensory Properties, and Antioxidant Activity of Bio-Fermented Camel Milk. Fermentation 2022, 8, 192. [Google Scholar] [CrossRef]
- Shahein, M.R.; Atwaa, E.S.H.; El-Zahar, K.M.; Elmaadawy, A.A.; Hijazy, H.H.A.; Sitohy, M.Z.; Albrakati, A.; Elmahallawy, E.K. Remedial Action of Yoghurt Enriched with Watermelon Seed Milk on Renal Injured Hyperuricemic Rats. Fermentation 2022, 8, 41. [Google Scholar] [CrossRef]
- Shahein, M.R.; Atwaa, E.S.H.; Radwan, H.A.; Elmeligy, A.A.; Hafiz, A.A.; Albrakati, A.; Elmahallawy, E.K. Production of a Yogurt Drink Enriched with Golden Berry (Physalis pubescens L.) Juice and Its Therapeutic Effect on Hepatitis in Rats. Fermentation 2022, 8, 112. [Google Scholar] [CrossRef]
- Shahein, M.R.; Atwaa, E.-S.H.; Babalghith, A.O.; Alrashdi, B.M.; Radwan, H.A.; Umair, M.; Abdalmegeed, D.; Mahfouz, H.; Dahran, N.; Cacciotti, I.; et al. Impact of Incorporating the Aqueous Extract of Hawthorn (C. oxyanatha) Leaves on Yogurt Properties and Its Therapeutic Effects against Oxidative Stress Induced by Carbon Tetrachloride in Rats. Fermentation 2022, 8, 200. [Google Scholar] [CrossRef]
- Shahein, M.R.; Elkot, W.F.; Albezrah, N.K.A.; Abdel-Hafez, L.J.M.; Alharbi, M.A.; Massoud, D.; Elmahallawy, E.K. Insights into the Microbiological and Physicochemical Properties of Bio-Frozen Yoghurt Made with Probiotic Strains in Combination with Jerusalem Artichoke Tubers Powder. Fermentation 2022, 8, 390. [Google Scholar] [CrossRef]
- Swelam, S.; Zommara, M.A.; Abd El-Aziz, A.E.-A.M.; Elgammal, N.A.; Baty, R.S.; Elmahallawy, E.K. Insights into Chufa Milk Frozen Yoghurt as Cheap Functional Frozen Yoghurt with High Nutritional Value. Fermentation 2021, 7, 255. [Google Scholar] [CrossRef]
- Shokri, F.; Shokoohi, M.; Niazkar, H.R.; Abadi, A.; Kalarestaghi, H.; Ahin, M. Investigation the Spermatogenesis and Testis Structure in Diabetic Rats After Treatment With Galega officinalis Extract. Crescent J. Med. Biol. Sci. 2019, 6, 31–36. [Google Scholar]
- Abtahi-Eivari, S.H.; Shokoohi, M.; Ghorbani, M.; Halimi, M.; Hajizadeh, H.; Pourlak, T.; Bahrami, J.; Ghoreishi, Z. Effects of hydroalcoholic extracts of cloves (Syzygium aromaticum) on serum biomarkers, antioxidant status and histopathological changes of kidneys in diabetic rats. Crescent J. Med. Biol. Sci. 2021, 8, 269–275. [Google Scholar]
- Eftekhari, A.; Khusro, A.; Ahmadian, E.; Dizaj, S.M.; Hasanzadeh, A.; Cucchiarini, M. Phytochemical and nutra-pharmaceutical attributes of Mentha spp.: A comprehensive review. Arab. J. Chem. 2021, 14, 103106. [Google Scholar] [CrossRef]
- Rajeshwari, C.; Preeti, M.; Andallu, B. Efficacy of mint (Mentha spicata L.) leaves in combating oxidative stress in type 2 diabetes. Int. J. Life Sci. 2012, 1, 28–34. [Google Scholar]
- Mihailović, M.; Dinić, S.; Arambašić Jovanović, J.; Uskoković, A.; Grdović, N.; Vidaković, M. The influence of plant extracts and phytoconstituents on antioxidant enzymes activity and gene expression in the prevention and treatment of impaired glucose homeostasis and diabetes complications. Antioxidants 2021, 10, 480. [Google Scholar] [CrossRef] [PubMed]
- Nazir, N.; Zahoor, M.; Nisar, M.; Khan, I.; Ullah, R.; Alotaibi, A. Antioxidants isolated from elaeagnus umbellata (Thunb.) protect against bacterial infections and diabetes in streptozotocin-induced diabetic rat model. Molecules 2021, 26, 4464. [Google Scholar] [CrossRef]
- Hassan, H.A.; Hafez, H.S.; Goda, M.S. Mentha piperita as a pivotal neuro-protective agent against gamma irradiation induced DNA fragmentation and apoptosis: Mentha extract as a neuroprotective against gamma irradiation. Cytotechnology 2013, 65, 145–156. [Google Scholar] [CrossRef] [Green Version]
- Chandirasegaran, G.; Elanchezhiyan, C.; Suhasini, S.; Babby, A. Antihyperglycemic activity of Mentha piperita ethanol leaves extract on streptozotocin induced diabetic rats. Int. J. Pharm. Res. Sch 2014, 3, 2277–7873. [Google Scholar]
- Hamidpour, M.; Hamidpour, R.; Hamidpour, S.; Shahlari, M. Chemistry, Pharmacology, and Medicinal Property of Sage (Salvia) to Prevent and Cure Illnesses such as Obesity, Diabetes, Depression, Dementia, Lupus, Autism, Heart Disease, and Cancer. J. Tradit. Complement. Med. 2014, 4, 82–88. [Google Scholar] [CrossRef] [Green Version]
- Khashan, K.T.; Al-Khefaji, K.A. Effects of Salvia officinalis L. (sag) leaves extracts in normal and alloxan -induced diabetes in white rats. Int. J. Sci. Eng. Res. 2015, 2015, 20–28. [Google Scholar]
- Mahdizadeh, R.; Moein, S.; Soltani, N.; Malekzadeh, K.; Moein, M. Study the molecular mechanism of salvia species in prevention of diabetic. Int. J. Pharm. Sci. Res. 2018, 9, 4512–4521. [Google Scholar] [CrossRef]
- Agawane, S.B.; Gupta, V.S.; Kulkarni, M.J.; Bhattacharya, A.K.; Koratkar, S.S. Chemo-biological evaluation of antidiabetic activity of Mentha arvensis L. and its role in inhibition of advanced glycation end products. J. Ayurveda Integr. Med. 2019, 10, 166–170. [Google Scholar] [CrossRef]
- Eidi, A.; Eidi, M. Antidiabetic effects of sage (Salvia officinalis L.) leaves in normal and streptozotocin-induced diabetic rats. Diabetes Metab. Syndr. Clin. Res. Rev. 2009, 3, 40–44. [Google Scholar] [CrossRef]
- Figueroa-Pérez, M.G.; Gallegos-Corona, M.A.; Ramos-Gomez, M.; Reynoso-Camacho, R. Salicylic acid elicitation during cultivation of the peppermint plant improves anti-diabetic effects of its infusions. Food Funct. 2015, 6, 1865–1874. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; Dhar, P.S.; Anika, F.; Ahmed, L.; Islam, M.R.; Sultana, N.A.; Cavalu, S.; Pop, O.; Rauf, A. Exploring the plant-derived bioactive substances as antidiabetic agent: An extensive review. Biomed. Pharmacother. 2022, 152, 113217. [Google Scholar] [CrossRef] [PubMed]
- Shori, A.B. Camel milk as a potential therapy for controlling diabetes and its complications: A review of in vivo studies. J. Food Drug Anal. 2015, 23, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, M.A.; Palakkott, A.R.; Ashraf, A.; Iratni, R. The molecular basis of the anti-diabetic properties of camel milk. Diabetes Res. Clin. Pract. 2018, 146, 305–312. [Google Scholar] [CrossRef]
- Molitch, M.E.; DeFronzo, R.A.; Franz, M.J.; Keane, W.F.; Mogensen, C.E.; Parving, H.H.; Steffes, M.W. Nephropathy in diabetes. Diabetes Care 2004, 27 (Suppl. S1), S79–S83. [Google Scholar] [CrossRef] [Green Version]
- Lima, C.F.; Valentao, P.C.; Andrade, P.B.; Seabra, R.M.; Fernandes-Ferreira, M.; Pereira-Wilson, C. Water and methanolic extracts of Salvia officinalis protect HepG2 cells from t-BHP induced oxidative damage. Chem.-Biol. Interact. 2007, 167, 107–115. [Google Scholar] [CrossRef] [Green Version]
- Farnad, N.; Heidari, R.; Aslanipour, B. Phenolic composition and comparison of antioxidant activity of alcoholic extracts of Peppermint (Mentha piperita). J. Food Meas. Charact. 2014, 8, 113–121. [Google Scholar] [CrossRef]
- Yu, M.; Gouvinhas, I.; Rocha, J.; Barros, A.I. Phytochemical and antioxidant analysis of medicinal and food plants towards bioactive food and pharmaceutical resources. Sci. Rep. 2021, 11, 10041. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Christensen, K.B.; Olsen, L.C.; Christensen, L.P.; Grevsen, K.; Færgeman, N.J.; Kristiansen, K.; Young, J.F.; Oksbjerg, N. Bioactive components from flowers of Sambucus nigra L. increase glucose uptake in primary porcine myotube cultures and reduce fat accumulation in Caenorhabditis elegans. J. Agric. Food Chem. 2013, 61, 11033–11040. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Ni, C.-C.; Yin, M.-C.; Lii, C.-K. Flavonoids protect pancreatic beta-cells from cytokines mediated apoptosis through the activation of PI3-kinase pathway. Cytokine 2012, 59, 65–71. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Oksbjerg, N.; Young, J.; Jeppesen, P. Caffeic acid, naringenin and quercetin enhance glucose-stimulated insulin secretion and glucose sensitivity in INS-1E cells. Diabetes Obes. Metab. 2014, 16, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Oršolić, N.; Sirovina, D.; Odeh, D.; Gajski, G.; Balta, V.; Šver, L.; Jazvinšćak Jembrek, M. Efficacy of caffeic acid on diabetes and its complications in the mouse. Molecules 2021, 26, 3262. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, R.; Singh, S.V.; Jaiswal, K.; Kumar, R.; Pandey, A.K. Modulatory effect of caffeic acid in alleviating diabetes and associated complications. World J. Diabetes 2023, 14, 62. [Google Scholar] [CrossRef] [PubMed]
- Miao, L.; Zhang, H.; Cheong, M.S.; Zhong, R.; Garcia-Oliveira, P.; Prieto, M.A.; Cheng, K.-W.; Wang, M.; Cao, H.; Nie, S. Anti-diabetic potential of apigenin, luteolin, and baicalein via partially activating PI3K/Akt/Glut-4 signaling pathways in insulin-resistant HepG2 cells. Food Sci. Hum. Wellness 2023, 12, 1991–2000. [Google Scholar] [CrossRef]
- Bagul, P.K.; Deepthi, N.; Sultana, R.; Banerjee, S.K. Resveratrol ameliorates cardiac oxidative stress in diabetes through deacetylation of NFkB-p65 and histone 3. J. Nutr. Biochem. 2015, 26, 1298–1307. [Google Scholar] [CrossRef] [PubMed]
- Sheweita, S.A.; Newairy, A.A.; Mansour, H.A.; Yousef, M.I. Effect of some hypoglycemic herbs on the activity of phase I and II drug-metabolizing enzymes in alloxan-induced diabetic rats. Toxicology 2002, 174, 131–139. [Google Scholar] [CrossRef]
- Behr, G.A.; da Silva, E.G.; Ferreira, A.R.; Cerski, C.T.; Dal-Pizzol, F.; Moreira, J.C. Pancreas beta-cells morphology, liver antioxidant enzymes and liver oxidative parameters in alloxan-resistant and alloxan-susceptible Wistar rats: A viable model system for the study of concepts into reactive oxygen species. Fundam. Clin. Pharm. 2008, 22, 657–666. [Google Scholar] [CrossRef]
- Ceretta, L.B.; Réus, G.Z.; Abelaira, H.M.; Ribeiro, K.F.; Zappellini, G.; Felisbino, F.F.; Steckert, A.V.; Dal-Pizzol, F.; Quevedo, J. Increased oxidative stress and imbalance in antioxidant enzymes in the brains of alloxan-induced diabetic rats. Exp. Diabetes Res. 2012, 8, 302682. [Google Scholar] [CrossRef] [Green Version]
- Samarth, R.M. Protection against radiation induced hematopoietic damage in bone marrow of Swiss albino mice by Mentha piperita (Linn). J. Radiat. Res. 2007, 48, 523–528. [Google Scholar] [CrossRef] [Green Version]
- Samarth, R.M.; Samarth, M. Protection against radiation-induced testicular damage in Swiss albino mice by Mentha piperita (Linn.). Basic Clin. Pharmacol. Toxicol. 2009, 104, 329–334. [Google Scholar] [CrossRef]
- Sun, Z.; Wang, H.; Wang, J.; Zhou, L.; Yang, P. Chemical Composition and Anti-Inflammatory, Cytotoxic and Antioxidant Activities of Essential Oil from Leaves of Mentha piperita Grown in China. PLoS ONE 2014, 9, e114767. [Google Scholar] [CrossRef] [Green Version]
- Brahmi, F.; Boulekbache-Makhlouf, L.; Yalaoui-Guellal, D.; Mohamed, C.; Madani, K. Comparative study on the antioxidant effect of aqueous and ethanolic extracts of Mentha pulegium L. grown at two different locations. PhytoChem. BioSub. J. 2014, 8, 138–149. [Google Scholar]
- Fatiha, B.; Didier, H.; Naima, G.; Khodir, M.; Martin, K.; Léocadie, K.; Caroline, S.; Mohamed, C.; Pierre, D. Phenolic composition, in vitro antioxidant effects and tyrosinase inhibitory activity of three Algerian Mentha species: M. spicata (L.), M. pulegium (L.) and M. rotundifolia (L.) Huds (Lamiaceae). Ind. Crop. Prod. 2015, 74, 722–730. [Google Scholar] [CrossRef]
- El-Sayed, M.; Awad, S.; Ibrahim, A. Impact of Purslane (Portulaca oleracea L.) Extract as Antioxidant and Antimicrobial Agent on Overall Quality and Shelf Life of Greek-Style Yoghurt. Egypt. J. Food Sci. 2019, 47, 51–64. [Google Scholar] [CrossRef]
- Hussain, H.; Wattoo, F.H.; Wattoo, M.H.S.; Gulfraz, M.; Masud, T.; Shah, I.; Ali, S.; Alavi, S.E. Camel milk as an alternative treatment regimen for diabetes therapy. Food Sci. Nutr. 2021, 9, 1347–1356. [Google Scholar] [CrossRef]
- Shori, A.B.; Baba, A.S. Comparative antioxidant activity, proteolysis and in vitro α-amylase and α-glucosidase inhibition of Allium sativum-yogurts made from cow and camel milk. J. Saudi Chem. Soc. 2014, 18, 456–463. [Google Scholar] [CrossRef] [Green Version]
- Mansour, A.A.; Nassan, M.A.; Saleh, O.M.; Soliman, M.M. Protective Effect of Camel Milk As Anti-Diabetic Supplement: Biochemical, Molecular And Immunohistochemical Study. Afr. J. Tradit. Complement. Altern. Med. AJTCAM 2017, 14, 108–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sboui, A.; Khorchani, T.; Djegham, M.; Agrebi, A.; Elhatmi, H.; Belhadj, O. Anti-diabetic effect of camel milk in alloxan-induced diabetic dogs: A dose-response experiment. J. Anim. Physiol. Anim. Nutr. 2010, 94, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Hamad, E.M.; Abdel-Rahim, E.A.; Romeih, E.A. Beneficial effect of camel milk on liver and kidneys function in diabetic Sprague-Dawley rats. Int. J. Dairy Sci. 2011, 9, 190–197. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, R.; Swami, S.C.; Beniwal, R.; Kochar, D.; Sahani, M.S.; Tuteja, F.; Ghorui, S. Effect of camel milk on glycemic control, lipid profile and diabetes quality of life in type 1 diabetes: A randomised prospective controlled cross over study. Indian J. Anim. Sci. 2003, 73, 1105–1110. [Google Scholar]
- Agrawal, R.P.; Dogra, R.; Mohta, N.; Tiwari, R.; Singhal, S.; Sultania, S. Beneficial effect of camel milk in diabetic nephropathy. Acta Bio-Med. Atenei Parm. 2009, 80, 131–134. [Google Scholar]
- Agrawal, R.P.; Beniwal, R.; Sharma, S.; Kochar, D.K.; Tuteja, F.C.; Ghorui, S.K.; Sahani, M.S. Effect of raw camel milk in type 1 diabetic patients: 1 year randomised study. J. Camel Pract. Res. 2005, 12, 27–35. [Google Scholar]
- Mudgil, P.; Kamal, H.; Yuen, G.C.; Maqsood, S. Characterization and identification of novel antidiabetic and anti-obesity peptides from camel milk protein hydrolysates. Food Chem. 2018, 259, 46–54. [Google Scholar] [CrossRef]
- Nongonierma, A.B.; Cadamuro, C.; Le Gouic, A.; Mudgil, P.; Maqsood, S.; FitzGerald, R.J. Dipeptidyl peptidase IV (DPP-IV) inhibitory properties of a camel whey protein enriched hydrolysate preparation. Food Chem. 2019, 279, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Mudgil, P.; Baby, B.; Ngoh, Y.-Y.; Kamal, H.; Vijayan, R.; Gan, C.-Y.; Maqsood, S. Molecular binding mechanism and identification of novel anti-hypertensive and anti-inflammatory bioactive peptides from camel milk protein hydrolysates. LWT 2019, 112, 108193. [Google Scholar] [CrossRef]
- Nongonierma, A.B.; FitzGerald, R.J. Features of dipeptidyl peptidase IV (DPP-IV) inhibitory peptides from dietary proteins. J. Food Biochem. 2019, 43, e12451. [Google Scholar] [CrossRef] [Green Version]
- Ashraf, A.; Mudgil, P.; Palakkott, A.; Iratni, R.; Gan, C.Y.; Maqsood, S.; Ayoub, M.A. Molecular basis of the anti-diabetic properties of camel milk through profiling of its bioactive peptides on dipeptidyl peptidase IV (DPP-IV) and insulin receptor activity. J. Dairy Sci. 2021, 104, 61–77. [Google Scholar] [CrossRef]
- Abdulrahman, A.O.; Ismael, M.A.; Al-Hosaini, K.; Rame, C.; Al-Senaidy, A.M.; Dupont, J.; Ayoub, M.A. Differential Effects of Camel Milk on Insulin Receptor Signaling—Toward Understanding the Insulin-Like Properties of Camel Milk. Front. Endocrinol. 2016, 7, 4. [Google Scholar] [CrossRef] [Green Version]
- Mehaia, M.A.; Hablas, M.A.; Abdel-Rahman, K.M.; El-Mougy, S.A. Milk composition of Majaheim, Wadah and Hamra camels in Saudi Arabia. Food Chem. 1995, 52, 115–122. [Google Scholar] [CrossRef]
- Gayathri, G.A.; Mahalingam, G. Review on enhancement of glucose uptake and up-regulation of glucose transporters by antidiabetic medicinal plants. Asian J. Pharm. Clin. Res. 2016, 9, 34–39. [Google Scholar]
- Angel, J.; Sailesh, S.K.; Mukkadan, J.K. A study on Anti—Diabetic effect of peppermint in alloxan induced diabetic model of wistar rats. J. Clin. Biomed. Sci. 2013, 3, 177–181. [Google Scholar] [CrossRef]
- Awad, S.; El-Sayed, M.I.; Wahba, A.; El Attar, A.; Yousef, M.I.; Zedan, M. Antioxidant activity of milk protein hydrolysate in alloxan-induced diabetic rats. J. Dairy Sci. 2016, 99, 8499–8510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marjani, A. Lipid peroxidation alterations in type 2 diabetic patients. Pak. J. Biol. Sci. PJBS 2010, 13, 723–730. [Google Scholar] [CrossRef] [Green Version]
- Eidi, M.; Eidi, A.; Zamanizadeh, H. Effect of Salvia officinalis L. leaves on serum glucose and insulin in healthy and streptozotocin-induced diabetic rats. J. Ethnopharmacol. 2005, 100, 310–313. [Google Scholar] [CrossRef] [PubMed]
- Ejtahed, H.S.; Niasari Naslaji, A.; Mirmiran, P.; Zraif Yeganeh, M.; Hedayati, M.; Azizi, F.; Moosavi Movahedi, A. Effect of camel milk on blood sugar and lipid profile of patients with type 2 diabetes: A pilot clinical trial. Int. J. Endocrinol. Metab. 2015, 13, e21160. [Google Scholar] [CrossRef] [Green Version]
- Khattab, H.A.; Mohamed, R.A.; Hashemi, J.M. Evaluation of Hypoglycemic Activity of Salvia officinalis L. (Sage) Infusion on Streptozotocin-Induced Diabetic Rats. J. Am. Sci. 2012, 8, 411–416. [Google Scholar]
- Hernández-Saavedra, D.; Pérez Ramírez, I.; Ramos-Gómez, M.; Mendoza-Díaz, S.; Reynoso-Camacho, R. Phytochemical characterization and effect of Calendula officinalis, Hypericum perforatum, and Salvia officinalis infusions on obesity-associated cardiovascular risk. Med. Chem. Res. 2016, 25, 163–172. [Google Scholar] [CrossRef]
- Barbalho, S.M.; Damasceno, D.C.; Spada, A.P.; da Silva, V.S.; Martuchi, K.A.; Oshiiwa, M.; Machado, F.M.; Mendes, C.G. Metabolic Profile of Offspring from Diabetic Wistar Rats Treated with Mentha piperita (Peppermint). Evid.-Based Complement. Altern. Med. Ecam 2011, 2011, 430237. [Google Scholar] [CrossRef] [Green Version]
- Radovanović, B.C.; Radovanović, A.N.; Souquet, J.M. Phenolic profile and free radical-scavenging activity of Cabernet Sauvignon wines of different geographical origins from the Balkan region. J. Sci. Food Agric. 2010, 90, 2455–2461. [Google Scholar] [CrossRef] [PubMed]
- Belhadj, S.; Hentati, O.; Hammami, M.; Ben Hadj, A.; Boudawara, T.; Dammak, M.; Zouari, S.; El Feki, A. Metabolic impairments and tissue disorders in alloxan-induced diabetic rats are alleviated by Salvia officinalis L. essential oil. Biomed. Pharmacother. Biomed. Pharmacother. 2018, 108, 985–995. [Google Scholar] [CrossRef]
- Bouché, C.; Serdy, S.; Kahn, C.R.; Goldfine, A.B. The cellular fate of glucose and its relevance in type 2 diabetes. Endocr. Rev. 2004, 25, 807–830. [Google Scholar] [CrossRef]
- El-Sayed, M.I.; Awad, S.; Wahba, A.; El Attar, A.; Yousef, M.I.; Zedan, M. In Vivo Anti-diabetic and Biological Activities of Milk Protein and Milk Protein Hydrolyaste. Adv. Dairy Res. 2016, 4, 1–6. [Google Scholar] [CrossRef]
- Mohamad, R.H.; Zekry, Z.K.; Al-Mehdar, H.A.; Salama, O.; El-Shaieb, S.E.; El-Basmy, A.A.; Al-said, M.G.; Sharawy, S.M. Camel milk as an adjuvant therapy for the treatment of type 1 diabetes: Verification of a traditional ethnomedical practice. J. Med. Food 2009, 12, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, R.P.; Jain, S.; Shah, S.; Chopra, A.; Agarwal, V. Effect of camel milk on glycemic control and insulin requirement in patients with type 1 diabetes: 2-years randomized controlled trial. Eur. J. Clin. Nutr. 2011, 65, 1048–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Habori, M.; Al-Aghbari, A.; Al-Mamary, M.; Baker, M. Toxicological evaluation of Catha edulis leaves: A long term feeding experiment in animals. J. Ethnopharmacol. 2002, 83, 209–217. [Google Scholar] [CrossRef]
- Alsahli, M.; Gerich, J.E. Hypoglycemia in Patients with Diabetes and Renal Disease. J. Clin. Med. 2015, 4, 948–964. [Google Scholar] [CrossRef] [Green Version]
- Daniel, E.E.; Mohammed, A.; Tanko, Y.; Ahmed, A. Effect of Lycopene on Altered Kidney Antioxidant Enzymes Activity and Functions in Streptozotocin-Induced Diabetic Wistar Rats. Cell Biol. 2015, 3, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Trujillo, J.; Chirino, Y.I.; Molina-Jijón, E.; Andérica-Romero, A.C.; Tapia, E.; Pedraza-Chaverrí, J. Renoprotective effect of the antioxidant curcumin: Recent findings. Redox Biol. 2013, 1, 448–456. [Google Scholar] [CrossRef] [Green Version]
- Öztürk, H.İ.; Aydın, S.; Sözeri, D.; Demirci, T.; Sert, D.; Akın, N. Fortification of set-type yoghurts with Elaeagnus angustifolia L. flours: Effects on physicochemical, textural, and microstructural characteristics. Lwt Food Sci. Technol. 2018, 90, 620–626. [Google Scholar] [CrossRef]
- Association of Official Analytical Chemists; Association of Official Agricultural Chemists (US). Official Method of Analysis: Association of Analytical Chemists; Association of Official Analytical Chemists: Rockville, MD, USA, 2012; pp. 121–130. [Google Scholar]
- Singh, P.; Bajpai, V.; Khandelwal, N.; Varshney, S.; Gaikwad, A.N.; Srivastava, M.; Singh, B.; Kumar, B. Determination of bioactive compounds of Artemisia Spp. plant extracts by LC–MS/MS technique and their in-vitro anti-adipogenic activity screening. J. Pharm. Biomed. Anal. 2021, 193, 113707. [Google Scholar] [CrossRef]
- Abirami, A.; Nagarani, G.; Siddhuraju, P. In vitro antioxidant, anti-diabetic, cholinesterase and tyrosinase inhibitory potential of fresh juice from Citrus hystrix and C. maxima fruits. Food Sci. Hum. Wellness 2014, 3, 16–25. [Google Scholar] [CrossRef] [Green Version]
- Barros, L.; Cabrita, L.; Boas, M.V.; Carvalho, A.M.; Ferreira, I.C.F.R. Chemical, biochemical and electrochemical assays to evaluate phytochemicals and antioxidant activity of wild plants. Food Chem. 2011, 127, 1600–1608. [Google Scholar] [CrossRef]
- Lim, Y.; Quah, E.P.L. Antioxidant Properties of Different Cultivars of Portulaca oleracea. Food Chem. 2007, 103, 734–740. [Google Scholar] [CrossRef]
- Oyaizu, M. Studies on Products of Browning Reaction. Antioxidative Activities of Products of Browning Reaction Prepared from Glucosamine. Jpn. J. Nutr. Diet. 1986, 44, 307–315. [Google Scholar] [CrossRef] [Green Version]
- Association of Official Analytical Chemist. Official Methods of Analysis of Association of Official Analytical Chemistry, 18th ed.; AOAC International: Gaithersburg, MD, USA, 2005. [Google Scholar]
- Tamime, A.Y.; Robinson, R.K. Tamime and Robinson’s Yoghurt: Science and Technology, 3rd ed.; Woodhead Publishing Limited: Cambridge, UK, 2007; pp. 11–118. [Google Scholar]
- Desai, A.C.; Bhide, M.B. Hypoglycaemic activity of Hamiltonia suaveolens. Indian J. Med. Res. 1985, 81, 86–91. [Google Scholar] [PubMed]
- National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 1994, 28, 1039–1057. [Google Scholar]
- AIN. American Institute of Purified Diet for Laboratory Rodent, Final Report. J. Nutr. 1993, 123, 1939–1951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Althnaian, T.; Albokhadaim, I.; El-Bahr, S.M. Biochemical and histopathological study in rats intoxicated with carbontetrachloride and treated with camel milk. SpringerPlus 2013, 2, 57. [Google Scholar] [CrossRef] [Green Version]
- El-Demerdash, F.M.; Yousef, M.I.; El-Naga, N.I. Biochemical study on the hypoglycemic effects of onion and garlic in alloxan-induced diabetic rats. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2005, 43, 57–63. [Google Scholar] [CrossRef]
- Trinder, P. Determination of Glucose in Blood Using Glucose Oxidase with an Alternative Oxygen Acceptor. Ann. Clin. Biochem. 1969, 6, 24–27. [Google Scholar] [CrossRef]
- Chaney, A.L.; Marbach, E.P. Modified reagents for determination of urea and ammonia. Clin. Chem. 1962, 8, 130–132. [Google Scholar] [CrossRef] [PubMed]
- Searcy, R.L.; Reardon, J.E.; Foreman, J.A. A new photometric method for serum urea nitrogen determination. Am. J. Med. Technol. 1967, 33, 15–20. [Google Scholar] [PubMed]
- Tabacco, A.; Meiattini, F.; Moda, E.; Tarli, P. Simplified enzymic/colorimetric serum urea nitrogen determination. Clin. Chem. 1979, 25, 336–337. [Google Scholar] [CrossRef] [PubMed]
- Bartels, H.; Böhmer, M. Micro-determination of creatinine. Clin. Chim. Acta Int. J. Clin. Chem. 1971, 32, 81–85. [Google Scholar] [CrossRef]
- Fabiny, D.L.; Ertingshausen, G. Automated reaction-rate method for determination of serum creatinine with the CentrifiChem. Clin. Chem. 1971, 17, 696–700. [Google Scholar] [CrossRef] [PubMed]
- Bucolo, G.; David, H. Quantitative determination of serum triglycerides by the use of enzymes. Clin. Chem. 1973, 19, 476–482. [Google Scholar] [CrossRef]
- Fossati, P.; Prencipe, L. Serum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxide. Clin. Chem. 1982, 28, 2077–2080. [Google Scholar] [CrossRef] [PubMed]
- Meiattini, F.; Prencipe, L.; Bardelli, F.; Giannini, G.; Tarli, P. The 4-hydroxybenzoate/4-aminophenazone chromogenic system used in the enzymic determination of serum cholesterol. Clin. Chem. 1978, 24, 2161–2165. [Google Scholar] [CrossRef]
- Grove, T.H. Effect of reagent pH on determination of high-density lipoprotein cholesterol by precipitation with sodium phosphotungstate-magnesium. Clin. Chem. 1979, 25, 560–564. [Google Scholar] [CrossRef]
- Burstein, M.; Scholnick, H.R.; Morfin, R. Rapid method for the isolation of lipoproteins from human serum by precipitation with polyanions. J. Lipid Res. 1970, 11, 583–595. [Google Scholar] [CrossRef]
- Reitman, S.; Frankel, S. A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am. J. Clin. Pathol. 1957, 28, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Belfield, A.; Goldberg, D.M. Revised assay for serum phenyl phosphatase activity using 4-amino-antipyrine. Enzyme 1971, 12, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Abraham, E.C.; Huff, T.A.; Cope, N.D.; Wilson, J.B., Jr.; Bransome, E.D., Jr.; Huisman, T.H. Determination of the glycosylated hemoglobins (HB AI) with a new microcolumn procedure. Suitability of the technique for assessing the clinical management of diabetes mellitus. Diabetes 1978, 27, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.A.; Miles, L.E. Radioimmunoassay of Insulin in Handbook of Radio Immunoassay; Abraham, G.E., Ed.; Marcel Dekker Inc.: New York, NY, USA, 1977; p. 275. [Google Scholar]



| Composition% | Peppermint (Mentha peperita) Leaves Powder (%) | Sage (Salvia officinalis) Leaves Powder (%) |
|---|---|---|
| Ash | 21 | 7.12 |
| Crude | 9.4 | 26.23 |
| Lipids | 5.68 | 7.91 |
| Proteins | 7.6 | 8.73 |
| Carbohydrates | 56.32 | 50.01 |
| Property | Sage | Mint |
|---|---|---|
| DPPH (%) | 71.64 ± 3.45 a | 45.32 ± 3.45 b |
| FRAP (mg GAE/g) | 0.236 ± 0.008 b | 0.466 ± 0.041 a |
| Total phenolic (mg GA/g) | 7.35 ± 0.026 a | 6.60 ± 0.137 b |
| Total flavonoids (µg/mL) | 170.87 ± 4.04 b | 184.92 ± 4.96 a |
| N | RT | Compound | Mint Extract µg/g | Sage Extract µg/g |
|---|---|---|---|---|
| 1 | 7.35 | Chlorogenic acid | 40.07 | 155.47 |
| 2 | 12.9 | Daidzein | ND | ND |
| 3 | 3.89 | Gallic acid | 24.34 | 6.81 |
| 4 | 8.04 | Caffeic acid | 339.87 | 394.85 |
| 5 | 9.73 | Rutin | 25.47 | 0.15 |
| 6 | 9.53 | Coumaric acid | 15.43 | 36.12 |
| 7 | 9.5 | Vanillin | ND | 18.50 |
| 8 | 15.03 | Naringenin | 4933.35 | 2137.01 |
| 9 | 13.56 | Quercetin | 4.16 | 45.62 |
| 10 | 9.94 | Ellagic acid | 9.61 | 17.80 |
| 11 | 5.73 | 3.4-Dihydroxybenzoic acid | 123.53 | 54.87 |
| 12 | 15.57 | Hesperetin | 81.01 | 2.61 |
| 13 | 14.1 | Cinnamic acid | ND | ND |
| 14 | 7.42 | Methyl gallate | 0.10 | 0.08 |
| 15 | 15.33 | Kaempferol | 0.29 | 9.99 |
| 16 | 10.21 | Ferulic acid | 10.91 | 17.26 |
| 17 | 8.37 | Syringic acid | 20.13 | 33.89 |
| 18 | 15.03 | Apigenin | 38.16 | 107.64 |
| 19 | 7.35 | Catechin | ND | ND |
| 20 | 13.5 | Luteolin | 281.54 | 372.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahein, M.R.; El-Sayed, M.I.; Raya-Álvarez, E.; Elmeligy, A.A.; Hussein, M.A.M.; Mubaraki, M.A.; Agil, A.; Elmahallawy, E.K. Fortification of Fermented Camel Milk with Salvia officinalis L. or Mentha piperita Leaves Powder and Its Biological Effects on Diabetic Rats. Molecules 2023, 28, 5749. https://doi.org/10.3390/molecules28155749
Shahein MR, El-Sayed MI, Raya-Álvarez E, Elmeligy AA, Hussein MAM, Mubaraki MA, Agil A, Elmahallawy EK. Fortification of Fermented Camel Milk with Salvia officinalis L. or Mentha piperita Leaves Powder and Its Biological Effects on Diabetic Rats. Molecules. 2023; 28(15):5749. https://doi.org/10.3390/molecules28155749
Chicago/Turabian StyleShahein, Magdy Ramadan, Mahmoud Ibrahim El-Sayed, Enrique Raya-Álvarez, Abdelmoneim Ahmed Elmeligy, Mohamed A. Mohamady Hussein, Murad A. Mubaraki, Ahmad Agil, and Ehab Kotb Elmahallawy. 2023. "Fortification of Fermented Camel Milk with Salvia officinalis L. or Mentha piperita Leaves Powder and Its Biological Effects on Diabetic Rats" Molecules 28, no. 15: 5749. https://doi.org/10.3390/molecules28155749








