Molecular Characteristics of Methicillin-Resistant Staphylococcus epidermidis on the Abdominal Skin of Females before Laparotomy
Abstract
:1. Introduction
2. Results
2.1. SCCmec Typing of MRSE
2.2. Antimicrobial Susceptibility of MRSE
2.3. PFGE of MRSE
3. Discussion
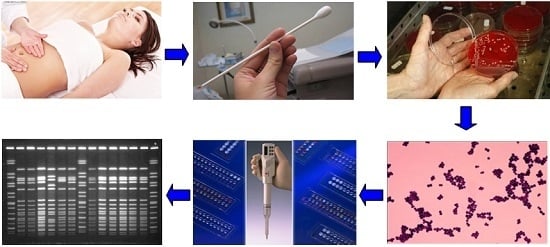
4. Materials and Methods
4.1. Specimen Collection
4.2. Bacterial Isolation
4.3. Detection of mecA, icaA Gene, and SCCmec Typing
4.4. Antimicrobial Susceptibility Testing
4.5. PFGE Typing
4.6. Quality Control
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| MRSE | methicillin-resistant Staphylococcus epidermidis |
| MSSE | methicillin-susceptible Staphylococcus epidermidis |
| SCCmec | staphylococcal cassette chromosome mec |
| PFGE | pulsed field gel electrophoresis |
| NT | non-typeable |
| SSIs | surgical site infections |
| MICs | minimal inhibitory concentrations |
References
- Suwal, A.; Shrivastava, V.R.; Giri, A. A prospective study of wound infections after laparotomy in obstetrics and gynaecology department. Nepal. Med. Coll. J. 2012, 14, 267–270. [Google Scholar] [PubMed]
- Shrestha, S.; Shrestha, R.; Shrestha, B.; Dongol, A. Incidence and risk factors of surgical site infection following cesarean section at Dhulikhel Hospital. Kathmandu Univ. Med. J. 2014, 12, 113–116. [Google Scholar] [CrossRef]
- Shahane, V.; Bhawal, S.; Lele, U. Surgical site infections: A one year prospective study in a tertiary care center. Int. J. Health Sci. 2012, 6, 79–84. [Google Scholar] [CrossRef]
- Altemeier, W.A.; Culbertson, W.R.; Hummel, R.P. Surgical considerations of endogenous infections—Sources, types, and methods of control. Surg. Clin. N. Am. 1968, 48, 227–240. [Google Scholar] [PubMed]
- Kleinschmidt, S.; Huygens, F.; Faoagali, J.; Rathnayake, I.U.; Hafner, L.M. Staphylococcus epidermidis as a cause of bacteremia. Future Microbiol. 2015, 10, 1859–1879. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, S.; Kakutani, K.; Maeno, K.; Takada, T.; Yurube, T.; Kurosaka, M.; Nishida, K. Surgical debridement with retention of spinal instrumentation and long-term antimicrobial therapy for multidrug-resistant surgical site infections after spinal surgery: A case series. Int. Orthop. 2015, in press. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Ahn, D.K.; Kim, J.W.; Kim, G.W. Particular features of surgical site infection in posterior lumbar interbody fusion. Clin. Orthop. Surg. 2015, 7, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Jabbar, A.; Berven, S.H.; Hu, S.S.; Chou, D.; Mummaneni, P.V.; Takemoto, S.; Ames, C.; Deviren, V.; Tay, B.; Weinstein, P.; et al. Surgical site infections in spine surgery: Identification of microbiologic and surgical characteristics in 239 cases. Spine (Phila Pa 1976) 2013, 38, E1425–E1431. [Google Scholar] [CrossRef] [PubMed]
- Martens, M.G.; Kolrud, B.L.; Faro, S.; Maccato, M.; Hammill, H. Development of wound infection or separation after cesarean delivery. Prospective evaluation of 2,431 cases. J. Reprod. Med. 1995, 40, 171–175. [Google Scholar] [PubMed]
- Diekema, D.J.; Pfaller, M.A.; Schmitz, F.J.; Smayevsky, J.; Bell, J.; Jones, R.N.; Beach, M. Survey of infections due to Staphylococcus species: Frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997–1999. Clin. Infect. Dis. 2001, 32, S114–S132. [Google Scholar] [PubMed]
- Wang, L.F.; Li, J.L.; Ma, W.H.; Li, J.Y. Drug resistance analysis of bacterial strains isolated from burn patients. Genet. Mol. Res. 2014, 13, 9727–9734. [Google Scholar] [CrossRef] [PubMed]
- Turlej, A.; Hryniewicz, W.; Empel, J. Staphylococcal cassette chromosome mec (Sccmec) classification and typing methods: An overview. Pol. J. Microbiol. 2011, 60, 95–103. [Google Scholar] [PubMed]
- Miragaia, M.; Couto, I.; de Lencastre, H. Genetic diversity among methicillin-resistant Staphylococcus epidermidis (MRSE). Microb. Drug Resist. 2005, 11, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Hanssen, A.M.; Sollid, J.U. Multiple staphylococcal cassette chromosomes and allelic variants of cassette chromosome recombinases in Staphylococcus aureus and coagulase-negative staphylococci from Norway. Antimicrob. Agents Chemother. 2007, 51, 1671–1677. [Google Scholar] [CrossRef] [PubMed]
- Miragaia, M.; Carriço, J.A.; Thomas, J.C.; Couto, I.; Enright, M.C.; de Lencastre, H. Comparison of molecular typing methods for characterization of Staphylococcus epidermidis: Proposal for clone definition. J. Clin. Microbiol. 2008, 46, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Ibrahem, S.; Salmenlinna, S.; Virolainen, A.; Kerttula, A.M.; Lyytikäinen, O.; Jägerroos, H.; Broas, M.; Vuopio-Varkila, J. Carriage of methicillin-resistant Staphylococci and their SCCmec types in a long-term-care facility. J. Clin. Microbiol. 2009, 47, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Urbaniak, C.; Cummins, J.; Brackstone, M.; Macklaim, J.M.; Gloor, G.B.; Baban, C.K.; Scott, L.; O’Hanlon, D.M.; Burton, J.P.; Francis, K.P.; et al. Bacteria microbiota of human breast tissue. Appl. Environ. Microbiol. 2014, 80, 3007–3014. [Google Scholar] [CrossRef] [PubMed]
- Tomic-Canic, M.; Perez-Perez, G.I.; Blumenberg, M. Cutaneous microbiome studies in the times of affordable sequencing. J. Dermatol. Sci. 2014, 75, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Whiteside, S.A.; Razvi, H.; Dave, S.; Reid, G.; Burton, J.P. The microbiome of the urinary tract—A role beyond infection. Nat. Rev. Urol. 2015, 12, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Szumała-Kakol, A.; Szymanowski, K.; Owedyk, M.; Banaszewski, S.; Skrzypczak, J. Microbiological flora cultured from peritoneal fluid of women in reproductive age. Ginekol. Pol. 2000, 71, 1026–1030. [Google Scholar] [PubMed]
- Hanssen, A.M.; Kjeldsen, G.; Sollid, J.U. Local variants of Staphylococcal cassette chromosome mec in sporadic methicillin-resistant staphylococcus aureus and methicillin-resistant coagulase-negative Staphylococci: Evidence of horizontal gene transfer? Antimicrob. Agents Chemother. 2004, 48, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Barbier, F.; Ruppé, E.; Hernandez, D.; Lebeaux, D.; Francois, P.; Felix, B.; Desprez, A.; Maiga, A.; Woerther, P.L.; Gaillard, K.; et al. Methicillin-resistant coagulase-negative staphylococci in the community: High homology of SCCmec IVa between staphylococcus epidermidis and major clones of methicillin-resistant staphylococcus aureus. J. Infect. Dis. 2010, 202, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Otto, M. Coagulase-negative staphylococci as reservoirs of genes facilitating MRSA infection: Staphylococcal commensal species such as staphylococcus epidermidis are being recognized as important sources of genes promoting MRSA colonization and virulence. Bioessays 2013, 35, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.L.; Wang, J.T.; Chen, S.Y.; Chen, Y.C.; Chang, S.C. Distribution of staphylococcal cassette chromosome mec Types and correlation with comorbidity and infection type in patients with MRSA bacteremia. PLoS ONE 2010, 5, e9489. [Google Scholar] [CrossRef] [PubMed]
- Jamaluddin, T.Z.; Kuwahara-Arai, K.; Hisata, K.; Terasawa, M.; Cui, L.; Baba, T.; Sotozono, C.; Kinoshita, S.; Ito, T.; Hiramatsu, K. Extreme genetic diversity of methicillin-resistant staphylococcus epidermidis strains disseminated among healthy Japanese children. J. Clin. Microbiol. 2008, 46, 3778–3783. [Google Scholar] [CrossRef] [PubMed]
- Wisplinghoff, H.; Rosato, A.E.; Enright, M.C.; Noto, M.; Craig, W.; Archer, G.L. Related clones containing SCCmec type IV predominate among clinically significant Staphylococcus epidermidis isolates. Antimicrob. Agents Chemother. 2003, 47, 3574–3579. [Google Scholar] [CrossRef] [PubMed]
- Al-Bakri, A.G.; Al-Hadithi, H.; Kasabri, V.; Othman, G.; Kriegeskorte, A.; Becker, K. The epidemiology and molecular characterization of methicillin-resistant staphylococci sampled from a healthy Jordanian population. Epidemiol. Infect. 2013, 141, 2384–2391. [Google Scholar] [CrossRef] [PubMed]
- Shitrit, P.; Openhaim, M.; Reisfeld, S.; Paitan, Y.; Regev-Yochay, G.; Carmeli, Y.; Chowers, M. Characteristics of SCCmec IV and V Methicillin-Resistant Staphylococcus aureus (MRSA) in Israel. Isr. Med. Assoc. J. 2015, 17, 470–475. [Google Scholar] [PubMed]
- Zong, Z.; Peng, C.; Lü, X. Diversity of SCCmec elements in methicillin-resistant coagulase-negative staphylococci clinical isolates. PLoS ONE 2011, 6, e20191. [Google Scholar] [CrossRef] [PubMed]
- Bukharie, H.A. A review of community-acquired methicillin-resistant staphylococcus aureus for primary care physicians. J. Family Community Med. 2010, 17, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; McClure, J.A.; Elsayed, S.; Louie, T.; Conly, J.M. Novel multiplex PCR assay for characterization and concomitant subtyping of staphylococcal cassette chromosome mec types I to V in methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 2005, 43, 5026–5033. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- McDougal, L.K.; Steward, C.D.; Killgore, G.E.; Chaitram, J.M.; McAllister, S.K.; Tenover, F.C. Pulsed-field gel electrophoresis typing of oxacillin-resistant staphylococcus aureus isolates from the united states: Establishing a national database. J. Clin. Microbiol. 2003, 41, 5113–5120. [Google Scholar] [CrossRef] [PubMed]

| Antibiotics | MSSE (n = 103) | MRSE (n = 54) | MIC Range | ||||
|---|---|---|---|---|---|---|---|
| %R(n) | MIC50 | MIC90 | %R(n) | MIC50 | MIC90 | ||
| Penicillin G | 85.4(88) | 16 | 16 | 96.3(52) | 16 | 16 | 0.03–16 |
| Ampicillin | 84.5(87) | 16 | 16 | 96.3(52) | 16 | 16 | 0.25–16 |
| Oxacillin | 0(0) | 0.25 | 0.25 | 90.7(49) | 4 | 4 | 0.25–4 |
| Gentamicin | 4.9(5) | 4 | 4 | 14.8(8) | 4 | 16 | 4–16 |
| Rifampin | 0(0) | 1 | 1 | 0(0) | 1 | 1 | 1–1 |
| Ciprofloxacin | 3.9(4) | 1 | 1 | 29.6(16) | 1 | 4 | 1–4 |
| Gatifloxacin | 0(0) | 2 | 2 | 0(0) | 2 | 2 | 2–2 |
| Levofloxacin | 2.9(3) | 2 | 2 | 31.5(17) | 2 | 8 | 2–8 |
| Moxifloxacin | 0(0) | 2 | 2 | 0(0) | 2 | 2 | 2–2 |
| Trimethoprim/Sulfamethoxazole | 25.2(26) | 2 | 4 | 59.3(32) | 4 | 4 | 2–4 |
| Clindamycin | 12.6(13) | 0.5 | 2 | 14.8(8) | 0.5 | 4 | 0.5–4 |
| Azithromycin | 38.8(40) | 2 | 8 | 64.8(35) | 8 | 8 | 2–8 |
| Erythromycin | 47.6(49) | 0.5 | 8 | 68.5(37) | 8 | 8 | 0.5–8 |
| Linezolid | 0(0) | 2 | 2 | 0(0) | 2 | 2 | 2–4 |
| Vancomycin | 0(0) | 2 | 2 | 0(0) | 2 | 4 | 2–16 |
| Chloramphenicol | 7.8(8) | 8 | 8 | 11.1(6) | 8 | 32 | 8–32 |
| Quinupristin/Dalfopristin | 0(0) | 1 | 1 | 0(0) | 1 | 1 | 1–1 |
| Tetracycline | 7.8(8) | 4 | 4 | 9.3(5) | 4 | 4 | 4–16 |
| Antibiotics | Resistant Isolates of SCCmec Type [% (n)] | ||||||
|---|---|---|---|---|---|---|---|
| I (n = 1) | II + IVb (n = 1) | III (n = 4) | Iva (n = 28) | IVd (n = 3) | V (n = 3) | NT (n = 14) | |
| Penicillin G | 100(1) | 100(1) | 100(4) | 96.4(27) | 66.7(2) | 100(3) | 100(14) |
| Ampicillin | 100(1) | 100(1) | 100(4) | 96.4(27) | 66.7(2) | 100(3) | 100(14) |
| Oxacillin | 100(1) | 100(1) | 75(3) | 89.3(25) | 66.7(2) | 100(3) | 100(14) |
| Gentamicin | 100(1) | 0(0) | 0(0) | 10.7(3) | 33.3(1) | 0(0) | 21.4(3) |
| Rifampin | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) |
| Ciprofloxacin | 0(0) | 100(1) | 50(2) | 21.4(6) | 0(0) | 66.7(2) | 35.7(5) |
| Gatifloxacin | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) |
| Levofloxacin | 0(0) | 100(1) | 50.0(2) | 25.0(7) | 0(0) | 66.7(2) | 35.7(5) |
| Moxifloxacin | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) |
| Trimethoprim/Sulfamethoxazole | 0(0) | 100(1) | 25(1) | 67.9(19) | 66.7(2) | 100(3) | 42.9(6) |
| Clindamycin | 0(0) | 0(0) | 25(1) | 7.1(2) | 0(0) | 0(0) | 35.7(5) |
| Azithromycin | 100(1) | 100(1) | 25(1) | 60.7(17) | 66.7(2) | 66.7(2) | 78.6(11) |
| Erythromycin | 100(1) | 100(1) | 25(1) | 67.9(19) | 66.7(2) | 66.7(2) | 78.6(11) |
| Linezolid | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) |
| Vancomycin | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) |
| Chloramphenicol | 0(0) | 0(0) | 0(0) | 7.1(2) | 0(0) | 0(0) | 28.6(4) |
| Quinupristin/Dalfopristin | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) | 0(0) |
| Tetracycline | 0(0) | 100(1) | 25(1) | 7.1(2) | 0(0) | 0(0) | 7.1(1) |
| Resistance Patterns | No. of Isol. | % Isol. | SCCmec Type (n) | PFGE Type (n) |
|---|---|---|---|---|
| ERY | 2 | 3.7 | IVa(2) | 9(2) |
| SXT | 1 | 1.9 | IVa(1) | 17(1) |
| OXA | 4 | 7.4 | III(1), IVa(1), IVd(1), NT(1) | 1(4) |
| SXT + ERY | 1 | 1.9 | IVd(1) | 1(1) |
| SXT + CIP | 1 | 1.9 | III(1) | 25(1) |
| OXA + TCY | 1 | 1.9 | III(1) | 28(1) |
| OXA + CHL | 1 | 1.9 | NT(1) | 13(1) |
| OXA + ERY | 3 | 5.6 | IVa(1), NT(2) | 16(1), 19(2) |
| OXA + CLI | 2 | 3.7 | IVa(2) | 1(1), 12(1) |
| OXA + SXT | 3 | 5.6 | IVa(3) | 20(1), 23(1), 24(1) |
| OXA + GEN | 1 | 1.9 | IVa(1) | 12(1) |
| OXA + CLI + ERY | 1 | 1.9 | NT(1) | 1(1) |
| OXA + SXT + CHL | 1 | 1.9 | IVa(1) | 17(1) |
| OXA + SXT + ERY | 6 | 11.1 | IVa(5), V(1) | 7(1),9(1),15(1), 7(1), 18(1), 19(1) |
| OXA + CIP + ERY | 1 | 1.9 | IVa(1) | 22(1) |
| OXA + CIP + SXT | 1 | 1.9 | V(1) | 1(1) |
| OXA + GEN + ERY | 1 | 1.9 | I(1) | 12(1) |
| OXA + CLI + ERY + CHL | 3 | 5.6 | NT(3) | 1(3) |
| OXA + SXT + ERY + TCY | 2 | 3.7 | IVa(2) | 11(1), 17(1) |
| OXA + SXT + ERY + CHL | 1 | 1.9 | IVa(1) | 15(1) |
| OXA +SXT + CLI + ERY | 2 | 3.7 | IVa(1), NT(1) | 15(1), 29(1) |
| OXA + CIP + CLI + ERY | 2 | 3.7 | IVa(1), III(1) | 2(1), 10(1) |
| OXA + CIP + SXT + ERY | 5 | 9.3 | IVa(2),V(1), NT(2) | 1(2),8(1),14(1), 26(1) |
| OXA + GEN + SXT + ERY | 1 | 1.9 | IVd(1) | 5(1) |
| OXA + GEN + CIP + SXT | 1 | 1.9 | NT(1) | 3(1) |
| OXA + CIP + SXT + ERY + TCY | 1 | 1.9 | IVb/II(1) | 11(1) |
| OXA + CIP + SXT + CLI + ERY | 1 | 1.9 | IVa(1) | 21(1) |
| OXA + GEN + CIP + SXT + ERY | 2 | 3.7 | IVa(2) | 6(1), 27(1) |
| OXA + GEN + CIP + SXT + ERY + CHL | 1 | 1.9 | NT(1) | 3(1) |
| OXA + GEN + CIP + SXT + ERY + CHL + TCY | 1 | 1.9 | NT(1) | 4(1) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, P.-J.; Xie, C.-B.; Sun, F.-H.; Guo, L.-J.; Dai, M.; Cheng, X.; Ma, Y.-X. Molecular Characteristics of Methicillin-Resistant Staphylococcus epidermidis on the Abdominal Skin of Females before Laparotomy. Int. J. Mol. Sci. 2016, 17, 992. https://doi.org/10.3390/ijms17060992
Wang P-J, Xie C-B, Sun F-H, Guo L-J, Dai M, Cheng X, Ma Y-X. Molecular Characteristics of Methicillin-Resistant Staphylococcus epidermidis on the Abdominal Skin of Females before Laparotomy. International Journal of Molecular Sciences. 2016; 17(6):992. https://doi.org/10.3390/ijms17060992
Chicago/Turabian StyleWang, Pin-Jia, Cheng-Bin Xie, Feng-Hui Sun, Li-Juan Guo, Min Dai, Xi Cheng, and Yong-Xin Ma. 2016. "Molecular Characteristics of Methicillin-Resistant Staphylococcus epidermidis on the Abdominal Skin of Females before Laparotomy" International Journal of Molecular Sciences 17, no. 6: 992. https://doi.org/10.3390/ijms17060992
APA StyleWang, P. -J., Xie, C. -B., Sun, F. -H., Guo, L. -J., Dai, M., Cheng, X., & Ma, Y. -X. (2016). Molecular Characteristics of Methicillin-Resistant Staphylococcus epidermidis on the Abdominal Skin of Females before Laparotomy. International Journal of Molecular Sciences, 17(6), 992. https://doi.org/10.3390/ijms17060992