Linear and Non-Linear Optical Imaging of Cancer Cells with Silicon Nanoparticles
Abstract
:1. Introduction
2. Results
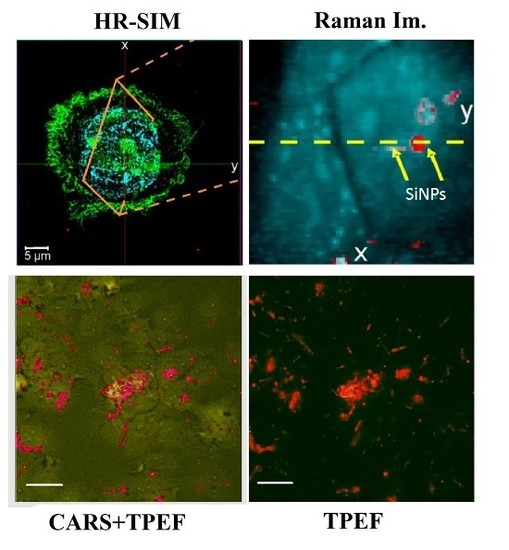
3. Discussion
4. Materials and Methods
4.1. Nanoparticle Formation
4.2. Analysis of SiNPs
4.3. Cell Cultivation and Sample Preparation
4.4. High-Resolution Structured Illumination Microscopy
4.5. Micro-Raman Spectroscopy
4.6. Two-Photon Excited Fluorescence and Coherent Anti-Stokes Raman Scattering
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Low, S.P.; Voelcker, D.N.H. Biocompatibility of porous silicon. In Handbook of Porous Silicon; Canham, L.T., Ed.; Springer International Publishing: Cham, Switzerland, 2014; pp. 1–13. [Google Scholar]
- Shabir, Q. Biodegradability of porous silicon. In Handbook of Porous Silicon; Canham, L.T., Ed.; Springer International Publishing: Cham, Switzerland, 2014; pp. 395–401. [Google Scholar]
- Santos, H.A. Porous Silicon for Biomedical Applications, 1st ed.; Santos, H.A., Ed.; Woodhead Publishing: Philadelphia, PA, USA, 2014. [Google Scholar]
- Erogbogbo, F.; Chang, C.-W.; May, J.L.; Liu, L.; Kumar, R.; Law, W.-C.; Ding, H.; Yong, K.T.; Roy, I.; Sheshadri, M.; et al. Bioconjugation of luminescent silicon quantum dots to gadolinium ions for bioimaging applications. Nanoscale 2012, 4, 5483. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.F.; Ruckenstein, E. Water-soluble poly(acrylic acid) grafted luminescent silicon nanoparticles and their use as fluorescent biological staining labels. Nano Lett. 2004, 4, 1463–1467. [Google Scholar] [CrossRef]
- Salonen, J. Drug delivery with porous silicon. In Handbook of Porous Silicon; Canham, L.T., Ed.; Springer International Publishing: Cham, Switzerland, 2014; pp. 909–919. [Google Scholar]
- Santos, H.A.; Mäkilä, E.; Airaksinen, A.J.; Bimbo, L.M.; Hirvonen, J. Porous silicon nanoparticles for nanomedicine: Preparation and biomedical applications. Nanomedicine 2014, 9, 535–554. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Gu, L.; von Maltzahn, G.; Ruoslahti, E.; Bhatia, S.N.; Sailor, M.J. Biodegradable luminescent porous silicon nanoparticles for in vivo applications. Nat. Mater. 2009, 8, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Anglin, E.J.; Cheng, L.; Freeman, W.R.; Sailor, M.J. Porous silicon in drug delivery devices and materials. Adv. Drug Deliv. Rev. 2008, 60, 1266–1277. [Google Scholar] [CrossRef] [PubMed]
- Osminkina, L.; Tamarov, K.P.; Sviridov, A.P.; Galkin, R.; Gongalsky, M.B.; Solovyev, V.V.; Kudryavtsev, A.; Timoshenko, V.Y. Photoluminescent biocompatible silicon nanoparticles for cancer theranostic applications. J. Biophotonics 2012, 5, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Tamarov, K.P.; Osminkina, L.; Zinovyev, S.V.; Maximova, K.; Kargina, J.V.; Gongalsky, M.B.; Ryabchikov, Y.; Al-Kattan, A.; Sviridov, A.P.; Sentis, M.; et al. Radio frequency radiation-induced hyperthermia using Si nanoparticle-based sensitizers for mild cancer therapy. Sci. Rep. 2014, 4, 7034. [Google Scholar] [CrossRef] [PubMed]
- Gongalsky, M.B.; Osminkina, L.A.; Pereira, A.; Manankov, A.A.; Fedorenko, A.A. Laser-synthesized oxide-passivated bright Si quantum dots for bioimaging. Sci. Rep. 2016, 6, 24732. [Google Scholar] [CrossRef] [PubMed]
- Pi, X.D.; Liptak, R.W.; Deneen Nowak, J.; Wells, N.P.; Carter, C.B.; Campbell, S.; Kortshagen, U. Air-stable full-visible-spectrum emission from silicon nanocrystals synthesized by an all-gas-phase plasma approach. Nanotechnology 2008, 19, 245603. [Google Scholar] [CrossRef] [PubMed]
- Canham, L.T. Silicon quantum wire array fabrication by electrochemical and chemical dissolution of wafers. Appl. Phys. Lett. 1990, 57, 1046–1048. [Google Scholar] [CrossRef]
- Osminkina, L.A.; Sivakov, V.A.; Mysov, G.A.; Georgobiani, V.A.; Natashina, U.А.; Talkenberg, F.; Solovyev, V.V.; Kudryavtsev, A.A.; Timoshenko, V.Y. Nanoparticles prepared from porous silicon nanowires for bio-imaging and sonodynamic therapy. Nanoscale Res. Lett. 2014, 9, 463. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Su, Y. Silicon Nano-Biotechnology; Springer Berlin Heidelberg: Berlin, Germany, 2014. [Google Scholar]
- Tolstik, E.; Osminkina, L.A.; Matthäus, C.; Burkhardt, M.; Tsurikov, K.E.; Natashina, U.A.; Timoshenko, V.Y.; Heintzmann, R.; Popp, J.; Sivakov, V. Studies of silicon nanoparticles uptake and biodegradation in cancer cells by Raman spectroscopy. Nanomed. Nanotechnol. Biol. Med. 2016. [Google Scholar] [CrossRef] [PubMed]
- Chernenko, T.; Matthäus, C.; Milane, L.; Quintero, L.; Amiji, M.; Diem, M. Label-free Raman spectral imaging of intracellular delivery and degradation of polymeric nanoparticle systems. ACS Nano 2009, 3, 3552–3559. [Google Scholar] [CrossRef] [PubMed]
- Matthäus, C.; Chernenko, T.; Quintero, L. Confocal Raman Microscopy; Dieing, T., Hollricher, O., Toporski, J., Eds.; Springer Berlin Heidelberg: Berlin, Germany, 2011. [Google Scholar]
- Neugebauer, U.; Clement, J.H.; Bocklitz, T.; Krafft, C.; Popp, J. Identification and differentiation of single cells from peripheral blood by Raman spectroscopic imaging. J. Biophotonics 2010, 3, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, G.; Tiwari, R.; Sriwastawa, B.; Bhati, L.; Pandey, S.; Pandey, P.; Bannerjee, S.K. Drug delivery systems: An updated review. Int. J. Pharm. Investig. 2012, 2, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Gordon, K.C.; McGoverin, C.M. Raman mapping of pharmaceuticals. Int. J. Pharm. 2011, 417, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.H.; Kim, K.H.; Park, J.S.; Jeong, S.H.; Park, K. Evaluation of drug delivery profiles in geometric three-layered tablets with various mechanical properties, in vitro-in vivo drug release, and Raman imaging. J. Control. Release 2013, 172, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Tolstik, T.; Marquardt, C.; Beleites, C.; Matthäus, C.; Bielecki, C.; Bürger, M.; Krafft, C.; Dirsch, O.; Settmacher, U.; Popp, J.; et al. Classification and prediction of HCC tissues by Raman imaging with identification of fatty acids as potential lipid biomarkers. J. Cancer Res. Clin. Oncol. 2015, 141, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Cicchi, R.; Cosci, A.; Rossari, S.; Kapsokalyvas, D.; Baria, E.; Maio, V.; Massi, D.; de Giorgi, V.; Pimpinelli, N.; Saverio Pavone, F. Combined fluorescence-Raman spectroscopic setup for the diagnosis of melanocytic lesions. J. Biophotonics 2014, 7, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Sćepanović, O.R.; Volynskaya, Z.; Kong, C.-R.; Galindo, L.H.; Dasari, R.R.; Feld, M.S. A multimodal spectroscopy system for real-time disease diagnosis. Rev. Sci. Instrum. 2009, 80, 43103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bräutigam, K.; Bocklitz, T.; Silge, A.; Dierker, C.; Ossig, R.; Schnekenburger, J.; Cialla, D.; Rösch, P.; Popp, J. Comparative two- and three-dimensional analysis of nanoparticle localization in different cell types by Raman spectroscopic imaging. J. Mol. Struct. 2014, 1073, 44–50. [Google Scholar] [CrossRef]
- Silge, A.; Bräutigam, K.; Bocklitz, T.; Rösch, P.; Vennemann, A.; Schmitz, I.; Popp, J.; Wiemann, M. ZrO2 nanoparticles labeled via a native protein corona: Detection by fluorescence microscopy and Raman microspectroscopy in rat lungs. Analyst 2015, 140, 5120–5118. [Google Scholar] [CrossRef] [PubMed]
- Gong, X.; Lu, W.; Paau, M.C.; Hu, Q.; Wu, X.; Shuang, S.; Dong, C.; Choi, M.M.F. Facile synthesis of nitrogen-doped carbon dots for Fe3+ sensing and cellular imaging. Anal. Chim. Acta 2015, 861, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Jia, F.; Liu, X.; Li, L.; Mallapragada, S.; Narasimhan, B.; Wang, Q. Multifunctional nanoparticles for targeted delivery of immune activating and cancer therapeutic agents. J. Control. Release 2013, 172, 1020–1034. [Google Scholar] [CrossRef] [PubMed]
- Jiang, K.; Sun, S.; Zhang, L.; Lu, Y.; Wu, A.; Cai, C.; Lin, H. Red, green, and blue luminescence by carbon dots: Full-color emission tuning and multicolor cellular imaging. Angew. Chem. Int. Ed. 2015, 54, 5360–5363. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Liu, X.; Wang, G.; Li, M.; Bratlie, K.M.; Cochran, E.; Wang, Q. Polymeric multifunctional nanomaterials for theranostics. J. Mater. Chem. B 2015, 3, 6856–6870. [Google Scholar] [CrossRef]
- Sharma, P.; Brown, S.; Walter, G.; Santra, S.; Moudgil, B. Nanoparticles for bioimaging. Adv. Colloid Interface Sci. 2006, 123–126, 471–485. [Google Scholar] [CrossRef] [PubMed]
- Miki, K.; Kimura, A.; Inoue, T.; Matsuoka, H.; Harada, H.; Hiraoka, M.; Ohe, K. Synthesis of biocompatible polysaccharide analogues and their application to in vivo optical tumor imaging. Bull. Chem. Soc. Jpn. 2015, 88, 792–803. [Google Scholar] [CrossRef]
- Wang, Q.; Cheng, H.; Peng, H.; Zhou, H.; Li, P.Y.; Langer, R. Non-genetic engineering of cells for drug delivery and cell-based therapy. Adv. Drug Deliv. Rev. 2015, 91, 125–140. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Deng, H.; Peng, H.; Wang, Q. Functional nanoparticles in targeting glioma diagnosis and therapies. J. Nanosci. Nanotechnol. 2014, 14, 415–432. [Google Scholar] [CrossRef] [PubMed]
- Yue, S.; Slipchenko, M.N.; Cheng, J.-X. Multimodal nonlinear optical microscopy. Laser Photonics Rev. 2011, 5. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.S.; Cheng, J.; Potma, E. Coherent anti-Stokes Raman scattering microscopy. In Handbook Of Biological Confocal Microscopy; Springer US: New York, NY, USA, 2006; pp. 595–606. [Google Scholar]
- Tolles, W.M.; Nibler, J.W.; McDonald, J.R.; Harvey, A.B. A Review of the Theory and Application of Coherent Anti-Stokes Raman Spectroscopy (CARS). Appl. Spectrosc. 1977, 31, 253–271. [Google Scholar] [CrossRef]
- Denk, W.; Strickler, J.; Webb, W. Two-photon laser scanning fluorescence microscopy. Science 1990, 248, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T.; Dietzek, B.; Krafft, C.; Romeike, B.F.M.; Reichart, R.; Kalff, R.; Popp, J. Nonlinear optical imaging: Toward chemical imaging during neurosurgery. In SPIE BiOS; International Society for Optics and Photonics: Bellingham, WA, USA, 2011; p. 78833W. [Google Scholar]
- Krafft, C.; Ramoji, A.A.; Bielecki, C.; Vogler, N.; Meyer, T.; Akimov, D.; Rösch, P.; Schmitt, M.; Dietzek, B.; Petersen, I.; et al. A comparative Raman and CARS imaging study of colon tissue. J. Biophotonics 2009, 2, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Handbook of Biomedical Nonlinear Optical Microscopy. Available online: http://www.amazon.com/Handbook-Biomedical-Nonlinear-Optical-Microscopy/dp/B005M4K62Q (accessed on 13 May 2016).
- Helmchen, F.; Denk, W. Deep tissue two-photon microscopy. Nat. Methods 2005, 2, 932–40. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T.; Guntinas-Lichius, O.; von Eggeling, F.; Ernst, G.; Akimov, D.; Schmitt, M.; Dietzek, B.; Popp, J. Multimodal nonlinear microscopic investigations on head and neck squamous cell carcinoma: Toward intraoperative imaging. Head Neck 2013, 35, E280–E287. [Google Scholar] [CrossRef] [PubMed]
- Moger, J.; Johnston, B.D.; Tyler, C.R. Imaging metal oxide nanoparticles in biological structures with CARS microscopy. Opt. Express 2008, 16, 3408. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Chen, H.; Tong, L.; Cheng, J.-X. Imaging gold nanorods by plasmon-resonance-enhanced four wave mixing. J. Phys. Chem. C 2009, 113, 2657–2663. [Google Scholar] [CrossRef]
- Baltog, I.; Baibarac, M.; Lefrant, S. Coherent anti-Stokes Raman scattering on single-walled carbon nanotubes and copper phthalocyanine thin films excited through surface plasmons. J. Opt. Pure Appl. Opt. 2005, 7, 632–639. [Google Scholar] [CrossRef]
- Baltog, I.; Baibarac, M.; Lefrant, S. Coherent anti-Stokes Raman scattering on single-walled carbon nanotube thin films excited through surface plasmons. Phys. Rev. B 2005, 72, 245402. [Google Scholar] [CrossRef]
- Baltog, I.; Baibarac, M.; Mihut, L.; Lefrant, S. Abnormal anti-Stokes Raman spectra of single walled carbon nanotubes raised from coherent anti-Stokes Raman scattering and optical cooling processes. Dig. J. Nanomater. Biostruct. 2007, 2, 185–198. [Google Scholar]
- Li, J.-L.; Bao, H.-C.; Hou, X.-L.; Sun, L.; Wang, X.-G.; Gu, M. Graphene oxide nanoparticles as a nonbleaching optical probe for two-photon luminescence imaging and cell therapy. Angew. Chem. Int. Ed. Engl. 2012, 51, 1830–1834. [Google Scholar] [CrossRef] [PubMed]
- Garrett, N.; Whiteman, M.; Moger, J. Imaging the uptake of gold nanoshells in live cells using plasmon resonance enhanced four wave mixing microscopy. Opt. Express 2011, 19, 17563–17574. [Google Scholar] [CrossRef] [PubMed]
- Garrett, N.L.; Lalatsa, A.; Uchegbu, I.; Schätzlein, A.; Moger, J. Exploring uptake mechanisms of oral nanomedicines using multimodal nonlinear optical microscopy. J. Biophotonics 2012, 5, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Rago, G.; Bauer, B.; Svedberg, F.; Gunnarsson, L.; Ericson, M.B.; Bonn, M.; Enejder, A. Uptake of gold nanoparticles in healthy and tumor cells visualized by nonlinear optical microscopy. J. Phys. Chem. B 2011, 115, 5008–5016. [Google Scholar] [CrossRef] [PubMed]
- Larson, D.R.; Zipfel, W.R.; Williams, R.M.; Clark, S.W.; Bruchez, M.P.; Wise, F.W.; Webb, W.W. Water-soluble quantum dots for multiphoton fluorescence imaging in vivo. Science 2003, 300, 1434–1436. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Wang, X.; Meziani, M.J.; Lu, F.; Wang, H.; Luo, P.G.; Lin, Y.; Harruff, B.A.; Veca, L.M.; Murray, D.; et al. Carbon dots for multiphoton bioimaging. J. Am. Chem. Soc. 2007, 129, 11318–11319. [Google Scholar] [CrossRef] [PubMed]
- Nonlinear Optical Properties of Silicon Carbide (SiC) Nanoparticles by Carbothermal Reduction. Available online: http://adsabs.harvard.edu/abs/2016SPIE.9722E..13R (accessed on 14 July 2016).
- Kachynski, A.V.; Kuzmin, A.N.; Nyk, M.; Roy, I.; Prasad, P.N. Zinc oxide nanocrystals for nonresonant nonlinear optical microscopy in biology and medicine. J. Phys. Chem. C 2008, 112, 10721–10724. [Google Scholar] [CrossRef] [PubMed]
- Durr, N.J.; Larson, T.; Smith, D.K.; Korgel, B.A.; Sokolov, K.; Ben-Yakar, A. Two-photon luminescence imaging of cancer cells using molecularly targeted gold nanorods. Nano Lett. 2007, 7, 941–945. [Google Scholar] [CrossRef] [PubMed]
- Tu, C.; Ma, X.; Pantazis, P.; Kauzlarich, S.M.; Angelique, Y. Paramagnetic, silicon quantum dots for magnetic resonance and two photon imaging of macrophages. J. Am. Chem. Soc. 2016, 132, 2016–2023. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Tong, L.; Tanaudommongkon, A.; Cheng, J.-X.; Yang, C. In vitro and in vivo nonlinear optical imaging of silicon nanowires. Nano Lett. 2009, 9, 2440–2444. [Google Scholar] [CrossRef] [PubMed]
- Golovan, L.A.; Gonchar, K.A.; Osminkina, L.A.; Timoshenko, V.Y.; Petrov, G.I.; Yakovlev, V.V. Coherent anti-Stokes Raman scattering in silicon nanowire ensembles. Laser Phys. Lett. 2012, 9, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Pliss, A.; Kuzmin, A.N.; Kachynski, A.V.; Prasad, P.N. Nonlinear optical imaging and Raman microspectrometry of the cell nucleus throughout the cell cycle. Biophys. J. 2010, 99, 3483–3491. [Google Scholar] [CrossRef] [PubMed]
- Vogler, N.; Medyukhina, A.; Latka, I.; Kemper, S.; Böhm, M.; Dietzek, B.; Popp, J. Towards multimodal nonlinear optical tomography - experimental methodology. Laser Phys. Lett. 2011, 8, 617–624. [Google Scholar] [CrossRef]
- König, K.; Breunig, H.G.; Bückle, R.; Kellner-Höfer, M.; Weinigel, M.; Büttner, E.; Sterry, W.; Lademann, J. Optical skin biopsies by clinical CARS and multiphoton fluorescence/SHG tomography. Laser Phys. Lett. 2011, 8, 465–468. [Google Scholar] [CrossRef]
- Heuke, S.; Vogler, N.; Meyer, T.; Akimov, D.; Kluschke, F.; Röwert-Huber, H.-J.; Lademann, J.; Dietzek, B.; Popp, J. Detection and discrimination of non-melanoma skin cancer by multimodal imaging. Healthcare 2013, 1, 64–83. [Google Scholar] [CrossRef] [PubMed]
- Vogler, N.; Meyer, T.; Akimov, D.; Latka, I.; Krafft, C.; Bendsoe, N.; Svanberg, K.; Dietzek, B.; Popp, J. Multimodal imaging to study the morphochemistry of basal cell carcinoma. J. Biophotonics 2010, 3, 728–36. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Cheng, J.; Thrall, M.J.; Liu, Z.; Wang, X.; Wong, S.T.C. Multimodal non-linear optical imaging for label-free differentiation of lung cancerous lesions from normal and desmoplastic tissues. Biomed. Opt. Express 2013, 4, 2855–68. [Google Scholar] [CrossRef] [PubMed]
- Koropecki, R.R.; Arce, R. Infrared study of the kinetics of oxidation in porous amorphous silicon. J. Appl. Phys. 1986, 60, 1802–1807. [Google Scholar] [CrossRef]
- Yorikawa, H.; Muramatsu, S. Photoluminescence and particle size distribution in porous silicon. J. Lumin. 2000, 87–89, 423–425. [Google Scholar] [CrossRef]
- Gonchar, K.; Osminkina, L.; Galkin, R.; Gongalsky, M.B.; Marshov, V.S.; Timoshenko, V.Y.; Kulmas, M.N.; Solovyev, V.V.; Kudryavtsev, A.A.; Sivakov, V. Growth, structure and optical properties of silicon nanowires formed by metal-assisted chemical etching. J. Nanoelectron. Optoelectron. 2012, 7, 602–606. [Google Scholar] [CrossRef]
- Momose, M.; Hirasaka, M.; Furukawa, Y. Raman spectroscopic study on phosphorous-doped silicon nanoparticles. Appl. Spectrosc. 2015, 69, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Sirenko, A.A.; Fox, J.R.; Akimov, I.A.; Xi, X.X.; Ruvimov, S.; Liliental-Weber, Z. In situ Raman scattering studies of the amorphous and crystalline Si nanoparticles. Solid State Commun. 2000, 113, 553–558. [Google Scholar] [CrossRef]
- Campbell, I.H.; Fauchet, P.M. The effects of microcrystal size and shape on the one phonon Raman spectra of crystalline semiconductors. Solid State Commun. 1986, 58, 739–741. [Google Scholar] [CrossRef]
- Tolstik, E.; Shukla, S.; Heintzmann, R. High-resolution far-field microscopy. In The Optics Encyclopedia; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2015. [Google Scholar]
- Matthäus, C.; Krafft, C.; Dietzek, B.; Brehm, B.R.; Lorkowski, S.; Popp, J. Noninvasive imaging of intracellular lipid metabolism in macrophages by Raman microscopy in combination with stable isotopic labeling. Anal. Chem. 2012, 84, 8549–8556. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, J.M.P.; Dias, J.M.B. Vertex component analysis: A fast algorithm to unmix hyperspectral data. IEEE Trans. Geosci. Remote Sens. 2005, 43, 898–910. [Google Scholar] [CrossRef]
- Mazur, A.I.; Monahan, J.L.; Miljković, M.; Laver, N.; Diem, M.; Bird, B. Vibrational spectroscopic changes of B-lymphocytes upon activation. J. Biophotonics 2013, 6, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Tolstik, T.; Marquardt, C.; Matthäus, C.; Bergner, N.; Bielecki, C.; Krafft, C.; Stallmach, A.; Popp, J. Discrimination and classification of liver cancer cells and proliferation states by Raman spectroscopic imaging. Analyst 2014, 139, 6036–6043. [Google Scholar] [CrossRef] [PubMed]
- Lasch, P. Spectral pre-processing for biomedical vibrational spectroscopy and microspectroscopic imaging. Chemom. Intell. Lab. Syst. 2012, 117, 100–114. [Google Scholar] [CrossRef]
- Bielecki, C.; Bocklitz, T.W.; Schmitt, M.; Krafft, C.; Marquardt, C.; Gharbi, A.; Knösel, T.; Stallmach, A.; Popp, J. Classification of inflammatory bowel diseases by means of Raman spectroscopic imaging of epithelium cells. J. Biomed. Opt. 2012, 17, 76030. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T.; Akimov, D.; Tarcea, N.; Chatzipapadopoulos, S.; Muschiolik, G.; Kobow, J.; Schmitt, M.; Popp, J. Three-dimensional molecular mapping of a multiple emulsion by means of CARS microscopy. J. Phys. Chem. B 2008, 112, 1420–1426. [Google Scholar] [CrossRef] [PubMed]





© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tolstik, E.; Osminkina, L.A.; Akimov, D.; Gongalsky, M.B.; Kudryavtsev, A.A.; Timoshenko, V.Y.; Heintzmann, R.; Sivakov, V.; Popp, J. Linear and Non-Linear Optical Imaging of Cancer Cells with Silicon Nanoparticles. Int. J. Mol. Sci. 2016, 17, 1536. https://doi.org/10.3390/ijms17091536
Tolstik E, Osminkina LA, Akimov D, Gongalsky MB, Kudryavtsev AA, Timoshenko VY, Heintzmann R, Sivakov V, Popp J. Linear and Non-Linear Optical Imaging of Cancer Cells with Silicon Nanoparticles. International Journal of Molecular Sciences. 2016; 17(9):1536. https://doi.org/10.3390/ijms17091536
Chicago/Turabian StyleTolstik, Elen, Liubov A. Osminkina, Denis Akimov, Maksim B. Gongalsky, Andrew A. Kudryavtsev, Victor Yu. Timoshenko, Rainer Heintzmann, Vladimir Sivakov, and Jürgen Popp. 2016. "Linear and Non-Linear Optical Imaging of Cancer Cells with Silicon Nanoparticles" International Journal of Molecular Sciences 17, no. 9: 1536. https://doi.org/10.3390/ijms17091536