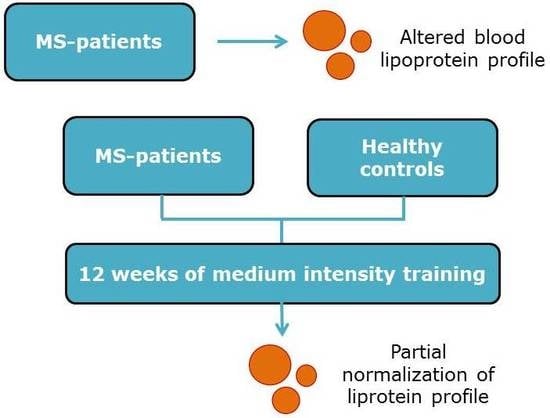
Twelve Weeks of Medium-Intensity Exercise Therapy Affects the Lipoprotein Profile of Multiple Sclerosis Patients
Abstract
:1. Introduction
2. Results
Twelve Weeks of Medium-Intensity Endurance Training Affects the Lipoprotein Profile of MS Patients
3. Discussion
4. Materials and Methods
4.1. Subjects
4.2. Study Design
4.3. Sample Processing
4.4. Nuclear Magnetic Resonance Spectroscopy
4.5. Statistical Analysis
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wens, I.; Dalgas, U.; Deckx, N.; Cools, N.; Eijnde, B. Does multiple sclerosis affect glucose tolerance? Mult. Scler. 2013, 20, 1273–1276. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, S.R.; Simao, A.N.; Kallaur, A.P.; de Almeida, E.R.; Morimoto, H.K.; Lopes, J.; Dichi, I.; Kaimen-Maciel, D.R.; Reiche, E.M. Disability in patients with multiple sclerosis: Influence of insulin resistance, adiposity, and oxidative stress. Nutrition 2014, 30, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Jorissen, W.; Wouters, E.; Bogie, J.F.; Vanmierlo, T.; Noben, J.P.; Sviridov, D.; Hellings, N.; Somers, V.; Valcke, R.; Vanwijmeersch, B.; et al. Relapsing-remitting multiple sclerosis patients display an altered lipoprotein profile with dysfunctional HDL. Sci. Rep. 2017, 7, 43410. [Google Scholar] [CrossRef] [PubMed]
- Penesova, A.; Vlcek, M.; Imrich, R.; Vernerova, L.; Marko, A.; Meskova, M.; Grunnerova, L.; Turcani, P.; Jezova, D.; Kollar, B. Hyperinsulinemia in newly diagnosed patients with multiple sclerosis. Metab. Brain Dis. 2015, 30, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Marrie, R.A.; Rudick, R.; Horwitz, R.; Cutter, G.; Tyry, T.; Campagnolo, D.; Vollmer, T. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology 2010, 74, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Weinstock-Guttman, B.; Zivadinov, R.; Horakova, D.; Havrdova, E.; Qu, J.; Shyh, G.; Lakota, E.; O’Connor, K.; Badgett, D.; Tamano-Blanco, M.; et al. Lipid profiles are associated with lesion formation over 24 months in interferon-beta treated patients following the first demyelinating event. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1186–1191. [Google Scholar] [CrossRef] [PubMed]
- Fellows, K.; Uher, T.; Browne, R.W.; Weinstock-Guttman, B.; Horakova, D.; Posova, H.; Vaneckova, M.; Seidl, Z.; Krasensky, J.; Tyblova, M.; et al. Protective associations of HDL with blood-brain barrier injury in multiple sclerosis patients. J. Lipid Res. 2015, 56, 2010–2018. [Google Scholar] [CrossRef] [PubMed]
- Weinstock-Guttman, B.; Zivadinov, R.; Mahfooz, N.; Carl, E.; Drake, A.; Schneider, J.; Teter, B.; Hussein, S.; Mehta, B.; Weiskopf, M.; et al. Serum lipid profiles are associated with disability and MRI outcomes in multiple sclerosis. J. Neuroinflamm. 2011, 8, 127. [Google Scholar] [CrossRef] [PubMed]
- Giubilei, F.; Antonini, G.; Di Legge, S.; Sormani, M.P.; Pantano, P.; Antonini, R.; Sepe-Monti, M.; Caramia, F.; Pozzilli, C. Blood cholesterol and MRI activity in first clinical episode suggestive of multiple sclerosis. Acta Neurol. Scand. 2002, 106, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Zorzon, M. A nexus between lipids and multiple sclerosis? J. Neurol. Neurosurg. Psychiatry 2013, 84, 1181. [Google Scholar] [CrossRef] [PubMed]
- Tettey, P.; Simpson, S.; Taylor, B.; Ponsonby, A.L.; Lucas, R.M.; Dwyer, T.; Kostner, K.; Group, A.I.; van der Mei, I.A. An adverse lipid profile and increased levels of adiposity significantly predict clinical course after a first demyelinating event. J. Neurol. Neurosurg. Psychiatry 2017, 88, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Salemi, G.; Gueli, M.C.; Vitale, F.; Battaglieri, F.; Guglielmini, E.; Ragonese, P.; Trentacosti, A.; Massenti, M.F.; Savettieri, G.; Bono, A. Blood lipids, homocysteine, stress factors, and vitamins in clinically stable multiple sclerosis patients. Lipids Health Dis. 2010, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Palavra, F.; Marado, D.; Mascarenhas-Melo, F.; Sereno, J.; Teixeira-Lemos, E.; Nunes, C.C.; Goncalves, G.; Teixeira, F.; Reis, F. New markers of early cardiovascular risk in multiple sclerosis patients: Oxidized-LDL correlates with clinical staging. Dis. Mark. 2013, 34, 341–348. [Google Scholar] [CrossRef]
- Çomoğlu, S.; Yardimci, S.; Okçu, Z. Body fat distribution and plasma lipid profiles of patients with multiple sclerosis. Turk. J. Med. Sci. 2004, 34, 43–48. [Google Scholar]
- Sternberg, Z.; Leung, C.; Sternberg, D.; Li, F.; Karmon, Y.; Chadha, K.; Levy, E. The prevalence of the classical and non-classical cardiovascular risk factors in multiple sclerosis patients. CNS Neurol. Disord. Drug Targets 2013, 12, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Tettey, P.; Simpson, S., Jr.; Taylor, B.; Blizzard, L.; Ponsonby, A.L.; Dwyer, T.; Kostner, K.; van der Mei, I. An adverse lipid profile is associated with disability and progression in disability, in people with MS. Mult. Scler. 2014, 20, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Mandoj, C.; Renna, R.; Plantone, D.; Sperduti, I.; Cigliana, G.; Conti, L.; Koudriavtseva, T. Anti-annexin antibodies, cholesterol levels and disability in multiple sclerosis. Neurosci. Lett. 2015, 606, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Meyers, L.; Groover, C.J.; Douglas, J.; Lee, S.; Brand, D.; Levin, M.C.; Gardner, L.A. A role for Apolipoprotein A-I in the pathogenesis of multiple sclerosis. J. Neuroimmunol. 2014, 277, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Jamroz-Wisniewska, A.; Beltowski, J.; Stelmasiak, Z.; Bartosik-Psujek, H. Paraoxonase 1 activity in different types of multiple sclerosis. Mult. Scler. 2009, 15, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Besler, H.T.; Comoglu, S. Lipoprotein oxidation, plasma total antioxidant capacity and homocysteine level in patients with multiple sclerosis. Nutr. Neurosci. 2003, 6, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, G.; Bacchetti, T.; Principi, F.; Di Ludovico, F.; Viti, B.; Angeleri, V.A.; Danni, M.; Provinciali, L. Increased levels of lipid hydroperoxides in plasma of patients with multiple sclerosis: A relationship with paraoxonase activity. Mult. Scler. 2005, 11, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Wens, I.; Hansen, D.; Verboven, K.; Deckx, N.; Kosten, L.; Stevens, A.L.; Cools, N.; Eijnde, B.O. Impact of 24 Weeks of Resistance and Endurance Exercise on Glucose Tolerance in Persons with Multiple Sclerosis. Am. J. Phys. Med. Rehabil. 2015, 94 (Suppl. 1), 838–847. [Google Scholar] [CrossRef] [PubMed]
- Deckx, N.; Wens, I.; Nuyts, A.H.; Hens, N.; De Winter, B.Y.; Koppen, G.; Goossens, H.; Van Damme, P.; Berneman, Z.N.; Eijnde, B.O.; et al. 12 Weeks of Combined Endurance and Resistance Training Reduces Innate Markers of Inflammation in a Randomized Controlled Clinical Trial in Patients with Multiple Sclerosis. Mediat. Inflamm. 2016, 2016, 6789276. [Google Scholar] [CrossRef] [PubMed]
- Wens, I.; Keytsman, C.; Deckx, N.; Cools, N.; Dalgas, U.; Eijnde, B.O. Brain derived neurotrophic factor in multiple sclerosis: Effect of 24 weeks endurance and resistance training. Eur. J. Neurol. 2016, 23, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Wens, I.; Dalgas, U.; Vandenabeele, F.; Grevendonk, L.; Verboven, K.; Hansen, D.; Eijnde, B.O. High Intensity Exercise in Multiple Sclerosis: Effects on Muscle Contractile Characteristics and Exercise Capacity, a Randomised Controlled Trial. PLoS ONE 2015, 10, e0133697. [Google Scholar] [CrossRef] [PubMed]
- Dalgas, U.; Stenager, E.; Ingemann-Hansen, T. Multiple sclerosis and physical exercise: Recommendations for the application of resistance-, endurance- and combined training. Mult. Scler. 2008, 14, 35–53. [Google Scholar] [CrossRef] [PubMed]
- Wens, I.; Dalgas, U.; Verboven, K.; Kosten, L.; Stevens, A.; Hens, N.; Eijnde, B.O. Impact of high intensity exercise on muscle morphology in EAE rats. Physiol. Res. 2015, 64, 907–923. [Google Scholar] [PubMed]
- Duvivier, B.M.; Schaper, N.C.; Bremers, M.A.; van Crombrugge, G.; Menheere, P.P.; Kars, M.; Savelberg, H.H. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS ONE 2013, 8, e55542. [Google Scholar] [CrossRef] [PubMed]
- Duvivier, B.M.; Schaper, N.C.; Hesselink, M.K.; van Kan, L.; Stienen, N.; Winkens, B.; Koster, A.; Savelberg, H.H. Breaking sitting with light activities vs. structured exercise: A randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia 2017, 60, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Jeyarajah, E.J.; Cromwell, W.C.; Otvos, J.D. Lipoprotein particle analysis by nuclear magnetic resonance spectroscopy. Clin. Lab. Med. 2006, 26, 847–870. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.F.; Steiner, G. Hypertriglyceridemia and its metabolic consequences as a risk factor for atherosclerotic cardiovascular disease in non-insulin-dependent diabetes mellitus. Diabetes Metab. Rev. 1996, 12, 37–56. [Google Scholar] [CrossRef]
- Lamarche, B.; Lewis, G.F. Atherosclerosis prevention for the next decade: Risk assessment beyond low density lipoprotein cholesterol. Can. J. Cardiol. 1998, 14, 841–851. [Google Scholar] [PubMed]
- Ginsberg, H.N. Lipoprotein physiology in nondiabetic and diabetic states. Relationship to atherogenesis. Diabetes Care 1991, 14, 839–855. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M. Atherogenic dyslipidemia: Lipoprotein abnormalities and implications for therapy. Am. J. Cardiol. 1995, 75, 45B–52B. [Google Scholar] [CrossRef]
- Raina Elley, C.; Kenealy, T. Lifestyle interventions reduced the long-term risk of diabetes in adults with impaired glucose tolerance. Evid.-Based Med. 2008, 13, 173. [Google Scholar] [CrossRef] [PubMed]
- Hawley, J.A. Exercise as a therapeutic intervention for the prevention and treatment of insulin resistance. Diabetes Metab. Res. Rev. 2004, 20, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Unwin, N.; Shaw, J.; Zimmet, P.; Alberti, K.G. Impaired glucose tolerance and impaired fasting glycaemia: The current status on definition and intervention. Diabet. Med. 2002, 19, 708–723. [Google Scholar] [PubMed]
- Oldroyd, J.C.; Unwin, N.C.; White, M.; Mathers, J.C.; Alberti, K.G. Randomised controlled trial evaluating lifestyle interventions in people with impaired glucose tolerance. Diabetes Res. Clin. Pract. 2006, 72, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Blair, S.N.; Jakicic, J.M.; Manore, M.M.; Rankin, J.W.; Smith, B.K. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc. 2009, 41, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Daussin, F.N.; Zoll, J.; Dufour, S.P.; Ponsot, E.; Lonsdorfer-Wolf, E.; Doutreleau, S.; Mettauer, B.; Piquard, F.; Geny, B.; Richard, R. Effect of interval versus continuous training on cardiorespiratory and mitochondrial functions: Relationship to aerobic performance improvements in sedentary subjects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 295, R264–R272. [Google Scholar] [CrossRef] [PubMed]
- Krauss, R.M. Atherogenicity of triglyceride-rich lipoproteins. Am. J. Cardiol. 1998, 81, 13B–17B. [Google Scholar] [CrossRef]
- Sutherland, W.H.; Restieaux, N.J.; Nye, E.R.; Williams, M.J.; de Jong, S.A.; Robertson, M.C.; Walker, H.L. IDL composition and angiographically determined progression of atherosclerotic lesions during simvastatin therapy. Arterioscler. Thromb. Vasc. Biol. 1998, 18, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Lyons, T.J.; Jenkins, A.J.; Zheng, D.; Klein, R.L.; Otvos, J.D.; Yu, Y.; Lackland, D.T.; McGee, D.; McHenry, M.B.; Lopes-Virella, M.; et al. Nuclear magnetic resonance-determined lipoprotein subclass profile in the DCCT/EDIC cohort: Associations with carotid intima-media thickness. Diabet. Med. 2006, 23, 955–966. [Google Scholar] [CrossRef] [PubMed]
- Batista, M.C.; Welty, F.K.; Diffenderfer, M.R.; Sarnak, M.J.; Schaefer, E.J.; Lamon-Fava, S.; Asztalos, B.F.; Dolnikowski, G.G.; Brousseau, M.E.; Marsh, J.B. Apolipoprotein A-I, B-100, and B-48 metabolism in subjects with chronic kidney disease, obesity, and the metabolic syndrome. Metabolism 2004, 53, 1255–1261. [Google Scholar] [CrossRef] [PubMed]
- Werner, R.M.; Pearson, T.A. LDL-cholesterol: A risk factor for coronary artery disease—From epidemiology to clinical trials. Can. J. Cardiol. 1998, 14 (Suppl. B), 3B–10B. [Google Scholar] [PubMed]
- Rahilly-Tierney, C.R.; Lawler, E.V.; Scranton, R.E.; Michael Gaziano, J. Low-density lipoprotein reduction and magnitude of cardiovascular risk reduction. Prev. Cardiol. 2009, 12, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Zhornitsky, S.; McKay, K.A.; Metz, L.M.; Teunissen, C.E.; Rangachari, M. Cholesterol and markers of cholesterol turnover in multiple sclerosis: Relationship with disease outcomes. Mult. Scler. Relat. Disord. 2016, 5, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Millar, J.S.; Packard, C.J. Heterogeneity of apolipoprotein B-100-containing lipoproteins: What we have learnt from kinetic studies. Curr. Opin. Lipidol. 1998, 9, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Krauss, R.M. Lipids and lipoproteins in patients with type 2 diabetes. Diabetes Care 2004, 27, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Zambon, A.; Bertocco, S.; Vitturi, N.; Polentarutti, V.; Vianello, D.; Crepaldi, G. Relevance of hepatic lipase to the metabolism of triacylglycerol-rich lipoproteins. Biochem. Soc. Trans. 2003, 31, 1070–1074. [Google Scholar] [CrossRef] [PubMed]
- Nigon, F.; Lesnik, P.; Rouis, M.; Chapman, M.J. Discrete subspecies of human low density lipoproteins are heterogeneous in their interaction with the cellular LDL receptor. J. Lipid Res. 1991, 32, 1741–1753. [Google Scholar] [PubMed]
- Tribble, D.L.; Holl, L.G.; Wood, P.D.; Krauss, R.M. Variations in oxidative susceptibility among six low density lipoprotein subfractions of differing density and particle size. Atherosclerosis 1992, 93, 189–199. [Google Scholar] [CrossRef]
- Williams, P.T. Relationships of heart disease risk factors to exercise quantity and intensity. Arch. Intern. Med. 1998, 158, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Earnest, C.P.; Artero, E.G.; Sui, X.; Lee, D.C.; Church, T.S.; Blair, S.N. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. Mayo Clin. Proc. 2013, 88, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Burgomaster, K.A.; Heigenhauser, G.J.; Gibala, M.J. Effect of short-term sprint interval training on human skeletal muscle carbohydrate metabolism during exercise and time-trial performance. J. Appl. Physiol. (1985) 2006, 100, 2041–2047. [Google Scholar] [CrossRef] [PubMed]
- Tomlin, D.L.; Wenger, H.A. The relationship between aerobic fitness and recovery from high intensity intermittent exercise. Sports Med. 2001, 31, 1–11. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, G.; Owen, A.; Bird, S.R.; Kearney, E.M.; Nevill, A.M.; Jones, D.W.; Woolf-May, K. Changes in cardiorespiratory fitness and coronary heart disease risk factors following 24 wk of moderate- or high-intensity exercise of equal energy cost. J. Appl. Physiol. (1985) 2005, 98, 1619–1625. [Google Scholar] [CrossRef] [PubMed]
- Thoumie, P.; Lamotte, D.; Cantalloube, S.; Faucher, M.; Amarenco, G. Motor determinants of gait in 100 ambulatory patients with multiple sclerosis. Mult. Scler. 2005, 11, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Shalaurova, I.; Connelly, M.A.; Garvey, W.T.; Otvos, J.D. Lipoprotein insulin resistance index: A lipoprotein particle-derived measure of insulin resistance. Metab. Syndr. Relat. Disord. 2014, 12, 422–429. [Google Scholar] [CrossRef] [PubMed]

| Parameter | HC | MS | p Value |
|---|---|---|---|
| N | 40 | 41 | |
| Age | 47.5 ± 1.8 | 46 ± 1.5 | 0.511 |
| Male gender, % | 12 (30%) | 19 (46%) | 0.17 |
| BMI | 24.3 ± 0.5 | 24.7 ± 0.7 | 0.919 |
| EDSS score | NA | 2.8 ± 0.4 | NA |
| Conventional lipid panel | |||
| Total cholesterol, mg/dL | 191.6 ± 5.7 | 181.4 ± 5.1 | 0.185 |
| Triglycerides, mg/dL | 97.8 ± 7.1 | 105.3 ± 5.0 | 0.104 |
| HDL-c, mg/dL | 66.6 ± 1.8 | 62.0 ± 2.9 | 0.175 |
| LDL-c, mg/dL | 115.3 ± 5.6 | 110.3 ± 5.0 | 0.501 |
| Lipoprotein subclasses | |||
| HDL | |||
| Size nm | 9.7 ± 0.1 | 9.4 ± 0.1 | 0.075 |
| Total particle count, μmol/L | 36.4 ± 0.8 | 35.3 ± 1.0 | 0.413 |
| Small particle count, μmol/L | 13.0 ± 1.0 | 14.3 ± 1.1 | 0.368 |
| Medium particle count, μmol/L | 13.2 ± 1.0 | 12.8 ± 1.3 | 0.758 |
| Large particle count, μmol/L | 8.6 ± 0.5 | 7.4 ± 0.7 | 0.084 |
| LDL | |||
| Size, nm | 21.4 ± 0.1 | 21.1 ± 0.1 * | 0.033 |
| Total particle count, nmol/L | 1122.4 ± 63.4 | 1106.6 ± 52.3 | 0.931 |
| Small particle count, nmol/L | 280.4 ± 38.9 | 286.0 ± 36.1 | 0.794 |
| Large particle count, nmol/L | 535.2 ± 32.4 | 506.2 ± 33.2 | 0.535 |
| IDL | |||
| Particle count, nmol/L | 192.8 ± 19.3 | 204.5 ± 20.9 | 0.794 |
| VLDL | |||
| Size, nm | 47.9 ± 1.0 | 50.7 ± 1.1 | 0.115 |
| Total particle count, nmol/L | 40.8 ± 4.1 | 43.2 ± 3.6 | 0.663 |
| Small particle count, nmol/L | 21.7 ± 2.0 | 24.1 ± 2.6 | 0.470 |
| Medium particle count, nmol/L | 17.2 ± 2.6 | 16.1 ± 2.4 | 0.882 |
| Large particle count, nmol/L | 2.9 ± 0.5 | 4.0 ± 0.4 *** | 0.0004 |
| VLDL-Triglycerides, mg/dL | 59.7 ± 5.4 | 67.7 ± 4.1 | 0.085 |
| LP-IR index (0–100) | 29.7 ± 2.7 | 44.3 ± 2.8 *** | 0.0003 |
| Parameter | Medium-Intensity Training | High-Intensity Training | ||||
|---|---|---|---|---|---|---|
| N | 21 | 20 | ||||
| Age | 48.0 ± 2.7 | 44.0 ± 2.6 | ||||
| Male gender, % | 10 (47.6%) | 9 (45%) | ||||
| BMI | 24.6 ± 1.3 | 24.7 ± 1.0 | ||||
| EDSS score | 3.2 ± 0.4 | 2.52 ± 0.3 | ||||
| PRE | POST | p value | PRE | POST | p value | |
| Conventional lipid panel | ||||||
| Total cholesterol, mg/dL | 180.7 ± 7.6 | 176.7 ± 7.6 (−2.2%) | 0.42 | 182.1 ± 6.9 | 183.0 ± 7.7 (+0.5%) | 0.43 |
| Triglycerides, mg/dL | 106.2 ± 8.5 | 106.9 ± 6.6 (+0.7%) | 0.90 | 104.3 ± 5.4 | 116.0 ± 9.4 (+11.2%) | 0.33 |
| HDL-c, mg/dL | 60.4 ± 4.2 | 61.2 ± 4.7 (+1.3%) | 0.60 | 63.6 ± 4.0 | 64.2 ± 4.0 (+0.9%) | 0.75 |
| LDL-c, mg/dL | 112.5 ± 7.7 | 103.9 ± 5.8 $ (−7.6%) | 0.042 | 107.9 ± 6.5 | 106.9 ± 8.3 (−0.9%) | 0.14 |
| Lipoprotein subclasses | ||||||
| HDL | ||||||
| Size nm | 9.4 ± 0.2 | 9.4 ± 0.1 (no % change) | 0.58 | 9.5 ± 0.1 | 9.5 ± 0.1 (no % change) | 0.55 |
| Total particle count, μmol/L | 34.6 ± 1.5 | 35.08 ± 1.5 (+1.4%) | 0.63 | 36.1 ± 1.3 | 36.7 ± 1.2 (+1.7%) | 0.31 |
| Small particle count, μmol/L | 15.1 ± 1.5 | 14.0 ± 1.8 (−7.3%) | 0.41 | 13.5 ± 1.6 | 12.7 ± 1.6 (−5.9%) | 0.64 |
| Medium particle count, μmol/L | 11.7 ± 1.8 | 12.6 ± 2.0 (+7.7%) | 0.48 | 14.0 ± 2.0 | 15.5 ± 1.7 (+10.7%) | 0.92 |
| Large particle count, μmol/L | 6.6 ± 0.9 | 7.2 ± 1.0 (+9.1%) | 0.11 | 8.2 ± 0.9 | 8.4 ± 0.9 (+2.4%) | 0.80 |
| LDL | ||||||
| Size, nm | 21.1 ± 0.1 | 21.2 ± 0.1 (+0.5%) | 0.60 | 21.1 ± 0.1 | 21.0 ± 0.1 (−0.5%) | 0.06 |
| Total particle count, nmol/L | 1108.1 ± 79.1 | 1044.2 ± 68.1 (−5.8%) | 0.10 | 1105.0 ± 70.1 | 1114.3 ± 101.2 (+0.8%) | 0.33 |
| Small particle count, nmol/L | 233.1 ± 44.9 | 279.4 ± 53.1 (+19.9%) | 0.21 | 341.6 ± 55.6 | 348.4 ± 72.5 (+2.0%) | 0.86 |
| Large particle count, nmol/L | 497.7 ± 49.3 | 514.5 ± 40.1 (+3.4%) | 0.64 | 515.2 ± 45.3 | 504.9 ± 51.1 (−2.0%) | 0.79 |
| IDL | ||||||
| Particle count, nmol/L | 265.6 ± 30.4 †† | 150.3 ± 24.5 $$ (−43.4%) | 0.002 | 140.4 ± 21.0 | 156.1 ± 24.5 (+11.2%) | 0.74 |
| VLDL | ||||||
| Size, nm | 53.2 ± 1.6 † | 49.7 ± 1.4 $ (−6.6%) | 0.047 | 48.0 ± 1.1 | 49.4 ± 1.1 (+2.9%) | 0.09 |
| Total particle count, nmol/L | 39.1 ± 5.6 | 47.0 ± 5.0 (+20.2%) | 0.10 | 47.5 ± 4.3 | 50.3 ± 6.3 (+5.9%) | 0.65 |
| Small particle count, nmol/L | 18.2 ± 3.2 † | 27.8 ± 3.6 (+52.7%) | 0.058 | 30.3 ± 3.8 | 29.9 ± 3.6 (−1.3%) | 0.88 |
| Medium particle count, nmol/L | 17.8 ± 4.2 | 15.6 ± 2.0 (−12.4%) | 0.98 | 14.3 ± 2.3 | 16.8 ± 4.1 (+17.5%) | 0.84 |
| Large particle count, nmol/L | 4.4 ± 0.7 | 4.4 ± 0.6 (no % change) | 0.79 | 3.5 ± 0.3 | 4.5 ± 0.7 (+28.6%) | 0.08 |
| VLDL-Triglycerides, mg/dL | 68.7 ± 7.2 | 71.7 ± 5.1 (+4.4%) | 0.71 | 66.5 ± 4.2 | 77.4 ± 8.0 (+16.8%) | 0.28 |
| LP-IR index (0–100) | 48.8 ± 4.4 | 43.3 ± 3.7 (−11.3%) | 0.09 | 39.6 ± 3.4 | 43.0 ± 4.6 (+8.6%) | 0.15 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jorissen, W.; Vanmierlo, T.; Wens, I.; Somers, V.; Van Wijmeersch, B.; Bogie, J.F.; Remaley, A.T.; Eijnde, B.O.; Hendriks, J.J.A. Twelve Weeks of Medium-Intensity Exercise Therapy Affects the Lipoprotein Profile of Multiple Sclerosis Patients. Int. J. Mol. Sci. 2018, 19, 193. https://doi.org/10.3390/ijms19010193
Jorissen W, Vanmierlo T, Wens I, Somers V, Van Wijmeersch B, Bogie JF, Remaley AT, Eijnde BO, Hendriks JJA. Twelve Weeks of Medium-Intensity Exercise Therapy Affects the Lipoprotein Profile of Multiple Sclerosis Patients. International Journal of Molecular Sciences. 2018; 19(1):193. https://doi.org/10.3390/ijms19010193
Chicago/Turabian StyleJorissen, Winde, Tim Vanmierlo, Inez Wens, Veerle Somers, Bart Van Wijmeersch, Jeroen F. Bogie, Alan T. Remaley, Bert O. Eijnde, and Jerome J. A. Hendriks. 2018. "Twelve Weeks of Medium-Intensity Exercise Therapy Affects the Lipoprotein Profile of Multiple Sclerosis Patients" International Journal of Molecular Sciences 19, no. 1: 193. https://doi.org/10.3390/ijms19010193
APA StyleJorissen, W., Vanmierlo, T., Wens, I., Somers, V., Van Wijmeersch, B., Bogie, J. F., Remaley, A. T., Eijnde, B. O., & Hendriks, J. J. A. (2018). Twelve Weeks of Medium-Intensity Exercise Therapy Affects the Lipoprotein Profile of Multiple Sclerosis Patients. International Journal of Molecular Sciences, 19(1), 193. https://doi.org/10.3390/ijms19010193