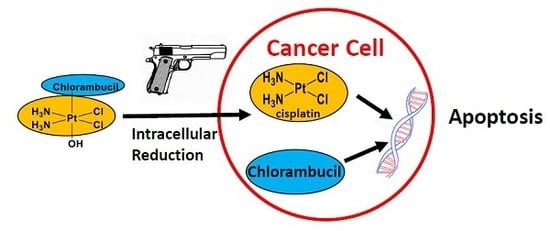
A Pt(IV) Prodrug Combining Chlorambucil and Cisplatin: A Dual-Acting Weapon for Targeting DNA in Cancer Cells
Abstract
:1. Introduction
2. Results and Discussion
2.1. Synthesis and Characterization
2.2. Reduction Studies
2.3. Cytotoxicity Studies
2.4. Cellular Uptake and DNA Platination
2.5. DNA Fragmentation and Apoptosis Induction
3. Materials and Methods
3.1. Synthesis
3.2. Biological Methods
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rosemberg, B.; Van Camp, L.; Krigas, T. Inhibition of Cell Division in Escherichia Coli by Electrolysis Products from Platinum Electrode. Nature 1965, 205, 698–699. [Google Scholar] [CrossRef]
- Hannon, M.J. Metal-based anticancer drugs: From a Past Anchored in nPlatinum hemistry to a post-genomic future of diverse chemistry and biology. Pure Appl. Chem. 2007, 79, 2243–2261. [Google Scholar] [CrossRef]
- Siegel, A.; Sigel, H. Metal Ions in Biological Systems Vol. 42 Metal Complexes in Tumour Diagnosis and as Anticancer Agents; CRC Press: New York, NY, USA, 2004; Chapter 8; pp. 251–296. [Google Scholar]
- Wilson, J.J.; Lippard, S.J. Synthetic Methods for the preparation of Platinum Anticancer Complexes. Chem. Rev. 2014, 114, 4470–4495. [Google Scholar] [CrossRef] [PubMed]
- Gibson, D. Platinum(IV) anticancer prodrugs- hypotheses and facts. Dalton. Trans. 2016, 45, 12983–12991. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.Z.; Bonnitcha, P.; Wezselb;att, E.; Klein, A.V.; Najajreh, Y.; Gibson, D.; Hambley, T.W. Facile Preparation of Mono-, Di- and Mixed-Carboxylato Platinum(IV) Complexes for Versatile Anticancer Prodrug Design. Chem. Eur. J. 2013, 19, 1672–1676. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, T.C.; Suntharalingam, K.; Lippard, J.S. The Next Generation of Platinum Drugs: Targeted Pt(II) Agents, Nanoparticle Delivery and Pt(IV) Prodrugs. Chem. Rev. 2016, 116, 3436–3486. [Google Scholar] [CrossRef] [PubMed]
- Harper, B.W.; Krause-Heuer, A.M.; Grant, M.P.; Monohar, M.; Garbutcheon-Singh, K.B.; Aldrich-Wright, J.R. Advances in Platinum Chemotherapeutics. Chem. Eur. J. 2010, 16, 7064–7077. [Google Scholar] [CrossRef]
- Yang, J.; Sun, X.; Mao, W.; Sui, M.; Tang, J.; Shen, Y. Conjugate of Pt(IV)-Histone Deacetylase Inhibitor as a Prodrug for Cancer Chemotherapy. Mol. Pharm. 2012, 9, 2793–2800. [Google Scholar] [CrossRef] [PubMed]
- Neumann, W.; Crews, B.C.; Marnett, L.J.; Hey-Hawkins, E. Conjugates of Cisplatin and Cyclooxygenase Inhibitors as Potent Antitumor Agents Overcoming Cisplatin Resistance. ChemMedChem 2014, 9, 1150–1153. [Google Scholar] [CrossRef] [Green Version]
- Chin, C.F.; Yap, S.Q.; Li, J.; Pastorin, G.; Ang, W.H. Ratiometric delivery of cisplatin and doxorubicin using tumour-targeting carbon nanotubes entrapping Pt(IV) prodrugs. Chem. Sci. 2014, 5, 2265–2270. [Google Scholar] [CrossRef]
- Raveendran, R.; Braude, J.P.; Wexselblatt, E.; Novohradsky, V.; Stuchlikova, O.; Brabec, V.; Gandin, V.; Gibson, D. Pt(IV) derivatives of cisplatin and oxalilplatin with phenylbutyrate axial ligand are potent cytotoxic agents that act by several mechanism of action. Chem. Sci. 2016, 7, 2381–2391. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Ma, R.; Wang, Y.; Zhu, X.; Zhang, J.; Chan, H.C.; Chen, X.; Zhang, W.; Chiu, S.K.; Zhu, G. Chalcoplatin, a dual-targeting and P53 activator-containing anticancer platinum(IV) prodrug with unique mode of action. Chem. Commun. 2015, 51, 6301–6304. [Google Scholar] [CrossRef]
- Wang, Q.; Huang, Z.; Ma, J.; Lu, X.; Zhang, L.; Wang, X.; Wang, P.G. Design, Synthesis and biological evaluation of a novel series of glycosylated platinum(IV) complexes as antitumor agents. Dalton Trans. 2016, 45, 10366–10374. [Google Scholar] [CrossRef] [PubMed]
- Almotairy, A.R.Z.; Gandin, V.; Morrison, L.; Marzano, C.; Montagner, D.; Erxleben, A. Antitumor platinum(IV) derivatives of carboplatin and the histone deacetylase inhibitor 4-phenylbutyric acid. J. Inorg. Biochem. 2017, 177, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lo Re, D.; Montagner, D.; Tolan, D.; Di Sanza, C.; Iglesias, M.; Calon, A.; Giralt, E. Increased immune cell infiltration in patient-derived tumor explants treated with Traniplatin: An original Pt(IV) pro-drugs based on cisplatin and Tranilast. Chem. Commun. 2018, 54, 8324–8327. [Google Scholar] [CrossRef] [PubMed]
- Petruzzella, E.; Sirota, R.; Solazzo, I.; Gandin, V.; Gibson, D. Triple Action Pt(IV) derivatives of cisplatin: A new class of potent anticancer agents that overcome resistance. Chem. Sci. 2018, 9, 4299–4307. [Google Scholar] [CrossRef] [PubMed]
- Faguet, G.B. Chronic lymphocytic leukemia: An update review. J. Clin. Oncol. 1994, 12, 1974–1990. [Google Scholar] [CrossRef]
- Urbaniak, M.D.; Bingham, J.P.; Hartley, J.A.; Woolfson, D.N.; Caddick, S. Design and Synthesis of a nitrogen mustard derivative stabilized by apo-neo-carzinostatin. J. Med. Chem. 2004, 47, 4710–4715. [Google Scholar] [CrossRef]
- Papaconstantinou, I.C.; Fousteris, M.A.; Koutsorea, A.I.; Pairas, G.N.; Papageorgoiu, A.D.; Nikolaropoulos, S.S. Steroidal esters of the aromatic nitrogen mustard 2-[4-N, N-bis(2-chloroethyl) amino-phenyl ] butanoic acid (2-PHE-BU): Synthesis and in vivo biological evaluation. Anticancer Drugs 2013, 24, 52–65. [Google Scholar] [CrossRef]
- Millard, M.; Gallagher, J.D.; Olenyuk, B.Z.; Neamati, N. A selective mitochondrial-targeted chlorambucil with remarkable cytotoxicity in breast and pancreatic cancers. J. Med. Chem. 2013, 56, 9170–9179. [Google Scholar] [CrossRef]
- Ciaccio, P.J.; Tew, K.D.; La Creta, F.P. Enzymatic conjugation of chlorambucil with glutathione by human glutathione S-transferase and inhibition by ethacrynic acid. Biochem. Pharmacol. 1991, 41, 1504–1507. [Google Scholar] [CrossRef]
- Qin, X.; Fang, L.; Chen, F.; Gou, S. Conjugation of Platinum(IV) complexes with Chlorambucil to overcome cisplatin resistance via a “joint action” mode toward DNA. Eur. J. Med. Chem. 2017, 137, 167–175. [Google Scholar] [CrossRef]
- Pathak, R.K.; Wen, R.; Kolishetti, N.; Dhar, S. A Prodrug of two approved Drugs, Cisplatin and Chlorambucil, for Chemo War Against Cancer. Mol. Cancer Ther. 2017, 16, 625–636. [Google Scholar] [CrossRef] [PubMed]
- Tolan, D.; Gandin, V.; Morrison, L.; El-Nahas, A.; Marzano, C.; Montagner, D.; Erxleben, A. Oxidative Stress Induced by Pt(IV) Pro-Drugs Based on Cisplatin Scaffold and Indole Carboxylic Acids in Axial Position. Sci. Rep. 2016, 6, 9367. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.G.Z.; Babak, M.V.; Weiss, A.; Dyson, P.J.; Nowak-Sliwinska, P.; Montagner, D.; Ang, W.H. Development of an efficient Dual-Action GST-Inhibithing Anrticancer Platinum(IV) Prodrug. ChemMedChem 2018, 13, 1210–1217. [Google Scholar] [CrossRef]
- Wong, D.Y.Q.; Yeo, C.H.F.; Ang, W.H. Immuno-Chemotherapeutic Platinum(IV) Prodrugs of Cisplatin as Multimodal Anticancer Agents. Angew. Chem. Int. Ed. 2014, 53, 6752–6756. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.Y.Q.; Ong, W.W.F.; Ang, W.H. Induction of Immunogenic Cell Death by Chemotherapeutic Platinum Complexes. Angew. Chem. Int. Ed. 2015, 54, 6483–6487. [Google Scholar] [CrossRef]
- Zhang, J.Z.; Wexselblatt, E.; Hambley, T.W.; Gibson, D. Pt(IV) analogs of oxalilplatin that do not follow the expected correlation between electrochemical reduction potential and rate of reduction by ascorbate. Chem. Commun. 2012, 48, 847–849. [Google Scholar]
- Das, S.; Ciombor, K.K.; Haraldsdottir, S.; Goldberg, R.M. Promising New Agents for Colorectal Cancer. Curr. Treat. Options Oncol. 2018, 19, 29. [Google Scholar] [CrossRef]
- Kim, J. Bin Three-dimensional tissue culture models in cancer biology. Semin. Cancer Biol. 2005, 15, 365–377. [Google Scholar] [CrossRef]
- Raveendran, R.; Braude, J.P.; Wexselblatt, E.; Novohradsky, V.; Stuchlikova, O.; Brabec, V.; Gandin, V.; Gibson, D. Pt(IV) derivatives of cisplatin and oxaliplatin with phenylbutyrate axial ligands are potent cytotoxic agents that act by several mechanisms of action. Chem. Sci. 2016, 7, 2381–2391. [Google Scholar] [CrossRef] [PubMed]
- Reithofer, M.R.; Bytzek, A.K.; Valiahdi, S.M.; Kowol, C.R.; Groessl, M.; Hartinger, C.G.; Jakupec, M.A.; Galanski, M.; Keppler, B.K. Tuning of lipophilicity and cytotoxic potency by structural variation of anticancer platinum(IV) complexes. J. Inorg. Biochem. 2011, 105, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Reithofer, M.R.; Schwarzinger, A.; Valiahdi, S.M.; Galanski, M.; Jakupec, M.A.; Keppler, B.K. Novel bis(carboxylato)dichlorido(ethane-1,2-diamine)platinum(IV) complexes with exceptionally high cytotoxicity. J. Inorg. Biochem. 2008, 102, 2072–2077. [Google Scholar] [CrossRef] [PubMed]
- Dhara, S.C. A rapid method for the Synthesis of cis-[Pt(NH3)2Cl2]. Indian J. Chem. 1970, 8, 193–197. [Google Scholar]
- Galanski, M.; Keppler, B.K. Carboxylation of Dihydroxoplatinum(IV) Complexes via a New Synthetic Pathway. Inorg. Chem. 1996, 35, 1709–1711. [Google Scholar] [CrossRef]






| Compound | IC50 (µM) ± SD | |||||||
|---|---|---|---|---|---|---|---|---|
| PSN1 | 2008 | C13* | LoVo | A431 | BxPC3 | HCT-15 | BCPAP | |
| 1 | 0.42 ± 0.1 | 0.31 ± 0.1 | 0.28 ± 0.1 | 0.98 ± 0.1 | 0.41 ± 0.1 | 1.74 ± 0.5 | 0.39 ± 0.1 | 0.51 ± 0.2 |
| Chlorambucil | >100 | 34.58 ± 16.5 | >100 | >100 | 74.48 ± 8.2 | >100 | 44.52 ± 9.5 | >100 |
| CDDP | 18.11 ± 3.2 | 2.18 ± 0.9 | 22.11 ± 3.2 | 9.15 ± 2.1 | 2.21 ± 0.4 | 7.22 ± 2.2 | 15.28 ± 2.6 | 7.31 ± 1.2 |
| IC50 (µM) ± SD | |||
|---|---|---|---|
| 1 | CDDP | OXP | |
| HCT-15 | 40.4 ± 5.1 | 71.1 ± 3.9 | 33.2 ± 4.6 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montagner, D.; Tolan, D.; Andriollo, E.; Gandin, V.; Marzano, C. A Pt(IV) Prodrug Combining Chlorambucil and Cisplatin: A Dual-Acting Weapon for Targeting DNA in Cancer Cells. Int. J. Mol. Sci. 2018, 19, 3775. https://doi.org/10.3390/ijms19123775
Montagner D, Tolan D, Andriollo E, Gandin V, Marzano C. A Pt(IV) Prodrug Combining Chlorambucil and Cisplatin: A Dual-Acting Weapon for Targeting DNA in Cancer Cells. International Journal of Molecular Sciences. 2018; 19(12):3775. https://doi.org/10.3390/ijms19123775
Chicago/Turabian StyleMontagner, Diego, Dina Tolan, Emma Andriollo, Valentina Gandin, and Cristina Marzano. 2018. "A Pt(IV) Prodrug Combining Chlorambucil and Cisplatin: A Dual-Acting Weapon for Targeting DNA in Cancer Cells" International Journal of Molecular Sciences 19, no. 12: 3775. https://doi.org/10.3390/ijms19123775