Fatty Acid Potassium Had Beneficial Bactericidal Effects and Removed Staphylococcus aureus Biofilms while Exhibiting Reduced Cytotoxicity towards Mouse Fibroblasts and Human Keratinocytes
Abstract
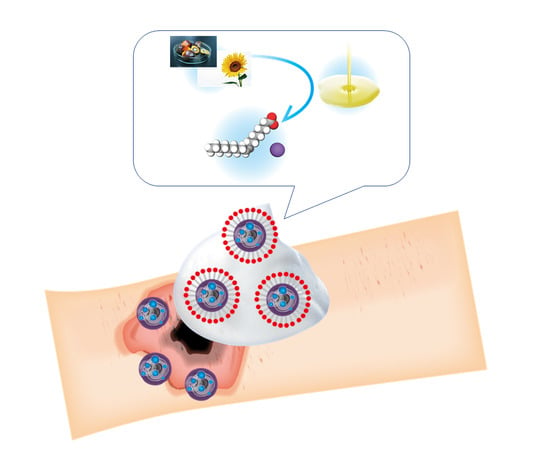
:1. Introduction
2. Results
2.1. Structures of Fatty Acid Potassium and Synthetic Surfactant Detergents
2.2. Cytotoxic Assays
2.2.1. LDH Leakage
2.2.2. Cell Viability
2.3. Anti-Bacterial Test
2.4. Effects on Biofilm-Forming MRSA
2.4.1. Crystal Violet Assay
2.4.2. Ultra-Microstructural Appearance after Treatment with Potassium Oleate (C18:1K)
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Preparation of Surfactant Solutions for the Cytotoxicity Assay
4.3. Preparation of Surfactant Solutions for the Antibacterial Test
4.4. Preparation of Surfactant Solutions for the Biofilm Removal Test
4.5. Cell Culture
4.6. Cytotoxicity Assay
4.7. Preparation of the Bacterial Suspensions
4.8. Anti-Bacterial Test
4.9. Biofilm Formation
4.10. Biofilm Removal Test
4.11. Biofilm Structure According to Scanning Electron Microscopy (SEM)
4.12. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| MRSA | Methicillin-resistant Staphylococcus aureus |
| SLES | Sodium lauryl ether sulfate |
| SLS | Sodium lauryl sulfate |
| SSI | Surgical site infection |
References
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human skin wounds: A major and snowballing threat to public health and the economy. Wound Repair Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [Green Version]
- Richmond, N.A.; Maderal, A.D.; Vivas, A.C. Evidence based management of common chronic lower extremity ulcers. Dermatol. Ther. 2013, 26, 187–196. [Google Scholar] [CrossRef]
- Rice, J.B.; Desai, U.; Cummings, A.K.; Birnbaum, H.G.; Skornicki, M.; Parsons, N.B. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care 2014, 37, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Garcia, G.A.; Nguyen, C.V.; Yonkers, M.A.; Tao, J.P. Baby Shampoo Versus Povidone-Iodine or Isopropyl Alcohol in Reducing Eyelid Skin Bacterial Load. Ophthalmic Plast. Reconstr. Surg. 2018, 34, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Karki, S.; Cheng, A.C. Impact of non-rinse skin cleansing with chlorhexidine gluconate on prevention of healthcare-associated infections and colonization with multi-resistant organisms: A systematic review. J. Hosp. Infect. 2012, 82, 71–84. [Google Scholar] [CrossRef]
- Webster, J.; Osborne, S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst. Rev. 2015, CD004985. [Google Scholar] [CrossRef] [PubMed]
- Popovich, K.J.; Hota, B.; Hayes, R.; Weinstein, R.A.; Hayden, M.K. Daily skin cleansing with chlorhexidine did not reduce the rate of central-line associated bloodstream infection in a surgical intensive care unit. Intensive Care Med. 2010, 36, 854–858. [Google Scholar] [CrossRef] [PubMed]
- Vali, L.; Davies, S.E.; Lai, L.L.; Dave, J.; Amyes, S.G. Frequency of biocide resistance genes, antibiotic resistance and the effect of chlorhexidine exposure on clinical methicillin-resistant Staphylococcus aureus isolates. J. Antimicrob. Chemother. 2008, 61, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Nherera, L.M.; Woodmansey, E.; Trueman, P.; Gibbons, G.W. Estimating the Clinical Outcomes and Cost Differences Between Standard Care with and without Cadexomer Iodine in the Management of Chronic Venous Leg Ulcers Using a Markov Model. Ostomy Wound Manag. 2016, 62, 26–40. [Google Scholar]
- Das Ghatak, P.; Mathew-Steiner, S.S.; Pandey, P.; Roy, S.; Sen, C.K. A surfactant polymer dressing potentiates antimicrobial efficacy in biofilm disruption. Sci. Rep. 2018, 8, 873. [Google Scholar] [CrossRef] [Green Version]
- Percival, S.L.; Mayer, D.; Salisbury, A.M. Efficacy of a surfactant-based wound dressing on biofilm control. Wound Repair Regen. 2017, 25, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Burnouf, T.; Chou, M.L.; Wu, Y.W.; Su, C.Y.; Lee, L.W. Antimicrobial activity of platelet (PLT)-poor plasma, PLT-rich plasma, PLT gel, and solvent/detergent-treated PLT lysate biomaterials against wound bacteria. Transfusion 2013, 53, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Finnerty, C.C.; Herndon, D.N.; Lee, J.O.; Rodriguez, N.A.; Al-Haj, I.H.; Wurzer, P.; Calhoun, B.R.; Jeschke, M.G. Morbidity and mortality in severely burned children with Clostridium difficile-associated diarrhea. Surgery 2016, 159, 1631–1637. [Google Scholar] [CrossRef] [PubMed]
- Farrokhi, A.; Pakyari, M.; Nabai, L.; Pourghadiri, A.; Hartwell, R.; Jalili, R.; Ghahary, A. Evaluation of Detergent-Free and Detergent-Based Methods for Decellularization of Murine Skin. Tissue Eng. Part A 2018, 24, 955–967. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Zhang, W.; Khan, M.; Lin, L.; Lin, J.M. MoS2-LA PEI nanocomposite carrier for real-time imaging of ATP metabolism in glioma stem cells co-cultured with endothelial cells on a microfluidic system. Biosens. Bioelectron. 2018, 99, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Galbiati, V.; Martínez, V.; Bianchi, S.; Mitjans, M.; Corsini, E. Establishment of an in vitro photoallergy test using NCTC2544 cells and IL-18 production. Toxicol. In Vitro 2013, 27, 103–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akers, K.S.; Mend, K.; Cheatle, K.A.; Zera, W.C.; Yu, X.; Beckius, M.L.; Aggarwal, D.; Li, P.; Sanchez, C.J.; Wenke, J.C.; et al. Biofilms and persistent wound infections in United States military trauma patients: A case-control analysis. BMC Infect. Dis. 2014, 14, 190. [Google Scholar] [CrossRef]
- Makino, T.; Jimi, S.; Oyama, T.; Nakano, Y.; Hamamoto, K.; Mamishin, K.; Yahiro, T.; Hara, S.; Takata, T.; Ohjimi, H. Infection mechanism of biofilm-forming Staphylococcus aureus on indwelling foreign materials in mice. Int. Wound J. 2015, 12, 122–131. [Google Scholar] [CrossRef]
- Jimi, S.; Miyazaki, M.; Takata, T.; Ohjimi, H.; Akita, S.; Hara, S. Increased drug resistance of meticillin-resistant Staphylococcus aureus biofilms formed on a mouse dermal chip model. J. Med. Microbiol. 2017, 66, 542–550. [Google Scholar] [CrossRef] [Green Version]
- Oyama, T.; Miyazaki, M.; Yoshimura, M.; Takata, T.; Ohjimi, H.; Jimi, S. Biofilm-Forming Methicillin-Resistant Staphylococcus aureus Survive in Kupffer Cells and Exhibit High Virulence in Mice. Toxins 2016, 8, 198. [Google Scholar] [CrossRef]
- Anglen, J.O.; Gainor, B.J.; Simpson, W.A.; Christensen, G. The use of detergent irrigation for musculoskeletal wounds. Int. Orthop. 2003, 27, 40–46. [Google Scholar]
- Amouroux, I.; Pesando, D.; Noël, H.; Girard, J.P. Mechanisms of cytotoxicity by cosmetic ingredients in sea urchin eggs. Arch. Environ. Contam. Toxicol. 1999, 36, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Larsen, H.F.; Ahlström, M.G.; Gjerdrum, L.M.R.; Mogensen, M.; Ghathian, K.; Calum, H.; Sørensen, A.L.; Forman, J.L.; Vandeven, M.; Holerca, M.N.; et al. Noninvasive measurement of reepithelialization and microvascularity of suction-blister wounds with benchmarking to histology. Wound Repair Regen. 2017, 25, 984–993. [Google Scholar] [CrossRef] [PubMed]
- Jovanovic, A.; Ermis, R.; Mewaldt, R.; Shi, L.; Carson, D. The Influence of Metal Salts, Surfactants, and Wound Care Products on Enzymatic Activity of Collagenase. Wounds 2012, 24, 242–253. [Google Scholar] [PubMed]
- Patil, S.; Singh, P.; Sarasour, K.; Maibach, H. Quantification the Wound Debriding Enzyme of sodium lauryl sulfate penetration into the skin and underlying tissue after topical application—Pharmacological and toxicological implications. J. Pharm. Sci. 1995, 84, 1240–1244. [Google Scholar] [CrossRef] [PubMed]
- Kadono, T.; Uezu, K.; Kosaka, T.; Kawano, T. Altered toxicities of fatty acid salts in green paramecia cultured in different waters. Z. Naturforsch. C 2006, 61, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Arokiyaraj, S.; Arasu, M.V.; Vincent, S.; Prakash, N.U.; Choi, S.H.; Oh, Y.K.; Choi, K.C.; Kim, K.H. Rapid green synthesis of silver nanoparticles from Chrysanthemum indicum L and its antibacterial and cytotoxic effects: An in vitro study. Int. J. Nanomed. 2014, 9, 379–388. [Google Scholar] [CrossRef]
- Kovary, K.; Louvain, T.S.; Costa e Silva, M.C.; Albano, F.; Pires, B.B.; Laranja, G.A.; Lage, C.L.; Felzenszwalb, I. Biochemical behaviour of norbixin during in vitro DNA damage induced by reactive oxygen species. Br. J. Nutr. 2001, 85, 431–440. [Google Scholar] [CrossRef] [Green Version]
- Akhtar, M.J.; Ahamed, M.; Fareed, M.; Alrokayan, S.A.; Kumar, S. Protective effect of sulphoraphane against oxidative stress mediated toxicity induced by CuO nanoparticles in mouse embryonic fibroblasts BALB 3T3. J. Toxicol. Sci. 2012, 37, 139–148. [Google Scholar] [CrossRef] [Green Version]
- Minnich, K.E.; Stolarick, R.; Wilkins, R.G.; Chilson, G.; Pritt, S.L.; Unverdorben, M. The effect of a wound care solution containing polyhexanide and betaine on bacterial counts: Results of an in vitro study. Ostomy Wound Manag. 2012, 58, 32–36. [Google Scholar]
- Bauer, J.; Siala, W.; Tulkens, P.M.; Van Bambeke, F. A combined pharmacodynamic quantitative and qualitative model reveals the potent activity of daptomycin and delafloxacin against Staphylococcus aureus biofilms. Antimicrob. Agents Chemother. 2013, 57, 2726–2737. [Google Scholar] [CrossRef] [PubMed]
- Presterl, E.; Suchomel, M.; Eder, M.; Reichmann, S.; Lassnigg, A.; Graninger, W.; Rotter, M. Effects of alcohols, povidone-iodine and hydrogen peroxide on biofilms of Staphylococcus epidermidis. J. Antimicrob. Chemother. 2007, 60, 417–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qi, X.; Poernomo, G.; Wang, K.; Chen, Y.; Chan-Park, M.B.; Xu, R.; Chang, M.W. Covalent immobilization of nisin on multi-walled carbon nanotubes: Superior antimicrobial and anti-biofilm properties. Nanoscale 2011, 3, 1874–1880. [Google Scholar] [CrossRef] [PubMed]









| C18:1K (log CFU/mL) | Alcohol-Based Disinfectant (log CFU/mL) | |||||
|---|---|---|---|---|---|---|
| 1 min | 5 min | 10 min | 1 min | 5 min | 10 min | |
| Escherichia coli | 3.3 (0.4) | >4.3 (0.2) | >4.3 (0.2) | >4.3 (0.2) | >4.3 (0.2) | >4.3 (0.2) |
| Staphylococcus aureus | 1.7 (0.9) * | >4.4 (0.1) | >4.4 (0.2) | >4.5 (0.3) | >4.4 (0.3) | >4.4 (0.2) |
| Bacillus cereus | 0.2 (0.2) | 0.2 (0.3) | 0.3 (0.3) | 0.1 (0.2) | 0.2 (0.3) | 0.2 (0.4) |
| Clostridium difficile | >2.4 (0.5) * | >2.4 (0.5) * | >2.4 (0.5) ** | 0.4 (0.2) | 0.5 (0.3) | 0.5 (0.2) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawahara, T.; Takita, M.; Masunaga, A.; Morita, H.; Tsukatani, T.; Nakazawa, K.; Go, D.; Akita, S. Fatty Acid Potassium Had Beneficial Bactericidal Effects and Removed Staphylococcus aureus Biofilms while Exhibiting Reduced Cytotoxicity towards Mouse Fibroblasts and Human Keratinocytes. Int. J. Mol. Sci. 2019, 20, 312. https://doi.org/10.3390/ijms20020312
Kawahara T, Takita M, Masunaga A, Morita H, Tsukatani T, Nakazawa K, Go D, Akita S. Fatty Acid Potassium Had Beneficial Bactericidal Effects and Removed Staphylococcus aureus Biofilms while Exhibiting Reduced Cytotoxicity towards Mouse Fibroblasts and Human Keratinocytes. International Journal of Molecular Sciences. 2019; 20(2):312. https://doi.org/10.3390/ijms20020312
Chicago/Turabian StyleKawahara, Takayoshi, Miki Takita, Akihiro Masunaga, Hayato Morita, Tadayuki Tsukatani, Kohji Nakazawa, Daisuke Go, and Sadanori Akita. 2019. "Fatty Acid Potassium Had Beneficial Bactericidal Effects and Removed Staphylococcus aureus Biofilms while Exhibiting Reduced Cytotoxicity towards Mouse Fibroblasts and Human Keratinocytes" International Journal of Molecular Sciences 20, no. 2: 312. https://doi.org/10.3390/ijms20020312