Expression of Autotaxin–Lysophosphatidate Signaling-Related Proteins in Breast Cancer with Adipose Stroma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Histologic Evaluation
2.2. Tissue Microarray (TMA)
2.3. Immunohistochemistry
2.4. Interpretation of Immunohistochemical Staining
2.5. Western Blotting
2.6. Tumor Phenotype Classification
3. Statistical Analysis
4. Results
4.1. Characteristics of Patients According to Breast Cancer Stroma Type
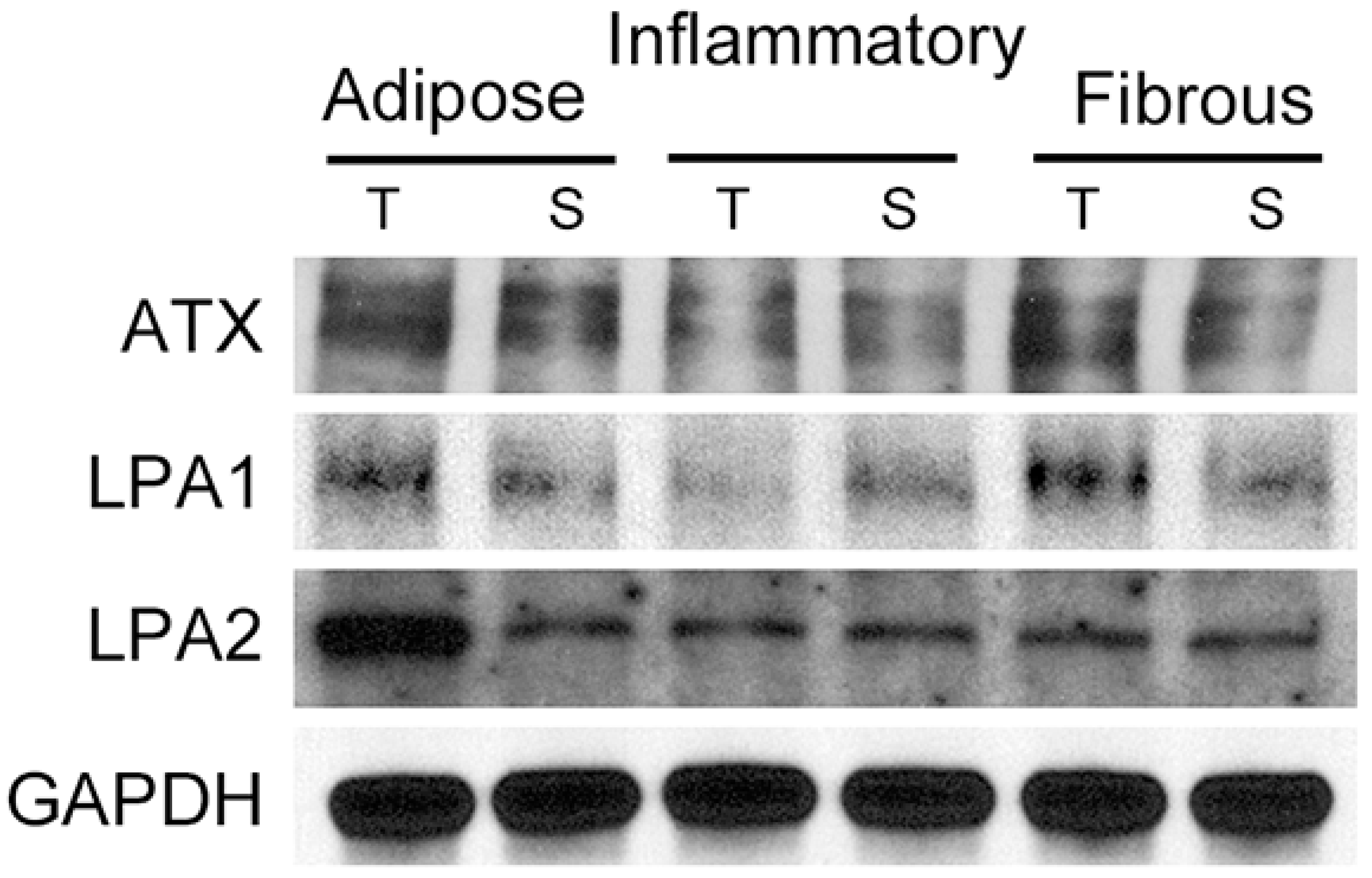
4.2. Expression of ATX-LPA Signaling-Related Proteins according to Breast Cancer Stroma Type
4.3. Correlation of the Expression of ATX-LPA Signaling-Related Proteins
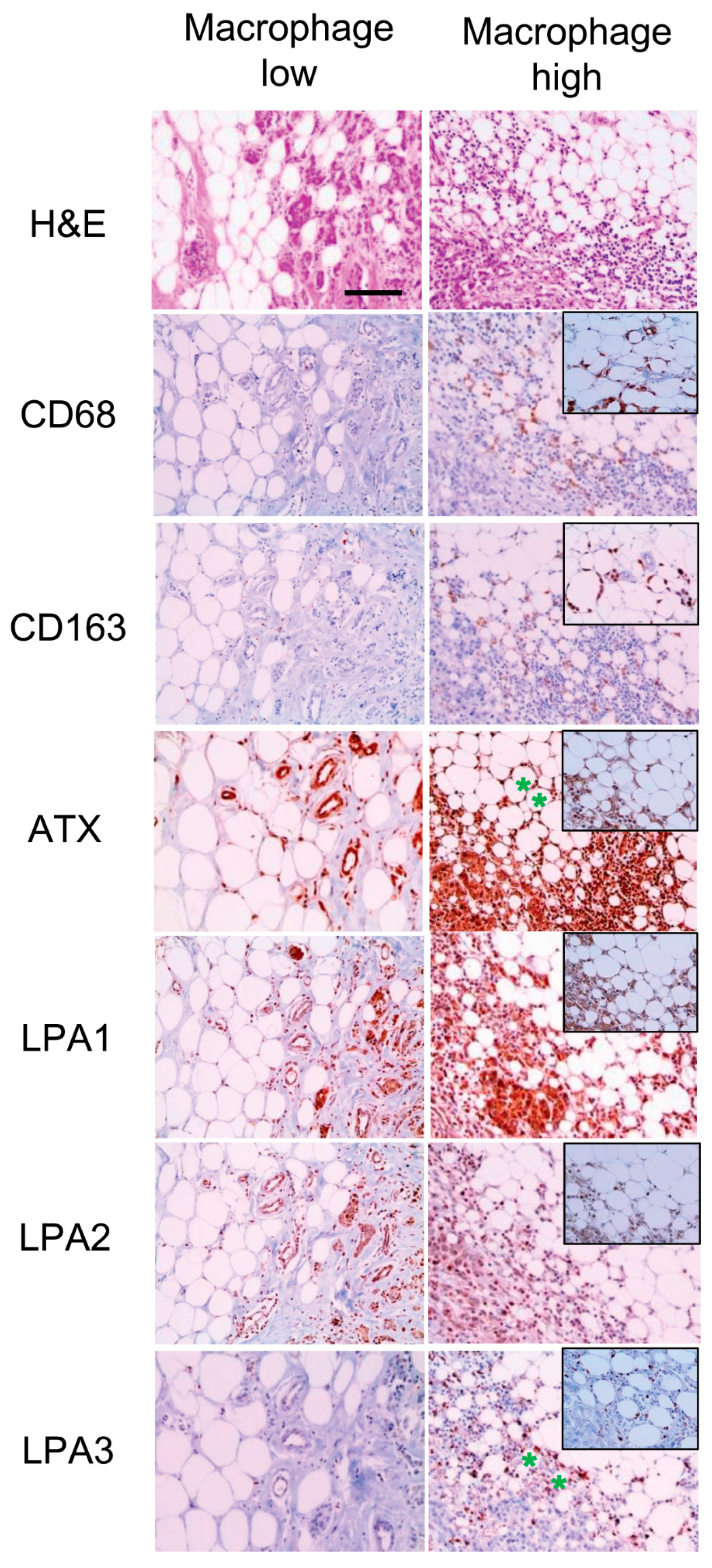
4.4. Correlation between the Expression of ATX-LPA Signaling-Related Proteins and Macrophages in Adipose Stroma
4.5. ATX-LPA Signaling-Related Proteins and Clinicopathologic Parameters
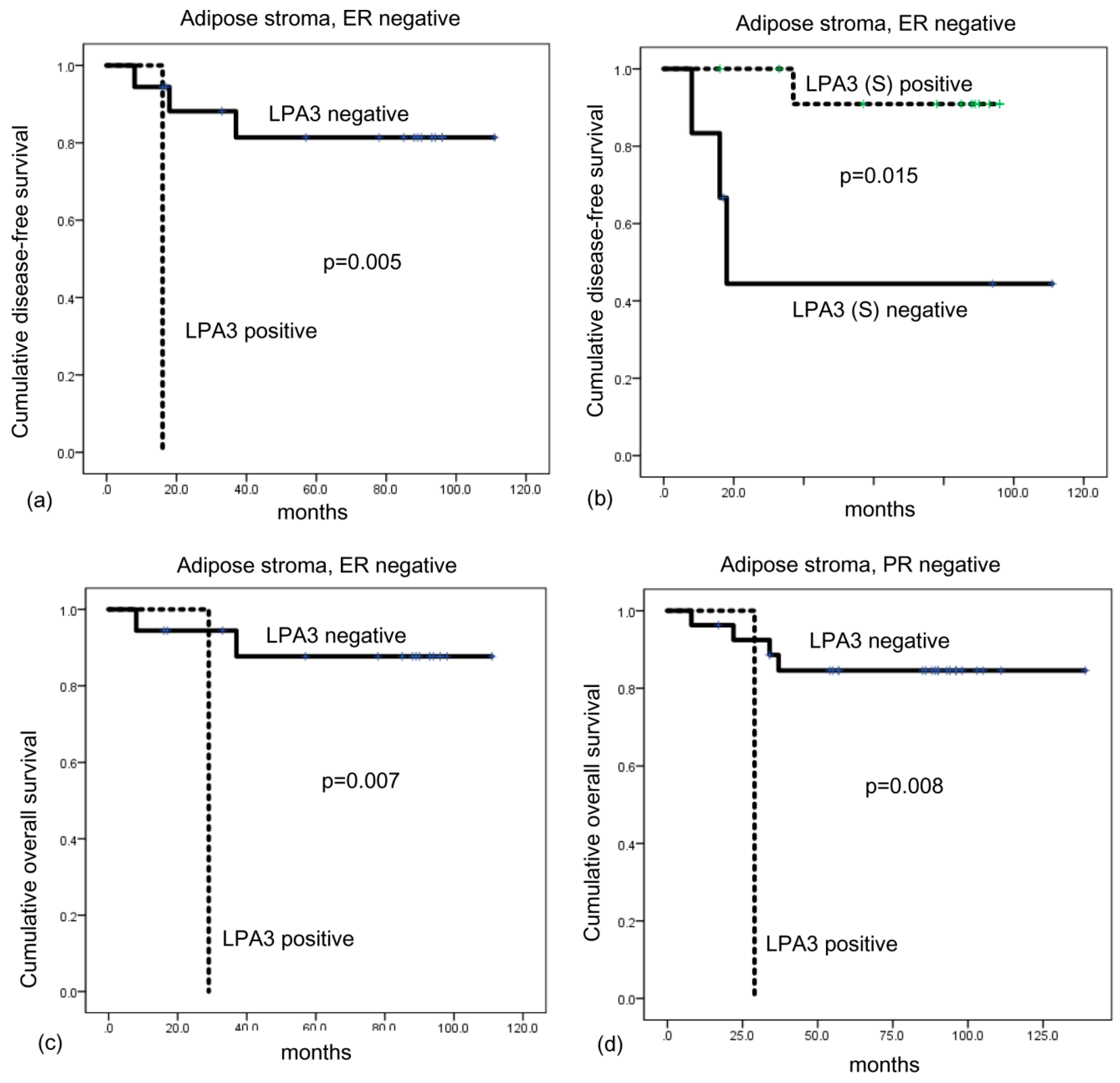
4.6. Impact of the Expression of ATX-LPA Signaling-Related Proteins on Patient Prognosis
5. Discussion
5.1. Compliance with Ethical Standards
Ethical Standards
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jansen, S.; Stefan, C.; Creemers, J.W.; Waelkens, E.; Van Eynde, A.; Stalmans, W.; Bollen, M. Proteolytic maturation and activation of autotaxin (npp2), a secreted metastasis-enhancing lysophospholipase d. J. Cell Sci. 2005, 118, 3081–3089. [Google Scholar] [CrossRef] [PubMed]
- van Meeteren, L.A.; Moolenaar, W.H. Regulation and biological activities of the autotaxin-lpa axis. Prog. Lipid Res. 2007, 46, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Herr, D.R.; Noguchi, K.; Yung, Y.C.; Lee, C.W.; Mutoh, T.; Lin, M.E.; Teo, S.T.; Park, K.E.; Mosley, A.N.; et al. Lpa receptors: Subtypes and biological actions. Annu. Rev. Pharmacol. Toxicol. 2010, 50, 157–186. [Google Scholar] [CrossRef] [PubMed]
- Chun, J.; Hla, T.; Lynch, K.R.; Spiegel, S.; Moolenaar, W.H. International union of basic and clinical pharmacology. Lxxviii. Lysophospholipid receptor nomenclature. Pharmacol. Rev. 2010, 62, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Houben, A.J.; Moolenaar, W.H. Autotaxin and lpa receptor signaling in cancer. Cancer Metastasis Rev. 2011, 30, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Willier, S.; Butt, E.; Grunewald, T.G. Lysophosphatidic acid (lpa) signalling in cell migration and cancer invasion: A focussed review and analysis of lpa receptor gene expression on the basis of more than 1700 cancer microarrays. Biol. Cell 2013, 105, 317–333. [Google Scholar] [CrossRef]
- Ferry, G.; Tellier, E.; Try, A.; Gres, S.; Naime, I.; Simon, M.F.; Rodriguez, M.; Boucher, J.; Tack, I.; Gesta, S.; et al. Autotaxin is released from adipocytes, catalyzes lysophosphatidic acid synthesis, and activates preadipocyte proliferation. Up-regulated expression with adipocyte differentiation and obesity. J. Biol. Chem. 2003, 278, 18162–18169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikitopoulou, I.; Oikonomou, N.; Karouzakis, E.; Sevastou, I.; Nikolaidou-Katsaridou, N.; Zhao, Z.; Mersinias, V.; Armaka, M.; Xu, Y.; Masu, M.; et al. Autotaxin expression from synovial fibroblasts is essential for the pathogenesis of modeled arthritis. J. Exp. Med. 2012, 209, 925–933. [Google Scholar] [CrossRef] [Green Version]
- Mao, Y.; Keller, E.T.; Garfield, D.H.; Shen, K.; Wang, J. Stromal cells in tumor microenvironment and breast cancer. Cancer Metastasis Rev. 2013, 32, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Boucharaba, A.; Serre, C.M.; Gres, S.; Saulnier-Blache, J.S.; Bordet, J.C.; Guglielmi, J.; Clezardin, P.; Peyruchaud, O. Platelet-derived lysophosphatidic acid supports the progression of osteolytic bone metastases in breast cancer. J. Clin. Investig. 2004, 114, 1714–1725. [Google Scholar] [CrossRef] [Green Version]
- Dusaulcy, R.; Rancoule, C.; Gres, S.; Wanecq, E.; Colom, A.; Guigne, C.; van Meeteren, L.A.; Moolenaar, W.H.; Valet, P.; Saulnier-Blache, J.S. Adipose-specific disruption of autotaxin enhances nutritional fattening and reduces plasma lysophosphatidic acid. J. Lipid Res. 2011, 52, 1247–1255. [Google Scholar] [CrossRef] [Green Version]
- Vandeweyer, E.; Hertens, D. Quantification of glands and fat in breast tissue: An experimental determination. Ann. Anat. Anat. Anz. Off. Organ Anat. Ges. 2002, 184, 181–184. [Google Scholar] [CrossRef]
- Ramsay, D.T.; Kent, J.C.; Hartmann, R.A.; Hartmann, P.E. Anatomy of the lactating human breast redefined with ultrasound imaging. J. Anat. 2005, 206, 525–534. [Google Scholar] [CrossRef] [Green Version]
- Teo, K.; Brunton, V.G. The role and therapeutic potential of the autotaxin-lysophosphatidate signalling axis in breast cancer. Biochem. J. 2014, 463, 157–165. [Google Scholar] [CrossRef]
- Elston, C.W.; Ellis, I.O. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: Experience from a large study with long-term follow-up. Histopathology 1991, 19, 403–410. [Google Scholar] [CrossRef]
- Salgado, R.; Denkert, C.; Demaria, S.; Sirtaine, N.; Klauschen, F.; Pruneri, G.; Wienert, S.; Van den Eynden, G.; Baehner, F.L.; Penault-Llorca, F.; et al. The evaluation of tumor-infiltrating lymphocytes (tils) in breast cancer: Recommendations by an international tils working group 2014. Ann. Anat. Anat. Anz. Off. Organ Anat. Ges. 2015, 26, 259–271. [Google Scholar] [CrossRef]
- Hammond, M.E.; Hayes, D.F.; Dowsett, M.; Allred, D.C.; Hagerty, K.L.; Badve, S.; Fitzgibbons, P.L.; Francis, G.; Goldstein, N.S.; Hayes, M.; et al. American society of clinical oncology/college of american pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 2784–2795. [Google Scholar] [CrossRef]
- Wolff, A.C.; Hammond, M.E.; Schwartz, J.N.; Hagerty, K.L.; Allred, D.C.; Cote, R.J.; Dowsett, M.; Fitzgibbons, P.L.; Hanna, W.M.; Langer, A.; et al. American society of clinical oncology/college of american pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2007, 25, 118–145. [Google Scholar] [CrossRef]
- Choi, J.; Jung, W.H.; Koo, J.S. Clinicopathologic features of molecular subtypes of triple negative breast cancer based on immunohistochemical markers. Histol. Histopathol. 2012, 27, 1481–1493. [Google Scholar]
- Goldhirsch, A.; Wood, W.C.; Coates, A.S.; Gelber, R.D.; Thurlimann, B.; Senn, H.J. Strategies for subtypes--dealing with the diversity of breast cancer: Highlights of the st. Gallen international expert consensus on the primary therapy of early breast cancer 2011. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2011, 22, 1736–1747. [Google Scholar] [CrossRef]
- Cha, Y.J.; Kim, E.S.; Koo, J.S. Tumor-associated macrophages and crown-like structures in adipose tissue in breast cancer. Breast Cancer Res. Treat. 2018. [Google Scholar] [CrossRef]
- Yang, S.Y.; Lee, J.; Park, C.G.; Kim, S.; Hong, S.; Chung, H.C.; Min, S.K.; Han, J.W.; Lee, H.W.; Lee, H.Y. Expression of autotaxin (npp-2) is closely linked to invasiveness of breast cancer cells. Clin. Exp. Metastasis 2002, 19, 603–608. [Google Scholar] [CrossRef]
- Li, T.T.; Alemayehu, M.; Aziziyeh, A.I.; Pape, C.; Pampillo, M.; Postovit, L.M.; Mills, G.B.; Babwah, A.V.; Bhattacharya, M. Beta-arrestin/ral signaling regulates lysophosphatidic acid-mediated migration and invasion of human breast tumor cells. Mol. Cancer Res. MCR 2009, 7, 1064–1077. [Google Scholar] [CrossRef]
- Popnikolov, N.K.; Dalwadi, B.H.; Thomas, J.D.; Johannes, G.J.; Imagawa, W.T. Association of autotaxin and lysophosphatidic acid receptor 3 with aggressiveness of human breast carcinoma. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2012, 33, 2237–2243. [Google Scholar] [CrossRef]
- Noh, D.Y.; Ahn, S.J.; Lee, R.A.; Park, I.A.; Kim, J.H.; Suh, P.G.; Ryu, S.H.; Lee, K.H.; Han, J.S. Overexpression of phospholipase d1 in human breast cancer tissues. Cancer Lett. 2000, 161, 207–214. [Google Scholar] [CrossRef]
- Kitayama, J.; Shida, D.; Sako, A.; Ishikawa, M.; Hama, K.; Aoki, J.; Arai, H.; Nagawa, H. Over-expression of lysophosphatidic acid receptor-2 in human invasive ductal carcinoma. Breast Cancer Res. BCR 2004, 6, R640–R646. [Google Scholar] [CrossRef] [Green Version]
- Bussard, K.M.; Mutkus, L.; Stumpf, K.; Gomez-Manzano, C.; Marini, F.C. Tumor-associated stromal cells as key contributors to the tumor microenvironment. Breast Cancer Res. BCR 2016, 18, 84. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.; Cha, Y.J.; Koo, J.S. Adipocyte biology in breast cancer: From silent bystander to active facilitator. Prog. Lipid Res. 2018, 69, 11–20. [Google Scholar] [CrossRef]
- Benesch, M.G.; Tang, X.; Dewald, J.; Dong, W.F.; Mackey, J.R.; Hemmings, D.G.; McMullen, T.P.; Brindley, D.N. Tumor-induced inflammation in mammary adipose tissue stimulates a vicious cycle of autotaxin expression and breast cancer progression. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2015, 29, 3990–4000. [Google Scholar] [CrossRef] [Green Version]
- Li, M.; Xiao, D.; Zhang, J.; Qu, H.; Yang, Y.; Yan, Y.; Liu, X.; Wang, J.; Liu, L.; Wang, J.; et al. Expression of lpa2 is associated with poor prognosis in human breast cancer and regulates hif-1alpha expression and breast cancer cell growth. Oncol. Rep. 2016, 36, 3479–3487. [Google Scholar] [CrossRef]
- Finak, G.; Bertos, N.; Pepin, F.; Sadekova, S.; Souleimanova, M.; Zhao, H.; Chen, H.; Omeroglu, G.; Meterissian, S.; Omeroglu, A.; et al. Stromal gene expression predicts clinical outcome in breast cancer. Nat. Med. 2008, 14, 518–527. [Google Scholar] [CrossRef]
- Liu, S.; Umezu-Goto, M.; Murph, M.; Lu, Y.; Liu, W.; Zhang, F.; Yu, S.; Stephens, L.C.; Cui, X.; Murrow, G.; et al. Expression of autotaxin and lysophosphatidic acid receptors increases mammary tumorigenesis, invasion, and metastases. Cancer Cell 2009, 15, 539–550. [Google Scholar] [CrossRef]
- Estrella, V.C.; Eder, A.M.; Liu, S.; Pustilnik, T.B.; Tabassam, F.H.; Claret, F.X.; Gallick, G.E.; Mills, G.B.; Wiener, J.R. Lysophosphatidic acid induction of urokinase plasminogen activator secretion requires activation of the p38mapk pathway. Int. J. Oncol. 2007, 31, 441–449. [Google Scholar] [CrossRef]
- Hao, F.; Tan, M.; Xu, X.; Han, J.; Miller, D.D.; Tigyi, G.; Cui, M.Z. Lysophosphatidic acid induces prostate cancer pc3 cell migration via activation of lpa(1), p42 and p38alpha. Biochim. et Biophys. Acta 2007, 1771, 883–892. [Google Scholar] [CrossRef]
- Kalari, S.; Zhao, Y.; Spannhake, E.W.; Berdyshev, E.V.; Natarajan, V. Role of acylglycerol kinase in lpa-induced il-8 secretion and transactivation of epidermal growth factor-receptor in human bronchial epithelial cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 2009, 296, 328–336. [Google Scholar] [CrossRef]
- Lewis, C.E.; Pollard, J.W. Distinct role of macrophages in different tumor microenvironments. Cancer Res. 2006, 66, 605–612. [Google Scholar] [CrossRef]
- Choi, J.; Gyamfi, J.; Jang, H.; Koo, J.S. The role of tumor-associated macrophage in breast cancer biology. Histol. Histopathol. 2018, 33, 133–145. [Google Scholar]
- David, M.; Ribeiro, J.; Descotes, F.; Serre, C.M.; Barbier, M.; Murone, M.; Clezardin, P.; Peyruchaud, O. Targeting lysophosphatidic acid receptor type 1 with debio 0719 inhibits spontaneous metastasis dissemination of breast cancer cells independently of cell proliferation and angiogenesis. Int. J. Oncol. 2012, 40, 1133–1141. [Google Scholar] [CrossRef]
- Marshall, J.C.; Collins, J.W.; Nakayama, J.; Horak, C.E.; Liewehr, D.J.; Steinberg, S.M.; Albaugh, M.; Vidal-Vanaclocha, F.; Palmieri, D.; Barbier, M.; et al. Effect of inhibition of the lysophosphatidic acid receptor 1 on metastasis and metastatic dormancy in breast cancer. J. Natl. Cancer Inst. 2012, 104, 1306–1319. [Google Scholar] [CrossRef]
- Zhang, H.; Xu, X.; Gajewiak, J.; Tsukahara, R.; Fujiwara, Y.; Liu, J.; Fells, J.I.; Perygin, D.; Parrill, A.L.; Tigyi, G.; et al. Dual activity lysophosphatidic acid receptor pan-antagonist/autotaxin inhibitor reduces breast cancer cell migration in vitro and causes tumor regression in vivo. Cancer Res. 2009, 69, 5441–5449. [Google Scholar] [CrossRef]
- Benesch, M.G.; Tang, X.; Maeda, T.; Ohhata, A.; Zhao, Y.Y.; Kok, B.P.; Dewald, J.; Hitt, M.; Curtis, J.M.; McMullen, T.P.; et al. Inhibition of autotaxin delays breast tumor growth and lung metastasis in mice. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2014, 28, 2655–2666. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Antibody | Company | Clone | Dilution |
|---|---|---|---|
| ATX-LPA pathway-related proteins | |||
| ATX | Abcam, Cambridge, UK | Polyclonal | 1:1000 |
| LPA1 | Abcam, Cambridge, UK | EPR9710 | 1:100 |
| LPA2 | Abcam, Cambridge, UK | Polyclonal | 1:100 |
| LPA3 | Abcam, Cambridge, UK | Polyclonal | 1:250 |
| Molecular subtype-related proteins | |||
| Estrogen receptor (ER) | Thermo Scientific, San Diego, CA, USA | SP1 | 1:100 |
| Progesterone receptor (PR) | DAKO, Glostrup, Denmark | PgR | 1:50 |
| Human epidermal growth factor receptor-2 (HER2) | DAKO, Glostrup, Denmark | Polyclonal | 1:1500 |
| Ki-67 | Abcam, Cambridge, UK | SP6 | 1:100 |
| Parameter | Total (n = 466) (%) | Adipose Stroma (n = 137) (%) | Non-Adipose Stroma (n = 329) (%) | p-Value * | p-Value | |
|---|---|---|---|---|---|---|
| Inflammatory (n = 81) (%) | Fibrous (n = 248) (%) | |||||
| Age (years) | 0.896 | 0.612 | ||||
| ≤50 | 287 (61.6) | 85 (62.0) | 46 (56.8) | 156 (62.6) | ||
| >50 | 179 (38.4) | 52 (38.0) | 35 (43.2) | 92 (37.1) | ||
| Histologic grade | 0.045 | <0.001 | ||||
| I/II | 341 (73.2) | 109 (79.6) | 43 (53.1) | 189 (76.2) | ||
| III | 125 (26.8) | 28 (20.4) | 38 (46.9) | 59 (23.8) | ||
| Tumor stage | 0.910 | 0.948 | ||||
| T1 | 257 (55.2) | 75 (54.7) | 46 (56.8) | 136 (54.8) | ||
| T2/T3 | 209 (44.8) | 62 (45.3) | 35 (43.2) | 112 (45.2) | ||
| Nodal metastasis | 0.936 | 0.537 | ||||
| Absent | 281 (60.3) | 83 (60.6) | 53 (65.4) | 145 (58.5) | ||
| Present | 185 (39.7) | 54 (39.4) | 28 (34.6) | 103 (41.5) | ||
| ER | <0.001 | <0.001 | ||||
| Negative | 115 (24.7) | 19 (13.9) | 39 (48.1) | 57 (23.0) | ||
| Positive | 351 (75.3) | 118 (86.1) | 42 (51.9) | 191 (77.0) | ||
| PR | 0.002 | <0.001 | ||||
| Negative | 141 (30.5) | 28 (20.4) | 39 (48.1) | 75 (30.2) | ||
| Positive | 324 (65.4) | 109 (79.6) | 42 (51.9) | 173 (69.8) | ||
| HER2 status | 0.157 | <0.001 | ||||
| Negative | 387 (83.0) | 119 (86.9) | 55 (67.9) | 213 (85.9) | ||
| Positive | 79 (17.0) | 18 (13.1) | 26 (32.1) | 35 (14.1) | ||
| Molecular subtype | <0.001 | <0.001 | ||||
| Luminal A | 270 (57.9) | 107 (78.1) | 23 (28.4) | 140 (56.5) | ||
| Luminal B | 105 (22.5) | 14 (10.2) | 28 (34.6) | 63 (25.4) | ||
| HER2 | 22 (4.7) | 2 (1.5) | 9 (11.1) | 11 (4.4) | ||
| Triple negative breast cancer (TNBC) | 69 (14.8) | 14 (10.2) | 21 (25.9) | 34 (13.7) | ||
| Parameter | Total (n = 466) (%) | Adipose Stroma (n = 137) (%) | Non-Adipose Stroma (n = 329) (%) | p-Value * | p-Value | |
|---|---|---|---|---|---|---|
| Inflammatory (n = 81) (%) | Fibrous (n = 248) (%) | |||||
| ATX | 0.086 | 0.062 | ||||
| Negative | 243 (52.1) | 63 (46.0) | 38 (46.9) | 142 (57.3) | ||
| Positive | 223 (47.9) | 74 (54.0) | 43 (53.1) | 106 (42.7) | ||
| ATX (S) | 0.357 | 0.511 | ||||
| Negative | 390 (83.7) | 118 (86.1) | 69 (85.2) | 203 (81.9) | ||
| Positive | 76 (16.3) | 19 (13.9) | 12 (14.8) | 45 (18.1) | ||
| LPA1 | 0.514 | 0.363 | ||||
| Negative | 249 (53.4) | 70 (51.1) | 49 (60.5) | 130 (52.4) | ||
| Positive | 217 (46.6) | 67 (48.9) | 32 (39.5) | 118 (47.6) | ||
| LPA1 (S) | 0.854 | 0.951 | ||||
| Negative | 382 (82.0) | 113 (82.5) | 67 (82.7) | 202 (81.5) | ||
| Positive | 84 (18.0) | 24 (17.5) | 14 (17.3) | 46 (18.5) | ||
| LPA2 | <0.001 | <0.001 | ||||
| Negative | 409 (87.8) | 85 (62.0) | 80 (98.8) | 244 (98.4) | ||
| Positive | 57 (12.2) | 52 (38.0) | 1 (1.2) | 4 (1.6) | ||
| LPA 3 | 0.451 | 0.121 | ||||
| Negative | 436 (93.6) | 130 (94.9) | 79 (97.5) | 227 (91.5) | ||
| Positive | 30 (6.4) | 7 (5.1) | 2 (2.5) | 21 (8.5) | ||
| LPA 3 (S) | 0.027 | <0.001 | ||||
| Negative | 304 (65.2) | 79 (57.7) | 34 (42.0) | 191 (77.0) | ||
| Positive | 162 (34.8) | 58 (42.3) | 47 (58.0) | 57 (23.0) | ||
| Parameters | ATX (S) | LPA1 | LPA1 (S) | LPA2 | LPA3 | LPA3 (S) |
|---|---|---|---|---|---|---|
| ATX | ||||||
| r-value | 0.348 | 0.367 | 0.125 | 0.159 | −0.036 | 0.081 |
| p-value | <0.001 | <0.001 | 0.007 | 0.001 | 0.443 | 0.082 |
| ATX (S) | ||||||
| r-value | 0.141 | 0.352 | 0.090 | −0.023 | 0.121 | |
| p-value | 0.002 | <0.001 | 0.051 | 0.616 | 0.009 | |
| LPA1 | ||||||
| r-value | 0.273 | 0.221 | 0.086 | 0.216 | ||
| p-value | <0.001 | <0.001 | 0.065 | <0.001 | ||
| LPA1 (S) | ||||||
| r-value | 0.085 | −0.017 | 0.291 | |||
| p-value | 0.066 | 0.715 | <0.001 | |||
| LPA2 | ||||||
| r value | 0.008 | 0.079 | ||||
| p-value | 0.871 | 0.089 | ||||
| LPA3 | ||||||
| r-value | −0.064 | |||||
| p-value | 0.165 |
| Parameter | CD68-Positive CLS | CD163-Positive CLS | ||||
|---|---|---|---|---|---|---|
| Absent (n = 114) (%) | Present (n = 23) (%) | p-Value | Absent (n = 119) (%) | Present (n = 18) (%) | p-Value | |
| ATX | 0.791 | 0.888 | ||||
| Negative | 53 (46.5) | 10 (43.5) | 55 (46.2) | 8 (44.4) | ||
| Positive | 61 (53.5) | 13 (56.5) | 64 (53.8) | 10 (55.6) | ||
| ATX (S) | 0.063 | 0.010 | ||||
| Negative | 101 (88.6) | 17 (73.9) | 106 (89.1) | 12 (66.7) | ||
| Positive | 13 (11.4) | 6 (26.1) | 13 (10.9) | 6 (33.3) | ||
| LPA 1 | 0.910 | 0.545 | ||||
| Negative | 58 (50.9) | 12 (52.2) | 62 (52.1) | 8 (44.4) | ||
| Positive | 56 (49.1) | 11 (47.8) | 57 (47.9) | 10 (55.6) | ||
| LPA 1 (S) | 0.017 | 0.219 | ||||
| Negative | 98 (86.0) | 15 (65.2) | 100 (84.0) | 13 (72.2) | ||
| Positive | 16 (14.0) | 8 (34.8) | 19 (16.0) | 5 (27.8) | ||
| LPA 2 | 0.731 | 0.665 | ||||
| Negative | 70 (61.4) | 15 (65.2) | 73 (61.3) | 12 (66.7) | ||
| Positive | 44 (38.6) | 8 (34.8) | 46 (38.7) | 6 (33.3) | ||
| LPA 3 | 0.222 | 0.291 | ||||
| Negative | 107 (93.9) | 23 (100.0) | 112 (94.1) | 18 (100.0) | ||
| Positive | 7 (6.1) | 0 (0.0) | 7 (5.9) | 0 (0.0) | ||
| LPA 3 (S) | 0.004 | 0.009 | ||||
| Negative | 72 (63.2) | 7 (30.4) | 74 (62.2) | 5 (27.8) | ||
| Positive | 42 (36.8) | 16 (69.6) | 45 (37.8) | 13 (72.2) | ||
| Parameter | The Number of CD68-Positive Macrophages in Adipocyte | The Number of CD163-Positive Macrophages in Adipocyte | ||
|---|---|---|---|---|
| Median (Range) | p-Value | Median (Range) | p-Value | |
| ATX | 0.234 | 0.526 | ||
| Negative | 5 (0–42) | 13 (0–79) | ||
| Positive | 1.5 (0–41) | 12 (0–62) | ||
| ATX (S) | 0.179 | 0.003 | ||
| Negative | 2 (0–42) | 12 (0–62) | ||
| Positive | 8 (0–32) | 20 (0–79) | ||
| LPA1 | 0.586 | 0.179 | ||
| Negative | 2 (0–42) | 10 (0–79) | ||
| Positive | 4 (0–41) | 13 (0–62) | ||
| LPA1 (S) | 0.066 | 0.094 | ||
| Negative | 2 (0–42) | 12 (0–79) | ||
| Positive | 7 (0–37) | 14 (0–52) | ||
| LPA 2 | 0.395 | 0.943 | ||
| Negative | 3 (0–42) | 12 (0–79) | ||
| Positive | 3 (0–36) | 12.5 (0–57) | ||
| LPA 3 | 0.350 | 0.576 | ||
| Negative | 3 (0–42) | 12 (0–79) | ||
| Positive | 3 (0–9) | 12 (0–20) | ||
| LPA 3 (S) | <0.001 | <0.001 | ||
| Negative | 0 (0–41) | 8 (0–79) | ||
| Positive | 8 (0–42) | 16.5 (0–62) | ||
| Parameter | Number of Patients/Recurrence/Death | Disease-Free Survival | Overall Survival | ||
|---|---|---|---|---|---|
| Mean Survival (95% CI) Months | p-Value | Mean Survival (95% CI) Months | p-Value | ||
| ATX | 0.842 | 0.649 | |||
| Negative | 243/13/22 | 119 (117–122) | 117 (114–120) | ||
| Positive | 223/13/18 | 133 (129–136) | 130 (125–135) | ||
| ATX (S) | 0.093 | 0.868 | |||
| Negative | 390/25/34 | 132 (129–134) | 129 (126–133) | ||
| Positive | 76/1/6 | 107 (106–108) | 104 (101–107) | ||
| LPA1 | 0.115 | 0.888 | |||
| Negative | 249/18/22 | 131 (128–135) | 129 (125–134) | ||
| Positive | 217/8/18 | 113 (111–115) | 110 (107–112) | ||
| LPA1 (S) | 0.152 | 0.544 | |||
| Negative | 382/24/34 | 132 (129–135) | 129 (125–133) | ||
| Positive | 84/2/6 | 113 (111–115) | 111 (108–114) | ||
| LPA 2 | 0.528 | 0.413 | |||
| Negative | 409/22/37 | 133 (131–135) | 129 (126–133) | ||
| Positive | 57/4/3 | 110 (105–115) | 112 (108–116) | ||
| LPA 3 | 0.607 | 0.770 | |||
| Negative | 436/25/38 | 133 (130–135) | 130 (127–133) | ||
| Positive | 30/1/2 | 112 (105–119) | 109 (101–118) | ||
| LPA 3 (S) | 0.661 | 0.504 | |||
| Negative | 304/16/28 | 133 (130–136) | 130 (127–133) | ||
| Positive | 162/10/12 | 112 (109–115) | 111 (108–114) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cha, Y.J.; Koo, J.S. Expression of Autotaxin–Lysophosphatidate Signaling-Related Proteins in Breast Cancer with Adipose Stroma. Int. J. Mol. Sci. 2019, 20, 2102. https://doi.org/10.3390/ijms20092102
Cha YJ, Koo JS. Expression of Autotaxin–Lysophosphatidate Signaling-Related Proteins in Breast Cancer with Adipose Stroma. International Journal of Molecular Sciences. 2019; 20(9):2102. https://doi.org/10.3390/ijms20092102
Chicago/Turabian StyleCha, Yoon Jin, and Ja Seung Koo. 2019. "Expression of Autotaxin–Lysophosphatidate Signaling-Related Proteins in Breast Cancer with Adipose Stroma" International Journal of Molecular Sciences 20, no. 9: 2102. https://doi.org/10.3390/ijms20092102





