Extracellular Vesicles Are More Potent Than Adipose Mesenchymal Stromal Cells to Exert an Anti-Fibrotic Effect in an In Vitro Model of Systemic Sclerosis
Abstract
:1. Introduction
2. Results
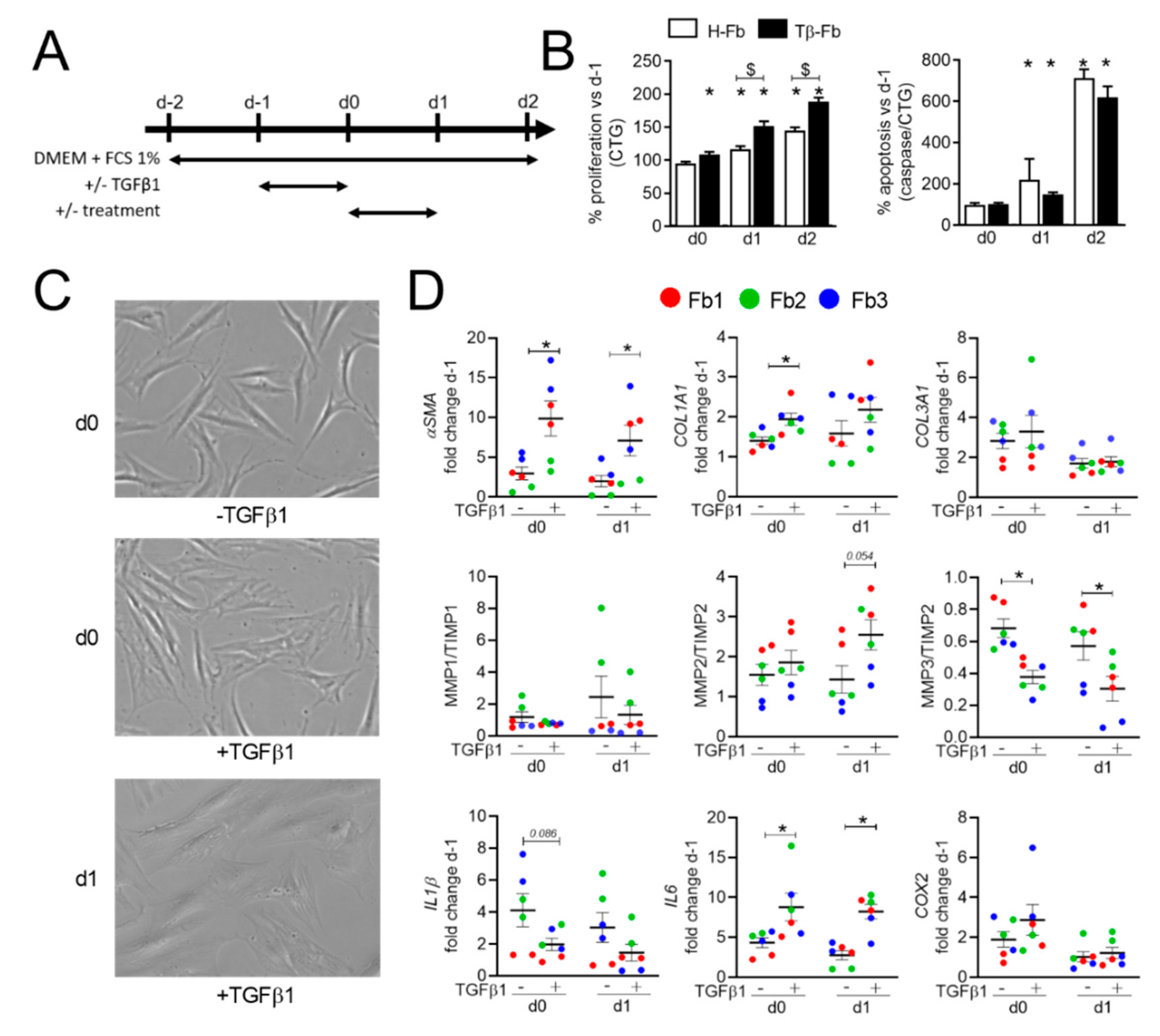
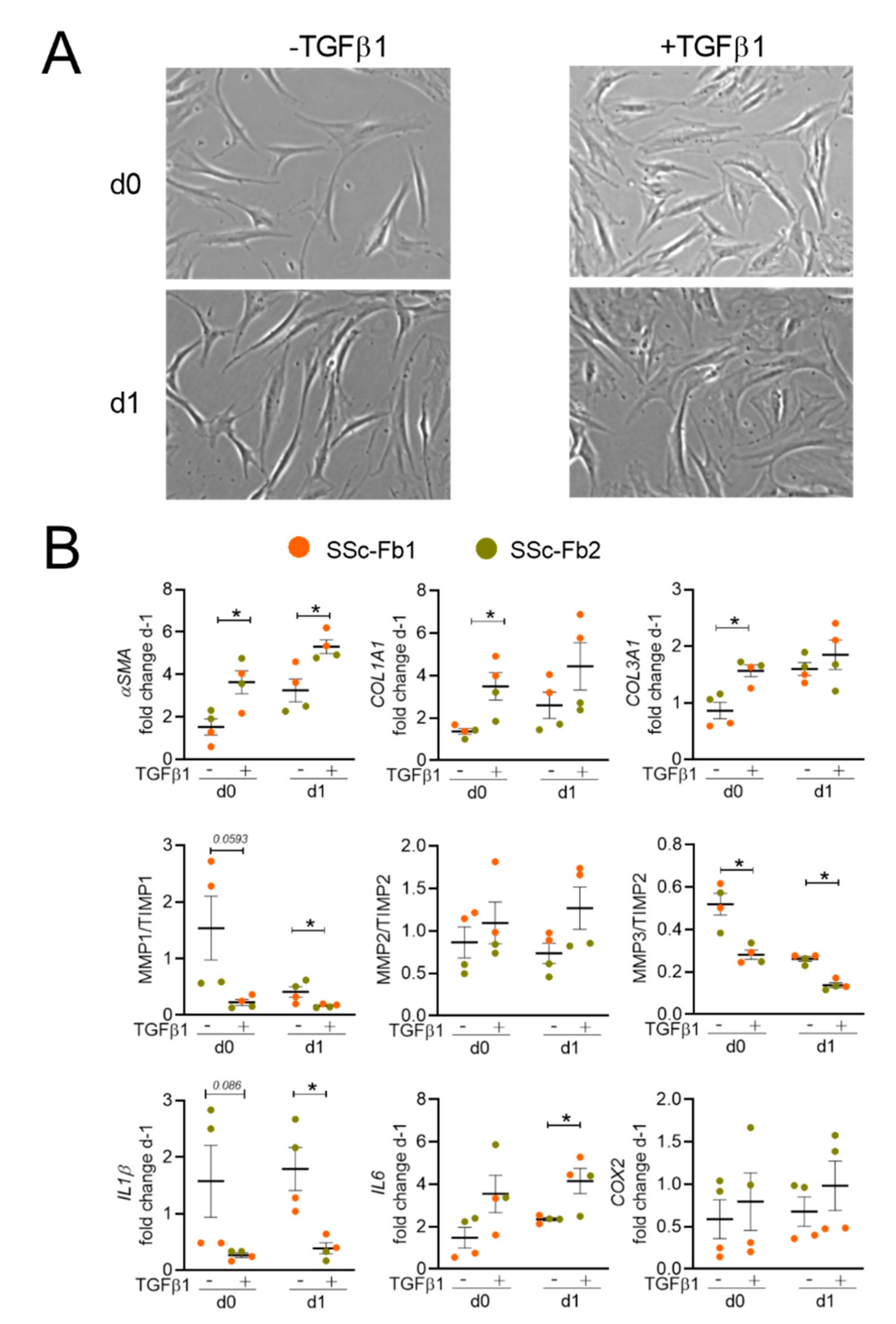
2.1. TGFβ1 Upregulates the Myofibroblastic Signature in Both Healthy and SSc Human Fibroblasts
2.2. TGFβ1-Induced Healthy and SSc Fibroblasts Display a Similar Myofibroblastic Phenotype
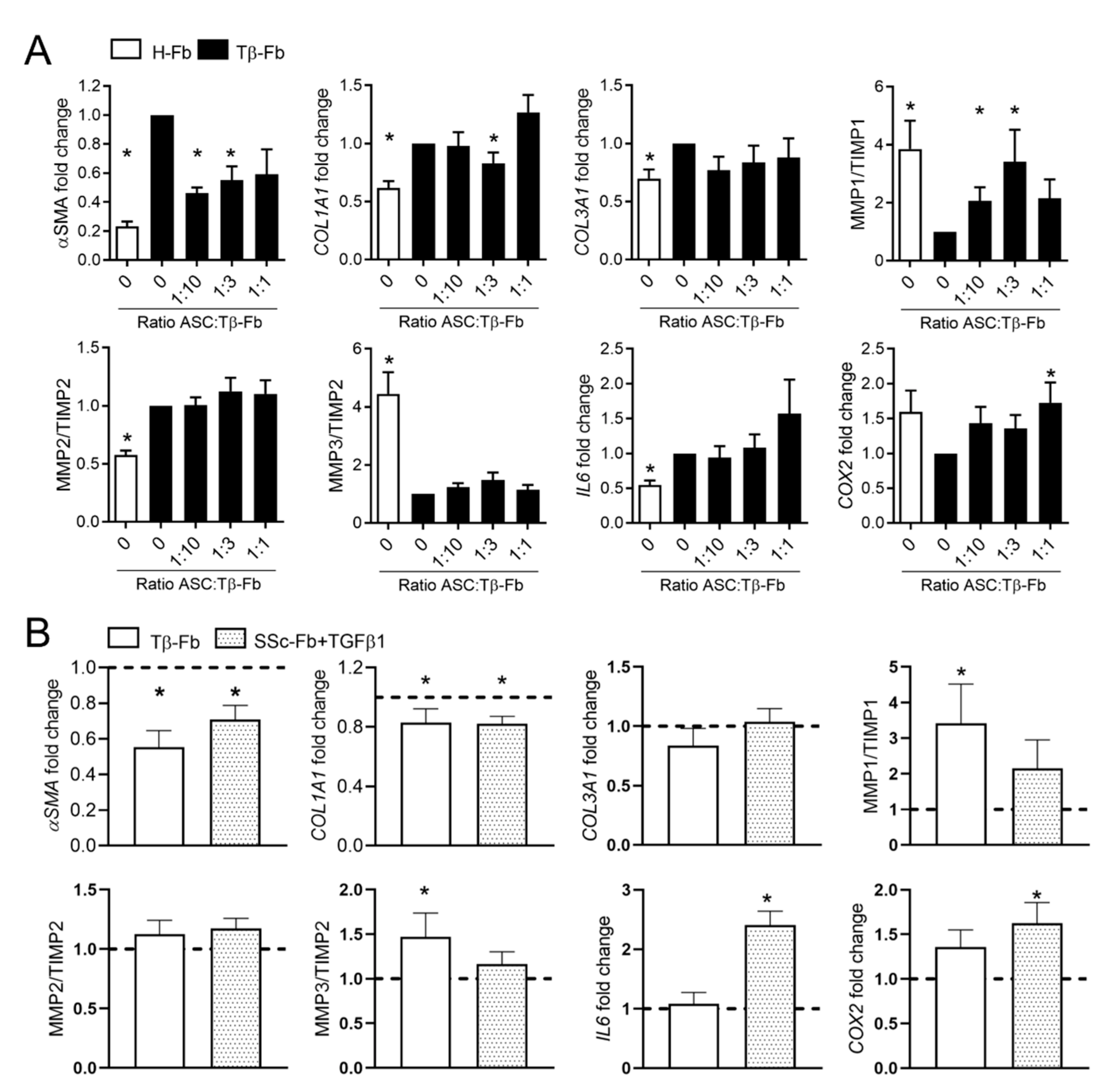
2.3. ASCs Partly Reversed the Myofibroblastic Phenotype of TGFβ1-Stimulated Fibroblasts
2.4. ASC Secretome and Derived EVs Are More Effective Than Parental Cells for Improving the Myofibroblastic Phenotype
3. Discussion
4. Materials and Methods
4.1. Cell Isolation and Expansion
4.2. Production and Isolation of EVs
4.3. In Vitro Model of TGFβ1-Induced Myofibroblasts
4.4. Proliferation and Apoptosis Quantification
4.5. RNA Extraction and RT-qPCR
4.6. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hughes, L.C.; Archer, C.W.; Ap Gwynn, I. The ultrastructure of mouse articular cartilage: Collagen orientation and implications for tissue functionality. A polarised light and scanning electron microscope study and review. Eur. Cells Mater. 2005, 9, 68–84. [Google Scholar] [CrossRef] [PubMed]
- Varga, J.; Whitfield, M.L. Transforming growth factor-beta in systemic sclerosis (scleroderma). Front. Biosci. 2009, 1, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.J.; Lerch, T.F.; Cook, R.W.; Jardetzky, T.S.; Woodruff, T.K. The structural basis of TGF-beta, bone morphogenetic protein, and activin ligand binding. Reproduction 2006, 132, 179–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massague, J. TGF-beta signal transduction. Annu. Rev. Biochem. 1998, 67, 753–791. [Google Scholar] [CrossRef] [PubMed]
- Milano, A.; Pendergrass, S.A.; Sargent, J.L.; George, L.K.; McCalmont, T.H.; Connolly, M.K.; Whitfield, M.L. Molecular subsets in the gene expression signatures of scleroderma skin. PLoS ONE 2008, 3, e2696. [Google Scholar] [CrossRef]
- Whitfield, M.L.; Finlay, D.R.; Murray, J.I.; Troyanskaya, O.G.; Chi, J.T.; Pergamenschikov, A.; McCalmont, T.H.; Brown, P.O.; Botstein, D.; Connolly, M.K. Systemic and cell type-specific gene expression patterns in scleroderma skin. Proc. Natl. Acad. Sci. USA 2003, 100, 12319–12324. [Google Scholar] [CrossRef] [Green Version]
- Corallo, C.; Pinto, A.M.; Renieri, A.; Cheleschi, S.; Fioravanti, A.; Cutolo, M.; Soldano, S.; Nuti, R.; Giordano, N. Altered expression of RXFP1 receptor contributes to the inefficacy of relaxin-based anti-fibrotic treatments in systemic sclerosis. Clin. Exp. Rheumatol. 2019, 37, 69–75. [Google Scholar]
- Haak, A.J.; Tsou, P.S.; Amin, M.A.; Ruth, J.H.; Campbell, P.; Fox, D.A.; Khanna, D.; Larsen, S.D.; Neubig, R.R. Targeting the myofibroblast genetic switch: Inhibitors of myocardin-related transcription factor/serum response factor-regulated gene transcription prevent fibrosis in a murine model of skin injury. J. Pharmacol. Exp. Ther. 2014, 349, 480–486. [Google Scholar] [CrossRef] [Green Version]
- Hinchcliff, M.; Huang, C.C.; Ishida, W.; Fang, F.; Lee, J.; Jafari, N.; Wilkes, M.; Bhattacharyya, S.; Leof, E.; Varga, J. Imatinib mesylate causes genome-wide transcriptional changes in systemic sclerosis fibroblasts in vitro. Clin. Exp. Rheumatol. 2012, 30, S86–S96. [Google Scholar]
- Liu, T.; Zhang, J.; Zhang, J.; Mu, X.; Su, H.; Hu, X.; Liu, W.; Zhao, E.; Li, W. RNA interference against platelet-derived growth factor receptor alpha mRNA inhibits fibroblast transdifferentiation in skin lesions of patients with systemic sclerosis. PLoS ONE 2013, 8, e60414. [Google Scholar]
- Chizzolini, C.; Brembilla, N.C.; Montanari, E.; Truchetet, M.E. Fibrosis and immune dysregulation in systemic sclerosis. Autoimmun. Rev. 2011, 10, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Altorok, N.; Wang, Y.; Kahaleh, B. Endothelial dysfunction in systemic sclerosis. Curr. Opin. Rheumatol. 2014, 26, 615–620. [Google Scholar] [CrossRef]
- Rozier, P.; Maria, A.; Goulabchand, R.; Jorgensen, C.; Guilpain, P.; Noel, D. Mesenchymal Stem Cells in Systemic Sclerosis: Allogenic or Autologous Approaches for Therapeutic Use? Front. Immunol. 2018, 9, 2938. [Google Scholar] [CrossRef] [Green Version]
- Maria, A.T.; Toupet, K.; Bony, C.; Pirot, N.; Vozenin, M.C.; Petit, B.; Roger, P.; Batteux, F.; Le Quellec, A.; Jorgensen, C.; et al. Antifibrotic, Antioxidant, and Immunomodulatory Effects of Mesenchymal Stem Cells in HOCl-Induced Systemic Sclerosis. Arthritis Rheumatol. 2016, 68, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Maria, A.T.; Toupet, K.; Maumus, M.; Fonteneau, G.; Le Quellec, A.; Jorgensen, C.; Guilpain, P.; Noel, D. Human adipose mesenchymal stem cells as potent anti-fibrosis therapy for systemic sclerosis. J. Autoimmun. 2016, 70, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Maumus, M.; Rozier, P.; Boulestreau, J.; Jorgensen, C.; Noel, D. Mesenchymal Stem Cell-Derived Extracellular Vesicles: Opportunities and Challenges for Clinical Translation. Front. Bioeng. Biotechnol. 2020, 8, 997. [Google Scholar] [CrossRef]
- Rozier, P.; Maumus, M.; Maria, A.T.J.; Toupet, K.; Lai-Kee-Him, J.; Jorgensen, C.; Guilpain, P.; Noel, D. Mesenchymal stromal cells-derived extracellular vesicles alleviate systemic sclerosis via miR-29a-3p. J. Autoimmun. 2021, 121, 102660. [Google Scholar] [CrossRef] [PubMed]
- Dooley, A.; Shi-Wen, X.; Aden, N.; Tranah, T.; Desai, N.; Denton, C.P.; Abraham, D.J.; Bruckdorfer, R. Modulation of collagen type I, fibronectin and dermal fibroblast function and activity, in systemic sclerosis by the antioxidant epigallocatechin-3-gallate. Rheumatology 2010, 49, 2024–2036. [Google Scholar] [CrossRef] [Green Version]
- Mori, Y.; Ishida, W.; Bhattacharyya, S.; Li, Y.; Platanias, L.C.; Varga, J. Selective inhibition of activin receptor-like kinase 5 signaling blocks profibrotic transforming growth factor beta responses in skin fibroblasts. Arthritis Rheum. 2004, 50, 4008–4021. [Google Scholar] [CrossRef]
- Wu, M.; Melichian, D.S.; Chang, E.; Warner-Blankenship, M.; Ghosh, A.K.; Varga, J. Rosiglitazone abrogates bleomycin-induced scleroderma and blocks profibrotic responses through peroxisome proliferator-activated receptor-gamma. Am. J. Pathol. 2009, 174, 519–533. [Google Scholar] [CrossRef] [Green Version]
- Avouac, J.; Clemessy, M.; Distler, J.H.; Gasc, J.M.; Ruiz, B.; Vacher-Lavenu, M.C.; Wipff, J.; Kahan, A.; Boileau, C.; Corvol, P.; et al. Enhanced expression of ephrins and thrombospondins in the dermis of patients with early diffuse systemic sclerosis: Potential contribution to perturbed angiogenesis and fibrosis. Rheumatology 2011, 50, 1494–1504. [Google Scholar] [CrossRef] [Green Version]
- Dufour, A.M.; Alvarez, M.; Russo, B.; Chizzolini, C. Interleukin-6 and Type-I Collagen Production by Systemic Sclerosis Fibroblasts Are Differentially Regulated by Interleukin-17A in the Presence of Transforming Growth Factor-Beta 1. Front. Immunol. 2018, 9, 1865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kikuchi, K.; Kadono, T.; Ihn, H.; Sato, S.; Igarashi, A.; Nakagawa, H.; Tamaki, K.; Takehara, K. Growth regulation in scleroderma fibroblasts: Increased response to transforming growth factor-beta 1. J. Investig. Dermatol. 1995, 105, 128–132. [Google Scholar] [CrossRef] [Green Version]
- Chaigne, B.; Clary, G.; Le Gall, M.; Dumoitier, N.; Fernandez, C.; Lofek, S.; Chafey, P.; Moinzadeh, P.; Krieg, T.; Denton, C.P.; et al. Proteomic Analysis of Human Scleroderma Fibroblasts Response to Transforming Growth Factor-ss. Proteom. Clin. Appl. 2019, 13, e1800069. [Google Scholar] [CrossRef] [PubMed]
- Chellini, F.; Tani, A.; Vallone, L.; Nosi, D.; Pavan, P.; Bambi, F.; Zecchi-Orlandini, S.; Sassoli, C. Platelet-Rich Plasma and Bone Marrow-Derived Mesenchymal Stromal Cells Prevent TGF-beta1-Induced Myofibroblast Generation but Are Not Synergistic when Combined: Morphological in vitro Analysis. Cells Tissues Organs 2018, 206, 283–295. [Google Scholar] [CrossRef] [PubMed]
- Hiwatashi, N.; Bing, R.; Kraja, I.; Branski, R.C. Mesenchymal stem cells have antifibrotic effects on transforming growth factor-beta1-stimulated vocal fold fibroblasts. Laryngoscope 2017, 127, E35–E41. [Google Scholar] [CrossRef]
- Li, X.; Wang, H.; Xu, W. HGF and bFGF Secreted by Adipose-Derived Mesenchymal Stem Cells Revert the Fibroblast Phenotype Caused by Vocal Fold Injury in a Rat Model. J. Voice 2020, in press. [Google Scholar] [CrossRef]
- Mias, C.; Lairez, O.; Trouche, E.; Roncalli, J.; Calise, D.; Seguelas, M.H.; Ordener, C.; Piercecchi-Marti, M.D.; Auge, N.; Salvayre, A.N.; et al. Mesenchymal stem cells promote matrix metalloproteinase secretion by cardiac fibroblasts and reduce cardiac ventricular fibrosis after myocardial infarction. Stem Cells 2009, 27, 2734–2743. [Google Scholar] [CrossRef] [PubMed]
- Verhoekx, J.S.N.; Mudera, V.; Walbeehm, E.T.; Hovius, S.E.R. Adipose-derived stem cells inhibit the contractile myofibroblast in Dupuytren’s disease. Plast. Reconstr. Surg. 2013, 132, 1139–1148. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Hu, X.; Xie, X.; He, A.; Liu, X.; Wang, J.A. Effects of mesenchymal stem cells on matrix metalloproteinase synthesis in cardiac fibroblasts. Exp. Biol. Med. 2011, 236, 1197–1204. [Google Scholar] [CrossRef]
- Chang, J.W.; Tsai, H.L.; Chen, C.W.; Yang, H.W.; Yang, A.H.; Yang, L.Y.; Wang, P.S.; Ng, Y.Y.; Lin, T.L.; Lee, O.K. Conditioned mesenchymal stem cells attenuate progression of chronic kidney disease through inhibition of epithelial-to-mesenchymal transition and immune modulation. J. Cell. Mol. Med. 2012, 16, 2935–2949. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhao, H.; Qi, C.; Zeng, Y.; Xu, F.; Du, Y. Direct intercellular communications dominate the interaction between adipose-derived MSCs and myofibroblasts against cardiac fibrosis. Protein Cell 2015, 6, 735–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noronha, N.C.; Mizukami, A.; Caliari-Oliveira, C.; Cominal, J.G.; Rocha, J.L.M.; Covas, D.T.; Swiech, K.; Malmegrim, K.C.R. Priming approaches to improve the efficacy of mesenchymal stromal cell-based therapies. Stem Cell Res. Ther. 2019, 10, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, S.; Xu, C.; Zhang, Y.; Xue, C.; Yang, C.; Bi, H.; Qian, X.; Wu, M.; Ji, K.; Zhao, Y.; et al. Umbilical Cord-Derived Mesenchymal Stem Cell-Derived Exosomal MicroRNAs Suppress Myofibroblast Differentiation by Inhibiting the Transforming Growth Factor-beta/SMAD2 Pathway During Wound Healing. Stem Cells Transl. Med. 2016, 5, 1425–1439. [Google Scholar] [CrossRef] [PubMed]
- Shao, L.; Zhang, Y.; Lan, B.; Wang, J.; Zhang, Z.; Zhang, L.; Xiao, P.; Meng, Q.; Geng, Y.J.; Yu, X.Y.; et al. MiRNA-Sequence Indicates That Mesenchymal Stem Cells and Exosomes Have Similar Mechanism to Enhance Cardiac Repair. BioMed Res. Int. 2017, 2017, 4150705. [Google Scholar] [CrossRef]
- Velier, M.; Simoncini, S.; Abellan, M.; Francois, P.; Eap, S.; Lagrange, A.; Bertrand, B.; Daumas, A.; Granel, B.; Delorme, B.; et al. Adipose-Derived Stem Cells from Systemic Sclerosis Patients Maintain Pro-Angiogenic and Antifibrotic Paracrine Effects In Vitro. J. Clin. Med. 2019, 8, 1979. [Google Scholar] [CrossRef] [Green Version]
- Bony, C.; Cren, M.; Domergue, S.; Toupet, K.; Jorgensen, C.; Noel, D. Adipose Mesenchymal Stem Cells Isolated after Manual or Water-jet-Assisted Liposuction Display Similar Properties. Front. Immunol. 2016, 6, 655. [Google Scholar] [CrossRef] [Green Version]


| Gene | Forward Sequence | Reverse Sequence |
|---|---|---|
| ACTA2 (αSMA) | CATCGGGATGGAGTCTGCTG | AGAAGCATTTGCGGTGGACA |
| COL1A1 | CCTGGATGCCATCAAAGTCT | CGCCATACTCGAACTGGAAT |
| COL3A1 | CGCCCTCCTAATGGTCAAGG | AGGGCCTGAAGGACCAGCTT |
| COX2 | CGGTGAAACTCTGGCTAGACAG | GCAAACCGTAGATGCTCAGGGA |
| IL-1Β | TGGCTTATTACAGTGGCAATGAGGAT | TCGGAGATTCGTAGCTGGATGCC |
| IL-6 | AGACAGCCACTCACCTCTTCAG | TTCTGCCAGTGCCTCTTTGCTG |
| MMP1 | AGGCCCAGGTATTGGAGGGGA | GCCGATGGGCTGGACAGGATT |
| MMP2 | GCCGTCGCCCATCATCAAGTT | ATAGAAGGTGTTCAGGTATTGCACTG |
| MMP3 | GTACCCACGGAACCTGTCCCTC | TTGCGCCAAAAGTGCCTGTCT |
| RPS9 | GATTACATCCTGGGCCTGAA | ATGAAGGACGGGATGTTCAC |
| TIMP1 | CCGGGGCTTCACCAAGACCT | AGGCAAGGTGACGGGACTGG |
| TIMP2 | AGGGCCAAAGCGGTCAGTGA | AACGTCCAGCGAGACCCCAC |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rozier, P.; Maumus, M.; Bony, C.; Maria, A.T.J.; Sabatier, F.; Jorgensen, C.; Guilpain, P.; Noël, D. Extracellular Vesicles Are More Potent Than Adipose Mesenchymal Stromal Cells to Exert an Anti-Fibrotic Effect in an In Vitro Model of Systemic Sclerosis. Int. J. Mol. Sci. 2021, 22, 6837. https://doi.org/10.3390/ijms22136837
Rozier P, Maumus M, Bony C, Maria ATJ, Sabatier F, Jorgensen C, Guilpain P, Noël D. Extracellular Vesicles Are More Potent Than Adipose Mesenchymal Stromal Cells to Exert an Anti-Fibrotic Effect in an In Vitro Model of Systemic Sclerosis. International Journal of Molecular Sciences. 2021; 22(13):6837. https://doi.org/10.3390/ijms22136837
Chicago/Turabian StyleRozier, Pauline, Marie Maumus, Claire Bony, Alexandre Thibault Jacques Maria, Florence Sabatier, Christian Jorgensen, Philippe Guilpain, and Danièle Noël. 2021. "Extracellular Vesicles Are More Potent Than Adipose Mesenchymal Stromal Cells to Exert an Anti-Fibrotic Effect in an In Vitro Model of Systemic Sclerosis" International Journal of Molecular Sciences 22, no. 13: 6837. https://doi.org/10.3390/ijms22136837






