Liquid Biopsy: A New Translational Diagnostic and Monitoring Tool for Musculoskeletal Tumors
Abstract
:1. Introduction
1.1. Soft Tissue and Bone Sarcomas
1.2. Liquid Biopsy
1.3. Research Strategy
1.4. Inclusion Criteria and Study Selection
1.5. Data Extracted
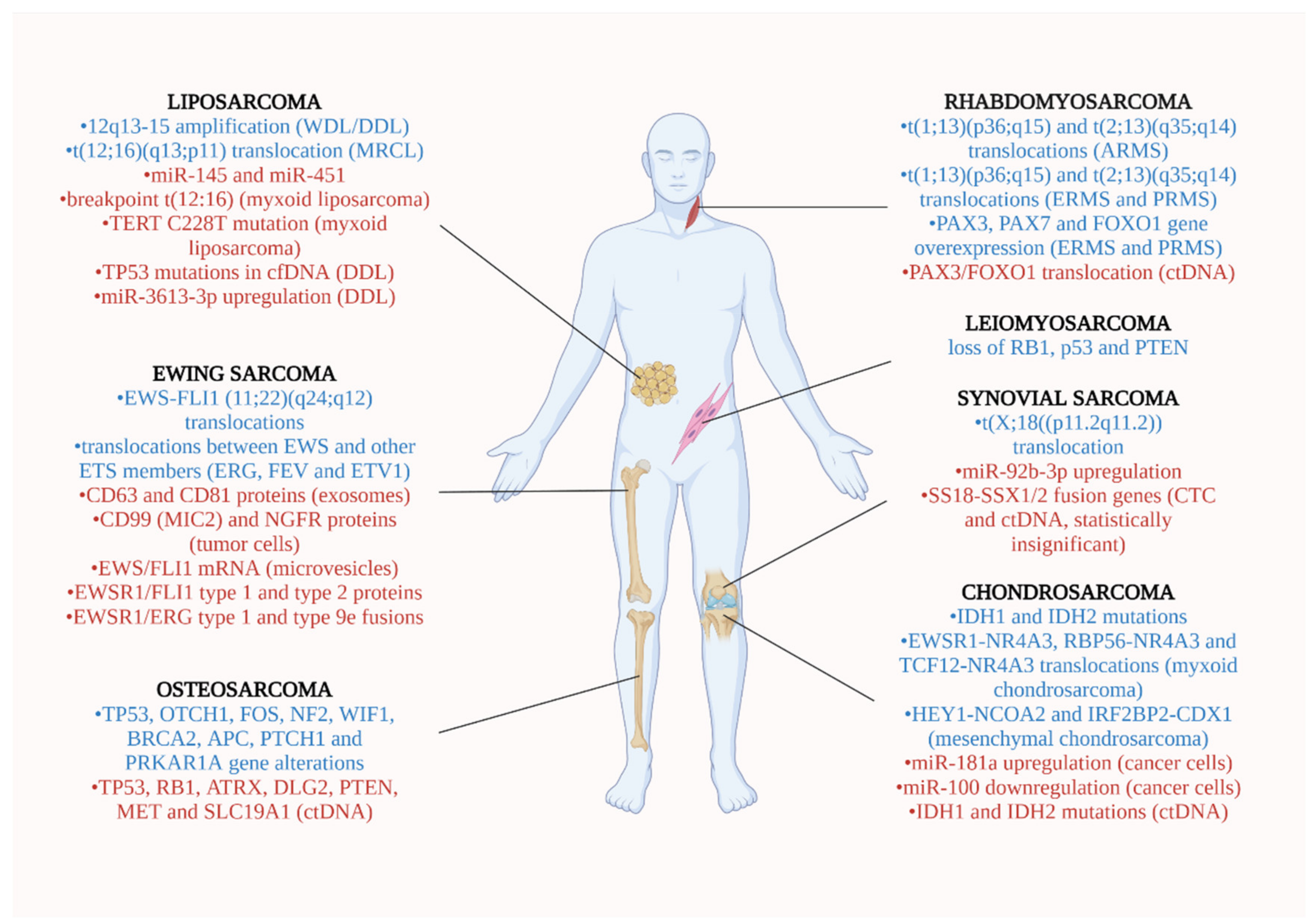
2. Soft Tissue Sarcomas
2.1. Liposarcoma (LPS)
2.2. Leiomyosarcoma (LMS)
2.3. Ewing Sarcoma (ES)
2.4. Rhabdomyosarcoma (RMS)
2.5. Synovial Sarcoma (SS)
3. Bone Sarcomas
3.1. Osteosarcoma (OS)
3.2. Chondrosarcoma (CS)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| OS | osteosarcoma |
| NGS | Next-generation sequencing |
| FISH | fluorescence in situ hybridization |
| CTCs | circulating tumor cells |
| IDH1 | Isocitrate dehydrogenase type 1 |
| IDH2 | Isocitrate dehydrogenase type 2 |
| miR | micro-RNA |
| ctDNA | circulating tumor DNA |
| cfDNA | cell-free DNA |
| STS | soft tissue sarcomas |
| CTC | circulating tumor cells |
| DDL | dedifferentiated liposarcoma |
| CGP | comprehensive genomic profiling |
| ptDNA | plasma tumor DNA |
| PDX | patient derived xenograft |
| ESFT | Ewing Sarcoma Family Tumors |
| sEVs | Small ESFT-associated extracellular vesicles |
| ARMS | alveolar rhabdomyosarcoma |
| RMS | rhabdomyosarcoma |
| ULP-WGS | ultralow passage whole-genome sequencing |
| SS | synovial sarcoma |
References
- Cancer Stat Facts: Soft Tissue including Heart Cancer. Available online: https://seer.cancer.gov/statfacts/html/soft.html (accessed on 21 October 2021).
- Bone Cancer (Sarcoma of Bone): Statistics. Available online: https://www.cancer.net/cancer-types/bone-cancer-sarcoma-bone/statistics (accessed on 21 October 2021).
- Kim, S.H.; Shin, K.H.; Moon, S.H.; Jang, J.; Kim, H.S.; Suh, J.S.; Yang, W.I. Reassessment of alkaline phosphatase as serum tumor marker with high specificity in osteosarcoma. Cancer Med. 2017, 6, 1311–1322. [Google Scholar] [CrossRef]
- Nakano, K.; Takahashi, S. Current molecular targeted therapies for bone and soft tissue sarcomas. Int. J. Mol. Sci. 2018, 19, 739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geyer, P.E.; Holdt, L.M.; Teupser, D.; Mann, M. Revisiting biomarker discovery by plasma proteomics. Mol. Syst. Biol. 2017, 13, 942. [Google Scholar] [CrossRef]
- Perez-Gracia, J.L.; Sanmamed, M.F.; Bosch, A.; Patiño-Garcia, A.; Schalper, K.A.; Segura, V.; Bellmunt, J.; Tabernero, J.; Sweeney, C.J.; Choueiri, T.K.; et al. Strategies to design clinical studies to identify predictive biomarkers in cancer research. Cancer Treat. Rev. 2017, 53, 79–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heidrich, I.; Ačkar, L.; Mossahebi Mohammadi, P.; Pantel, K. Liquid biopsies: Potential and challenges. Int. J. Cancer 2021, 148, 528–545. [Google Scholar] [CrossRef]
- Siravegna, G.; Mussolin, B.; Venesio, T.; Marsoni, S.; Seoane, J.; Dive, C.; Papadopoulos, N.; Kopetz, S.; Corcoran, R.B.; Siu, L.L.; et al. How liquid biopsies can change clinical practice in oncology. Ann. Oncol. 2019, 30, 1580–1590. [Google Scholar] [CrossRef] [Green Version]
- Palacín-Aliana, I.; García-Romero, N.; Asensi-Puig, A.; Carrión-Navarro, J.; González-Rumayor, V.; Ayuso-Sacido, Á. Clinical utility of liquid biopsy-based actionable mutations detected via ddpcr. Biomedicines 2021, 9, 906. [Google Scholar] [CrossRef]
- Kilgour, E.; Rothwell, D.G.; Brady, G.; Dive, C. Liquid Biopsy-Based Biomarkers of Treatment Response and Resistance. Cancer Cell 2020, 37, 485–495. [Google Scholar] [CrossRef]
- Gerber, T.; Taschner-Mandl, S.; Saloberger-Sindhöringer, L.; Popitsch, N.; Heitzer, E.; Witt, V.; Geyeregger, R.; Hutter, C.; Schwentner, R.; Ambros, I.M.; et al. Assessment of Pre-Analytical Sample Handling Conditions for Comprehensive Liquid Biopsy Analysis. J. Mol. Diagnostics 2020, 22, 1070–1086. [Google Scholar] [CrossRef] [PubMed]
- Gits, C.M.M.; Van Kuijk, P.F.; Jonkers, M.B.E.; Boersma, A.W.M.; Smid, M.; Van Ijcken, W.F.; Coindre, J.M.; Chibon, F.; Verhoef, C.; Mathijssen, R.H.J.; et al. MicroRNA expression profiles distinguish liposarcoma subtypes and implicate miR-145 and miR-451 as tumor suppressors. Int. J. Cancer 2014, 135, 348–361. [Google Scholar] [CrossRef] [PubMed]
- Braig, D.; Becherer, C.; Bickert, C.; Braig, M.; Claus, R.; Eisenhardt, A.E.; Heinz, J.; Scholber, J.; Herget, G.W.; Bronsert, P.; et al. Genotyping of circulating cell-free DNA enables noninvasive tumor detection in myxoid liposarcomas. Int. J. Cancer 2019, 145, 1148–1161. [Google Scholar] [CrossRef]
- Jung, J.; Lee, J.S.; Dickson, M.A.; Schwartz, G.K.; Le Cesne, A.; Varga, A.; Bahleda, R.; Wagner, A.J.; Choy, E.; De Jonge, M.J.; et al. TP53 mutations emerge with HDM2 inhibitor SAR405838 treatment in de-differentiated liposarcoma. Nat. Commun. 2016, 7, 1–7. [Google Scholar] [CrossRef]
- Fricke, A.; Cimniak, A.F.V.; Ullrich, P.V.; Becherer, C.; Bickert, C.; Pfeifer, D.; Heinz, J.; Stark, G.B.; Bannasch, H.; Braig, D.; et al. Whole blood MIRNA expression analysis reveals MIR-3613-3p as a potential biomarker for dedifferentiated liposarcoma. Cancer Biomarkers 2018, 22, 199–207. [Google Scholar] [CrossRef]
- Hemming, M.L.; Klega, K.; Rhoades, J.; Ha, G.; Acker, K.E.; Andersen, J.L.; Thai, E.; Nag, A.; Thorner, A.R.; Raut, C.P.; et al. Detection of Circulating Tumor DNA in Patients With Leiomyosarcoma With Progressive Disease. JCO Precis. Oncol. 2019, 3, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Demoret, B.; Gregg, J.; Liebner, D.A.; Tinoco, G.; Lenobel, S.; Chen, J.L. Prospective evaluation of the concordance of commercial circulating tumor dna alterations with tumor-based sequencing across multiple soft tissue sarcoma subtypes. Cancers 2019, 11, 1829. [Google Scholar] [CrossRef] [Green Version]
- Miller, I.V.; Raposo, G.; Welsch, U.; Prazeres da Costa, O.; Thiel, U.; Lebar, M.; Maurer, M.; Bender, H.U.; von Luettichau, I.; Richter, G.H.S.; et al. First identification of Ewing’s sarcoma-derived extracellular vesicles and exploration of their biological and potential diagnostic implications. Biol. Cell 2013, 105, 289–303. [Google Scholar] [CrossRef] [PubMed]
- Tsugita, M.; Yamada, N.; Noguchi, S.; Yamada, K.; Moritake, H.; Shimizu, K.; Akao, Y.; Ohno, T. Ewing Sarcoma Cells Secrete EWS/Fli-1 Fusion mRNA via Microvesicles. PLoS ONE 2013, 8, e0077416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benini, S.; Gamberi, G.; Cocchi, S.; Garbetta, J.; Alberti, L.; Righi, A.; Gambarotti, M.; Picci, P.; Ferrari, S. Detection of circulating tumor cells in liquid biopsy from Ewing sarcoma patients. Cancer Manag. Res. 2018, 10, 49–60. [Google Scholar] [CrossRef] [Green Version]
- Krumbholz, M.; Hellberg, J.; Steif, B.; Bäuerle, T.; Gillmann, C.; Fritscher, T.; Agaimy, A.; Frey, B.; Juengert, J.; Wardelmann, E.; et al. Genomic EWSR1 fusion sequence as highly sensitive and dynamic plasma tumor marker in ewing sarcoma. Clin. Cancer Res. 2016, 22, 4356–4365. [Google Scholar] [CrossRef] [Green Version]
- Allegretti, M.; Casini, B.; Mandoj, C.; Benini, S.; Alberti, L.; Novello, M.; Melucci, E.; Conti, L.; Covello, R.; Pescarmona, E.; et al. Precision diagnostics of Ewing’s sarcoma by liquid biopsy: Circulating EWS-FLI1 fusion transcripts. Ther. Adv. Med. Oncol. 2018, 10, 1758835918774337. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, M.; Chu, D.; Meyer, C.F.; Llosa, N.J.; McCarty, G.; Morris, C.D.; Levin, A.S.; Wolinsky, J.-P.; Albert, C.M.; Steppan, D.A.; et al. Highly Personalized Detection of Minimal Ewing Sarcoma Disease Burden from Plasma Tumor DNA. Cancer 2016, 122, 3015–3023. [Google Scholar] [CrossRef]
- Samuel, G.; Crow, J.; Klein, J.B.; Merchant, M.L.; Nissen, E.; Koestler, D.C.; Laurence, K.; Liang, X.; Neville, K.; Staggs, V.; et al. Ewing sarcoma family of tumors-derived small extracellular vesicle proteomics identify potential clinical biomarkers. Oncotarget 2020, 11, 2995–3012. [Google Scholar] [CrossRef] [PubMed]
- Klega, K.; Imamovic-Tuco, A.; Ha, G.; Clapp, A.N.; Meyer, S.; Ward, A.; Clinton, C.; Nag, A.; Van Allen, E.; Mullen, E.; et al. Detection of Somatic Structural Variants Enables Quantification and Characterization of Circulating Tumor DNA in Children With Solid Tumors. JCO Precis. Oncol. 2018, 2, 1–13. [Google Scholar] [CrossRef]
- Miyachi, M.; Tsuchiya, K.; Yoshida, H.; Yagyu, S.; Kikuchi, K.; Misawa, A.; Iehara, T.; Hosoi, H. Circulating muscle-specific microRNA, miR-206, as a potential diagnostic marker for rhabdomyosarcoma. Biochem. Biophys. Res. Commun. 2010, 400, 89–93. [Google Scholar] [CrossRef]
- Mihály, D.; Nagy, N.; Papp, G.; Pápai, Z.; Sápi, Z. Release of circulating tumor cells and cell-free nucleic acids is an infrequent event in synovial sarcoma: Liquid biopsy analysis of 15 patients diagnosed with synovial sarcoma. Diagn. Pathol. 2018, 13, 1–7. [Google Scholar] [CrossRef]
- Przybyl, J.; Van De Rijn, M.; Rutkowski, P. Detection of SS18-SSX1/2 fusion transcripts in circulating tumor cells of patients with synovial sarcoma. Diagn. Pathol. 2019, 14, 14–15. [Google Scholar] [CrossRef] [PubMed]
- Uotani, K.; Fujiwara, T.; Yoshida, A.; Iwata, S.; Morita, T.; Kiyono, M.; Yokoo, S.; Kunisada, T.; Takeda, K.; Hasei, J.; et al. Circulating MicroRNA-92b-3p as a Novel Biomarker for Monitoring of Synovial Sarcoma. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shulman, D.S.; Klega, K.; Imamovic-Tuco, A.; Clapp, A.; Nag, A.; Thorner, A.R.; Van Allen, E.; Ha, G.; Lessnick, S.L.; Gorlick, R.; et al. Detection of circulating tumour DNA is associated with inferior outcomes in Ewing sarcoma and osteosarcoma: A report from the Children’s Oncology Group. Br. J. Cancer 2018, 119, 615–621. [Google Scholar] [CrossRef]
- Barris, D.M.; Weiner, S.B.; Dubin, R.A.; Fremed, M.; Zhang, X.; Piperdi, S.; Zhang, W.; Maqbool, S.; Gill, J.; Roth, M.; et al. Detection of circulating tumor DNA in patients with osteosarcoma. Oncotarget 2018, 9, 12695–12704. [Google Scholar] [CrossRef] [Green Version]
- Raimondi, L.; De Luca, A.; Costa, V.; Amodio, N.; Carina, V.; Bellavia, D.; Tassone, P.; Pagani, S.; Fini, M.; Alessandro, R.; et al. Circulating biomarkers in osteosarcoma: New translational tools for diagnosis and treatment. Oncotarget 2017, 8, 100831–100851. [Google Scholar] [CrossRef] [Green Version]
- Satelli, A.; Li, S. Vimentin as a potential molecular target in cancer therapy Or Vimentin, an overview and its potential as a molecular target for cancer therapy. Cell Mol. Life Sci. 2011, 68, 3033–3046. [Google Scholar] [CrossRef] [Green Version]
- Zhong, G.X.; Feng, S.D.; Shen, R.; Wu, Z.Y.; Chen, F.; Zhu, X. The clinical significance of the Ezrin gene and circulating tumor cells in osteosarcoma. OncoTargets Ther. 2017, 10, 527–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Gao, P.; Xiao, X.; Heger, M.; Geng, L.; Fan, B.; Yuan, Y.; Huang, C.; Chen, G.; Liu, Y.; et al. A liquid biopsy-based method for the detection and quantification of circulating tumor cells in surgical osteosarcoma patients. Int. J. Oncol. 2017, 50, 1075–1086. [Google Scholar] [CrossRef]
- Baglio, S.R.; Lagerweij, T.; Pérez-Lanzón, M.; Ho, X.D.; Léveillé, N.; Melo, S.A.; Cleton-Jansen, A.M.; Jordanova, E.S.; Roncuzzi, L.; Greco, M.; et al. Blocking tumor-educated MSC paracrine activity halts osteosarcoma progression. Clin. Cancer Res. 2017, 23, 3721–3733. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.F.; Wang, Y.P.; Zhang, S.J.; Chen, Y.; Gu, H.F.; Dou, X.F.; Xia, B.; Bi, Q.; Fan, S.W. Exosomes containing differential expression of microRNA and mRNA in osteosarcoma that can predict response to chemotherapy. Oncotarget 2017, 8, 75968–75978. [Google Scholar] [CrossRef] [PubMed]
- Gutteridge, A.; Rathbone, V.M.; Gibbons, R.; Bi, M.; Archard, N.; Davies, K.E.J.; Brown, J.; Plagnol, V.; Pillay, N.; Amary, F.; et al. Digital PCR analysis of circulating tumor DNA: A biomarker for chondrosarcoma diagnosis, prognostication, and residual disease detection. Cancer Med. 2017, 6, 2194–2202. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Chen, S.; Luo, P.; Yan, W.; Wang, C. Liposarcoma: Advances in cellular and molecular genetics alterations and corresponding clinical treatment. J. Cancer 2020, 11, 100–107. [Google Scholar] [CrossRef] [Green Version]
- Huang, X.D.; Xiao, F.J.; Wang, S.X.; Yin, R.H.; Lu, C.R.; Li, Q.F.; Liu, N.; Zhang, Y.; Wang, L.S.; Li, P.Y. G protein pathway suppressor 2 (GPS2) acts as a tumor suppressor in liposarcoma. Tumor Biol. 2016, 37, 13333–13343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jo, V.Y.; Fletcher, C.D.M. WHO classification of soft tissue tumours: An update based on the 2013 (4th) edition. Pathology 2014, 46, 95–104. [Google Scholar] [CrossRef]
- Van Beeck, A.; van de Sande, M.; van Praag, V.; Dammerer, D.; Michielsen, J.; Schubert, T.; Kapanci, B.; Shumelinsky, F.; Somville, J.; Dijkstra, S. Clinical Outcome of Surgically Treated Leiomyosarcoma of the Extremities: A Retrospective Overview. Anticancer Res. 2020, 40, 5319–5325. [Google Scholar] [CrossRef]
- George, S.; Serrano, C.; Hensley, M.L.; Ray-Coquard, I. Soft tissue and uterine leiomyosarcoma. J. Clin. Oncol. 2018, 36, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Chudasama, P.; Mughal, S.S.; Sanders, M.A.; Hübschmann, D.; Chung, I.; Deeg, K.I.; Wong, S.H.; Rabe, S.; Hlevnjak, M.; Zapatka, M.; et al. Integrative genomic and transcriptomic analysis of leiomyosarcoma. Nat. Commun. 2018, 9, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulussen, M.; Ahrens, S.; Burdach, S.; Craft, A.; Dockhorn-Dworniczak, B.; Dunst, J.; Fröhlich, B.; Winkelmann, W.; Zoubek, A.; Jürgens, H. Primary metastatic (stage IV) Ewing tumor: Survival analysis of 171 patients from the EICESS studies. European Intergroup Cooperative Ewing Sarcoma Studies. Ann. Oncol. 1998, 9, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Ladenstein, R.; Pötschger, U.; Le Deley, M.C.; Whelan, J.; Paulussen, M.; Oberlin, O.; Van Den Berg, H.; Dirksen, U.; Hjorth, L.; Michon, J.; et al. Primary disseminated multifocal Ewing sarcoma: Results of the Euro-EWING 99 trial. J. Clin. Oncol. 2010, 28, 3284–3291. [Google Scholar] [CrossRef]
- Janknecht, R. EWS-ETS oncoproteins: The linchpins of Ewing tumors. Gene 2005, 363, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Skapek, S.X.; Ferrari, A.; Gupta, A.A.; Lupo, P.J.; Butler, E.; Shipley, J.; Barr, F.G.; Hawkins, D.S. Rhabdomyosarcoma. Nat. Rev. Dis. Prim. 2019, 5, 14–16. [Google Scholar] [CrossRef]
- Perez, E.A.; Kassira, N.; Cheung, M.C.; Koniaris, L.G.; Neville, H.L.; Sola, J.E. Rhabdomyosarcoma in children: A SEER population based study. J. Surg. Res. 2011, 170, e243–e251. [Google Scholar] [CrossRef]
- Lychou, S.E.; Gustafsson, G.G.; Ljungman, G.E. Higher rates of metastatic disease may explain the declining trend in Swedish paediatric rhabdomyosarcoma survival rates. Acta Paediatr. Int. J. Paediatr. 2016, 105, 74–81. [Google Scholar] [CrossRef]
- Sorensen, P.H.B.; Lynch, J.C.; Qualman, S.J.; Tirabosco, R.; Lim, J.F.; Maurer, H.M.; Bridge, J.A.; Crist, W.M.; Tricke, T.J.; Barr, F.G. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: A report from the Children’s Oncology Group. J. Clin. Oncol. 2002, 20, 2672–2679. [Google Scholar] [CrossRef]
- Baranov, E.; McBride, M.J.; Bellizzi, A.M.; Ligon, A.H.; Fletcher, C.D.M.; Kadoch, C.; Hornick, J.L. A Novel SS18-SSX Fusion-specific Antibody for the Diagnosis of Synovial Sarcoma. Am. J. Surg. Pathol. 2020, 44, 922–933. [Google Scholar] [CrossRef]
- El Beaino, M.; Araujo, D.M.; Lazar, A.J.; Lin, P.P. Synovial Sarcoma: Advances in Diagnosis and Treatment Identification of New Biologic Targets to Improve Multimodal Therapy. Ann. Surg. Oncol. 2017, 24, 2145–2154. [Google Scholar] [CrossRef]
- Amary, M.F.C.; Berisha, F.; Bernardi, F.D.C.; Herbert, A.; James, M.; Reis-Filho, J.S.; Fisher, C.; Nicholson, A.G.; Tirabosco, R.; Diss, T.C.; et al. Detection of SS18-SSX fusion transcripts in formalin-fixed paraffin-embedded neoplasms: Analysis of conventional RT-PCR, qRT-PCR and dual color FISH as diagnostic tools for synovial sarcoma. Mod. Pathol. 2007, 20, 482–496. [Google Scholar] [CrossRef]
- Wei, Y.; Wang, J.; Zhu, X.; Shi, D.; Hisaoka, M.; Hashimoto, H. Detection of SYT-SSX fusion transcripts in paraffin-embedded tissues of synovial sarcoma by reverse transcription-polymerase chain reaction. Chin. Med. J. 2002, 115, 1043–1047. [Google Scholar]
- Hashimoto, N.; Myoui, A.; Araki, N.; Asai, T.; Sonobe, H.; Hirota, S.; Yoshikawa, H. Detection of SYT-SSX fusion gene in peripheral blood from a patient with synovial sarcoma. Am. J. Surg. Pathol. 2001, 25, 406–410. [Google Scholar] [CrossRef]
- Mehle, N.; Dobnik, D.; Ravnikar, M.; Pompe Novak, M. Validated reverse transcription droplet digital PCR serves as a higher order method for absolute quantification of Potato virus Y strains. Anal. Bioanal. Chem. 2018, 410, 3815–3825. [Google Scholar] [CrossRef]
- Przybyl, J.; Kozak, K.; Kosela, H.; Falkowski, S.; Switaj, T.; Lugowska, I.; Szumera-Cieckiewicz, A.; Ptaszynski, K.; Grygalewicz, B.; Chechlinska, M.; et al. Gene expression profiling of peripheral blood cells: New insights into Ewing sarcoma biology and clinical applications. Med. Oncol. 2014, 31, 109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bishop, M.W.; Janeway, K.A.; Gorlick, R. Future Directions in the Treatment of Osteosarcoma. Curr. Opin Pediatr. 2016, 28, 26–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czarnecka, A.M.; Synoradzki, K.; Firlej, W.; Bartnik, E.; Sobczuk, P.; Fiedorowicz, M.; Grieb, P.; Rutkowski, P. Molecular biology of osteosarcoma. Cancers 2020, 12, 2130. [Google Scholar] [CrossRef] [PubMed]
- Zumárraga, J.P.; Baptista, A.M.; De La Rosa, L.P.; Caiero, M.T.; De Camargo, O.P. Serum values of alkaline phosphatase and lactate dehydrogenase in osteosarcoma. Acta Ortop. Bras. 2016, 24, 142–146. [Google Scholar] [CrossRef] [Green Version]
- Hu, T.; Yang, Q.; Xu, J.; Zhang, Z.; He, N.; Du, Y. Role of betaisomerized C-terminal telopeptides (beta-CTx) and total procollagen type 1 amino-terminal propeptide (tP1NP) as osteosarcoma biomarkers. Int. J. Clin. Exp. Med. 2015, 8, 890–896. [Google Scholar] [PubMed]
- Kong, Y.W.; Ferland-McCollough, D.; Jackson, T.J.; Bushell, M. MicroRNAs in cancer management. Lancet Oncol. 2012, 13, e249–e258. [Google Scholar] [CrossRef]
- Joosse, S.A.; Pantel, K. Biologic challenges in the detection of circulating tumor cells. Cancer Res. 2013, 73, 8–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whiteside, T. Tumor-derived exosomes and their role in cancer progression. Adv. Clin. Chem. 2016, 176, 100–106. [Google Scholar] [CrossRef]
- Leddy, L.R.; Holmes, R.E. Chondrosarcoma of bone. In Orthopaedic Oncology. Cancer Treatment and Research, 162th ed.; Peabody, T.D., Attar, S., Eds.; Springer: Cham, Switzerland, 2014; pp. 117–130. [Google Scholar]
- Benini, S.; Cocchi, S.; Gamberi, G.; Magagnoli, G.; Vogel, D.; Ghinelli, C.; Righi, A.; Picci, P.; Alberghini, M.; Gambarotti, M. Diagnostic utility of molecular investigation in extraskeletal myxoid chondrosarcoma. J. Mol. Diagn. 2014, 16, 314–323. [Google Scholar] [CrossRef]
- Yamagishi, A.; Ichiyanagi, O.; Naito, S.; Ito, H.; Kabasawa, T.; Yamakawa, M.; Tsuchiya, N. Primary mesenchymal chondrosarcoma of the kidney without HEY1-NCOA2 and IRF2BP2-CDX1 fusion: A case report and review. Oncol. Lett. 2020, 19, 885–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Markers Studied | Samples Included | Methods | Results | Ref |
|---|---|---|---|---|
| Liposarcoma | ||||
| 57 tissue samples and liquid biopsies | miR microarray |
| [12] |
| Patients with STS (n = 64) Patients with remission (n = 19) Healthy controls (n = 41) Patients with myxoid liposarcomas (n = 4)Patients with well-differentiated/de-differentiated liposarcomas (n = 5) | qRT-PCR |
| [13] |
| TP53 mutations in cfDNA | DDL (n = 21) | cfDNA isolation from plasma with double centrifugation |
| [14] |
| DDL patients (n = 6) Healthy individuals (n = 4) | qRT-PCR | miR-3613-3p is a specific biomarker for DDL | [15] |
| Leiomyosarcoma | ||||
| Patients (n = 30) 29/30 patients with matched tumor sample 8 patients with tumor samples only | Extracted DNA was quantified using Quant-iT PicoGreen dsDNA Assay Kit |
| [16] |
| Patients (n = 6)−blood samples | FoundationACT™ assay (F1ACT) | No correlation between tumor fraction or radiographic tumor volume | [17] |
| Ewing sarcoma | ||||
| ES cell lines (A673, SK-N-MC and SB-KMS-KS1) | qRT-PCR (Exosomes were prepared from the cell culture supernatant) | exosomes are potential biomarkers for diagnosis of minimal residual disease | [18] |
|
| qRT-PCR | EWS/Fli-1 mRNA in microvesicles is a potential non-invasive biomarker | [19] |
| Blood samples from
| qRT-PCR | CTCs in liquids can be used for prognostic and predictive purposes | [20] |
| 234 blood samples from 20 ES patients before and after multimodal treatment | droplet digital PCR | ctDNA for the monitoring of therapy response | [21] |
| EWS-FLI1 DNA breakpoints | Blood samples and tissue biopsy from ES patients (n=5) |
| EWS-FLI1 DNA useful in monitoring:
| [22] |
| EWS-ETS fusion gene breakpoint ptDNA fragments |
|
| EWS-ETS fusion gene breakpoint ptDNA fragments is a specific biomarker to monitor tumor relapse | [23] |
| EWS-ETS transcripts | ESFT cell lines (n = 5) | Proteomic study of ESFT-derived sEVs from 5 ESFT cell lines | sEVs are potential prognostic biomarkers | [24] |
| Rhabdomyosarcoma | ||||
| ctDNA | ARMS patients (n = 7) | ULP-WGS |
| [25] |
| miR-206 |
| RT-qPCR | serum miR-206 expression differentiates RMS and non-RMS tumors | [26] |
| Synovial sarcoma | ||||
| SS18-SSX fusion genes from CTCs or cell-free nucleic acids | Blood sample from SS patients (n = 15) |
|
| [27] |
| SS18-SSX1/2 fusion genes in CTCs | Blood samples from SS patients (n = 38) | nested PCR |
| [28] |
| miR-92b-3p |
| RT-qPCR |
| [29] |
| Markers Studied | Samples Included | Methods | Results | Ref |
|---|---|---|---|---|
| Osteosarcoma | ||||
| ctDNA | blood samples of OS patients (n = 72) | NGS assays |
| [30] |
| mutated alterations in TP53, RB1, ATRX, DLG2, PTEN, MET, and SLC19A1 in ctDNA | blood samples OS patients (n = 7) | NGS assays | clinical relapse in 3 patients with germline-tumor pairs | [31] |
| Blood samples of OS compared with health controls | RT-qPCR |
| [32] |
CTCs
| Blood samples of OS patients | RNA probe technology FISH to detect centromeres of chromosome 8 |
| [33,34,35] |
| extracellular vesicle (EV)-educated mesenchymal stem cells (TEMSC) which express a membrane-associated form of TGFβ | Blood samples from OS mice xenograft models | RT-qPCR | Prognostic and predictive tool in OS | [36] |
| Exosomes containing: miR-124, miR133a, miR-199a-3p, and miR-385 | Blood samples of:
| RT-qPCR | exosomal miRNAs could be reliable circulating biomarkers to discriminate poor from good treatment responders | [37] |
| Chondrosarcoma | ||||
| IDH1 and IDH2 mutations in ctDNA | Blood samples from patients with central chondrosarcoma (n = 29) | digital PCR |
| [38] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadjimichael, A.C.; Pergaris, A.; Kaspiris, A.; Foukas, A.F.; Theocharis, S.E. Liquid Biopsy: A New Translational Diagnostic and Monitoring Tool for Musculoskeletal Tumors. Int. J. Mol. Sci. 2021, 22, 11526. https://doi.org/10.3390/ijms222111526
Hadjimichael AC, Pergaris A, Kaspiris A, Foukas AF, Theocharis SE. Liquid Biopsy: A New Translational Diagnostic and Monitoring Tool for Musculoskeletal Tumors. International Journal of Molecular Sciences. 2021; 22(21):11526. https://doi.org/10.3390/ijms222111526
Chicago/Turabian StyleHadjimichael, Argyris C., Alexandros Pergaris, Angelos Kaspiris, Athanasios F. Foukas, and Stamatios E. Theocharis. 2021. "Liquid Biopsy: A New Translational Diagnostic and Monitoring Tool for Musculoskeletal Tumors" International Journal of Molecular Sciences 22, no. 21: 11526. https://doi.org/10.3390/ijms222111526






